Introduction
Lung cancer is the leading cause of cancer-related
mortality worldwide, approximately 80% of which is non-small cell
lung cancer (NSCLC) (1). Currently,
the traditional cytotoxic chemotherapy has reached a plateau with
respect to efficacy, with limited survival benefits for advanced
NSCLC patients.
Target-based therapies have improved survival rates
in patients with a variety of cancers, including NSCLC. Certain
epidermal growth factor receptor tyrosine kinase inhibitors
(EGFR-TKIs), including gefitinib and erlotinib, have been approved
as second-line treatments for lung cancer. However, EGFR-TKIs have
little effect in NSCLC patients with KRAS, BRAF or EGFR-T790M
mutations (2–4). The KRAS and BRAF mutations are tandem
activating mutations in the RAS/RAF/MEK/ERK signaling pathway.
Taken together, the KRAS or BRAF mutations may be present in
approximately 50% of NSCLCs (5).
The EGFR-T790M mutation is associated with acquired resistance to
EGFR-TKIs. Patients with this mutation are considered to be
resistant to cytotoxic chemotherapeutic agents and unsuitable for
EGFR-TKI treatment (6). Therefore,
there is an urgent requirement to identify new treatment strategies
to improve the clinical efficacy of NSCLC therapy.
Sorafenib (BAY 43-9006) is an oral multi-kinase
inhibitor that targets tumor growth, survival and angiogenesis.
Sorafenib inhibits tumor cell growth directly by affecting Raf
kinases, which are critical proliferation and cell survival
signaling molecules downstream of RAS in the RAF/MEK/ERK signaling
pathway. It also inhibits tumor angiogenesis and metastasis by
decreasing the activity of the vascular endothelial growth factor
receptor-2/3 (VEGFR-2 and VEGFR-3) and platelet-derived growth
factor receptor-β (PDGFR-β) (7).
Studies have shown that sorafenib inhibits MEK and ERK
phosphorylation and has a wide range of antitumor effects in
various cancer cell lines and tumor xenografts (8). Single-agent sorafenib has demonstrated
clinical activity against NSCLC in the first-line setting (9–11).
Currently, there is interest in assessing the
efficacy of sorafenib given in combination with conventional
cytotoxic chemotherapy agents. Gemcitabine is a pyrimidine
nucleoside antimetabolite agent with a favorable toxicity profile,
which is active against a variety of human malignancies, including
NSCLC, and has been frequently used in combinatorial treatments
with other anticancer agents (12).
In the current study we examined in vitro the
antitumor effect and related mechanisms of sorafenib combined with
gemcitabine in EGFR-TKI-resistant NSCLC cell lines.
Materials and methods
Cell lines and chemicals
EGFR-TKI-resistant lung cancer cell lines A549
(mutant KRAS/wild-type EGFR), H1666 (mutant BRAF/wild-type EGFR)
and H1975 (mutant EGFR-T790M/wild-type KRAS) were purchased from
the American Type Culture Collection (Manassas, VA, USA) and were
maintained in RPMI-1640 medium (Hyclone, Logan, UT, USA) with 10%
heat-inactivated fetal bovine serum (Hyclone), 100 U/ml penicillin
and 100 mg/l streptomycin at 37°C in a 5% CO2
atmosphere. Sorafenib was obtained from Bayer (Leverkusen, Germany)
and gemcitabine was purchased as a commercial product from our
hospital pharmacy.
Analysis of the antitumor effects of
sorafenib and gemcitabine
The MTT assay was used to determine the antitumor
effects of each drug. Briefly, cells in 96-well plates were treated
with escalating doses of sorafenib (0.78–25 μM) or
gemcitabine (0.78–25 nM) for 72 h and then 20 μl MTT
solution was added to 200 μl media in each well. The
absorbance was determined at 490 nm after 4 h of incubation. The
percentage of cell growth inhibition resulting from each drug was
calculated as: (OD490control cells − OD490treated
cells)/OD490control cells × 100. This assay was
repeated as more than three independent experiments.
Determination of a synergistic antitumor
effect between sorafenib and gemcitabine
The A549, H1666 and H1975 cells were concurrently
exposed to sorafenib and gemcitabine for 72 h. The combination drug
dosing was carried out using constant ratios of the IC50
values. Thus, the combination index (CI) value was calculated using
0.125, 0.25, 0.5, 1, 2 and 4 times the IC50 values of
sorafenib and gemcitabine combination doses. The CI values of the
interactions between sorafenib and gemcitabine were analyzed
according to the Chou and Talalay method using CompuSyn software
(ComboSyn, Inc., Paramus, NJ, USA). CI>1, CI=1 and CI<1
indicated antagonistic, additive and synergistic effects,
respectively (13).
Cell cycle analysis
Cell cycle analysis was conducted using flow
cytometry. The A549, H1666 and H1975 cells were treated with
sorafenib and gemcitabine as single agents or in combination using
constant ratios of the IC50 levels, harvested after 72 h
and fixed in 80% ethanol on ice. All cell samples were kept in a
−2°C freezer until analysis by flow cytometry. Once the cells were
removed from the freezer, 1 ml cold phosphate-buffered saline (PBS)
was added and the samples were centrifuged. After washing with cold
PBS twice, DNA staining was performed using a solution of propidium
iodide (0.05 mg/ml) and RNase (2 mg/ml) for 30 min at room
temperature. Cells were analyzed using a FACScan cytometer and the
percentages of cells in the G1, S and G2/M phases of the cell cycle
were estimated using Cell Lab Quanta SC Software.
Western blot analysis
A549, H1666 and H1975 cells (1×106/well)
were treated with sorafenib and gemcitabine as single agents and in
combination for 72 h. The cells were washed with ice-cold PBS
solution and scraped in lysis buffer. The lysates were centrifuged
at 14,000 rpm for 30 min at 4°C and the supernatant was collected.
Equivalent amounts of proteins were analyzed by sodium dodecyl
sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and
transferred to PVDF membranes. Appropriate primary antibodies to
B-RAF, C-RAF, pAKT, AKT, pERK1/2, ERK1/2, Bcl-2 and β-actin,
purchased from Cell Signaling Technology (Beverly, MA, USA), were
used. Proteins were visualized with a horseradish
peroxidase-coupled secondary antibody from Cell Signaling
Technology. Specific bands were detected using an enhanced
chemiluminescence reagent (ECL; PerkinElmer Life Sciences, Inc.,
Boston, MA, USA) on autoradiographic film and quantitated by
densitometry.
Statistical analysis
Unless specified, the results are expressed as the
mean ± SD of data collected from at least three independent
experiments. The Student’s t-test was used to determine the
differences between control and treatment groups. P<0.05 was
considered to indicate a statistically significant result.
Results
Antiproliferative effects of sorafenib
and gemcitabine alone or in combination in EGFR-TKI-resistant NSCLC
cells
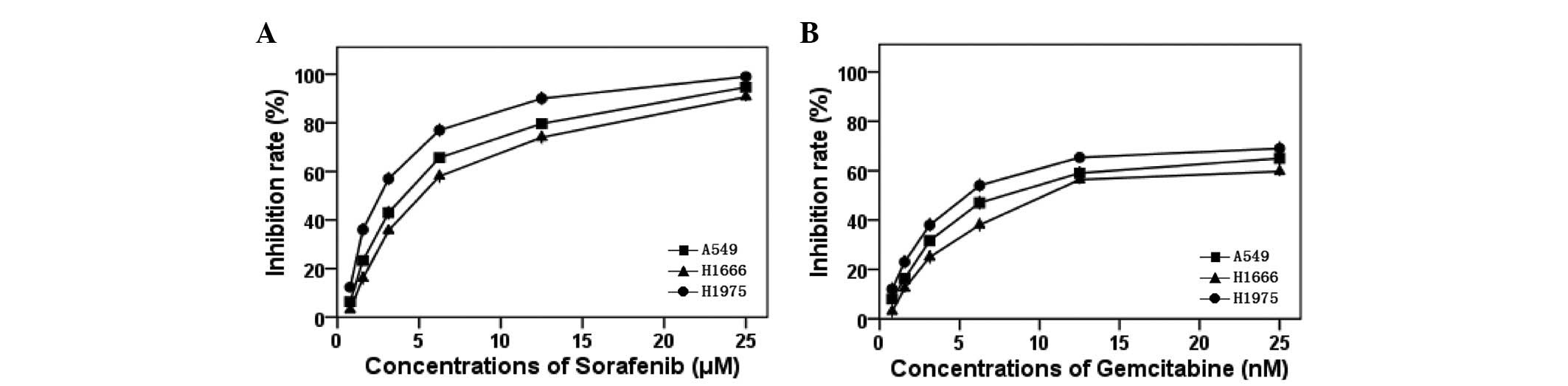
Sorafenib and gemcitabine showed a dose- and
time-dependent antitumor effect in the A549, H1666 and H1975 cells
(Fig. 1). After 72-h exposure to
sorafenib, the IC50 values in the A549, H1666 and H1975
cells were 4.08±0.14, 5.52±0.53 and 2.54±0.01 μM,
respectively. The IC50 values of sorafenib in the three
cells are within the clinically relevant concentration range for
this drug (14). We conclude that
the EGFR-TKI-resistant NSCLC cells are sensitive to sorafenib.
Table I summarizes the
IC50 values of gemcitabine and sorafenib.
 | Table IIC50 values of sorafenib
and gemcitabine determined by MTT assay. |
Table I
IC50 values of sorafenib
and gemcitabine determined by MTT assay.
| IC50 | A549 | H1666 | H1975 |
|---|
| Sorafenib
(μM) | 4.08±0.14 | 5.52±0.53 | 2.54±0.01 |
| Gemcitabine (nM) | 9.21±0.36 | 11.65±0.19 | 6.73±0.11 |
When exposed to a combination of sorafenib and
gemcitabine, synergistic activity was observed in the A549 and
H1666 cells (CI<1), while antagonistic activity was observed in
the H1975 cells (CI>1; Fig.
2).
Cell cycle effects of sorafenib and
gemcitabine
Flow cytometry was used to evaluate the cell cycle
phase distributions in the NSCLC cells following single-drug and
concurrent administration of gemcitabine and sorafenib for 72 h.
Following sorafenib treatment, the proportions of the A549, H1666
and H1975 cells in the G0/G1 phase were increased, relative to
control values (P<0.05). With gemcitabine alone, the S phase
fraction increased in the three cell lines (P<0.05; Fig. 3).
When exposed to the combination of gemcitabine and
sorafenib, the proportions of cells in the G0/G1 and S phases
increased in the A549 and H1666 cells (P<0.05). However, in the
H1975 cells, the proportion of cells in the G0/G1 phase increased
and the proportion in the S phase decreased (Fig. 3).
Effects of sorafenib and gemcitabine
alone or in combination on downstream signaling pathways
We identified that gemcitabine upregulated the level
of p-ERK in the three cell lines and increased the level of p-AKT
in the H1975 cells at its IC50. When the A549 and H1666
cells were exposed to sorafenib at its IC50 for 72 h,
the levels of p-AKT, p-ERK and Bcl-2 were decreased compared with
those of unexposed cells, while in H1975 cells, sorafenib decreased
only the levels of p-AKT (Fig. 4).
We found that sorafenib inhibited C-RAF in A549 cells but B-RAF in
H1666 and H1975 cells (Fig. 5).
In addition, we identified that when the A549 and
H1666 cells were exposed to a combination of gemcitabine and
sorafenib for 72 h, the levels of p-AKT, p-ERK and Bcl-2 were
decreased compared with their levels in the control, whereas, in
the H1975 cells, the combination of the two drugs increased the
levels of p-AKT and p-ERK. However, there was no significant
variation in the total ERK and AKT expression levels compared with
the control (Fig. 4).
Discussion
Targeted anticancer drugs, including the EGFR-TKIs
gefitinib and erlotinib, have been approved for the treatment of
lung cancer. Patients with EGFR mutations may greatly benefit from
treatment with EGFR-TKIs (15–17).
However, the presence of KRAS, BRAF and EGFR-T790M mutations are
associated with primary or acquired resistance to EGFR-TKIs. The
development of new treatment strategies for NSCLC patients is thus
an important clinical goal.
There is multilevel cross-stimulation among the
targets in lung cancer; when only one of these pathways is blocked
others act as salvage or escape mechanisms for the cancer cells.
Anticancer agents that interfere at different stages may preclude
an escape or salvage mechanism for the cancer cells and therefore
be more effective than single-targeted agents (18). The RAS/RAF/MEK/ERK and
RAS/PI3K/PTEN/AKT pathways interact with each other to regulate
growth and play key roles in the transmission of proliferative
signals, in some cases contributing to tumorigenesis. In NSCLC, the
activation of KRAS and BRAF leads to ERK1/2 overexpression through
the RAF/MEK/ERK signaling pathway (19–21).
Hence, inhibition of the RAS/RAF/MEK/ERK signaling pathway is an
important strategy in anticancer drug development. Sorafenib is a
novel, multi-kinase inhibitor that targets tumor proliferation and
tumor angiogenesis (7). It has been
approved for the treatment of advanced renal cell cancer (RCC) and
is currently being evaluated for the treatment of other tumors.
The present study was performed in
EGFR-TKI-resistant A549 (mutant KRAS/wild-type EGFR), H1666 (mutant
BRAF/wild-type EGFR) and H1975 (mutant EGFR-T790M/ wild-type KRAS)
human lung cancer cell lines to investigate the antiproliferative
effects of sorafinib as a single agent and in combination with
gemcitabine. We found that sorafenib and gemcitabine exhibited dose
dependent growth inhibition of cell growth when used as single
agents to treat A549, H1666 and H1975 lung cancer cells. This
suggests that sorafenib is efficacious for inhibiting growth in
EGFR-TKI-resistant NSCLC cell lines. Synergism was observed when
sorafenib was combined with gemcitabine in the A549 and H1666
cells, whereas antagonistic interactions were observed in the H1975
cells.
The synergistic and antagonistic effects may be
explained by differences in the changes induced in the cell cycle.
In our study, sorafenib arrested cells at the G1 phase and
gemcitabine caused S phase accumulation in all three cell lines.
When exposed to a combination of gemcitabine and sorafenib, the
proportions of cells in the G0/G1 and S phases increased in the
A549 and H1666 cells. We conclude that sorafenib and gemcitabine
modulate the cell cycle phase independently of each other in A549
and H1666 cells and generated an additive effect, without
disturbing each other. However, in the H1975 cells, the proportion
of cells in the G0/G1 phase increased and in the S phase decreased.
Sorafenib mainly arrested cells at the G1 phase, thereby
interfering with the cytotoxic effects of gemcitabine in the S
phase, resulting in decreased cytotoxicity.
The differences in the antiproliferative effects of
sorafenib combined with gemcitabine may also result from their
effects on growth signaling pathways. We identified that
gemcitabine increased the levels of p-ERK in the A549, H1666 and
H1975 cells and in the H1975 cells, p-AKT levels were also
upregulated by gemcitabine. Similar to our results, a previous
study reported that cell signaling pathways may be gradually
activated by chemotherapy (22).
Phosphorylated ERK and AKT play important roles in tumor cell
proliferation; gemcitabine induced ERK and AKT phosphorylation,
leading to the prevention of apoptosis.
We have shown that sorafenib inhibited the activity
of p-AKT, p-ERK and Bcl-2 in the A549 and H1666 cells after 72 h
exposure, while in the H1975 cells, sorafenib downregulated the
level of p-AKT but not the levels of p-ERK and Bcl-2. We conclude
that sorafenib inhibited the expression of Bcl-2 in the A549 and
H1666 cells, mainly due to its inhibition of the RAF/MEK/ERK
downstream pathway. We also identified that sorafenib decreased the
level of C-RAF in the A549 cells and of B-RAF in the H1666 and
H1975 cells. These results are similar to those in a previous study
which reported that sorafenib inhibits NSCLC cell growth by
targeting B-RAF in KRAS wild-type cells and C-RAF in KRAS mutant
cells. However, this previous study demonstrated that sorafenib
failed to inhibit p-ERK in NSCLC cell lines with KRAS mutations
(23). The different results may be
attributed to a shorter time of exposure to sorafenib.
When sorafenib was combined with gemcitabine, a
significant decrease in p-AKT, p-ERK and Bcl-2 levels was observed
in the A549 and H1666 cells, as compared with the control. We
conclude that the RAF/MEK/ERK signaling pathways activated by
gemcitabine may be blocked by sorafenib in KRAS or BRAF mutant
cells. This may be due to sorafenib inhibiting mutant RAS and RAF
kinases and directly blocking the RAF/MEK/ERK pathway. However, the
levels of p-AKT and p-ERK increased when sorafenib and gemcitabine
were applied together to the H1975 cells, demonstrating that the
downstream pathway activated by gemcitabine was not blocked by
sorafenib in cells harboring a EGFR-T790M mutation. These
observations of p-AKT, p-ERK and Bcl-2 in NSCLC cells may explain
the synergistic or antagonist growth inhibitory effects observed in
the three cell lines treated with sorafenib and gemcitabine.
In conclusion, we found that sorafenib exhibited
significant growth inhibitory effects in EGFR-TKI-resistant NSCLC
cells. Regardless of the mutation status of KRAS, BRAF or EGFR
T790M, sorafenib was a treatment of choice against NSCLC. Moreover,
sorafenib combined with gemcitabine generated synergistic effects
in KRAS or BRAF mutant cells, and antagonistic effects in
EGFR-T790M mutant cells. These data encourage the development of
sorafenib as a single targeted therapy or in combination with
cytotoxic chemotherapy drugs for treatment of NSCLC.
Acknowledgements
This study was supported by a grant
from the Anhui Provincial Science and Technology Agency Foundation
of China (No. 09020303042) and supported by The Central Laboratory
of The Third Affiliated Hospital of Anhui Medical University.
References
|
1
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar
|
|
2
|
Pao W, Wang TY, Riely GJ, et al: KRAS
mutations and primary resistance of lung adenocarcinomas to
gefitinib or erlotinib. PLoS Med. 2:e172005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
McCubrey JA, Steelman LS, Chappell WH, et
al: Roles of the Raf/MEK/ERK pathway in cell growth, malignant
transformation and drug resistance. Biochim Biophys Acta.
1773:1263–1284. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gazdar AF: Activating and resistance
mutations of EGFR in non-small-cell lung cancer: role in clinical
response to EGFR tyrosine kinase inhibitors. Oncogene. 28(Suppl 1):
S24–S31. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Adjei AA: K-ras as a Target for Lung
Cancer Therapy. J Thorac Oncol. 3(Suppl 2): S160–S163. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ladanyi M and Pao W: Lung adenocarcinoma:
guiding EGFR-targeted therapy and beyond. Mod Pathol. 21:S16–S22.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wilhelm SM, Carter C, Tang L, et al: BAY
43-9006 exhibits broad spectrum oral antitumor activity and targets
the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in
tumor progression and angiogenesis. Cancer Res. 64:7099–7109. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Carter CA, Chen C, Brink C, et al:
Sorafenib is efficacious and tolerated in combination with
cytotoxic or cytostatic agents in preclinical models of human
non-small cell lung carcinoma. Cancer Chemother Pharmacol.
59:183–195. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dal Lago L, D’Hondt V and Awada A:
Selected combination therapy with sorafenib: a review of clinical
data and perspectives in advanced solid tumors. Oncologist.
13:845–858. 2008.PubMed/NCBI
|
|
10
|
Blumenschein GR Jr, Gatzemeier U, Fossella
F, et al: Phase II, multicenter, uncontrolled trial of single-agent
sorafenib in patients with relapsed or refractory, advanced
non-small-cell lung cancer. J Clin Oncol. 27:4274–4280. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dy GK, Hillman SL, Rowland KM Jr, et al: A
front-line window of opportunity phase 2 study of sorafenib in
patients with advanced nonsmall cell lung cancer: North Central
Cancer Treatment Group Study N0326. Cancer. 116:5686–5693. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dougherty DW and Friedberg JW: Gemcitabine
and other new cytotoxic drugs: will any find their way into primary
therapy? Curr Hematol Malig Rep. 5:148–156. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chou TC and Talalay P: Quantitative
analysis of dose-effect relationships: the combined effects of
multiple drugs or enzyme inhibitors. Adv Enzyme Regul. 22:27–55.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Strumberg D, Clark JW, Awada A, et al:
Safety, pharmacokinetics, and preliminary antitumor activity of
sorafenib: a review of four phase I trials in patients with
advanced refractory solid tumors. Oncologist. 12:426–437. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mok TS, Wu YL, Thongprasert S, et al:
Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N
Engl J Med. 361:947–957. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Maemondo M, Inoue A, Kobayashi K, et al:
Gefitinib or chemotherapy for non-small-cell lung cancer with
mutated EGFR. N Engl J Med. 362:2380–2388. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Masago K, Fujita S, Togashi Y, et al:
Clinicopathologic factors affecting the progression-free survival
of patients with advanced non-small-cell lung cancer after
gefitinib therapy. Clin Lung Cancer. 12:56–61. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Petrelli A and Giordano S: From single- to
multi-target drugs in cancer therapy: when aspecificity becomes an
advantage. Curr Med Chem. 15:422–432. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Linardou H, Dahabreh IJ, Kanaloupiti D, et
al: Assessment of somatic K-Ras mutations as a mechanism associated
with resistance to EGFR-targeted agents: a systematic review and
meta-analysis of studies in advanced non-small cell lung cancer and
colorectal cancer. Lancet Oncol. 9:962–972. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lopez-Chavez A, Carter CA and Giaccone G:
The role of KRAS mutations in resistance to EGFR inhibition in the
treatment of cancer. Curr Opin Investig Drugs. 10:1305–1314.
2009.PubMed/NCBI
|
|
21
|
Kotoula V, Sozopoulos E, Litsiou H, et al:
Mutational analysis of the BRAF, RAS and EGFR genes in human
adrenocortical carcinomas. Endocr Relat Cancer. 16:565–572. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Torres K and Horwitz SB: Mechanisms of
taxol-induced cell death are concentration dependent. Cancer Res.
58:3620–3626. 1998.PubMed/NCBI
|
|
23
|
Takezawa K, Okamoto I, Yonesaka K,
Hatashita E, Yamada Y, Fukuoka M and Nakagawa K: Sorafenib inhibits
non-small cell lung cancer cell growth by targeting B-RAF in KRAS
wild-type cells and C-RAF in KRAS mutant cells. Cancer Res.
69:6515–6521. 2009. View Article : Google Scholar : PubMed/NCBI
|