Introduction
Solitary plasmacytomas (SPs) are rare and are
characterized by a localized accumulation of neoplastic monoclonal
plasma cells, without proof of systemic myelomatosis. The tumors
represent ≤5% of all plasma cell neoplasms (1) and mostly occur in the spine, pelvis,
ribs and pectoral girdle (1–3), while
rarely occurring in the sternum. Radiologically, SP of the bone
typically appears as an osteolytic lesion; the tumor usually
destroys the cortex in several places and invades the soft tissues
(2,4). In rare cases, the radiological
findings may take unusual forms, for example, they can manifest as
bony spicules on the surface of the bone, which resemble the
appearance of sunrays (5–12). The sites of bony spiculation in the
lesions previously described in the literature are the mandible,
orbit, vertebral body and skull vault (5–12).
The current study presents a case of a solitary
plasmacytoma of the sternum with a spiculated periosteal reaction
on radiological imaging. Written informed consent was obtained from
the patient.
Case report
A 74-year-old female presented with neck and
anterior chest wall pain, along with swelling in the chest area
that had persisted for one month. The past medical history
consisted of type II diabetes mellitus and hypertension. There was
no history of cancer. A physical examination revealed an
ill-defined swelling on the anterior chest wall. The area was
tender and no pulsation was noted. Routine urinalysis and
hematological and biochemical tests were within the normal limits.
A urine test for Bencae Jones protein was negative.
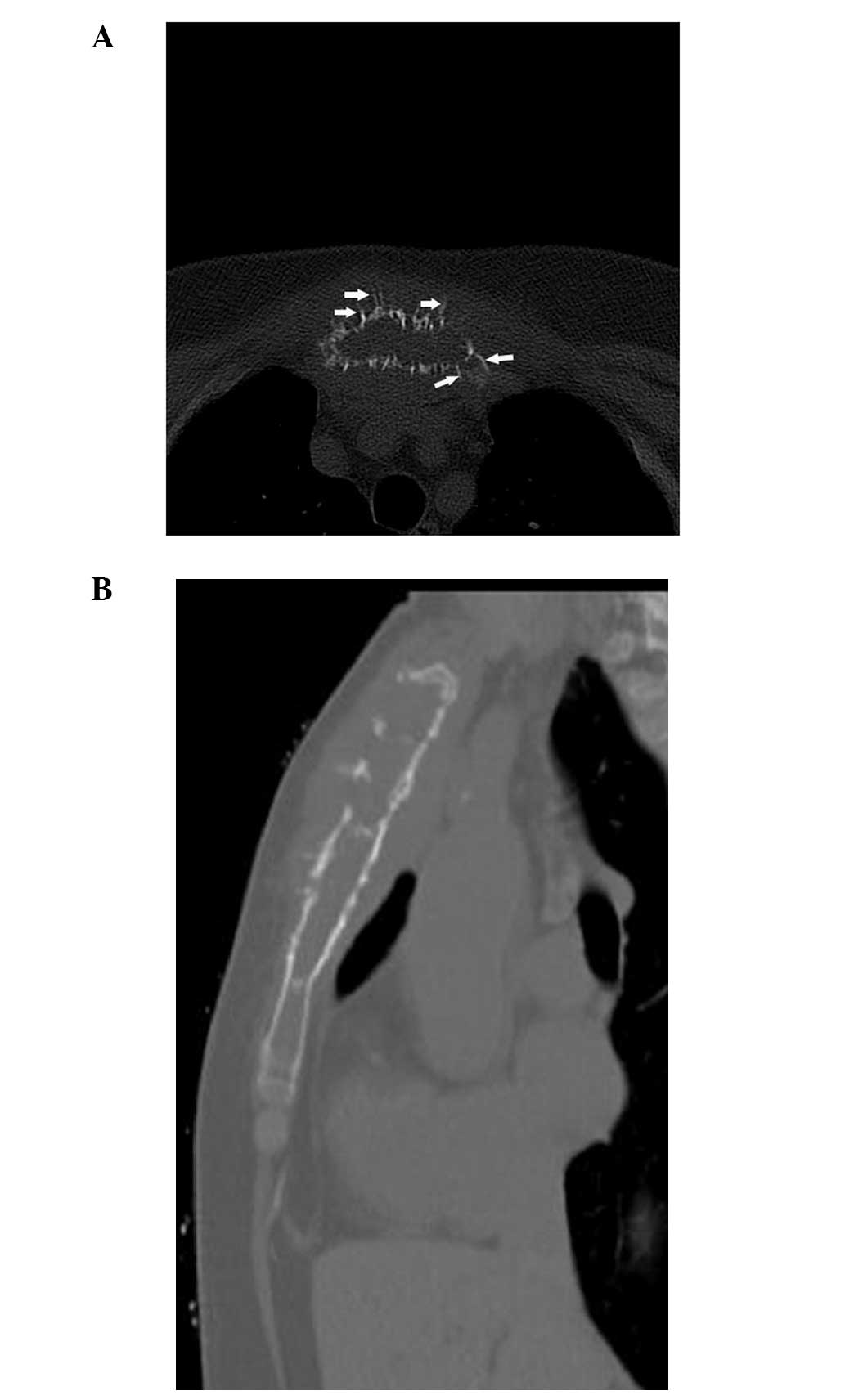
Conventional radiography of the chest was normal. On
the axial and sagittal computed tomography (CT) scans, the
manubrium and body of the sternum had extensive bony destruction,
with a large quantity of thick straight spicules on the surface of
the bone resembling a sunray in appearance. The lesion had slight
expansion and disruption of the cortex in certain places and had
spread to the adjacent soft tissues. There was no calcification in
the lesion (Fig. 1). The tumor
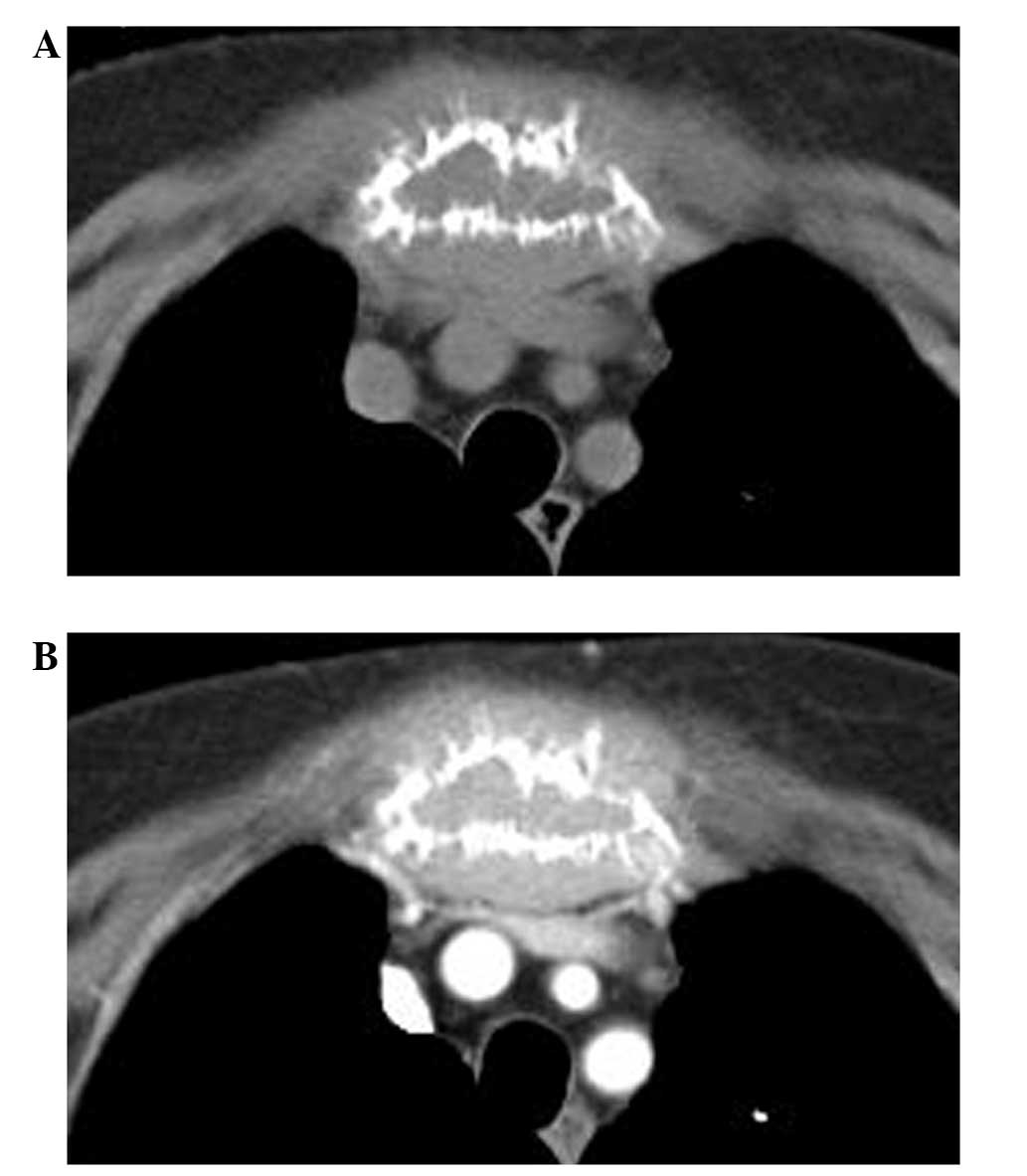
exhibited marked homogeneous enhancement on contrast-enhanced CT
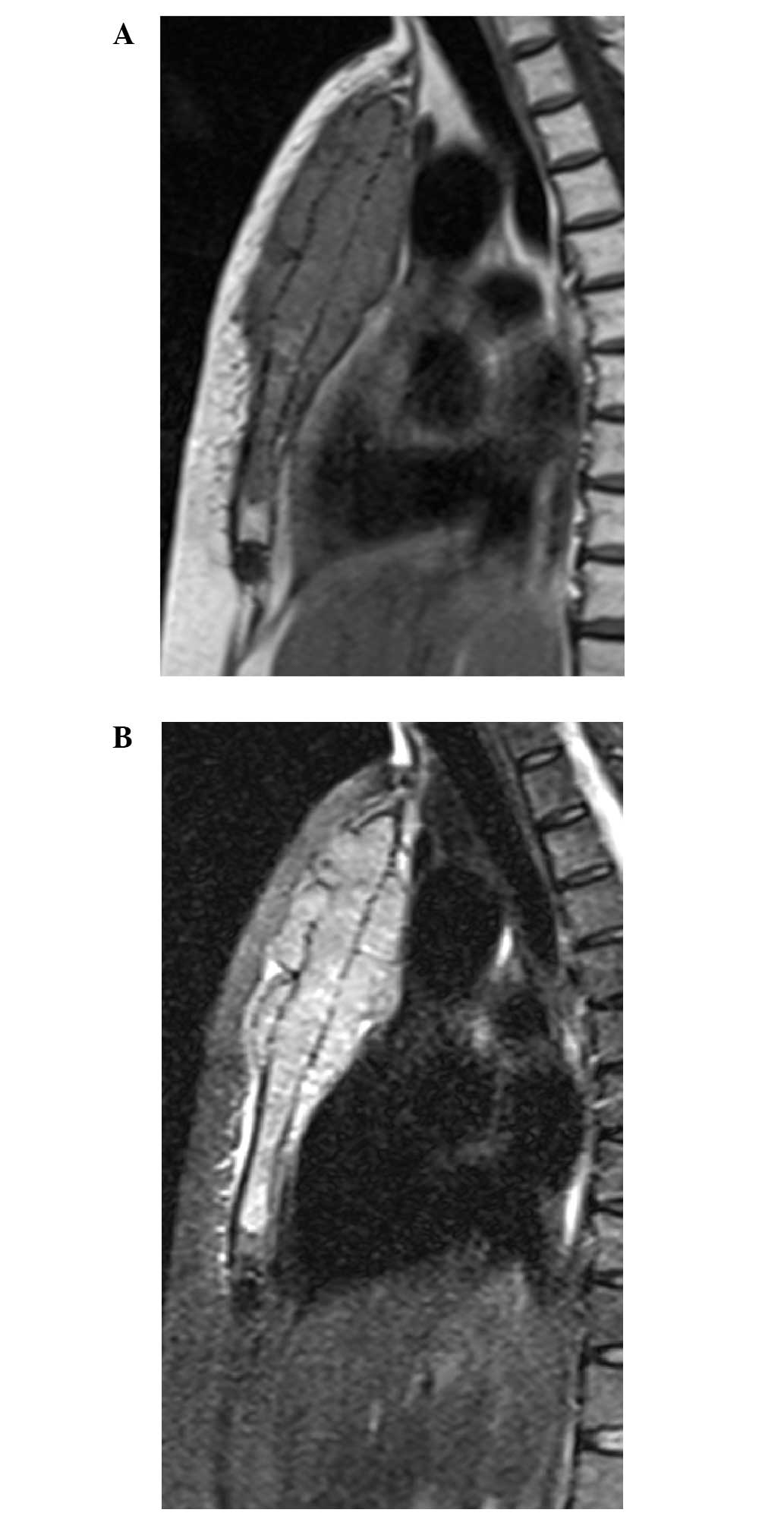
(Fig. 2). Magnetic resonance (MR)
imaging showed that the lesion displayed a homogeneous low signal
intensity on T1-weighted images, and a high signal intensity on
short-τ inversion recovery T2-weighted images. The soft-tissue mass
was clearly demonstrated (Fig. 3).
Use of 99mTc-labelled whole-body bone scintigraphy
disclosed normal results, with the exception of increased uptake in
the sternum.
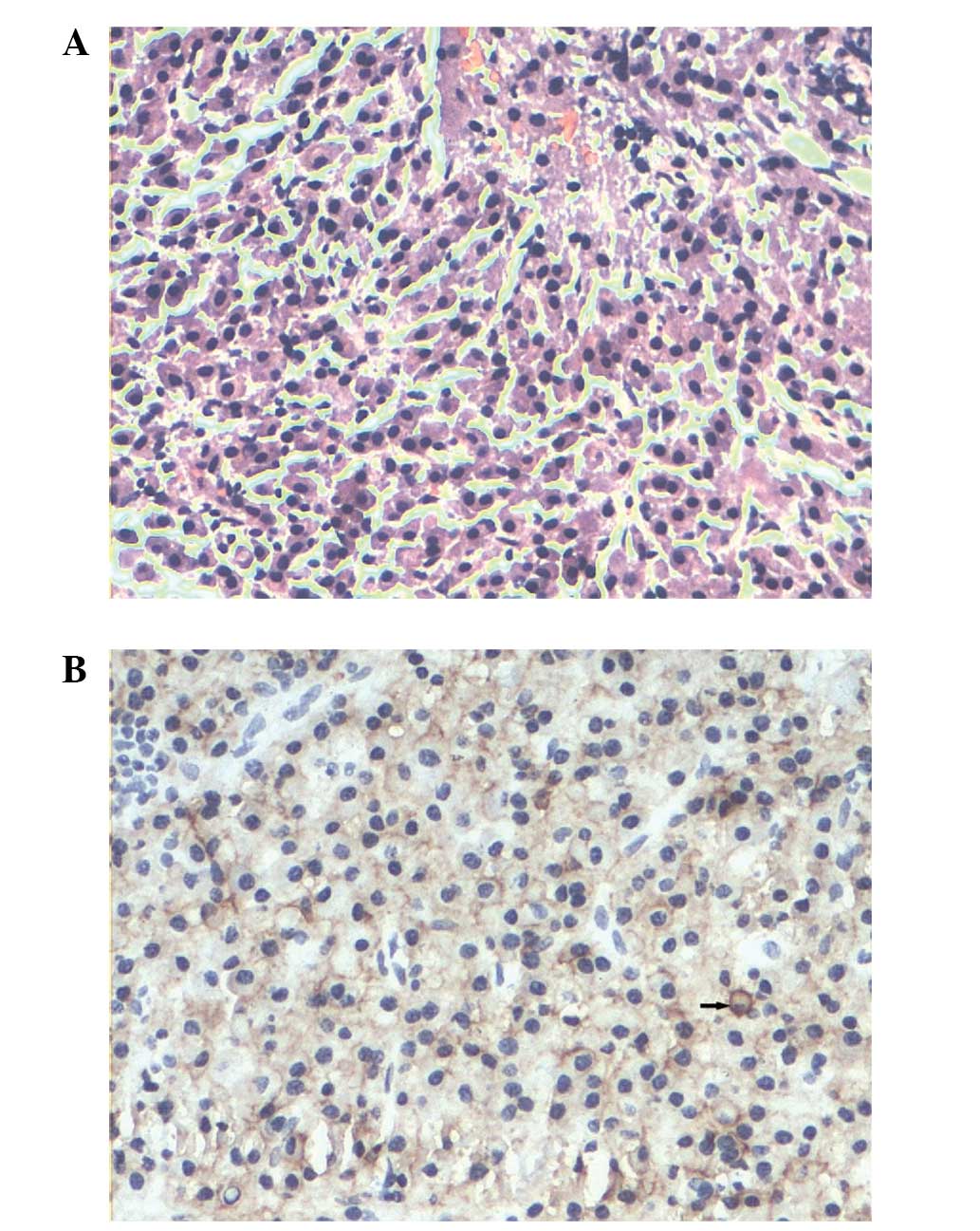
In order to obtain the correct diagnosis, an open
biopsy was performed at the sternum. The histopathological
examination demonstrated that the destroyed bone marrow had been
substituted with abundant neoplastic plasma cells with eccentric
‘clock-face’ nuclei and copious cytoplasm. Immunohistochemical
staining was positive for immunoglobulin (Ig) λ- and κ-light chain
antibodies, and cluster of differentiation (CD)38 and -138
(Fig. 4). The histological
diagnosis of the tumor was of a plasmacytoma. Immunoelectrophoresis
of the serum proteins revealed mild monoclonal gammopathy of IgA
(IgA λ-type). Iliac bone marrow aspiration revealed no evidence of
myeloma (<5% plasma cells). MR imaging of the cervical and
lumbar spine, a CT scan of the head and thorax, and a radiograph of
the pelvis revealed no other skeletal or extraskeletal lesions. The
overall findings met the diagnostic criteria of SP, therefore,
multiple myeloma was ruled out and the diagnosis of SP was
established.
The patient was initially treated with radiotherapy
at a dose of 45 Gy delivered in 15 fractions over 21 days. Half a
year later, chemotherapy consisting of vindesine (2 mg/day, days
1–4), Adriamycin (15 mg/day, days 1–4) and dexamethasone (20
mg/day, days 1–4, 9–12 and 17–20) was administered. In total, the
patient underwent 6 cycles of chemotherapy, with a total duration
of 7 months. The patient was followed for two years after beginning
therapy, without any signs of progressive disease or conversion to
multiple myeloma.
Discussion
The association between SP and multiple myeloma is
currently unclear. Certain individuals regard SP as a distinct
entity from multiple myeloma, while others regard SP as an early
presentation of multiple myeloma (3). The diagnostic criteria of SP of the
bone requires the presence of a solitary bone lesion confirmed by
skeletal survey, plasma cell infiltration proven by biopsy, the
absence of myeloma cells in the bone marrow and a lack of anemia,
hypercalcemia and renal involvement (13). The average age of onset of SP is
approximately one decade less than that for multiple meyloma, with
a median age of 56 years old (3).
The male to female ratio is approximately 2:1 (1). SP of the sternum is rare. The majority
of neoplasms of the sternum are metastases. Primary sternal
neoplasms are uncommon and are much more frequently malignant than
benign (2). In a study of the
Chinese literature that reported 30 cases and reviewed a total of
248 cases of sternal tumors, the most malignant tumors were
metastases, followed by myelomas, chondrosarcomas, lymphomas and
osteosarcomas; the most benign tumors were chondromas and
osteochondromas (14).
Sternal plasmacytoma usually presents as an
osteolytic expansile lesion or a typical ‘punched-out’ lytic lesion
on radiological examination (15).
The tumor usually destroys the cortex in several places and invades
the soft tissues (2,4). CT may demonstrate a subtle lytic
lesion or small soft-tissue masses of the sternal lesion that are
not visible by radiography (16).
On MR imaging, the tumors usually exhibit a low signal intensity on
T1-weighted images and a high signal intensity on T2-weighted
images (2).
In the present case, the tumor appeared as an
extensive, mildly expansile lytic lesion, with destruction of the
cortex and adjacent soft tissue mass. Around the periphery of the
lesion, there were straight bony spicules extending outward from
the cortex that resembled sunrays in appearance. To the best of our
knowledge, there have only been a few previous case studies with
bony spicules forming the appearance of sunrays (5–12). The
majority of these cases occurred in the mandible, while other
involved sites consisted of the orbit, vertebral body and skull
vault (5–12). The majority of these cases were
multiple myeloma; only two of the cases were SP (6,11).
Mohammadi et al reported a case of solitary mandibular
plasmacytoma, which displayed a lytic lesion with a sunray
periosteal reaction on the conventional radiograph (6). Lipper et al reported a solitary
osteosclerotic mandibular plasmacytoma with prominent sunray
spiculation, which radiologically mimicked an osteosarcoma
(11). This unique appearance can
be explained by the fact that any malignant cell has the potential
ability to stimulate the formation of new bone (6). Considering the radiological appearance
of the present case, malignant tumors should be considered.
Metastatic disease is the most common differential diagnosis; the
metastases are often multiple in number, with a larger soft-tissue
mass. In the present case, negative bone scintigraphy everywhere
except the sternum indicated a low possibility of metastatic
disease. The most common primary malignant tumor is chondrosarcoma.
It usually occurs in patients in the fourth to sixth decades of
life, and frequently appears as a large, lobulated mass with
multiple stippled calcifications (15). In the present case, there were no
calcifications in the lesion. Other conditions that can manifest
with a sunray appearance are osteosarcoma and Ewing’s sarcoma.
Osteosarcomas of the sternum generally occur in older patients
(median age, 42 years) compared with those of the extremities
(15). A mixed pattern consisting
of osteolysis and sclerosis is typical. With respect to the present
case, an expansile lytic lesion in a 74-year-old female is an
uncommon presentation for osteosarcoma. Ewing’s sarcoma is commonly
observed in young individuals, with 80% of cases recorded in
patients <20 years of age (5);
this condition was almost ruled out in the present case. Another
relatively common malignant tumor that occurs in the sternum is
lymphoma, which usually demonstrates permeated or moth-eaten bony
destruction with an extensive apparent mass. Occasionally, a
laminated periosteal bone reaction can be observed (5), however, an expansile lytic lesion with
a sunray periosteal reaction is rarely observed in lymphoma.
In conclusion, malignant tumors should be considered
if an osteolytic lesion with destruction of the cortex and soft
tissue mass is detected in the sternum. Although unusual, a
diagnosis of plasmacytoma must be considered in the presence of a
lytic lesion with peripheral bony spicules of sunray
appearance.
References
|
1
|
Reed V, Shah J, Medeiros LJ, et al:
Solitary plasmacytomas: outcome and prognostic factors after
definitive radiation therapy. Cancer. 117:4468–4474. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nakanishi K, Kashiwagi N, Hamada K, et al:
Solitary plasmacytoma of the sternum detected incidentally by MR
imaging of the cervical spine. Magn Reson Med Sci. 9:227–231. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Woodruff RK, Malpas JS and White FE:
Solitary plasmacytoma. II: Solitary plasmacytoma of bone. Cancer.
43:2344–2347. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Woodring JH, Umer MA and Bernardy MO:
Solitary plasmacytoma of the sternum: diagnosis by computed
tomography. J Comput Tomogr. 9:17–19. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ghosh S, Wadhwa P, Kumar A, et al:
Abnormal radiological features in a multiple myeloma patient: a
case report and radiological review of myelomas. Dentomaxillofac
Radiol. 40:513–518. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mohammadi A, Ilkhanizadeh B and
Ghasemi-Rad M: Mandibular plasmocytoma with sun-ray periosteal
reaction: A unique presentation. Int J Surg Case Rep. 3:296–298.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ramon Y, Oberman M, Horowitz I, et al: A
large mandibular tumor with a distinct radiological ‘sun-ray
effect’ as the primary manifestation of multiple myeloma. J Oral
Surg. 36:52–54. 1978.PubMed/NCBI
|
|
8
|
Baykul T, Aydin U and O Carroll MK:
Unusual combination of presenting features in multiple myeloma.
Dentomaxillofac Radiol. 33:413–419. 2004. View Article : Google Scholar
|
|
9
|
Porter EC: Osteogenesis in multiple
myeloma. Report of a case Radiology. 76:457–458. 1961.
|
|
10
|
Shozushima M, Suzuki M, Ito S, et al:
Multiple myeloma with a distinct ‘sun-ray appearance’ occurring in
the jaw. Oral Radiol. 3:121–126. 1987. View Article : Google Scholar
|
|
11
|
Lipper S, Kahn LB and Hesselson N:
Localised myeloma with osteogenesis and Russell body formation. S
Afr Med J. 49:2041–2045. 1975.PubMed/NCBI
|
|
12
|
Grover SB and Dhar A: Imaging spectrum in
sclerotic myelomas: an experience of three cases. Eur Radiol.
10:1828–1831. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bataille R and Sany J: Solitary myeloma:
clinical and prognostic features of a review of 114 cases. Cancer.
48:845–851. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jiang ZH: Radiologic diagnosis of tumors
of the sternum (analysis of 30 cases). Zhonghua Fang She Xue Za
Zhi. 22:286–289. 1988.(In Chinese). PubMed/NCBI
|
|
15
|
Restrepo CS, Martinez S, Lemos DF, et al:
Imaging appearances of the sternum and sternoclavicular joints.
Radiographics. 29:839–859. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jeung MY, Gangi A, Gasser B, et al:
Imaging of chest wall disorders. Radiographics. 19:617–637. 1999.
View Article : Google Scholar : PubMed/NCBI
|