Introduction
Struma ovarii is a rare ovarian neoplasm consisting
almost exclusively of mature thyroid tissue (>50%) derived from
germ cells in a mature teratoma (1). Few of these cases undergo malignant
transformation (2). Meigs’ syndrome
refers to a solid benign ovarian neoplasm, such as fibroma or
thecoma accompanied by ascites and hydrothorax which are required
to completely resolve following removal of the tumor (3). Pesudo-Meigs’ syndrome is often
characterized by pleural effusion and ascites caused by a pelvic
tumor other than an ovarian fibroma. Rare cases of ovarian tumors
have been associated with pseudo-Meigs’ syndrome, such as struma
ovarii tumors, mucinous or serous cystadenomas, germ cell tumors
and ovarian metastasis from colon and gastric cancers (2). When coexisting with pesudo-Meigs’
syndrome and elevation of CA 125, struma ovarii is highly suspected
as an ovarian malignancy. Struma ovarii mimicking advanced ovarian
carcinoma can cause difficulties in preoperative diagnosis
(1). Diagnosis of struma ovarii can
only be made by conducting histopathology (4). The present study focused on a patient
presenting with struma ovarii, who was initially thought to have an
ovarian malignancy prior to surgery based on clinical, radiological
findings and raised CA 125 levels. However, the frozen section and
final histopathology reports revealed benign struma ovarii. A
systematic review of the related literatures on struma ovarii
presenting as pseudo-Meigs’ syndrome with elevated serum CA 125 was
also conducted. Written informed consent was obtained from the
patient.
Case report
On April 3, 2014, a 52-year-old, Chinese female,
premenopausal, gravida 3, para 1, was admitted to the United
Hospital of Dezhou (Dezhou City, China), complaining of oppression
in chest and shortness of breath for 5 days. The patient’s previous
menstrual period was March 31, 2014. The patient did not complain
of any pain or changes in micturition or bowel movements. The
patient’s medical history included surgery for an ovarian tumor 26
years previously and surgery for a broad ligament tumor 10 years
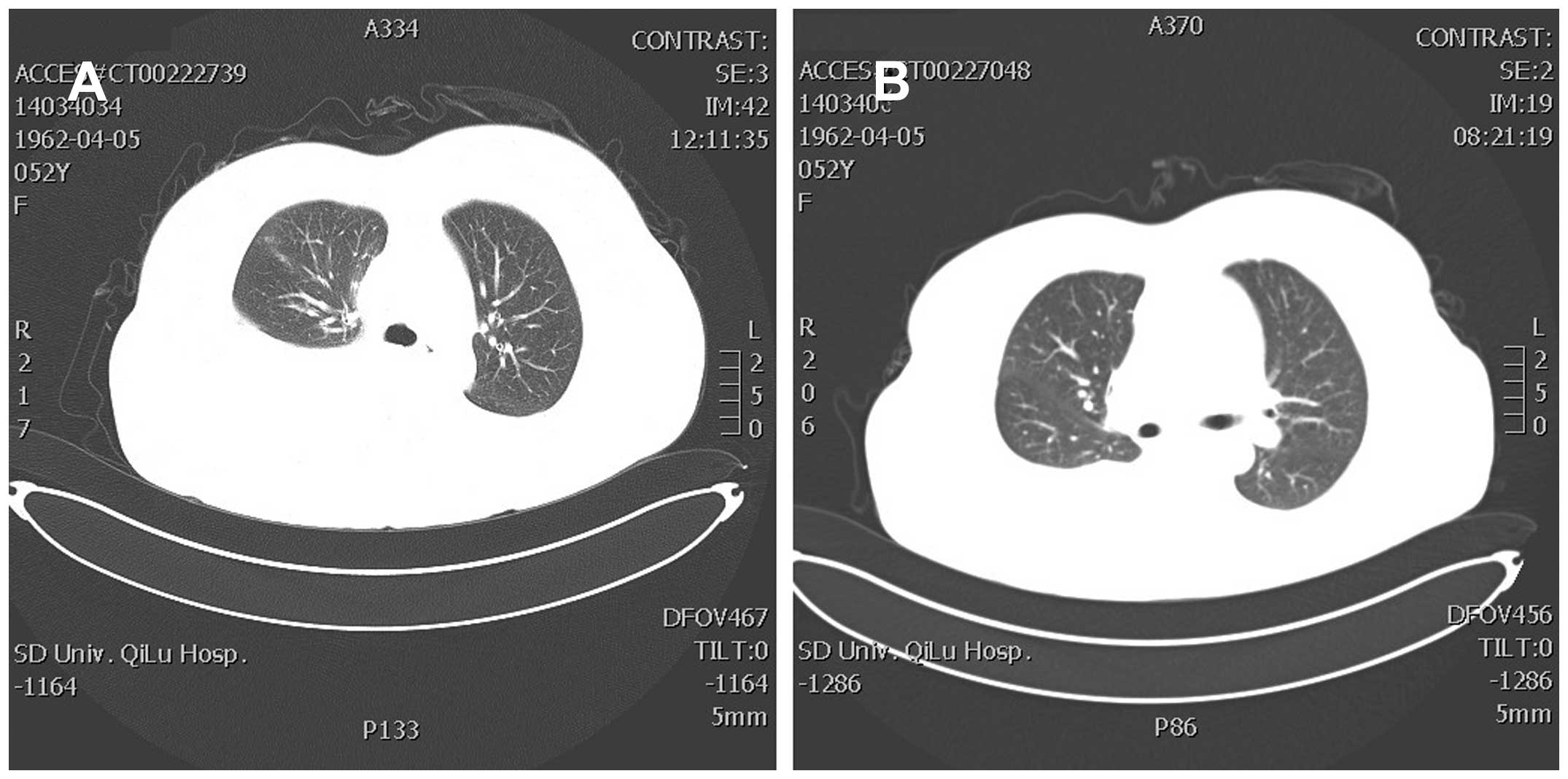
previously. Non-enhanced CT imaging of the chest showed bilateral
pleural effusions, particularly the right thoracic cavity. Marked
ascites, and a large solid and cystic mass (65×56×69 mm) in the
right ovary were detected by pelvic ultrasound. On April 8, 2014,
the patient was subsequently transferred to the Department of
Gynecology of Qilu Hospital, Shandong University (Jinan,
China).
On admission, the patient was found to have ascites
and bilateral pleural effusion. The gynecological examination
revealed a mass in the right adnexal region with a normal-sized
mobile uterus. Abdominal and pelvic ultrasound confirmed the
presence of ascites and a large irregular, cyst-solid-mixed mass in
the right ovary, ~75×56 mm in size. CT scan of the chest, abdomen,
and pelvis revealed bilateral lung basal atelectasis with a large
right pleural effusion, gross ascites, and a large loculated
complex cystic pelvic mass. There was no evidence of enlarged lymph
nodes. To alleviate symptoms and aid in the diagnosis,
thoracentesis was performed to yield straw-colored fluid (800 ml)
consistent with an exudative process. There was approximately 2,000
ml pleural effusion. Paracentesis yielded an exudate (2,200 ml),
found to be negative for malignant cells and mycobacterium
tuberculosis. Cytological examination of the fluid revealed benign
mesothelial cells and a few lymphocytes without malignant cells.
The serum CA 125 level was 1,289 U/ml (normal value <35 U/ml).
The AFP and CEA levels were within normal range. Liver function
tests were also within normal limits.
The patient was arranged for an exploratory
laparotomy through a vertical supraumbilical midline excision for
diagnostic and therapeutic purposes. The patient was found to have
ascites and 1,000 ml of straw-colored fluid was drained upon
entrance to the peritoneal cavity. Extensive adhesions between
posterior/left wall of uterus, left ovary, oviduct and intestinal
canal as well as its surrounding tissues were identified. A 7×5 cm
mixed cystic-solid neoplasm was found to arise from the right
ovary. The left ovary, the two fallopian tubes, the uterus,
diaphragm, bowel, and omentum appeared to be free of disease. There
was no evidence of enlarged lymph nodes or metastatic lesions. The
right tube and ovary were removed for frozen section and it was
suggestive of cystic mature teratoma with a large component of
thyroid. The patient and family member insisted on a hysterectomy
and left salpingo-oophorectomy, which were performed.
Thyroid function tests were not performed prior to
surgery as the struma ovarii was not taken into consideration.
Following the diagnosis, thyroid function tests were obtained on
the third postoperative day. The results of the tests revealed
normal thyroid function with serum FT3 levels at 2.05 pg/ml
(1.8–4.6 pg/ml), FT4 levels at 17.79 pmol/l (12–22 pmol/l) and TSH
levels at 2.9 uIU/ml (0.27–4.2 uIU/ml). Mild hypoalbuminemia was
observed. On the sixth day post-operation the level of CA 125 was
decreased to 609.6 U/ml. On the seventh day post-operation another
chest CT was taken, examined and compared with the pre-operative
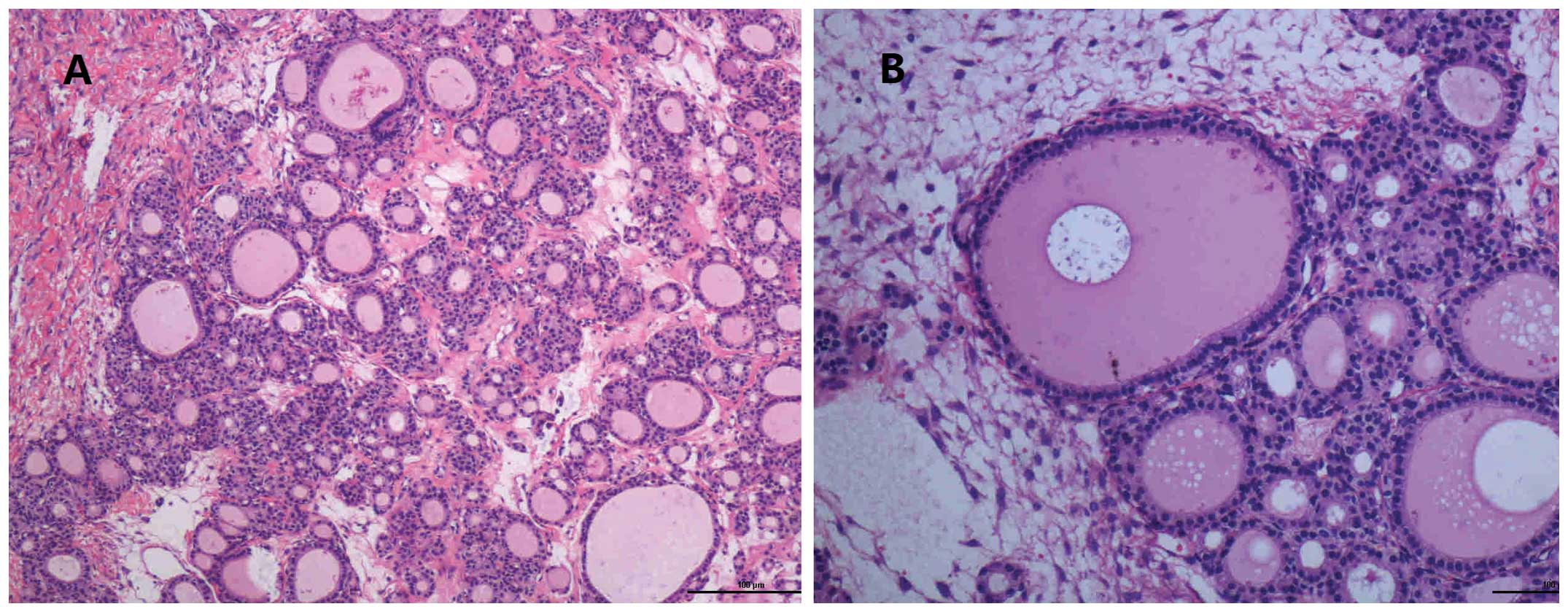
one (Fig. 1). The final pathology
revealed right struma ovarii with benign thyroid tissue confined to
the ovary (Fig. 2). The left ovary,
the uterus and bilateral fallopian tube were histologically
unremarkable. The rapid regression of effusions was demonstrated
following excision of the neoplasm. The patient recovered
uneventfully and was discharged on day 12 post-operatively.
Recovery was rapid, with no evidence of re-accumulation of the
pleural effusions or ascites. At 8 weeks follow-up, the patient was
clinically well, with no evidence of disease on physical
examination and normal CA 125 levels (6.5 U/ml).
Discussion
Struma ovarii is an uncommon benign neoplasm of
ovary that usually presents with asymptomatic mass and is difficult
to diagnose prior to surgery. Ascitic fluid is identified in 20% of
cases of struma ovarii (5). Struma
ovarii has been associated with pseudo-Meigs’ syndrome in 5% of
cases (6). The detailed mechanism
of ascites and pleural effusions is obscure. Potential explanations
include: irritation of the peritoneum by the tumor, obstruction of
the lymphatics, toxins and release of inflammatory products,
hypoalbuminemia, and discrepancy between the arterial supply and
the venous and lymphatic drainage (7). Regarding the mechanism of pleural
effusions, dye test results have shown that these effusions are
likely to originate from the peritoneal fluid by mechanical
transfer through diaphragmatic openings (7).
Serum tumor markers are useful in determining the
potential malignancy of a mass. CA 125 is a classical tumor marker
that is effective in the surveillance of treated epithelial ovarian
cancers. However, CA 125 has poor specificity in the diagnosis of
epithelial ovarian cancers, as its elevation may also be associated
with other malignancies and benign, physiological states, including
pregnancy, endometriosis and menstruation (8). Elevated CA 125 accompanied by Meigs’
syndrome is a rare clinical condition that was reported in only 27
cases (4). The exact reason for the
elevated CA 125 in Meigs’ and pesudo-Meigs’ syndrome remains
unclear. A possible explanation proposed by Mui et al
(4) is the irritation and
subsequent inflammation of pleura and peritoneum surface produced
by the presence of free fluid in these spaces.
A postmenopausal female presenting with a pelvic
mass, ascites, pleural effusions, and elevated CA 125 levels
generally is highly indicative of a malignant process. Few cases of
struma ovarii accompanied with pseudo-Meigs’ syndrome, elevated CA
125 have been described. We performed a systematic review of
related studies obtained from PubMed by using a combination of free
words and MeSH. The search was not limited by publication time or
English literature. Ten case reports of struma ovarii combined with
pesudo-Meigs’ syndrome and elevated CA 125 level were identified
(Tables I and II). We report an eleventh case in the
literature with struma ovarii associated with pseudo-Meigs’
syndrome and elevated CA 125. Struma ovarii occurs mainly during
the 5th-6th decade of life. Almost 73% (8/11) of cases were
postmenopausal women. The average reported size of the tumor was 10
cm in the large dimension, mostly unilateral, with only 9.1% being
bilateral, with a right-side predominance and CA 125 levels that
were moderately elevated [124.9 U/ml (9)] or extremely elevated [3,803 U/ml
(10)]. Approximately 36.4% (4/11)
cases coexisted with thyroid disease, 50% for hypo- and
hyperthyroidism, respectively. All the cases except those reported
by Rana et al (11) were
initially suspected to be a malignant tumor. Complete remission of
the ascites, hydrothorax, and CA 125 was obtained following surgery
without any adjuvant therapy. Positive prognosis for all the cases
was reported.
 | Table IGeneral characteristics of reported
struma ovarii associated with pseudo-Meigs’ syndrome and elevated
CA 125 levels. |
Table I
General characteristics of reported
struma ovarii associated with pseudo-Meigs’ syndrome and elevated
CA 125 levels.
| Author | Year | Age (years) | Menstruation | Tumor size (cm) | Unilateral or
bilateral | CA 125 (U/ml) | Ascites volume
(ml) | Pleural effusions
(ml) | Refs. |
|---|
| Bethune et
al | 1996 | 62 | Postmenopause | 9×5×5 | Right | 1621 | Small amount | 3500 | (12) |
| Long et
al | 2001 | 53 | Postmenopause | 15×11×7 | Left | 540 | 4100 | NA | (9) |
| | 78 | Postmenopause | 12×10×5.2 | Left | 124.9 | NA | NA | |
| Huh et al | 2002 | 65 | Postmenopause | 5×4×4 | Right | 402 | 20000 | NA | (13) |
| Loizzi et
al | 2005 | 65 | Postmenopause | 7×7 | Right | 161 | Few liters | Large amount | (5) |
| Obeidat et
al | 2007 | 52 | Postmenopause | 10×15×8 | Right | 149 | 4000 | NA | (14) |
| Mitrou et
al | 2008 | 55 | Postmenopause | 22×23×10 | Left | 3803 | 8000 | NA | (10) |
| Paladini et
al | 2008 | 42 | Premenopause | 11×7.3×8 | Right | 2548 | 8000 | NA | (15) |
| Rana et
al | 2009 | 70 | Postmenopause | 7.5×5.5×4 | Bilateral | 284 | NA | NA | (11) |
| Jiang et
al | 2010 | 46 | Premenopause | 20×18×15 | Right | 1230.9 | 6000 | NA | (1) |
| Present | 2014 | 52 | Premenopause | 7×5 | Right | 1289 | 1000 | 2000 | |
 | Table IIClinical symptoms, treatments,
coexisting thyroid disease of reported struma ovarii associated
with pseudo-Meigs’ syndrome and elevated CA 125 level. |
Table II
Clinical symptoms, treatments,
coexisting thyroid disease of reported struma ovarii associated
with pseudo-Meigs’ syndrome and elevated CA 125 level.
| Author | Clinical
symptoms | Treatments | Coexisting thyroid
disease | Refs. |
|---|
| Bethune et
al | Acute shortness of
breath and ascites | Total abdominal
hysterectomy and bilateral salpingo-oophorectomy | Absent | (12) |
| Long et
al | Abdominal distension
and weight loss | Total abdominal
hysterectomy, bilateral salpingo-oophorectomy and infracolic
omentectomy | Absent | (9) |
| Abdominal distension,
ielus and weight loss | Total abdominal
hysterectomy and bilateral salpingo-oophorectomy | Absent | |
| Huh et al | Abdominal distension,
dyspnea | Total hysterectomy
and bilateral salpingo-oophorectomy and appendectomy and omental
biopsy | Hypothyroidism | (13) |
| Loizzi et
al | Dyspnea and diffuses
abdominal pain | A right
salpingo-oophorectomy | Hyperthyroidism | (5) |
| Obeidat et
al | Shortness of breath
and marked ascites | A total abdominal
hysterectomy, bilateral salpingo-opherectomy and omentectomy | Absent | (14) |
| Mitrou et
al | Large pelvic mass,
marked cachexia, ascites | A total abdominal
hysterectomy with bilateral salpingo-oophorectomy, infracolic
omentectomy, and lymph node sampling | Hypothyroidism | (10) |
| Paladini et
al | Ascites, fever,
diarrhea, vomiting and significant weight loss | Right
salpingo-oophorectomy | Hyperthyroidism | (15) |
| Rana et
al | Progressive abdominal
distention and breathlessness | Total abdominal
hysterectomy with bilateral salpingo-oophorectomy and partial
omentectomy | Absent | (11) |
| Jiang et
al | Fatigue, anorexia,
and abdominal swelling | Total abdominal
hysterectomy with bilateral salpingo-oophorectomy | Absent | (1) |
| Present | Oppression in chest
and shortness of breath | Total abdominal
hysterectomy with bilateral salpingo-oophorectomy | Absent | |
A number of unique features were identified in the
patient. Firstly, she presented with the sudden onset of large
pleural effusions. Secondly, she was premenopausal, her age being
younger than that of patients in which the majority of these tumors
occur. The rapid onset of oppression in chest and shortness of
breath, sinister ultrasound findings (marked ascites, a 65×56×69 mm
solid and cystic mass to the right adnexal region) and a
significantly elevated CA 125 level were highly suspicious for an
ovarian malignancy. Struma ovarii accompanied by pseudo-Meigs’
syndrome and elevated serum CA 125 should be considered in the
differential diagnosis of ovarian epithelial cancer.
Acknowledgements
The study was supported by the National Natural
Science Foundation of China (grant no. 81072122).
References
|
1
|
Jiang W, Lu X, Zhu ZL, et al: Struma
ovarii associated with pseudo-Meigs’ syndrome and elevated serum CA
125: a case report and review of the literature. J Ovarian Res.
3:182010. View Article : Google Scholar
|
|
2
|
Zannoni GF, Gallotta V, Legge F, et al:
Pseudo-Meigs’ syndrome associated with malignant struma ovarii: a
case report. Gynecol Oncol. 94:226–228. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Meigs JV: Fibroma of the ovary with
ascites and hydrothorax; Meigs’ syndrome. Am J Obstet Gynecol.
67:962–985. 1954.PubMed/NCBI
|
|
4
|
Mui MP, Tam KF, Tam FK and Ngan HY:
Coexistence of struma ovarii with marked ascites and elevated
CA-125 levels: case report and literature review. Arch Gynecol
Obstet. 279:753–757. 2009. View Article : Google Scholar
|
|
5
|
Hurlow RA, Greening WP and Krantz E:
Ascites and hydrothorax in association with struma ovarii. Br J
Surg. 63:110–112. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Loizzi V, Cormio G, Resta L, et al:
Pseudo-Meigs syndrome and elevated CA125 associated with struma
ovarii. Gynecol Oncol. 97:282–284. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Amant F, Gabriel C, Timmerman D and
Vergote I: Pseudo-Meigs’ syndrome caused by a hydropic degenerating
uterine leiomyoma with elevated CA 125. Gynecol Oncol. 83:153–157.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jacobs I and Bast RC Jr: The CA 125
tumour-associated antigen: a review of the literature. Hum Reprod.
4:1–12. 1989.PubMed/NCBI
|
|
9
|
Long CY, Chen YH, Chen SC, et al:
Pseudo-Meigs syndrome and elevated levels of tumor markers
associated with benign ovarian tumors - two case reports. Kaohsiung
J Med Sci. 17:582–585. 2001.
|
|
10
|
Mitrou S, Manek S and Kehoe S: Cystic
struma ovarii presenting as pseudo-Meigs’ syndrome with elevated
CA125 levels. A case report and review of the literature. Int J
Gynecol Cancer. 18:372–375. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rana V, Srinivas V, Bandyopadhyay S, et
al: Bilateral benign non functional struma ovarii with
Pseudo-Meigs’ syndrome. Indian J Pathol Microbiol. 52:94–96. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bethune M, Quinn M and Rome R: Struma
ovarii presenting as acute pseudo-Meigs syndrome with an elevated
CA 125 level. Aust N Z J Obstet Gynaecol. 36:372–373. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Huh JJ, Montz FJ and Bristow RE: Struma
ovarii associated with pseudo-Meigs’ syndrome and elevated serum CA
125. Gynecol Oncol. 86:231–234. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Obeidat BR and Amarin ZO: Struma ovarii
with pseudo-Meigs’ syndrome and elevated CA125 levels. J Obstet
Gynaecol. 27:97–98. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Paladini D, Vassallo M, Sglavo G and Nappi
C: Struma ovarii associated with hyperthyroidism, elevated CA 125
and pseudo- Meigs syndrome may mimic advanced ovarian cancer.
Ultrasound Obstet Gynecol. 32:237–238. 2008. View Article : Google Scholar : PubMed/NCBI
|