Introduction
Malignant growth in the head and neck area affects a
large group of individuals and remains a serious health issue;
worldwide, >600,000 new cases of head and neck squamous cell
carcinoma (HNSCC) are diagnosed every year (1). Within this group, cancer of the lips and
the oral cavity are the most frequent, with an incidence of nearly
250,000 cases annually (1). The
five-year relative survival rate varies from 20–90% depending upon
the primary tumor site of the tumor and the clinical stage at the
presentation of disease (2).
Treatment options for HNSCC include surgery and/or
radio(chemo)therapy. Despite the plethora of novel chemotherapeutic
agents, refined radiation protocols and carefully selected patients
for surgery, the overall survival of affected patients has only
improved marginally during the last 30 years (3). Nevertheless, the requirement for novel
therapeutic approaches remains undisputed.
One common approach for the identification of
potential therapeutic agents is tests in a monolayer cell culture
system (4). In the last 50 years, a
multitude of oncological studies have been performed with this
classic two-dimensional (2D) model. Important advantages of this
model are its wide availability, ease of use and low costs, and a
number of significant discoveries have been gained from its
application (5). However, the
artificial environment limits cell-cell interactions and thus
prohibits a number of the physiological processes present in solid
tumors (6). Furthermore, studies
indicate that 2D cell cultures are a poor predictor for clinical
benefits (7,8). These limitations are well-documented and
the first attempts to mitigate these problems date back almost 40
years (9).
More sophisticated cell models were therefore
developed. Multi-cellular spheroids were first described in 1970
with glioblastoma cells (9). These
three-dimensional (3D) spheroids are considered to superiorly
replicate the tumor environment, since spheroids allow cell-cell
and cell-matrix contacts. As for the effectiveness of
chemotherapeutic agents, the gradient of drug concentration in
tumors plays an important role (10).
Furthermore, the expression of surviving factors figures
prominently in drug resistance (11).
Studies have shown divergent response rates in colorectal carcinoma
cells due to different protein expression profiles (11).
The extracellular matrix appears to be one
significant factor for the resistance of a variety of cancer cells
to radiation (12). Another
significant factor for radioresistance is hypoxia in tumor cells. A
lack of oxygen is often discussed as a mechanism for consecutive
radioresistance and has been reported in human glioma cell lines
(13).
In HNSCC, one important issue is the susceptibility
of a patient to radiotherapy, since ~20% of patients only achieve a
partial response or no response to irradiation (14). Another key problem is recurrence
(15), since up to 50% of the
patients are confronted with recurrent disease (16). The spheroid cell model may explain
tumor biology more precisely and actualize therapy outcomes already
in in vitro models. However, only limited data for 3D HNSCC
cell models in comparison to 2D cell culture models is available
(17–19).
Therefore, the present study sought to establish
stable HNSCC spheroid protocols and accentuate its different
features compared with 2D cell culture methods. Thus, the present
study assessed the expression of important HNSCC proteins in the
spheroids and compared the results with a 2D cell model.
Ultimately, an established cytotoxicity protocol was established,
and radiation and chemotherapy treatments were compared in each
model.
Materials and methods
Cell Culture
The HNSCC SCC25, CAL27 and FaDu cell lines were
obtained from the American Type Culture Collection (Manassas, VA,
USA) or the German Collection of Microorganisms and Cell Cultures
(Braunschweig, Germany). The tumor cells were cultured as described
previously (20). In brief, monolayer
cells were grown in RPMI medium supplemented with 1%
penicillin-streptomycin and 10% fetal bovine serum (all Gibco BRL,
Gaithersburg, MD, USA). Spheroids were grown in Dulbecco's modified
Eagle's medium Ham's F-12 (Lonza, Verviers, Belgium) enriched with
epidermal growth factor (EGF; Sigma-Aldrich, St. Louis, MO, USA),
basic fibroblast growth factor (bFGF; Sigma-Aldrich) and B27
(Invitrogen Life Technologies, Carlsbad, CA, USA) supplement to
conduce multicellular growth; these are commonly used supplements
in free-floating spheroid models. The two cell models were cultured
in a humidified 5% CO2 atmosphere at 37°C.
Cytotoxicity assay
For the assessment of growth inhibition, cell
counting kit 8 (CCK-8; Dojindo Molecular Technologies Inc.,
Gaithersburg, MD, USA) was used. For the 2D cell culture, the assay
was performed according to the manufacturer's instructions. Hence,
3×103 cells per well were added to 96-well plates
(Sarstedt, Inc., Newton, NC, USA) and allowed to rest for 24 h. For
the 3D cell culture, 2×104 cells per well were seeded
into Ultra Low Attachment plates (Costar, Corning Life Sciences,
Tewksbury, MA, USA) and allowed to rest for 72 h. In each culture
model, the cells were treated with increasing concentrations of
cisplatin (0–20 µM) or radiation doses (0, 2, 4, 6 and 8 Gy) using
a conventional radiation source with 150-kV X-rays (dose rate, 1
Gy/0.73 min). After 72 h of incubation, cell growth was measured.
All experiments were carried out in triplicate and performed as at
least three independent experiments.
Immunohistochemistry
In the 2D cell model, 7.5×104 cells were
spun onto microscopic slides using a Shandon Cytospin II centrifuge
(130 × g for 3 min; Thermo Fisher Scientific, Waltham, MA, USA)
fixated with acetone for 3 min at 4°C. For the 3D cell model,
spheroids were grown as aforementioned. After 5 days, the spheroids
were fixated in 8% formaldehyde solution for 30 min, and
consecutively casted with 4% agarose gel and stored in
phosphate-buffered saline at 7°C until paraffinization. Ultimately,
tumor sections of a 2–3-µm thickness were created.
Immunohistochemical staining was performed as
previously described (20,21). The three cell lines were stained for
Ki-67, vascular endothelial growth factor receptor (VEGFR), EGF
receptor (EGFR) and survivin. Ki-67 serves as a proliferation
marker (22), VEGFR is an
(lymph)angiogenesis receptor (23),
EGFR is a member of the Her/erbB receptor family and an important
receptor tyrosine kinase in HNSCC (24), and survivin is described as an
apoptotic inhibitory protein (25).
Primary antibodies for Ki-67 (monoclonal rabbit antibody; Abcam,
Cambridge, MA, USA; dilution, 1:400), VEGFR (polyclonal rabbit
antibody; Sigma-Aldrich; dilution, 1:100), EGFR (monoclonal rabbit
antibody; Abcam; dilution, 1:100) and survivin (monoclonal rabbit
antibody; Abcam; dilution, 1:500) were applied for 60 min. A
polymer enhancer was used for 10 min prior to adding the
high-resolution polymer (Thermo Fisher Scientific) for 15 min.
Slides were developed using diaminobenzidine reagent (Thermo Fisher
Scientific), counterstained with hematoxylin, dehydrated and
mounted under a coverslip. Samples were analyzed using an Olympus
BH-2 microscope (Olympus Corporation, Tokyo, Japan) and assigned to
one of four categories of marker expression: 0, <5%; 1 (weak),
5–30%; 2 (moderate), 30–60%; and 3 (strong), 60–100%. An average
expression score was calculated for every cell line. Experiments
were repeated three times and histological analysis was performed
by two independent investigators.
Statistical analysis
Data was analyzed by Student's t-test or one-way
analysis of variance using SPSS software version 21 (IBM SPSS,
Armonk, NY, USA). P<0.05 was considered to indicate a
statistically significant difference. All experiments were repeated
at least three times. Error bars represent the standard error of
the mean.
Results
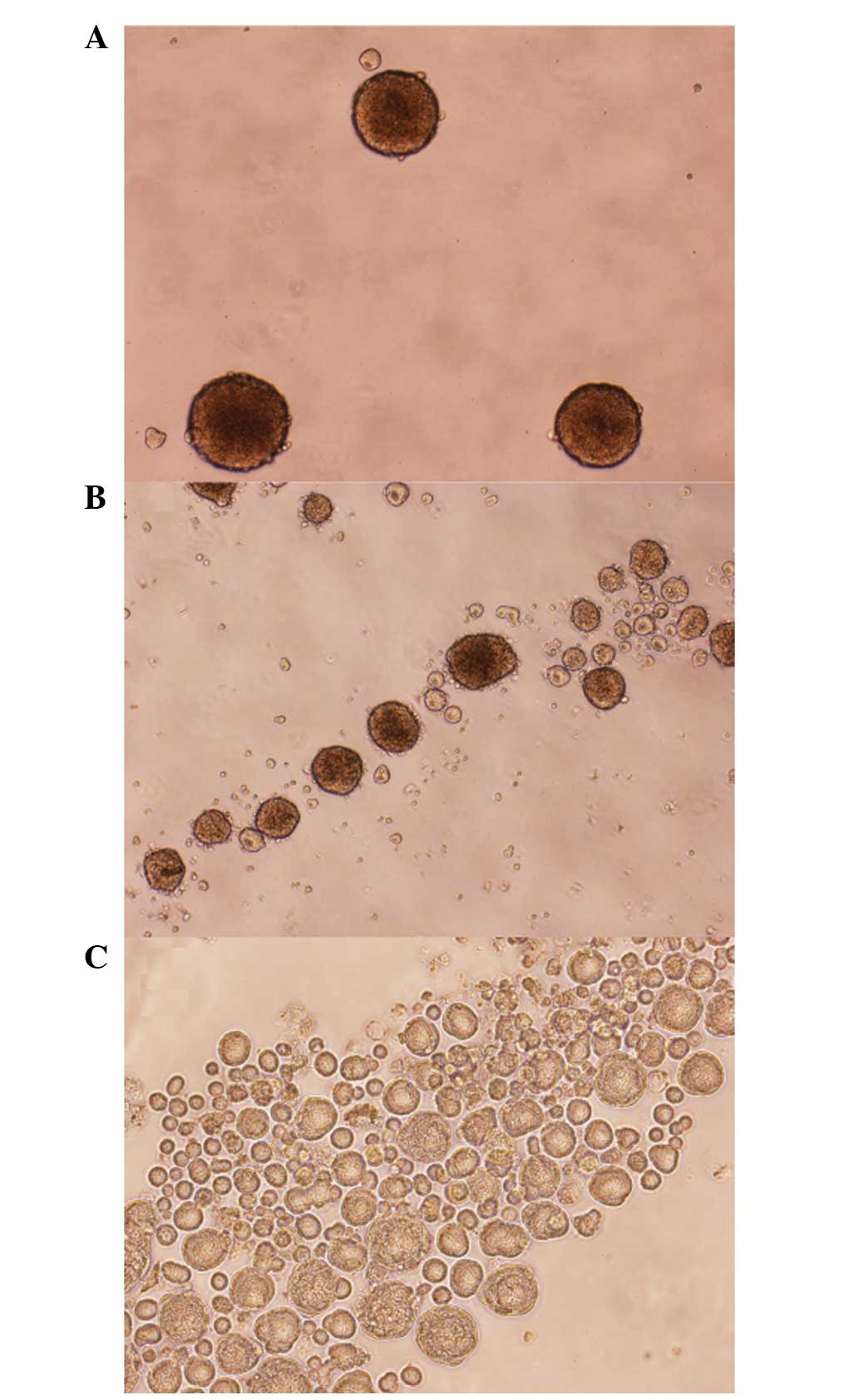
Spheroid cell growth
Culturing of the HNSCC SCC25, CAL27 and FaDu cell
lines according to the 3D protocol showed that all three cell lines
exhibit certain degrees of spheroid growth. The FaDu cells showed
the best cluster shape, cell-cell adherence and spheroid size
(Fig. 1A). The SCC25 cells grew in
denser and rounded clusters, whereas the CAL27 cells formed long
and loose clusters (Fig. 1B and
C).
Inhibitory concentrations of
cisplatin
To establish a 3D cytotoxicity assay, different cell
counts were seeded. After various incubation times (48 h for FaDu
cells; 72 h for CAL27 and SCC25 cells), the cells were submitted to
cisplatin treatment. The metabolic activity in the FaDu cell line
was strongest as it led to an intense change of color in the CCK-8
assay. While the SCC25 cells showed less enzymatic conversion, the
3D culture of the CAL27 cells did not lead to feasible results in
this assay. Hence, growth inhibition experiments were continued
with FaDu and SCC25 cell lines.
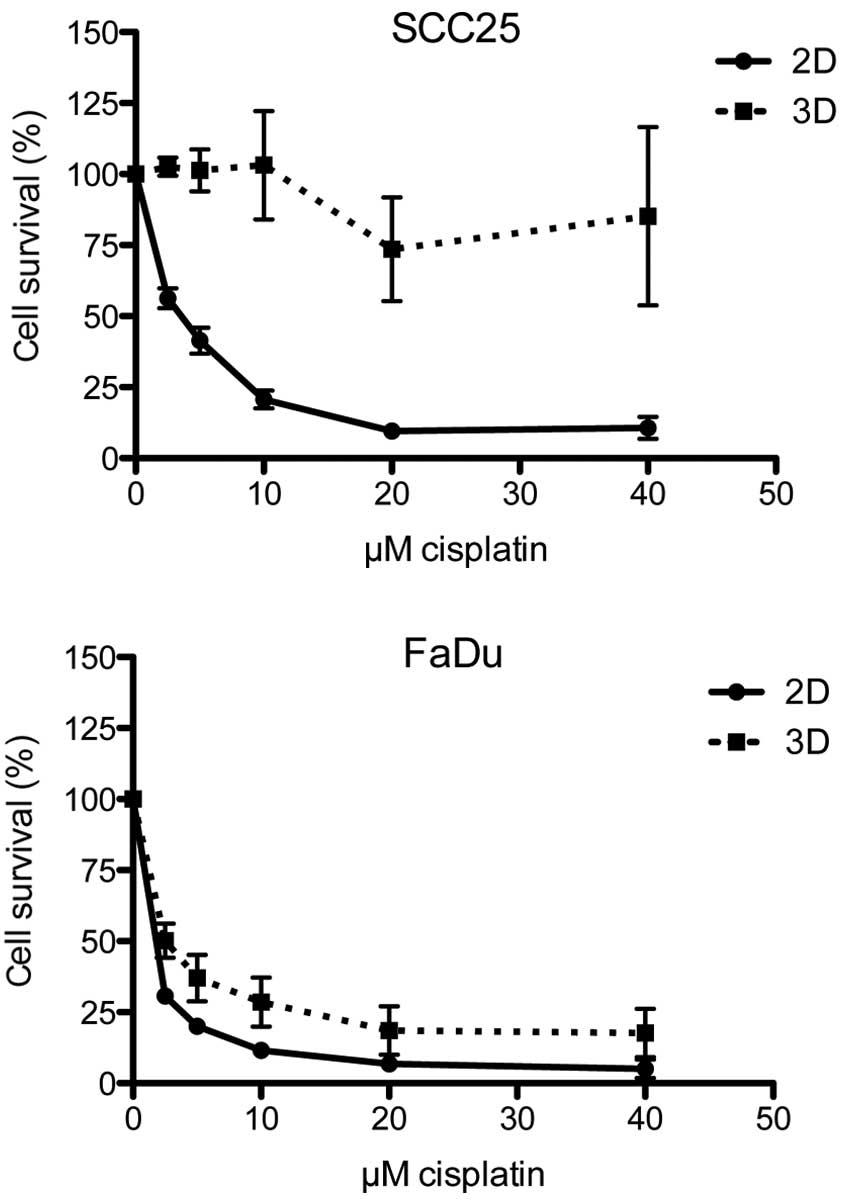
In the 2D cell model, the cells were incubated with
cisplatin concentrations ranging from 0–20 µM. In the two cell
lines, cisplatin led to strong growth inhibition, with a half
maximal inhibitory concentration (IC50) of 0.95 µM in
the FaDu cells and 3.26 µM in the SCC25 cells. By contrast, the
spheroids were less susceptible to cisplatin, with an
IC50 of 2.31 µM in the FaDu cells and 150.30 µM in the
SCC25 cells. Dose-response curves for each cell line and culture
model are shown in Fig. 2.
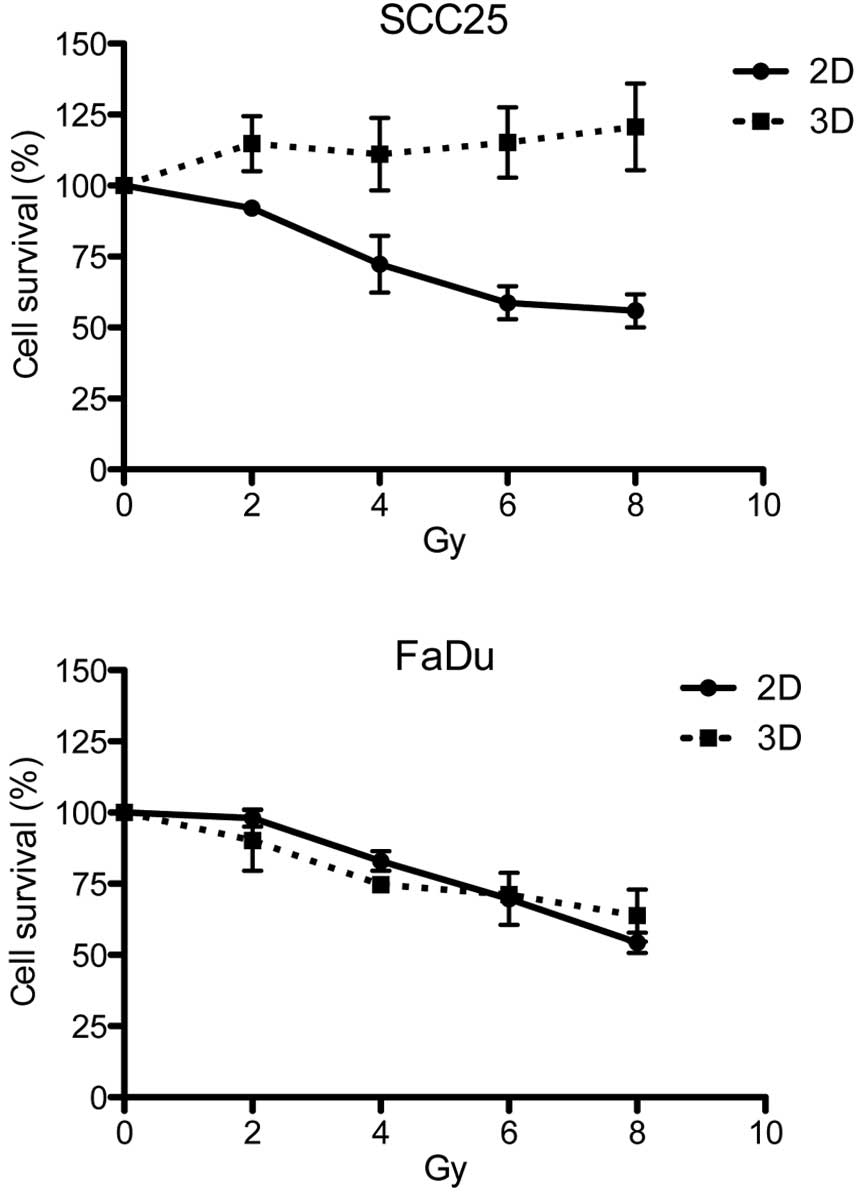
Response to radiation
The cells were exposed to increasing doses of
radiation (0–8 Gy). Dose-response curves are depicted in Fig. 3. In the FaDu cell line, a comparable
response to irradiation was observed in each cell model. However,
in the SCC25 cells, the 2D cell model was significantly more
susceptible to irradiation, since the spheroids showed no growth
inhibition even after 8 Gy in the 3D model.
Immunohistochemical staining
The cell culture models were compared with regard to
the expression of Ki-67, VEGFR, EGFR and survivin. Average
expression scores were calculated and a 2D:3D ratio was
established. Expression levels and ratios for all cell lines and
proteins are summarized in Table I.
With regard to Ki-67, moderate to strong staining was detected in
the 2D model in all three cell lines, and the average staining
score was three times higher than in the 3D cell model (P=0.0134).
Staining was observed in a high percentage of cells. By contrast,
only a few cells were stained with Ki-67 in the 3D model. The
majority of the Ki-67-expressing cells were located in the outer
third of a spheroid, solitary cells were observed in the
intermediary zone and no Ki-67 staining was observed in the
necrotic center (Fig. 4A and B).
 | Table I.Immunohistochemical analysis results
showing average protein expression levels for Ki-67, VEGFR, EGFR
and survivin in 2D and 3D cell models. |
Table I.
Immunohistochemical analysis results
showing average protein expression levels for Ki-67, VEGFR, EGFR
and survivin in 2D and 3D cell models.
| Parameter | SCC25 | CAL27 | FaDu | 2D:3D | P-value |
|---|
| Ki-67 |
|
|
|
|
|
| 2D | 2.7 | 2.5 | 2.3 | 3.2 | 0.0134 |
| 3D | 0.7 | 0.7 | 1.0 |
|
|
| VEGFR |
|
|
|
|
|
| 2D | 2.5 | 2.8 | 2.0 | 1.2 | 0.7289 |
| 3D | 3.0 | 1.5 | 1.5 |
|
|
| EGFR |
|
|
|
|
|
| 2D | 2.8 | 1.0 | 2.3 | 0.7 | 0.4460 |
| 3D | 3.0 | 3.0 | 2.8 |
|
|
| Survivin |
|
|
|
|
|
| 2D | 2.8 | 2.8 | 3.0 | 1.1 | 0.0595 |
| 3D | 2.6 | 2.6 | 3.0 |
|
|
The expression of VEGFR in the monolayer culture was
likewise ubiquitous, although FaDu showed less staining. In the
spheroids, VEGFR was expressed through all layers of the cell
cluster. In the CAL27 cells, lesser staining was observed in the 3D
cell model compared with the 2D model, whereas in the SCC25 and
FaDu cells an inverse staining pattern was assessed (Fig. 4C and D). In the CAL27 cells, only weak
staining of EGFR was observed in the monolayer model. However, in
the 3D culture, the CAL27 cells strongly expressed EGFR. In the
FaDu and SCC25 cells, moderate to high expression was observed
compared with high expression in the spheroids (Fig. 4E and F).
With regard to survivin, no differential expression
was observed in the 2D cell model compared with the 3D cell model
(Fig. 4G and H).
Discussion
The capability of spheroid cell culture to reflect
cancer biology more accurately in vitro has been described
in various studies (4,11,26,27).
Attempted explanations for the proximity of spheroid models to
in vivo tumors in terms of proliferation and therapy
response include cell heterogeneity and tumor microenvironment
(28) or different levels of drug and
oxygen diffusion (26).
To date, a certain number of studies on HNSCC
spheroids have been published (29–46) but
there is little knowledge on contraposing 2D to 3D cell cultures.
These previous studies have focused on novel drug treatments or
molecular expression patterns in 3D cell models. Therefore,
although there is a broad knowledge regarding 3D cell cultures in
HNSCC, a direct comparison between 2D and 3D cell cultures in HNSCC
remains to be investigated. Hence, the present study aimed to
establish a stable protocol for an HNSCC spheroid cell culture and
to compare important attributes between the conventional monolayer
and this spheroid cell culture. As expected from the previously
mentioned studies, all three HNSCC cell lines, SCC25, CAL27 and
FaDu, were able to grow in multicellular spheroids. Their growth
patterns, however, differed between the cell lines and CAL27 did
not exhibit reliable stability. Hence, this cell line was excluded
from the cytotoxicity assays.
The capability of spheroid cell culture to better
reflect cancer therapy resistance cultures has previously been
described in hepatocellular (5) and
colon (47) carcinoma. Since
cisplatin is the main chemotherapeutic drug in the treatment of
HNSCC, the present study exposed spheroids to cisplatin and
compared the results to a monolayer cell culture. For the first
time, a significant increase was observed in the IC50
dose in one cell line, while comparable results were shown by each
of the culture models in the other cell line. The site of origin
may serve as an explanation, since SCC25 is derived from a tongue
cancer and FaDu is from a hypopharyngeal tumor.
Since radiotherapy is a vital factor in HNSCC
therapy and radioresistance is a determinative problem, the
spheroids were irradiated. Notably, diverging growth inhibition was
observed in the cell lines. In the FaDu cells, surviving fractions
comparable to the monolayer cell culture were found, whereas in the
SCC25 cells, the spheroids were significantly less affected by
radiation than the monolayers.
Observations of resistance to irradiation have also
been described in glioma cells (48).
In the present study, an intermediate layer of hypoxia surrounding
the center of spheroids was described; therefore, irradiation had
less effect on spheroids. In addition, the protein expression of
Ki-67 was examined within the spheroids. As expected, staining was
concentrated at the periphery, since Ki-67 is considered as a
proliferation marker (22). VEGFR was
expressed throughout the whole spheroid. This finding is in
contrast to that of a study by Shweiki et al, which
described the weaker expression of VEGFR in the periphery of glial
rat tumor spheroids (49).
However, comparing the location of primary
expression in spheroids and the monolayer model is not possible,
since 2D cells are prepared prior to the staining process. However,
the staining intensity can be assessed and compared. In the present
study, a variation in staining intensity was noted for Ki-67, VEGFR
and EGFR, with partly stronger and partly weaker expression in the
spheroid cell model. Since VEGFR expression may result from hypoxia
and cellular stress (50), lower
expression was expected in the monolayer culture. However, only one
cell line (CAL27) exhibited this pattern. Likewise, a similar
expression pattern of EGFR was observed in the SCC25 and FaDu
cells, whereas the CAL27 cells showed stronger expression in the
spheroids. As for survivin, different staining intensities were
expected, as described in a previous study (51). However, no distinction was possible
between the spheroids and monolayer cells.
A spheroid cell culture was established from the
HNSCC cell lines in the present study. The study described their
response to cisplatin and radiotherapy for the first time. Despite
being of the same cell line, different protein expression
intensities and/or staining patterns were observed between
spheroids and monolayer cell cultures. Hence, growth in spheroids
alone alters the cellular pathways in the HNSCC cell lines. Thus,
spheroid cell culture may prove to be the more rational alternative
for cell culture due to the more physiological growth of the cells.
Limiting factors, however, are higher costs, more elaborate
maintenance and the impracticality of certain cell lines.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Myers EN: Head and neck oncology — 2010,
part II. Otolaryngol Pol. 64:204–214. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Carvalho AL, Nishimoto IN, Califano JA and
Kowalski LP: Trends in incidence and prognosis for head and neck
cancer in the United States: A site-specific analysis of the SEER
database. Int J Cancer. 114:806–816. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kimlin LC, Casagrande G and Virador VM:
In vitro three-dimensional (3D) models in cancer research:
An update. Mol Carcinog. 52:167–182. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bokhari M, Carnachan RJ, Cameron NR and
Przyborski SA: Culture of HepG2 liver cells on three dimensional
polystyrene scaffolds enhances cell structure and function during
toxicological challenge. J Anat. 211:567–576. 2007.PubMed/NCBI
|
|
6
|
Shain KH and Dalton WS: Cell adhesion is a
key determinant in de novo multidrug resistance (MDR): New targets
for the prevention of acquired MDR. Mol Cancer Ther. 1:69–78.
2001.PubMed/NCBI
|
|
7
|
Johnson JI, Decker S, Zaharevitz D,
Rubinstein LV, Venditti JM, Schepartz S, et al: Relationships
between drug activity in NCI preclinical in vitroin
vivo models and early clinical trials. Br J Cancer.
84:1424–1431. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Voskoglou-Nomikos T, Pater JL and Seymour
L: Clinical predictive value of the in vitro cell line,
human xenograft, and mouse allograft preclinical cancer models.
Clin Cancer Res. 9:4227–4239. 2003.PubMed/NCBI
|
|
9
|
Sutherland RM, McCredie JA and Inch WR:
Growth of multicell spheroids in tissue culture as a model of
nodular carcinomas. J Natl Cancer Inst. 46:113–120. 1971.PubMed/NCBI
|
|
10
|
Horning JL, Sahoo SK, Vijayaraghavalu S,
Dimitrijevic S, Vasir JK, Jain TK, et al: 3-D tumor model for in
vitro evaluation of anticancer drugs. Mol Pharm. 5:849–862.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Karlsson H, Fryknäs M, Larsson R and
Nygren P: Loss of cancer drug activity in colon cancer HCT-116
cells during spheroid formation in a new 3-D spheroid cell culture
system. Exp Cell Res. 318:1577–1585. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cordes N and Meineke V: Cell
adhesion-mediated radioresistance (CAM-RR). Extracellular
matrix-dependent improvement of cell survival in human tumor and
normal cells in vitro. Strahlenther Onkol. 179:337–344.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Khaitan D, Chandna S, Arya MB and
Dwarakanath BS: Establishment and characterization of multicellular
spheroids from a human glioma cell line; Implications for tumor
therapy. J Transl Med. 4:122006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lim Y, Keam B, Koh Y, Kim TM, Lee S-H, Hah
JH, et al: Clinical outcomes of radiation-based locoregional
therapy in locally advanced head and neck squamous cell carcinoma
patients not responding to induction chemotherapy. Oral Surg Oral
Med Oral Pathol Oral Radiol. 116:55–60. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vermorken JB and Specenier P: Optimal
treatment for recurrent/metastatic head and neck cancer. Ann Oncol.
21(Suppl 7): vii252–vii261. 2010.PubMed/NCBI
|
|
16
|
Ho AS, Tsao GJ, Chen FW, Shen T, Kaplan
MJ, Colevas AD, et al: Impact of positron emission
tomography/computed tomography surveillance at 12 and 24 months for
detecting head and neck cancer recurrence. Cancer. 119:1349–1356.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Eke I, Schneider L, Förster C, Zips D,
Kunz-Schughart LA and Cordes N: EGFR/JIP-4/JNK2 signaling
attenuates cetuximab-mediated radiosensitization of squamous cell
carcinoma cells. Cancer Res. 73:297–306. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Colley HE, Hearnden V, Avila-Olias M,
Cecchin D, Canton I, Madsen J, et al: Polymersome-mediated delivery
of combination anticancer therapy to head and neck cancer cells: 2D
and 3D in vitro evaluation. Mol Pharm. 11:1176–1188. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Eke I, Leonhardt F, Storch K, Hehlgans S
and Cordes N: The small molecule inhibitor QLT0267 Radiosensitizes
squamous cell carcinoma cells of the head and neck. PLoS One.
4:e64342009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kotowski U, Heiduschka G, Brunner M,
Czembirek C, Eder-Czembirek C, Schmidt R, et al: Radiosensitization
of head and neck cancer cells by the phytochemical agent
sulforaphane. Strahlenther Onkol. 187:575–580. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lill C, Schneider S, Pammer J, Loewe R,
Gedlicka W, Houben R, et al: Significant correlation of
peptidyl-prolyl isomerase overexpression in Merkel cell carcinoma
with overall survival of patients. Head Neck. 33:1294–1300. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xu W: CD133 and Ki-67 expression is
associated with gastrointestinal stromal tumor prognosis. Oncol
Lett. 6:1289–1294. 2013.PubMed/NCBI
|
|
23
|
Gildener-Leapman N, Ferris RL and Bauman
JE: Promising systemic immunotherapies in head and neck squamous
cell carcinoma. Oral Oncol. 49:1089–1096. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Erjala K, Sundvall M, Junttila TT, Zhang
N, Savisalo M, Mali P, et al: Signaling via ErbB2 and ErbB3
associates with resistance and epidermal growth factor receptor
(EGFR) amplification with sensitivity to EGFR inhibitor gefitinib
in head and neck squamous cell carcinoma cells. Clin Cancer Res.
12:4103–4111. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ye Q, Cai W, Zheng Y, Evers BM and She QB:
ERK and AKT signaling cooperate to translationally regulate
survivin expression for metastatic progression of colorectal
cancer. Oncogene. 33:1828–1839. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Desoize B, Gimonet D and Jardiller JC:
Cell culture as spheroids: An approach to multicellular resistance.
Anticancer Res. 18:4147–4158. 1998.PubMed/NCBI
|
|
27
|
Elliott NT and Yuan F: A review of
three-dimensional in vitro tissue models for drug discovery
and transport studies. J Pharm Sci. 100:59–74. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lee GY, Kenny PA, Lee EH and Bissell MJ:
Three-dimensional culture models of normal and malignant breast
epithelial cells. Nat Methods. 4:359–365. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ingargiola M, Runge R, Heldt J-M,
Freudenberg R, Steinbach J, Cordes N, et al: Potential of a
Cetuximab-based radioimmunotherapy combined with external
irradiation manifests in a 3-D cell assay. Int J Cancer.
135:968–980. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Rasanen K, Sriswasdi S, Valiga A, Tang
H-Y, Zhang G, Perego M, et al: Comparative secretome analysis of
epithelial and mesenchymal subpopulations of head and neck squamous
cell carcinoma identifies S100A4 as a potential therapeutic target.
Mol Cell Proteomics. 12:3778–3792. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yan M, Yang X, Wang L, Clark D, Zuo H, Ye
D, et al: Plasma membrane proteomics of tumor spheres identify
CD166 as a novel marker for cancer stem-like cells in head and neck
squamous cell carcinoma. Mol Cell Proteomics. 12:3271–3284. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Waldron NN, Barsky SH, Dougherty PR and
Vallera DA: A bispecific EpCAM/CD133-targeted toxin is effective
against carcinoma. Target Oncol. 9:239–249. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yang W-H, Lan H-Y, Tai S-K and Yang M-H:
Repression of bone morphogenetic protein 4 by let-7i attenuates
mesenchymal migration of head and neck cancer cells. Biochem
Biophys Res Commun. 433:24–30. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chang CC, Hsu WH, Wang CC, Chou CH, Kuo
MYP, Lin BR, et al: Connective tissue growth factor activates
pluripotency genes and mesenchymal-epithelial transition in head
and neck cancer cells. Cancer Res. 73:4147–4157. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Dennis M, Wang G, Luo J, Lin Y, Dohadwala
M, Abemayor E, et al: Snail controls the mesenchymal phenotype and
drives erlotinib resistance in oral epithelial and head and neck
squamous cell carcinoma cells. Otolaryngol Head Neck Surg.
147:726–732. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Duarte S, Loubat A, Momier D, Topi M,
Faneca H, Pedroso de Lima MC, et al: Isolation of head and neck
squamous carcinoma cancer stem-like cells in a syngeneic mouse
model and analysis of hypoxia effect. Oncol Rep. 28:1057–1062.
2012.PubMed/NCBI
|
|
37
|
Chen Y-S, Wu M-J, Huang C-Y, Lin S-C,
Chuang T-H, Yu C-C and Lo JF: CD133/Src axis mediates tumor
initiating property and epithelial-mesenchymal transition of head
and neck cancer. PLoS One. 6:e280532011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lim YC, Oh S-Y, Cha YY, Kim S-H, Jin X and
Kim H: Cancer stem cell traits in squamospheres derived from
primary head and neck squamous cell carcinomas. Oral Oncol.
47:83–91. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Krishnamurthy S, Dong Z, Vodopyanov D,
Imai A, Helman JI, Prince ME, et al: Endothelial cell-initiated
signaling promotes the survival and self-renewal of cancer stem
cells. Cancer Res. 70:9969–9978. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kross KW, Heimdal JH, Olsnes C, Olofsson J
and Aarstad HJ: Co-culture of head and neck squamous cell carcinoma
spheroids with autologous monocytes predicts prognosis. Scand J
Immunol. 67:392–399. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Harper LJ, Piper K, Common J, Fortune F
and Mackenzie IC: Stem cell patterns in cell lines derived from
head and neck squamous cell carcinoma. J Oral Pathol Med.
36:594–603. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Olsnes C, Heimdal J-H, Kross KW, Olofsson
J and Aarstad HJ: Viable head and neck tumor spheroids stimulate
in vitro autologous monocyte MCP-1 secretion through soluble
substances and CD14/lectin-like receptors. Eur Arch
Otorhinolaryngol. 262:953–960. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kross KW, Heimdal J-H, Olsnes C, Olofsson
J and Aarstad HJ: Head and neck squamous cell carcinoma spheroid-
and monocyte spheroid-stimulated IL-6 and monocyte chemotactic
protein-1 secretion are related to TNM stage, inflammatory state
and tumor macrophage density. Acta Otolaryngol. 125:1097–1104.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Heimdal JH, Olsnes C, Olofsson J and
Aarstad HJ: Monocyte and monocyte-derived macrophage secretion of
MCP-1 in co-culture with autologous malignant and benign control
fragment spheroids. Cancer Immunol Immunother. 50:300–306. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Heimdal JH, Aarstad HJ, Olsnes C and
Olofsson J: Human autologous monocytes and monocyte-derived
macrophages in co-culture with carcinoma F-spheroids secrete IL-6
by a non-CD14-dependent pathway. Scand J Immunol. 53:162–170. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Heimdal J, Aarstad HJ and Olofsson J:
Monocytes secrete interleukin-6 when co-cultured in vitro
with benign or malignant autologous fragment spheroids from
squamous cell carcinoma patients. Scand J Immunol. 51:271–278.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Fayad W, Brnjic S, Berglind D, Blixt S,
Shoshan MC, Berndtsson M, et al: Restriction of cisplatin induction
of acute apoptosis to a subpopulation of cells in a
three-dimensional carcinoma culture model. Int J Cancer.
125:2450–2455. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Sminia P, Acker H, Eikesdal HP, Kaaijk P,
Enger PØ, Slotman B and Bjerkvig R: Oxygenation and response to
irradiation of organotypic multicellular spheroids of human glioma.
Anticancer Res. 23:1461–1466. 2003.PubMed/NCBI
|
|
49
|
Shweiki D, Neeman M, Itin A and Keshet E:
Induction of vascular endothelial growth factor expression by
hypoxia and by glucose deficiency in multicell spheroids:
Implications for tumor angiogenesis. Proc Natl Acad Sci USA.
92:768–772. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Sivaraj KK, Takefuji M, Schmidt I, Adams
RH, Offermanns S and Wettschureck N: G13 controls angiogenesis
through regulation of VEGFR-2 expression. Dev Cell. 25:427–434.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Töyli M, Rosberg-Kulha L, Capra J,
Vuoristo J and Eskelinen S: Different responses in transformation
of MDCK cells in 2D and 3D culture by v-Src as revealed by
microarray techniques, RT-PCR and functional assays. Lab Invest.
90:915–928. 2010. View Article : Google Scholar : PubMed/NCBI
|