Introduction
A DSRCT is an aggressively malignant tumor that
predominantly occurs in adolescents and young adults. The condition
was first described by Gerald and Rosai in 1989 (1) and usually arises in the abdominal area
and/or the pelvic peritoneum, presenting with a diffuse peritoneal
extension. Extra-abdominal DSRCTs, particularly those arising in
the testis are rare. To the best of our knowledge, only one study
has been published with regard to a DSRCT of the paratesticular
region (2). The present study
describes an unusual case of DSRCT in a Chinese patient, and may be
the first primary DSRCT of the testes to be reported in the English
literature.
Case report
A 27-year-old male presented with gradual swelling
and intermittent testicular pain that had lasted for approximately
four months. There was no specific infection or a history of
trauma. The patient was initially diagnosed with epididymitis in a
clinic and treated with antibiotics for two weeks. However, no
significant improvement in the condition was observed. A physical
examination revealed a solid mass located in the right scrotum,
with no tenderness. Laboratory studies did not reveal any
abnormalities. A mass measuring ∼5×6 cm (Fig. 1) was identified in the right testis
using ultrasound sonography. A computed tomography (CT) scan
revealed a solitary mass of high intensity in the right testis,
with a regional extension to the epididymis. A low-density area was
identified inside the mass (Fig.
2). There was no evidence of metastasis to the local or distant
organs. The patient provided written informed consent.
The patient was diagnosed with a malignant tumor and
a radical orchectomy was performed. The post-operative course was
smooth. A formalin-fixed, paraffin-embedded tissue section was
obtained for a routine microscopic examination. The specimen was
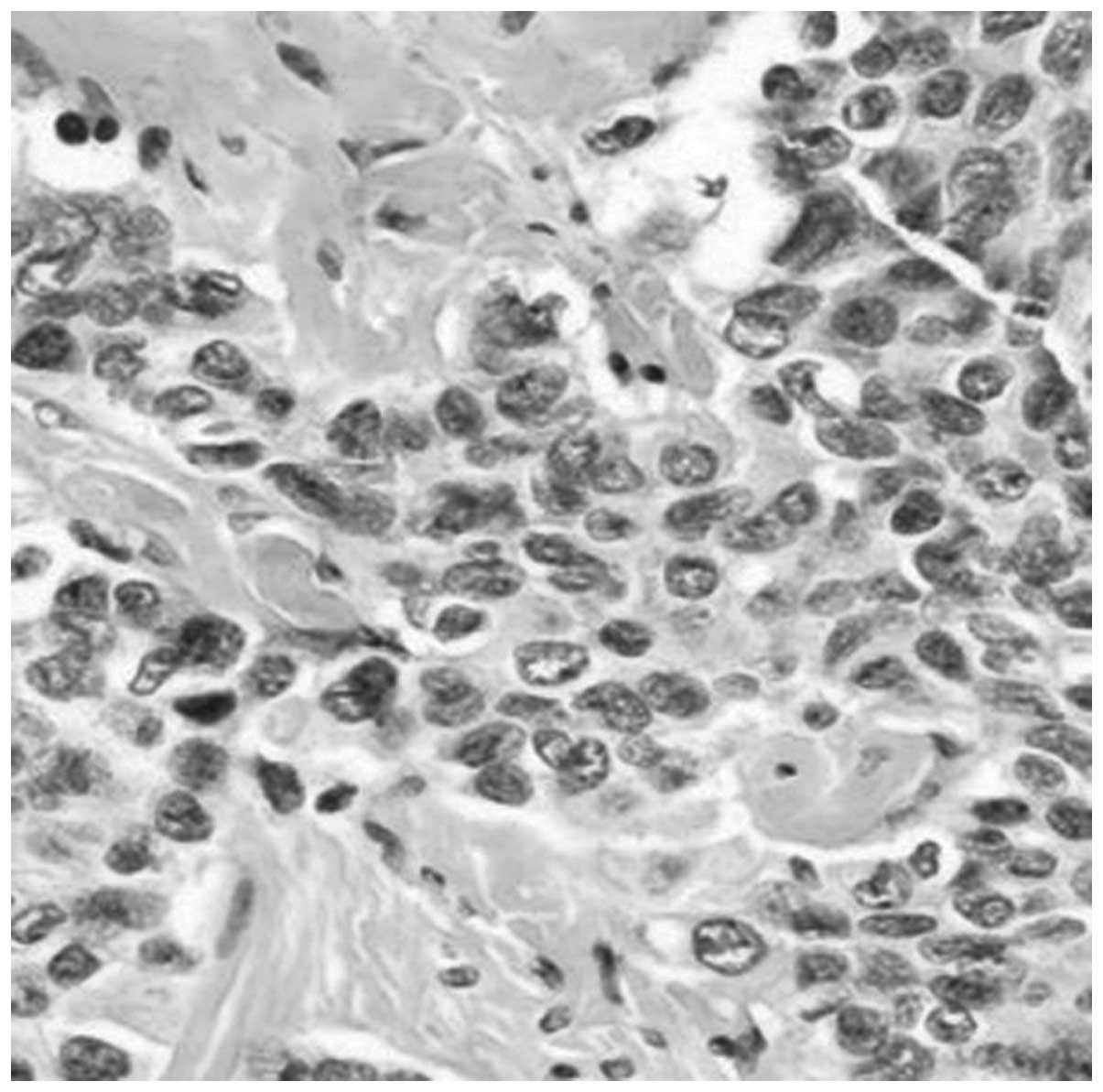
stained with hematoxylin and eosin. Microscopically, the tumors
consisted of nests of ‘small cells’, with scant cytoplasm embedded
in a densely fibrotic stroma and focal tubule formation. Numerous
mitotic figures were observed within the tissues. Certain figures
were arranged in well-defined cell nests, which were delimited by a
cellular desmoplastic stroma (Figs.
3 and 4). Immunohistochemical
staining was performed using the streptavidin-biotin peroxidase
method. Immunohistochemically, the tumor cells were positive for
smooth muscle actin (SMA), vimentin, CD99 and neuron-specific
enolase (NSE). However, the cells were non-reactive for Human
Melanoma Black-45 (HMB45) and cytokeratin (CK). The histological
and immunohistochemical findings supported the diagnosis of a
desmoplastic small round cell tumor (DSRCT). The patient was
administered treatment consisting of a multi-agent systemic
chemotherapy regimen every three weeks in four cycles with 1.4
mg/m2 vincristine on the first day, 60 mg/m2
doxorubicin on the second day and 2 g/m2 ifosfamide for
five days. The patient appeared to be disease-free at 14 months. No
evidence of recurrence was identified on the clinical or imaging
examinations during the 14-month follow-up period. However, the
patient succumbed to multi-organ metastases 12 months later.
Discussion
DSRCT is a rare and aggressive, malignant tumor. The
disease most commonly presents with a multinodular growth on the
serosal surfaces, including the peritoneum (3) and the pleura. DSRCT of the abdominal
cavity has also been frequently documented. Extra-abdominal DSCRTs,
particularly those arising in the genital system, are rare. Only
one abdominal DSRCT with scrotal metastases has been previously
reported and sporadic cases have occurred in the paratesticular
region (4,5). The present study provides the first
case of DSRCT arising in the testis to be reported in the English
literature.
Morphologically, DSRCT is characterized by nests of
mitotically active, small, round, blue cells that are proliferating
in a cellular fibrous stroma. Immunoreactivity indicates a
blastomatous cell of origin with a polyphenotypic appearance. The
immunohistochemical characteristics of DSRCT exhibit the typical
immunophenotype, consisting of positivity for keratin, vimentin,
desmin and NSE. The differential diagnosis of DSRCT is fairly broad
and includes tumors such as Ewing sarcoma, neuroblastoma, Wilms
tumor, rhabdomyosarcoma, small cell carcinoma and lymphoma. A
definite diagnosis may only be achieved with a demonstrated
multidirectional differentiation and coexpression of epithelial,
mesenchymal and neural antigens in the same cell (6). The presence of perinuclear dot-like
immunostaining with desmin strongly suggests a diagnosis of DSRCT
(7).
Clinically, laboratory test results are
non-contributory. Several studies have described DSRCT with
elevated serum CA 125 and lactic dehydrogenase levels in certain
cases (8,9). These may be useful markers for DSRCT
and may allow a clinician to monitor the progress of the
treatment.
A DSRCT is characterized by a growth on the serosal
surface. Certain studies have described an extra-abdominal location
as the primary site of the tumor (10). To the best of our knowledge, the
extra-abdominal testicular location of the tumor of the current
case has not been previously reported. The most frequent presenting
complaint for DSRCT is a painless mass and metastasis. This
suggests that DSRCT should be included in the differential
diagnosis of other testicular germ cell cancers.
The most common CT feature that has been reported
for DSRCT is the synchronous presence of multiple abdominal masses
and scrotal nodules without a clear organ of origin (5). Large homogeneous soft-tissue masses
that nearly fill the entire peritoneal space have been identified.
DSRCT should be suspected in young males that present with multiple
bulky heterogeneous soft-tissue masses (11,12). A
differential diagnosis of DSRCT arising in the testis is difficult
to distinguish from other germ cell carcinomas according to the
imaging features.
Despite aggressive treatment, the survival rate of
patients with DSRCT remains poor. The optimum treatment remains to
be determined. According to a literature review and our experience,
a surgical resection, followed by aggressive chemotherapy is
recommended as a treatment for DSRCT. Aggressive multimodality
therapies with immunotherapy or bone marrow ablation, and
dose-intensive chemotherapy with autologous peripheral blood stem
cell support, may provide potential benefits for patients with
DSRCT and be promising new treatment approaches (13). The survival rate may be improved
using high-dose multi-drug combination chemotherapy followed by an
aggressive surgical resection, radiotherapy and myeloablative
chemotherapy with stem cell rescue (14).
In conclusion, primary DSRCTs of the testis are
rare. In the present case, there were no specific characteristics
in the clinical symptoms or the imaging studies, which resulted in
a difficulty in diagnosing DSRCT. To date, no standard treatment
has been established and the prognosis of affected patients is
poor. Further investigation is required to identify the optimum
treatment approach.
References
|
1.
|
Gerald WL and Rosai J: Case 2.
Desmoplastic small cell tumor with divergent differentiation.
Pediatr Pathol. 9:177–183. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Cummings OW, Ulbright TM, Young RH, Dei
Tos AP, Fletcher CD and Hull MT: Desmoplastic small round cell
tumors of the paratesticular region. A report of six cases Am J
Surg Pathol. 21:219–225. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Choi JK, van Hoeven K, Brooks JJ and Gupta
PK: Desmoplastic small round cell tumor presenting in pleural fluid
and accompanied by desmin-positive mesothelial cells. Acta Cytol.
39:377–378. 1995.PubMed/NCBI
|
|
4.
|
Roganovich J, Bisogno G, Cecchetto G, et
al: Paratesticular desmoplastic small round cell tumor: case report
and review of the literature. J Surg Oncol. 71:269–272. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Takhtani D, Saleeb SF and Teplick SK:
General case of the day. Desmoplastic small round cell tumor of the
abdomen with scrotal metastases. Radiographics. 19:252–254.
1999.PubMed/NCBI
|
|
6.
|
Chang F: Desmoplastic small round cell
tumors: cytologic, histologic, and immunohistochemical features.
Arch Pathol Lab Med. 130:728–732. 2006.PubMed/NCBI
|
|
7.
|
Ordóñez NG: Desmoplastic small round cell
tumor: I: a histopathologic study of 39 cases with emphasis on
unusual histological patterns. Am J Surg Pathol. 22:1303–1313.
1998.PubMed/NCBI
|
|
8.
|
Yoshizawa J, Maie M, Eto T, et al: A case
of intra-abdominal desmoplastic small-round-cell tumor with
elevated serum CA125. Pediatr Surg Int. 18:238–240. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Kretschmar CS, Colbach C, Bhan I and
Crombleholme M: Desmoplastic small cell tumor: a report of three
cases and a review of the literature. J Pediatr Hematol Oncol.
18:293–298. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Gerald WL, Miller HK, Battifora H, et al:
Intra-abdominal desmoplastic small round-cell tumor: Report of 19
cases of a distinctive type of high-grade polyphenotypic malignancy
affecting young individuals. Am J Surg Pathol. 15:499–513. 1991.
View Article : Google Scholar
|
|
11.
|
Bellah R, Suzuki-Bordalo L, Brecher E, et
al: Desmoplastic small round cell tumor in the abdomen and pelvis:
report of CT findings in 11 affected children and young adults. AJR
Am J Roentgenol. 184:1910–1914. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Tateishi U, Hasegawa T, Kusumoto M, et al:
Desmoplastic small round cell tumor: imaging findings associated
with clinicopathologic features. J Comput Assist Tomogr.
26:579–583. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Mazuryk M, Paterson AH, Temple W, et al:
Benefit of aggressive multimodality therapy with autologous stem
cell support for intra-abdominal desmoplastic small round cell
tumor. Bone Marrow Transplant. 21:961–963. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Quaglia MP and Brennan MF: The clinical
approach to desmoplastic small round cell tumor. Surg Oncol.
9:77–81. 2000. View Article : Google Scholar : PubMed/NCBI
|