Introduction
Pulmonary benign metastasizing leiomyoma (BML) is a
rare disease that is commonly thought to develop years after the
diagnosis and resection of uterine leiomyoma. The majority of BML
patients reported in the literature possess a previous history of
uterine leiomyoma resectioning, with the time period between
uterine leiomyoma resectioning and nodule detection varying between
three and 20 years (1). The
majority of cases of BML reported in the literature presented as
diffuse bilateral pulmonary nodules, occasionally accompanied by
multiple pleural or peritoneal nodules (2). The main metastatic site of BML is the
lung, of which the majority are bilateral nodules, 17% are
unilateral nodules and 13% are solitary nodules (3), however, extrapulmonary lesions have
been identified in the skin, greater omentum, inferior vena cava,
right atrium of the heart, pelvis, muscle and brain (2,4). The
present study reports an asymptomatic presentation of BML, in which
histological examination, immunohistochemistry studies and clinical
history correlation were performed to support the diagnosis.
Written informed consent was obtained from the patient.
Case report
The present study reports the case of a 45-year-old
female who was referred to the Tianjn Medical University General
Hospital (Tianjin, China) in March 2013 for the further examination
of multiple bilateral pulmonary nodules that were incidentally
identified on imaging during a regular check-up five months prior
to the referral, on October 31, 2012. The patient was asymptomatic
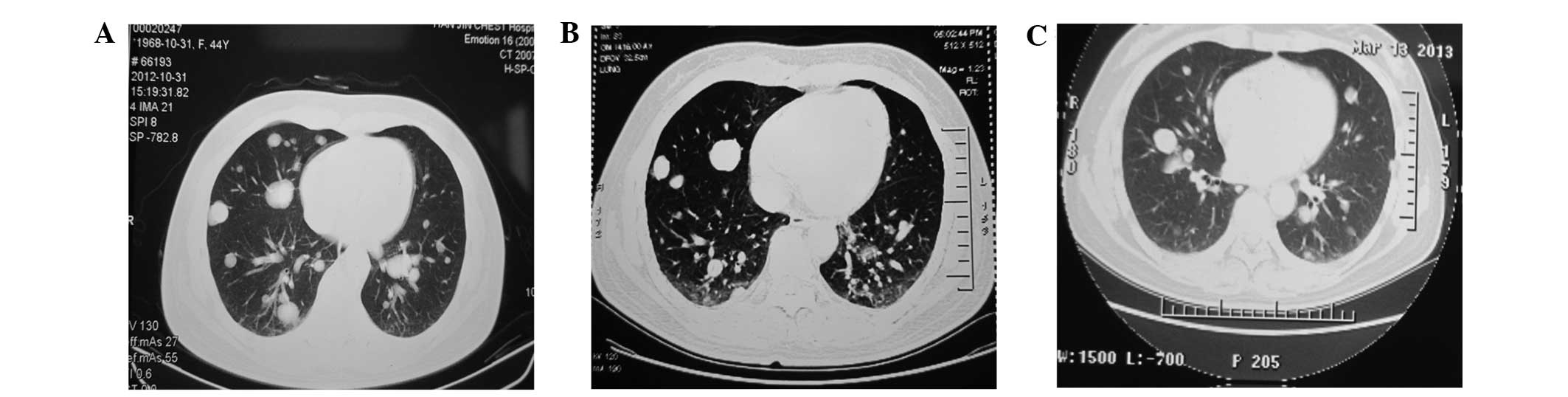
prior to hospitalization. Chest computed tomography (CT) was
performed at Tianjin Chest Hospital (Tianjin, China), which
revealed multiple variable-sized bilateral pulmonary nodules and a
soft-tissue mass in the basal segment of the left upper and
bilateral lower lobes (Fig. 1). The
patient was subsequently administered intravenous levofloxacin (0.5
g/day) for one week. The results of the pulmonary function testing
and the bronchoscopic examination were normal. Positron emission
tomography combined with CT (PET/CT), performed at Tianjin Medical
University Cancer Institute and Hospital (Tianjin, China), revealed
an abnormal fluorodeoxyglucose uptake, with the suspicion of
multiple variable-sized bilateral pulmonary nodules and lumps, and
no evident radioactivity concentration was revealed. The patient
was re-examined every two months using pulmonary CT due to the
suspicion of metastasizing leiomyoma. No additional drugs were
administered to the patient as no clinical symptoms were
observed.
Five days prior to admission, an enhanced chest CT
at the Tianjin Medical University General Hospital revealed
multiple variable-sized bilateral pulmonary nodules and lumps.
Certain nodules demonstrated significant enhancement, and other
regions were attached to intrapulmonary vessels. Non-enlarged
bilateral hilar lymph nodes, non-enlarged multiple small lymph
nodes in the mediastinum and non-thickened bilateral pleura were
observed. The quantity of nodules and lumps had increased compared
with the PET/CT results obtained four months previously, which
indicated a metastatic disease, without the exclusion of
granulomatous angiitis (Fig. 1). An
aspiration biopsy was performed for further diagnosis. The patient
had experienced uterine leiomyoma 11 years prior to the current
presentation, for which a laparoscopic myomectomy had been
performed. The previous health of the patient was reasonable,
without any smoking, drinking or familial history of cancer.
The results of the clinical examination were
unremarkable, and the results from the routine laboratory tests
were as follows. The results of the routine blood, urine and stool
tests and liver and kidney function were normal, as were the four
checking categories of lung cancer (carcino-embryonic antigen,
neuron specific enolase, squamous cell carcinoma antigen and serum
cytokeratin 19 fragment levels), and the levels of terminal
restriction fragment, carbohydrate antigen (CA) 19-9, CA242, CA153
and human epididymis protein 4. The results of immune complex
testing and testing for rheumatoid and anti-neutrophil cytoplasm
antibodies were normal. The level of the antibodies against
Mycoplasma pneumonia, Chlamydia pneumonia and
Legionella pneumophila were normal. The results of the
1–3-β-D polyglucosan and purified protein derivative tests revealed
negative results. Using a blood gas analyzer, the erythrocyte
sedimentation rate in the patient was found to be 11 mm/h, while
the blood pH was 7.46, the partial pressure of carbon dioxide was
37 mmHg, the partial pressure of oxygen was 84 mmHg and the oxygen
saturation was 97%. The lavage liquid consisted of 77.5%
macrophages, 19.5% lymphocytes, 3% neutrophil granulocyte and 0%
eosinophilic granulocytes. No bacteria, fungi or yeast were
identified in the alveolar lavage fluid, and acid-fast staining did
not yield a positive result. The pelvic scan revealed a normal
uterine shape, a non-uniformity of signals in the muscular layer
and multiple cervical cysts.
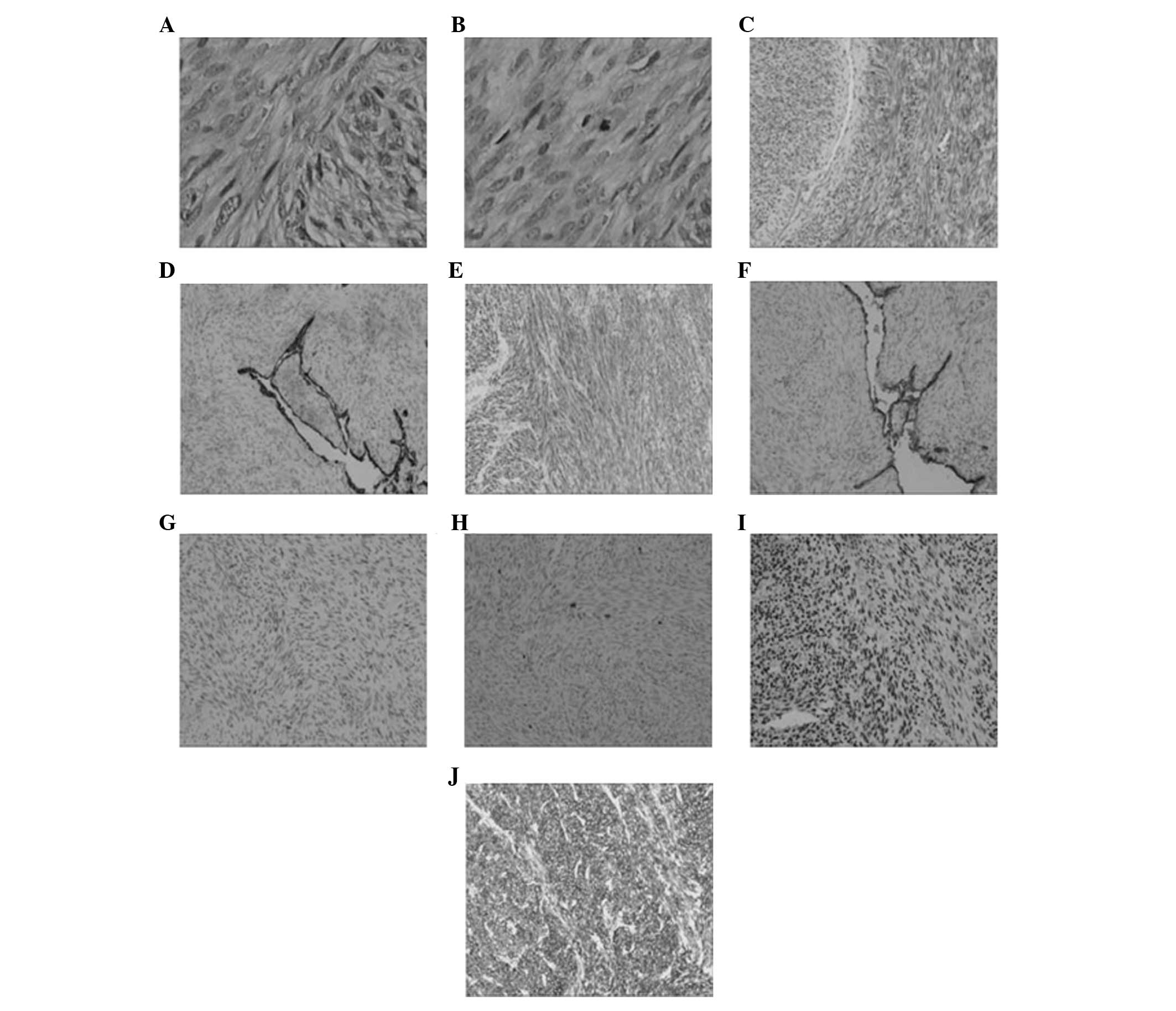
A pulmonary wedge resection was performed on the
right lung using video-assisted thoracoscopic surgery one week
subsequent to admission. During the surgery, multiple nodules that
were 1–2.5 cm at the maximum dimension were noted in each lobe of
the right lung. Certain nodules extended to the two pleural
surfaces. A hard and oval-shaped lump located in the middle and
lower lobes was 3 cm in length and exhibited a similar appearance
to the pulmonary surface, which connected with the right pulmonary
lower lobe via the pleural surface. Intra-operative frozen section
examination revealed that the lung wedge specimen was composed of
three hoary nodules that were 3×2.8×1.5 cm, 1.2×1.2×0.7 cm, and
0.7×0.6×0.5 cm in size. However, BML in the right pulmonary lower
lobe was accompanied by local necrosis. Immunohistochemical studies
revealed that these cells were positive for the expression of
smooth muscle actin, desmin, estrogen receptor, progesterone
receptor and B-cell lymphoma-2, while there was no expression of
cytokeratin or epithelial membrane antigen. Staining for Ki-67
revealed expression in ~1% of the spindle cells. These findings
were consistent with benign metastasizing leiomyoma that developed
from the known primary uterine leiomyoma (Fig. 2). The patient was discharged without
any early post-operative complications. After five months of
follow-up the general condition of the patient was satisfactory,
without any radiological evidence of recurrent disease or distant
metastases. Patient follow up is ongoing.
Discussion
BML occurs mainly in premenopausal and
perimenopausal females with a mean age of 47 years old (range,
30–74 years old). All BML patients reported in the literature
possess a previous history of resectioning for uterine leiomyoma,
with the time period between uterine leiomyoma resectioning and
nodule detection varying between three and 20 years (1). The radiological presentation of BML is
diffuse bilateral pulmonary nodules (2), occasionally accompanied by multiple
pleural or peritoneal nodules. The main metastatic site of BML is
the lung, of which the majority are bilateral nodules, 17% are
unilateral nodules and 13% are solitary nodules (3), but extrapulmonary lesions have been
documented in the skin, greater omentum, inferior vena cava, right
atrium, pelvis, muscle and brain (2,4). The
majority of patients with BML are asymptomatic and are diagnosed
during physical examinations. The severity of the symptoms is
strongly correlated with the size and quantity of nodules.
Approximately one-third of patients present with cough, dyspnea and
chest pain, and progressively develop respiratory insufficiency and
failure, eventually succumbing to the disease. There are three
clinical types of BML, according to the tumor position: a) BML in
the pulmonary interstitium accompanied by chest tightness and
dyspnea during tumor growth, which is common and asymptomatic; b)
BML in the endobronchial lesions resulting in a non-specific,
irritating cough and recurrent obstructive pulmonary emphysema at
the early stage, which is not as common as the aforementioned type;
and c) BML in the pulmonary vessels with repeated hemoptysis, which
is rare. The patient in the present study possessed BML of the
pulmonary interstitium.
The nature and etiology of BML remain controversial.
Certain researchers hypothesize that BML is a type of multiple
smooth muscle in situ proliferation that is induced by
estrogen and progesterone, while others support that BML results
from the monoclonal, hematogenous spread of a differentiated
uterine leiomyoma (5). However, the
majority of studies concur with BML being a metastatic leiomyoma
that metastasizes between the uterus and the lung, due to all
reported cases being in women with a previous history of uterine
leiomyoma resectioning (1). The
patient possessing multiple nodular lesions of various sizes in the
bilateral lungs reported in the present study had undergone
excision of uterine leiomyoma 10 years previously. Certain studies
have reported cases with BML accompanied by multiple pleural or
peritoneal nodules. In addition, the majority of recent findings
are also consistent with the hypothesis of a monoclonal origin of
the uterine and pulmonary tumors (6). All these studies indicate that
pulmonary leiomyoma is metastatic. However, BML has been determined
to be a benign lesion as these tumors consist of
well-differentiated, benign-appearing smooth muscle cells with a
regular karyotype that lacks pleomorphism or mitotic figures.
However, additional study is required to determine the existence of
primary pulmonary leiomyoma, as leiomyoma arising in men and
children has been reported as non-metastatic, with residual alveoli
in the lesions and no vascular tumor thrombus in the lung (7).
The majority of patients with BML possess a good
prognosis, with the median survival time of 94 months (range, 6–101
months) subsequent to the excision of the intrapulmonary lesions
(8). Schneider et al
reported 10 cases with a median follow-up duration of 4.7 years
(9). No local complications
occurred, and no patients succumbed to BML. However, mortality is
reported in certain cases. Therefore, BML is a borderline tumor
with benign histological features, despite the biological behavior
indicating malignancy (10).
In conclusion, although BML is a rare condition, it
should be considered during the diagnosis of asymptomatic females
of reproductive age with a history of uterine leiomyoma that
present with solitary or multiple pulmonary nodules.
Abbreviations:
|
BML
|
benign metastasizing leiomyoma
|
|
CT
|
computed tomography
|
|
PET/CT
|
positron emission tomography
|
|
SMA
|
smooth muscle actin
|
|
ER
|
estrogen receptor
|
|
PR
|
progesterone receptorl
|
References
|
1
|
Taftaf R, Starnes S, Wang J, et al: Benign
metastasizing leiomyoma: A rare type of lung metastases - two case
reports and review of the literature. Case Rep Oncol Med.
2014:8428412014.
|
|
2
|
Egberts JH, Schafmayer C, Bauerschlag DO,
Jänig U and Tepel J: Benign abdominal and pulmonary metastasizing
leiomyoma of the uterus. Arch Gynecol Obstet. 274:319–322. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Allen MS: Multiple benign lung tumors.
Semin Thorac Cardiovasc Surg. 15:310–314. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yoon G, Kim TJ, Sung CO, et al: Benign
metastasizing leiomyoma with multiple lymph node metastasis: a case
report. Cancer Res Treat. 43:131–133. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nakanishi S, Nakano K, Hiramoto T, Shimizu
M, Nakamura K and Yamane N: So-called benign metastasizing
leiomyoma of the lung presenting with bone metastases. Nihon
Kokyuki Gakkai Zasshi. 37:146–150. 1999.(In Japanese). PubMed/NCBI
|
|
6
|
Tietze L, Günther K, Hörbe A, et al:
Benign metastasizing leiomyoma: a cytogenetically balanced but
clonal disease. Hum Pathol. 31:126–128. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Maredia R, Snyder BJ, Harvey LA and
Schwartz AM: Benign metastasizing leiomyoma in the lung.
Radiographics. 18:779–782. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Patton KT, Cheng L, Papavero V, et al:
Benign metastasizing leiomyoma: clonality, telomere length and
clinicopathologic analysis. Mod Pathol. 19:130–140. 2006.
View Article : Google Scholar
|
|
9
|
Schneider T, Kugler C, Kayser K and
Dienemann H: Benignes, pulmonal metastasierendes Leiomyom des
Uterus. Der Chirurg. 72:308–311. 2001.(In German). View Article : Google Scholar
|
|
10
|
Ki EY, Hwang SJ, Lee KH, Park JS and Hur
SY: Benign metastasizing leiomyoma of the lung. World J Surg Oncol.
11:2792013. View Article : Google Scholar : PubMed/NCBI
|