Introduction
Solitary extramedullary plasmacytoma (EMP) is a rare
plasma cell neoplasm that occurs most frequently in head and neck
soft-tissue regions, with the nasopharynx, nasal cavity and
paranasal sinuses most commonly affected (1). The occurrence of EMP in the spleen is
extremely rare. According to a literature search performed in
PubMed, a total of six cases of splenic EMP have been previously
reported, with only four cases published in English (2–4).
However, no studies examining the computed tomography (CT) findings
of splenic EMP have been published. The present study investigated
an extremely rare case of solitary splenic EMP in a 23-year-old
female, examining the imaging features of the lesion, in particular
the multiple-phase spiral CT findings, and presented a review of
the literature. To the best of our knowledge, this is the first
study to examine the CT findings of EMP involving the spleen.
Case report
A 23-year-old female was admitted to the Second
Affiliated Hospital, Zhejiang University School of Medicine
(Hangzhou, China) following the discovery of a splenic mass during
a routine abdominal ultrasound. The patient had a history of
bleeding gums, but not of nausea, dyspnea, fever, abdominal pain or
intubation. Furthermore, no positive findings were identified
during a physical examination. The results of laboratory tests
revealed a hemoglobin level of 129 g/l, a platelet count of
259×109/l and a white blood cell (WBC) count of
8.0×109/l (normal ranges: Hemoglobin level, 113–151 g/l;
platelet count, 100–300×109/l; WBC count,
4.0–10.0×109/l). The differential WBC count identified a
total of 1.3% eosinophils, 25.3% lymphocytes and 6.2% monocytes
monocytes (normal ranges: Eosinophils, 0.0–10.0%; lymphocytes,
20–40%; monocytes, 4.0–12.0%). In addition, the tumor marker levels
of carcinoembryonic antigen, α-fetoprotein, carbohydrate antigen
(CA)19-9 and CA-125 were normal. An abdominal ultrasound revealed a
non-uniform, low echo, 8.4×7.5-cm, round lesion in the spleen. A
number of radiological and laboratory tests were performed in order
to eliminate systemic plasmacytoma. The full blood count and levels
of creatinine, serum calcium and uric acid were within the normal
ranges. The chest CT scan was normal, with the absence of any
pulmonary lesions or mediastinal lymph nodes. In addition, the
emission computed tomography skeletal survey was normal.
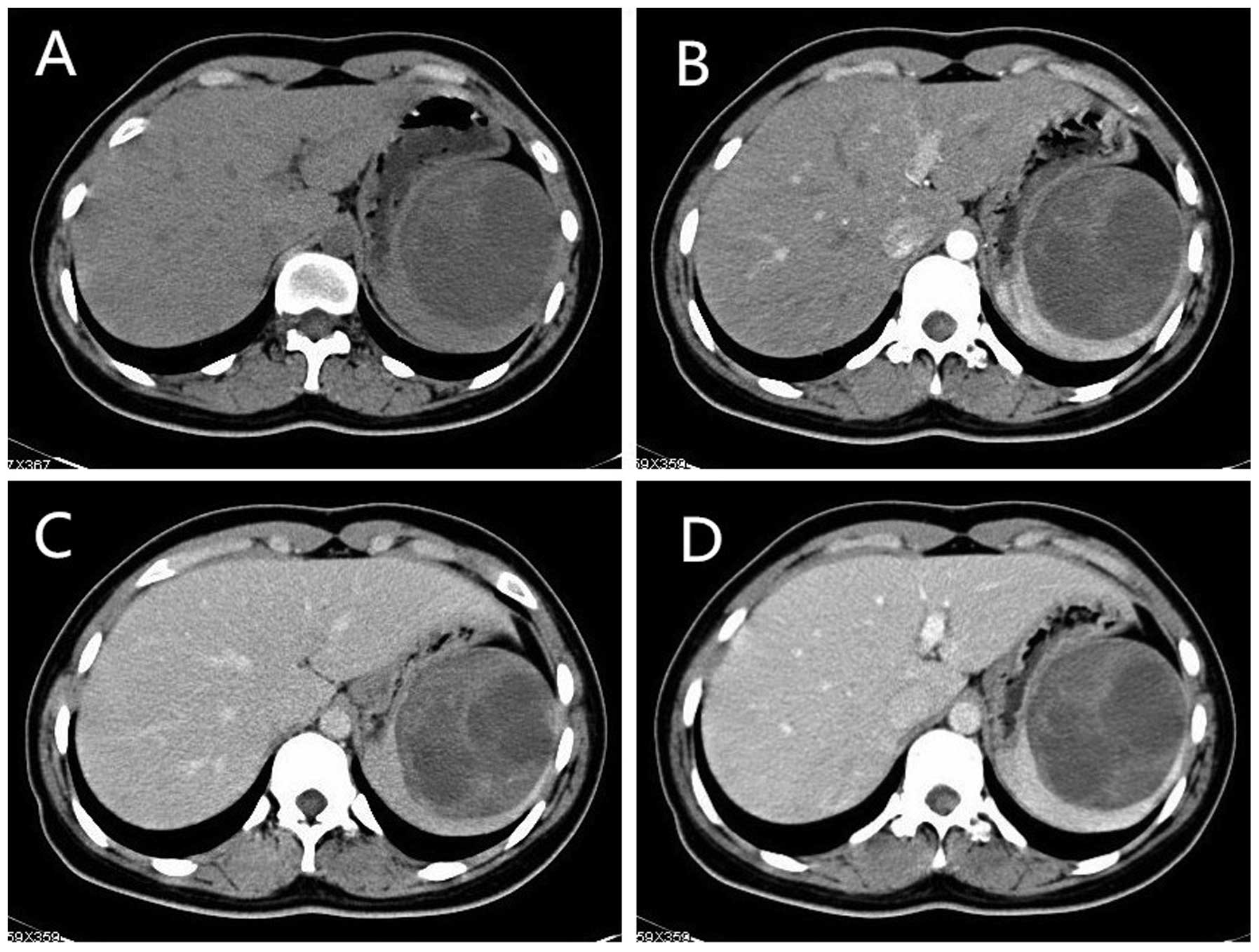
The pre-contrast CT revealed that the spleen was
enlarged and contained a solitary, well-defined mass, with areas of
variable cystic degeneration and necrosis. The mean CT attenuation
value of the solid portion was 39 HU, while the values observed for
the areas of necrosis and cystic degeneration were 21–23 HU
(Fig. 1A). Following a bolus
injection of the nonionic contrast agent iopamidol, the cystic
wall, internal septa and solid portion of the spleen demonstrated
mild enhancement, with a 43 HU attenuation value during the hepatic
artery phase. The areas of necrosis and cystic degeneration,
however, were non-enhancing (Fig.
1B). During the portal venous and hepatic parenchymal phases,
the cystic wall, internal septa and solid portion demonstrated a
slight and progressive enhancement, with mean CT attenuation values
of 54 HU and 63 HU, respectively (Fig.
1C and D).
The patient was transferred to the Department of
Surgery at the Second Affiliated Hospital, Zhejiang University
School of Medicine, where a laparotomy and splenectomy were
performed. The resected spleen was enlarged, with lymphoma-like
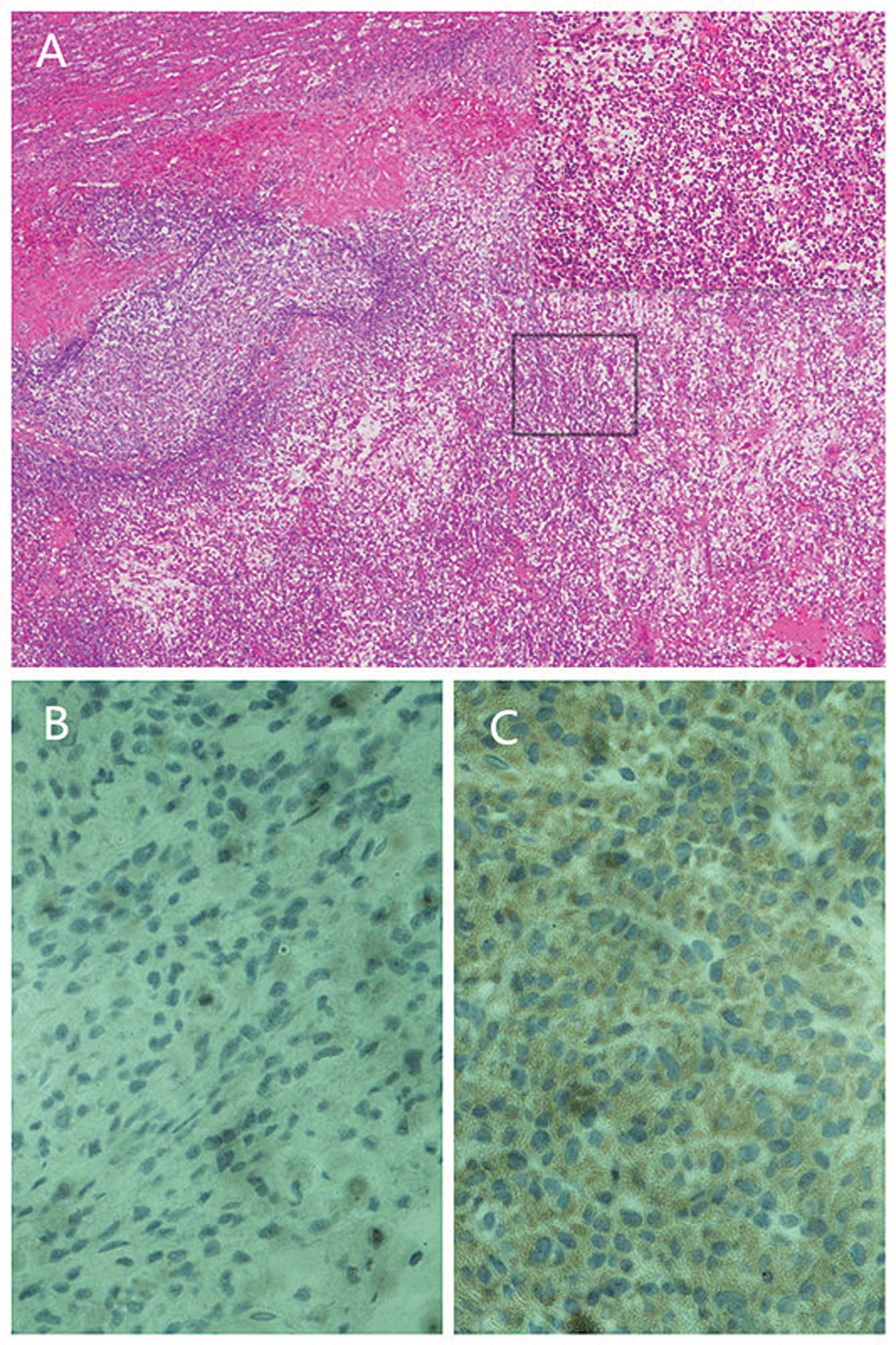
tumors infiltrating the parenchyma. Histopathology revealed a dense
monoclonal infiltrate of plasma cells with eccentrically situated
nuclei and a mild degree of nuclear polymorphism. In addition to a
variety of binuclear cellular forms with scattered mitoses,
perinuclear halos were observed in a number of the cells (Fig. 2A). The immunohistochemical analysis
revealed that the cells were cluster of differentiation
(CD)79A-positive and CD20-negative. Furthermore, the
immunohistochemical staining was positive for λ-light chains, but
negative for κ-light chains (Fig. 2B
and C). These findings were consistent with the diagnostic
criteria of plasmacytoma.
Post-operatively, the patient recovered without
complications, and no evidence of tumor recurrence has occurred
during the past two years of follow-up.
Discussion
In total, <10% of patients with plasma cell
neoplasms present with solitary plasmacytoma (SP). SP is classified
according to location as either solitary plasmacytoma of the bone
(SPB) or EMP (5). The majority of
cases of SPB occur in areas of the axial skeleton, such as the
vertebrae and the skull (5),
whereas cases of EMP are usually observed in the head and neck. A
study consisting of 334 cases of EMP revealed that lesions existing
in the upper respiratory tract (in particular the nasal sinuses and
pharynx nasalis) accounted for 75% of cases, while the lower
respiratory tract represented 4%, the lymph nodes and spleen 6%,
the thyroid 3%, the testis 1% and other sites 4% (6).
The median age of patients with either SPB or EMP is
55 years old (5). The overall male
to female ratio for SP is 2:1 (7).
In the present study, the patient was a 23-year-old female who was
considerably below the median age for EMP, and was the youngest
reported patient with splenic EMP. Pasch et al (8) advocated that trauma may have a
potential role in the pathogenesis of SPB affecting young
individuals of <30 years old. However, in the present case
study, the patient denied the incidence of prior trauma.
Furthermore, the symptoms of splenic EMP are often unremarkable.
According to the four reported cases of splenic EMP in the English
literature (2–4), one patient was admitted to hospital
due to right pleuritic chest pain and shortness of breath, and a
second experienced chills, night sweats, malaise, a temperature of
>38.5°C and a 6-kg loss in weight a month prior to admission. In
the present case study, the patient was asymptomatic and discovery
of the tumor was incidental. Due to a localized presentation and
favorable diagnosis, EMP is distinct from SPB and multiple myeloma
(6). Treatment with radiotherapy
alone may confer long-term disease-free survival for ~30 and 65% of
patients with SPB and EMP, respectively.
Owing to the rarity of the condition, the CT
findings of splenic EMP, in particular the radiological
manifestations of multiple-phase spiral CT, have not been
well-studied. A number of studies investigating the CT findings of
EMPs in other organs were identified during the literature search
for the present study. One study, which examined a case of
pancreatic EMP, demonstrated a large homogeneously-enhancing mass
in the region of the pancreatic head (9). A second study revealed a
well-demarcated, minimally homogeneously-enhancing, 1.5×1.0×1.2-cm
mass in the left arytenoid region of the larynx (10). However, in the present study, CT
identified a heterogeneously-enhancing mass with a non-enhancing
hypointense area. This observation may be associated with the
larger size of the tumor. Upon review of the literature of SPB, the
tumor often manifests as a well-defined, ‘punched-out’ lesion with
associated soft-tissue masses and bone cortex destruction, with
occasional thick-ridging at the periphery, and rare incidences of
necrosis or cystic degeneration (11). In the present study, the splenic
tumor demonstrated variable areas of necrosis and cystic
degeneration, which suggested that EMP may have a different
manifestation upon spiral CT than that observed for SPB.
A number of differential diagnoses exist that should
be considered when a large, solitary, splenic mass with variable
areas of necrosis is detected (12). Malignant tumors, including
hematolymphangioma, hemangiosarcoma and lymphoma, and cases of
solitary metastasis or abscess, should be ruled out during
diagnosis.
The present case study described the case of a
23-year-old female with a large SP of the spleen. To the best of
our knowledge, this patient was the youngest of all reported cases.
Although EMP of the spleen is extremely rare, and a diagnosis can
only be confirmed by pathological examination, the disease should
be considered during the differential diagnosis of large, splenic,
malignant tumors. In order to reduce the misdiagnosis of EMP,
future studies should focus on extending existing
clinicopathological knowledge of the disease.
Acknowledgements
The authors would like to thank the Department of
Pathology, Second Affiliated Hospital, Zhejiang University School
of Medicine for providing support with the immunohistochemical
analysis.
References
|
1
|
Horny HP and Kaiserling E: Involvement of
the larynx by hemopoietic neoplasms. An investigation of autopsy
cases and review of the literature. Pathol Res Pract. 191:130–138.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Perry-Thornton E, Verly GP, Karkala J and
Walker M: An unusual presentation of multiple myeloma: primary
plasmacytoma of the spleen. J Natl Med Assoc. 81:1095–1096.
1989.PubMed/NCBI
|
|
3
|
Colović MD, Janković GM, Colović RB and
Martinović-Cemerikić VM: Non-secretory solitary plasmacytoma of the
spleen. Med Oncol. 15:286–288. 1998. View Article : Google Scholar
|
|
4
|
Horny HP, Saal J and Kaiserling E: Primary
splenic presentation of plasma cell dyscrasia: report of two cases.
Hematol Pathol. 6:155–160. 1992.PubMed/NCBI
|
|
5
|
Dimopoulos MA, Moulopoulos LA, Maniatis A
and Alexanian R: Solitary plasmacytoma of bone and asymptomatic
multiple myeloma. Blood. 96:2037–2044. 2000.PubMed/NCBI
|
|
6
|
Kayrouz T, Jose B, Chu AM and Scott RM:
Solitary plasmacytoma. J Surg Oncol. 24:46–48. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Galieni P, Cavo M, Pulsoni A, Avvisati G,
Bigazzi C, Neri S, et al: Clinical outcome of extramedullary
plasmacytoma. Haematologica. 85:47–51. 2000.PubMed/NCBI
|
|
8
|
Pasch W, Zhao X and Rezk SA: Solitary
plasmacytoma of the bone involving young individuals, is there a
role for preceding trauma? Int J Clin Exp Pathol. 5:463–467.
2012.PubMed/NCBI
|
|
9
|
Smith A, Hal H and Frauenhoffer E:
Extramedullary plasmacytoma of the pancreas: a rare entity. Case
Rep Radiol. 2012:7982642012.PubMed/NCBI
|
|
10
|
Kim KS, Yang HS, Park ES and Bae TH:
Solitary extramedullary plasmacytoma of the apex of arytenoid:
endoscopic, CT, and pathologic findings. Clin Exp Otorhinolaryngol.
5:107–111. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jeung MY, Gangi A, Gasser B, Vasilescu C,
Massard G, Wihlm JM and Roy C: Imaging of chest wall disorders.
Radiographics. 19:617–637. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Thompson WM, Levy AD, Aguilera NS, Gorospe
L and Abbott RM: Angiosarcoma of the spleen: imaging
characteristics in 12 patients. Radiology. 235:106–115. 2005.
View Article : Google Scholar : PubMed/NCBI
|