Introduction
Nasal-type extranodal natural killer/T-cell lymphoma
(NKTL) is a rare type of lymphoma, which is associated with the
Epstein-Barr virus (EBV). NKTL has also been referred to as lethal
midline granuloma and polymorphic reticulosis. When NKTL occurs
outside the nasal cavity, such as in the skin, soft tissue,
gastrointestinal tract and other extranasal sites, it may have
various presentations (1–7). As a result of advances in
immunohistochemistry, the disease can now be more easily
identified. The current study presents a case of a 23-year-old male
with CD30+ nasal-type extranodal NKTL, with skeletal
muscle involvement mimicking phlegmonous myositis and fever of
undetermined origin (FUO). In addition, the diagnosis of extranodal
NKTL and FUO is discussed. The patient provided written informed
consent.
Case report
Patient history
In August 2011, a 23-year-old male presented with
swelling, tenderness and high skin temperature of the left lower
limb, particularly around the ankle as the patient did not have a
fever the patient did not seek treatment. However, one month later,
pharyngalgia and fever developed and the patient was treated with
antibiotics for the inflammation at a local health center, however,
the symptoms were not improved. The patient was subsequently
transferred to the Chengdu First People’s Hospital (Chengdu, China)
for hospitalization.
Laboratory tests
The laboratory tests (9 Aug, 2011) showed
leukopenia, with a white blood cell (WBC) count of
1.45×109/l and 0% eosinophils. The serum biochemistry
revealed alanine aminotransferase (ALT) levels of 114 IU/l (normal
range, <55 IU/l), aspartate transaminase (AST) levels of 83 IU/l
(normal range, <46 IU/l), lactate dehydrogenase (LDH) levels of
479 IU/l (normal range, 110–220 IU/l) and creatine phosphokinase
levels of 736 IU/l (normal range, 25–190 IU/l). B type ultrasound
(9 Aug, 2011) showed splenomegaly and swelling of the soft tissue
in the left lower limb, with reduced blood flow and a small mass in
the vein. The bone marrow biopsy was normal. A complete blood count
(CBC) was performed (12 Aug, 2011) and showed a WBC count of
10.79×109/l (84.6% neutrophils).
Treatment and further testing
Multiple antibiotics were administered continuously,
however, the patient showed no clinical response. During
hospitalization, the patient’s condition deteriorated, with the
highest temperature reaching 40.4°C and weight loss of 5 kg over
two months. The patient was referred to the Infection Disease
Center (West China Hospital, Chengdu, China) due to FUO. On
physical examination, purulent secretion was found in the patient’s
nose and the spleen was palpable 5 cm below the costal margin. The
laboratory tests (22 Aug, 2011) showed a WBC count of
1.57×109/l (36.5% neutrophils), platelet count of
71×109/l, ALT levels of 184 IU/l, AST levels of 197
IU/l, LDH levels of 554 IU/l and γ-glutamyltransferase levels of
432 IU/l.
Computed tomography, magnetic resonance
imaging and biopsy
A computed tomography scan of the laryngopharynx
identified inflammatory changes, particularly in the left
nasopharynx and the soft palate, as well as hyperplasia of the
submandibular lymph nodes. Magnetic resonance imaging of the lower
extremity detected a diffuse infiltrative lesion, mimicking
phlegmonous myositis (Fig. 1). A
bone marrow biopsy was performed again and showed a depression with
normal morphology. Prominent ulceration and necrosis with fungal
elements (usually oidiomycetic) were observed in the soft palate by
pharyngoscopy. Taking into consideration the fever, ulceration in
the nasopharynx, splenomegaly, weight loss and cachexy, the
diagnosis of extranodal NKTL was determined. In addition, the
muscle biopsy of the left limb and repeat biopsy of the pharynx was
of concern. Diffuse infiltration of medium-sized atypical lymphoid
cells with irregular nuclei was shown in the gastrocnemius
biopsy.
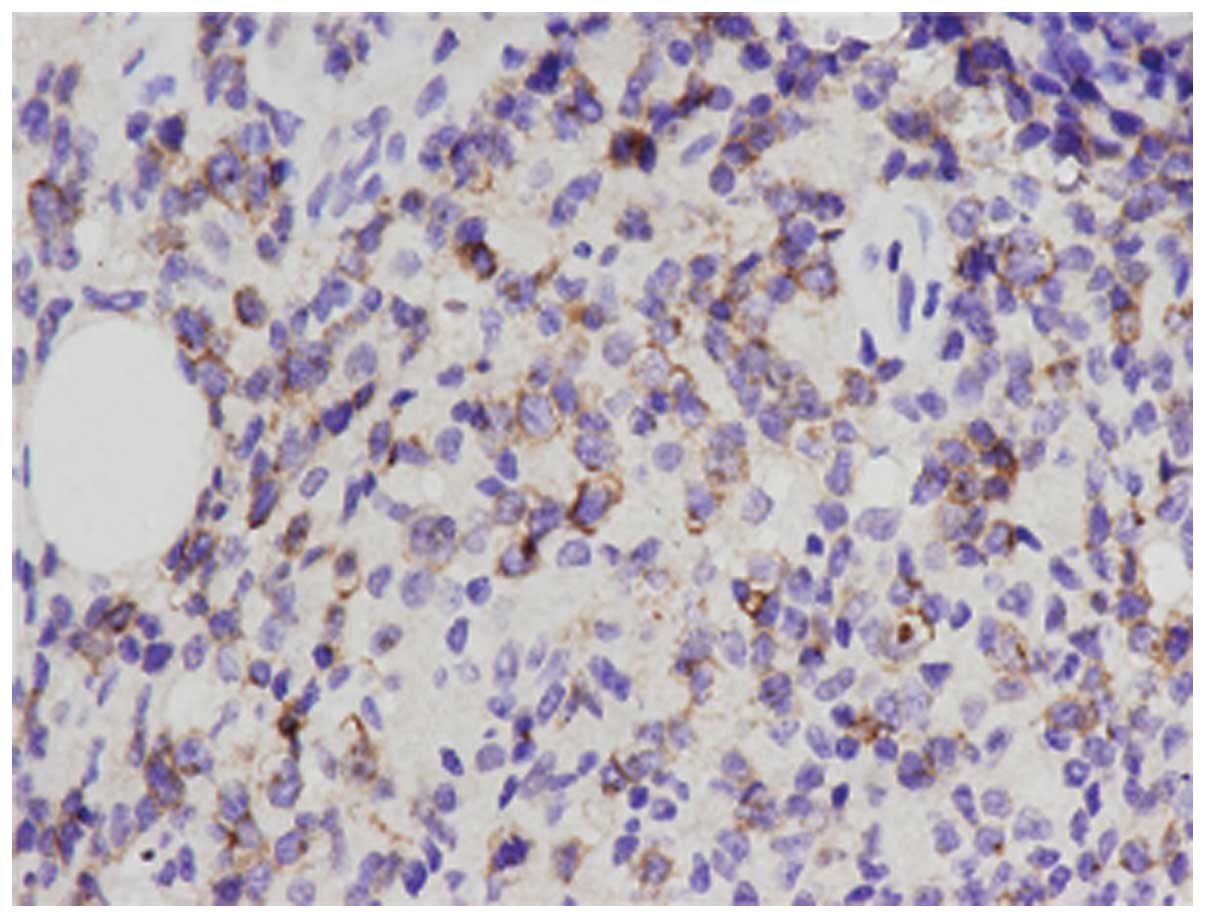
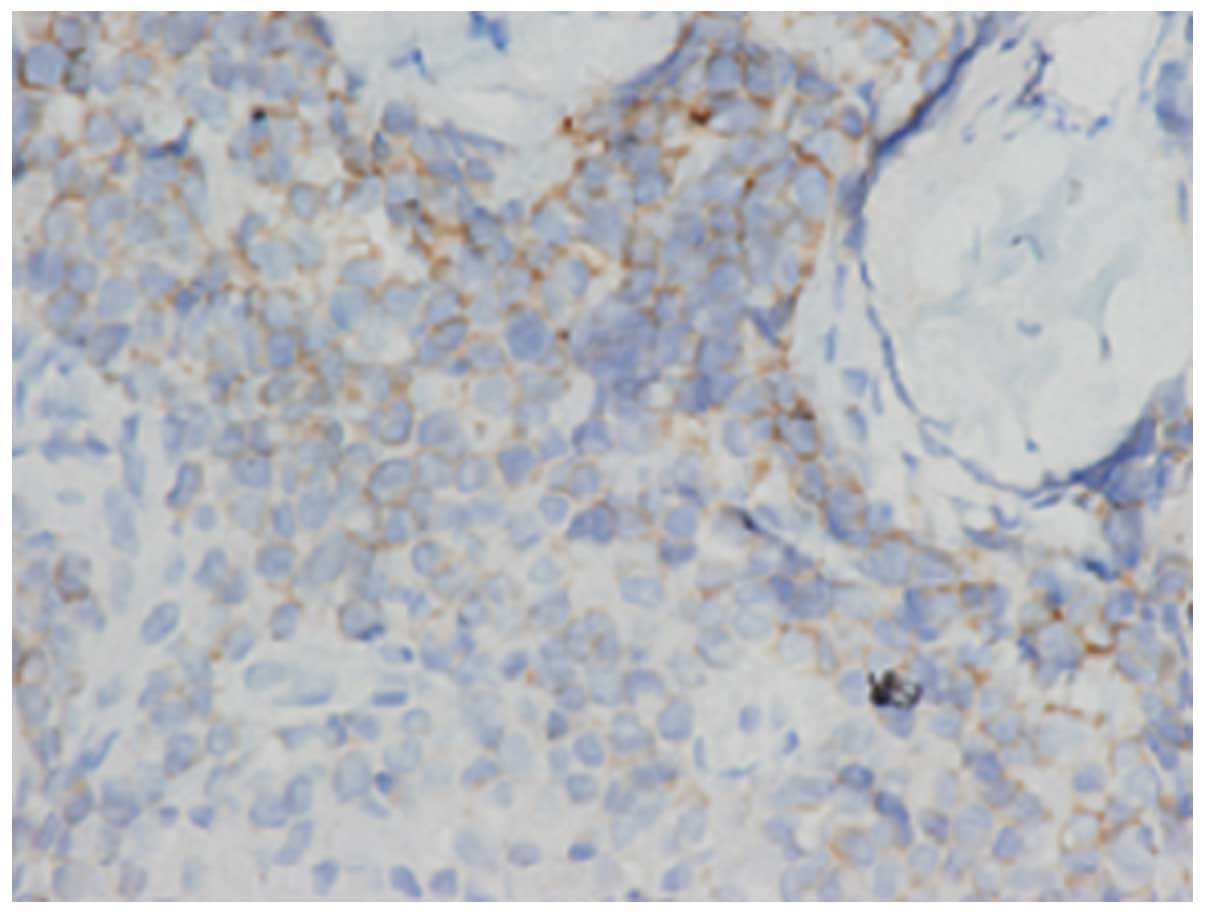
Immunohistochemical analysis
Immunohistochemical staining
[avidin-biotin-peroxidase and elivision methods (8)] was performed on the paraffin-embedded
sections using the following commercial antibodies: rabbit
monoclonal anti-CD3 (SP7, 1:50; LabVision-NeoMarkers, Fremont, CA,
USA), polyclonal rabbit anti human CD3ɛ (1:50; Dakopatts, Glostrup,
Denmark), monoclonal mouse anti-CD20 (L26, 1:100; Zymed, South San
Francisco, CA, USA), monoclonal mouse anti-CD30 (Ber-H2, 1:50;
LabVision-NeoMarkers), monoclonal mouse anti-CD45RO (UCHL1, 1:100;
Zymed), monoclonal mouse anti-CD56 (123C3, 1:100; Zymed),
monoclonal mouse anti-GranzymeB (GZB01, 1:100;
LabVision-NeoMarkers), polyclonal rabbit anti-Ki67 (MIB-1, 1:100;
LabVision- NeoMarkers), monoclonal mouse anti-human ALK1 (ALK1,
1:100; Dako, Carpinteria, CA, USA). In situ hybridization
for EBV to encode RNA (EBER1/2) was performed on fixed
paraffin-embedded sections. The fluorescein
isothiocynate-conjugated EBER peptide nucleic acid probe (Y5200)
was purchased from Dakopatts. The histochemical staining was
positive for CD45, CD30 (Fig. 2),
the majority of CD56 cells (Fig.
3), granzyme B and Ki-67, and negative for CD3ɛ, CD20 and
activin receptor-like kinase 1 (ALK1). The in situ
hybridization for EBV-encoded small RNA (EBER) was strongly
positive.
Follow-up
Based on the clinical manifestations and
pathological observations, a diagnosis of nasal-type extranodal
NKTL was determined and the patient was transferred to the
Department of Hematology (West China Hospital, Chengdu, China) for
chemotherapy with GL-IDE: Gemcitabine (1.6 g on days 1 and 8);
L-asparaginase (10,000 U/m2 on days 4, 6, 8 and 10);
Ifosfamide (1.6 g on days 1, 2 and 3); Dexamethasone (20 mg on days
1, 2, 3 and 4); Etoposide (160 mg on days 1, 2 and 3). The patient
succumbed as a result of the rapid progression of the disease two
months later.
Discussion
Nasal-type extranodal NKTL has also been referred to
as lethal midline granuloma or polymorphic reticulosis and may have
variable presentations depending on the predominant site of
involvement. To date, only sporadic cases concerning skin, muscle
and ocular involvement have previously been reported (1–4). Min
et al (5) reported a case of
extranodal NKTL with muscle involvement that initially manifested
with granulomatous myositis, with a normal CBC count and without
fever. In addition, Paik et al (6) reported a case of extranodal NKTL with
skeletal muscle involvement and heavy eosinophilic infiltration,
with a peripheral blood eosinophilia of 22.2% on CBC count.
However, the current patient presented with swelling, tenderness
and a high skin temperature of the left lower limb, followed by
hyperpyrexia. The patient’s WBC count reached
10.79×109/l (84.6% neutrophils and 0% eosinophils),
which mimicked phlegmonous myositis. The present case illustrated
the requirement for caution when diagnosing NKTL as it may be a
rare cause of unexplained phlegmonous myositis, particularly when
accompanied with FUO and symptoms in the nasopharynx.
Extranodal NKTL is characterized by vascular damage,
prominent necrosis and is associated with the EBV (7,9–11). The
typical immunophenotype for extranodal NKTL is CD2+,
CD56+, surface CD3− and cytoplasmic
CD3ɛ+, as well as positivity for cytotoxic molecules
(granzyme B, T-cell intracellular antigen 1 and perforin) (13–15).
As observed in the present case, early biopsy may give a false
indication of an inflammatory disorder due to the paucity of
neoplastic cells; however, in NKTL, a large number of inflammatory
cells are recruited by the innate natural killer cell immune
response and extensive necrosis is caused by angiodestructive tumor
cells. However, in the present study, the repeat biopsy (which
showed atypical lymphoid cells positive for granzyme B, EBER, CD45
and CD56, and negative for CD20 and ALK1) showed features that were
consistent with NKTL. This emphasized the requirement for a repeat
biopsy when NKTL is suspected, as necrosis is often present in
biopsy. The biological meaning for the positivity of CD30 is not
clearly understood. As CD30 is normally associated with anaplastic
large cell lymphoma, the positivity for CD30 has been reported in
few cases of cutaneous NKTL. The present case showed that
extranodal NKTL must be considered as a differential diagnosis of
CD30+ and CD56+ lymphoma.
In conclusion, in patients who exhibit FUO,
infectious diseases, malignancies, collagen vascular diseases and a
variety of miscellaneous disorders must be considered. The cause of
FUO is partially age-related and neoplastic disorders have replaced
infectious diseases as the most common cause of FUO; non-Hodgkin’s
lymphoma is the first cause of FUO that has been linked to cancer
(16,17). Although neoplastic disorders are
more commonly observed in elderly patients, the present patient was
23-years-old, which is relatively different from the median age (50
years) of those with NKTL, indicating that NKTL is occasionally
found in younger patients.
References
|
1
|
Cimino L, Chan CC, Shen D, Masini L,
Ilariucci F, Masetti M, et al: Ocular involvement in nasal natural
killer T-cell lymphoma. Int Ophthalmol. 29:275–279. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen CS, Miller NR, Lane A and Eberhart C:
Third cranial nerve palsy caused by intracranial extension of a
sino-orbital natural killer T-cell lymphoma. J Neuroophthalmol.
28:31–35. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yousuf SJ, Kumar N, Kidwell ED Jr and
Copeland RA Jr: Rapidly fatal nasal natural killer/T-cell lymphoma:
orbital and ocular adnexal presentations. Orbit. 30:120–121. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Stokkermans-Dubois J, Jouary T, Vergier B,
Delaunay MM and Taieb A: A case of primary cutaneous nasal type
NK/T-cell lymphoma and review of the literature. Dermatology.
213:345–349. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Min HS, Hyun CL, Paik JH, Jeon YK, Choi G,
Park SH, et al: An autopsy case of aggressive CD30+
extra-nodal NK/T-cell lymphoma initially manifested with
granulomatous myositis. Leuk Lymphoma. 47:347–352. 2006.PubMed/NCBI
|
|
6
|
Paik JH, Jeon YK, Go HJ and Kim CW:
Extranodal NK/T cell lymphoma accompanied by heavy eosinophilic
infiltration and peripheral blood eosinophilia, involving skeletal
muscles. Korean J Pathol. 45(Suppl 1): S70–S74. 2011. View Article : Google Scholar
|
|
7
|
Wood PB, Parikh SR and Krause JR:
Extranodal NK/T-cell lymphoma, nasal type. Proc (Bayl Univ Med
Cent). 24:251–254. 2011.PubMed/NCBI
|
|
8
|
He Q, Xu H, Shao MM and Yu XW: Evaluation
of rapid immunohistochemical staining technique in intraoperative
frozen section diagnosis of breast tumors. Chinese J Clin Exp
Pathol. 23:553–556. 2007.
|
|
9
|
Salinas F, Mulero F, Marin M, Padilla A
and Fernandez I: Fever of unknown origin (FUO), scintigraphy with
Gallium 67 citrate scintigraphy and malignant lymphoma of soft
tissues. Rev Esp Med Nucl. 23:427–428. 2004.(In Spanish).
|
|
10
|
Li YX, Fang H, Liu QF, Lu J, Qi SN, Wang
H, et al: Clinical features and treatment outcome of nasal-type
NK/T-cell lymphoma of Waldeyer ring. Blood. 112:3057–3064. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li YX, Liu QF, Fang H, Qi SN, Wang H, Wang
WH, et al: Variable clinical presentations of nasal and Waldeyer
ring natural killer/T-cell lymphoma. Clin Cancer Res. 15:2905–2912.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Qin W, Yin Z and Madge SN: Acute
presentation of nasal-type natural killer/T-cell lymphoma of the
orbit. Eur J Ophthalmol. 19:679–682. 2009.PubMed/NCBI
|
|
13
|
Yang Y, Luo Q, He W and Tang L: Primary
ocular natural killer/T-cell lymphomas: clinicopathologic features
and diagnosis. Ophthalmologica. 221:173–179. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Takahashi E, Ohshima K, Kimura H, Hara K,
Suzuki R, Kawa K, et al: Clinicopathological analysis of the
age-related differences in patients with Epstein-Barr virus
(EBV)-associated extranasal natural killer (NK)/T-cell lymphoma
with reference to the relationship with aggressive NK cell
leukaemia and chronic active EBV infection-associated
lymphoproliferative disorders. Histopathology. 59:660–671.
2011.
|
|
15
|
Kim JE, Kim YA, Jeon YK, Park SS, Heo DS
and Kim CW: Comparative analysis of NK/T-cell lymphoma and
peripheral T-cell lymphoma in Korea: Clinicopathological
correlations and analysis of EBV strain type and 30-bp deletion
variant LMP1. Pathol Int. 53:735–743. 2003. View Article : Google Scholar
|
|
16
|
Ferrari P, Schneemann M and Zimmerli L:
FUO: fever of unknown origin. Praxis (Bern 1994). 98:1253–1259.
2009.(In German).
|
|
17
|
Arce-Salinas CA, Morales-Velázquez JL,
Villaseñor-Ovies P and Muro-Cruz D: Classical fever of unknown
origin (FUO): current causes in Mexico. Rev Invest Clin.
57:762–769. 2005.PubMed/NCBI
|