Introduction
Aromatase inhibitors have been widely administered
as adjuvant treatment for hormone receptor-positive breast cancer
in postmenopausal women. The results of recent clinical trials have
demonstrated that third-generation aromatase inhibitors, including
anastrozole, letrozole and exemestane, are more effective than
tamoxifen in treating early stage or metastatic breast cancer in
postmenopausal women (1). Thus,
aromatase inhibitors are now considered to be the gold standard of
endocrine therapy for such patients in adjuvant and metastatic
settings (2,3). Characterization of the risk of
recurrence for patients who receive aromatase inhibitors is
important for selecting appropriate treatment. However, factors
that can predict the outcomes of aromatase inhibitor treatment
remain unknown.
A number of studies have investigated tumor
biomarkers that indicated differential benefit from aromatase
inhibitors versus tamoxifen in patients with early breast cancer
(4–6).
Such biomarkers included the conventional factors, estrogen
receptor (ER), progesterone receptor (PgR), human epidermal growth
factor receptor type 2 (HER2) and Ki-67, and did not identify
patients who derived a differential relative benefit from aromatase
inhibitors over tamoxifen. Expression of the PgR gene is thought to
largely depend on an intact ER signaling pathway, and the
expression of PgR is associated with endocrine responsiveness
(7). Low PgR expression was found to
be associated with a poor prognosis in patients treated with
adjuvant tamoxifen therapy (8).
However, the prognostic significance of PgR in patients treated
with adjuvant aromatase inhibitors has remained unclear.
The risk of breast cancer risk among postmenopausal
women is positively associated with higher circulating
concentrations of estrogen. Obese women have higher circulating
estradiol levels as adipose tissue is an important source of
estrogens in postmenopausal women (9–11). As
obesity is associated with increased adipose tissue and aromatase
activity, aromatase inhibitors may be less effective in women who
are overweight or obese.
The ~15% of breast cancer patients with
overexpressed HER2 are treated with trastuzumab, a monoclonal
antibody targeting HER2, combined with adjuvant chemotherapy
(12). Conversely, the selection
criteria of adjuvant treatment in patients with the ER+/HER2-
subtype is particularly difficult to define. Patients who are at
high risk for recurrence need to be distinguished from those at low
risk, for whom adjuvant aromatase inhibitors may be sufficient
(4–6).
Based on this background, we postulated that
PgR/body mass index (BMI) status would affect the outcomes of
adjuvant aromatase inhibitor therapy in postmenopausal women, as
PgR is an endocrine-related tumor factor and BMI is an
endocrine-related factor. The aim of the current study was to
attempt to classify patients with ER+/HER2- breast cancer by
analyzing the associations between PgR/BMI status and
clinicopathological factors, including prognosis.
Patients and methods
Patients
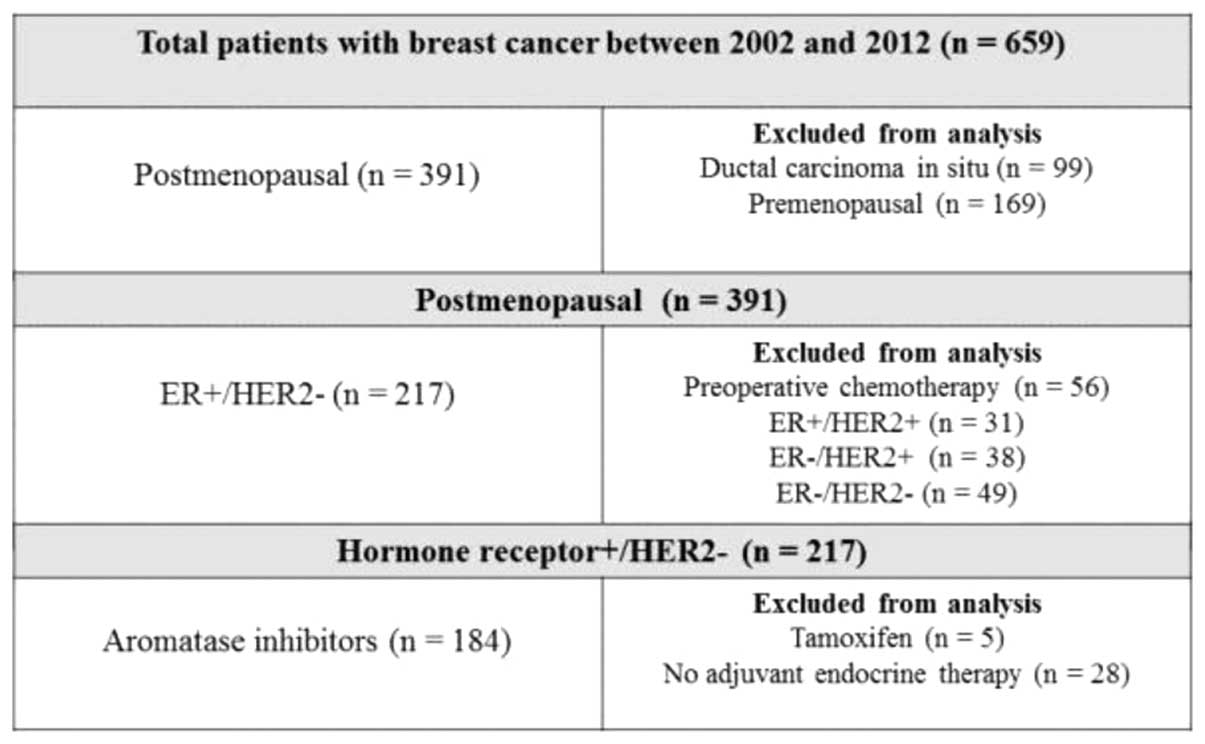
Between September 2002 and October 2012, 659
consecutive patients with primary breast cancer underwent curative
surgery at Hiroshima Prefectural Hospital. Among the 391
postmenopausal patients who had breast cancer while menopausal, 56
who had received preoperative chemotherapy and 118 who were either
ER- or HER2+ were excluded from the analysis. In addition, 5
patients who were treated with tamoxifen and 28 who did not undergo
endocrine therapy were also excluded. Finally, data derived from
184 postmenopausal patients with a median age of 64 years (range,
50–91 years) and with ER+/HER2- breast cancer treated with
aromatase inhibitors were analyzed (Fig.
1). Patients who were considered to be at high risk according
to prevalent breast cancer guidelines were administered with
chemotherapy (13–18). A total of 4 cycles of doxorubicin (60
mg/m2) and cyclophosphamide (600 mg/m2) every
3 weeks were administered. A total of 4 cycles of docetaxel (75
mg/m2) every 3 weeks were added if the nodal status was
positive. BMI was defined as weight (kg) divided by the square of
height in meters (kg/m2) at the time of primary breast
cancer surgery. The World Health Organization (WHO) cut-off value
was applied to assign the patients to high (≥25 kg/m2;
BMI-H) or low (≥25 kg/m2; BMI-H) BMI groups (19). The follow-up period (median, 46.1
months) ended on 31 July, 2013. Demographic and medical data,
including age, menopausal status, weight, height, type of breast
surgery and history of treatment for breast cancer and endocrine
therapy, were collected from medical charts. The institutional
review board of Hiroshima Prefectural Hospital approved the study
(no. H25-55) and waived the requirement for informed consent from
individual patients.
Clinicopathological factors
Clinicopathological factors were determined
according to the General Rules for Clinical and Pathological
Recording of Breast Cancer, 16th edition (20). Positive ER and PgR status was
determined by immunohistochemistry (IHC) and scored according to
the Allred system (21). Tumors were
defined as HER2+ when IHC scores were 3+ or HER2 amplification
ratios (HER2/CEP17) by fluorescence in situ hybridization
were >2.2. Ki-67 was detected by staining with a MIB1 antibody.
Different areas of densely stained lesions were selected under
microscopy and >500 cancer cells were assessed to determine
Ki-67 expression levels; values were expressed as the percentage of
positive cells in each case. Cases with a Ki-67 labeling index ≥20%
were defined as positive, whilst cases with an index <20% were
defined as negative (22). Briefly,
tumor specimens were stained using rabbit monoclonal anti-ER
antibody (SP1; 790–4324, Ventana Medical Systems, pre-diluted),
rabbit monoclonal anti-PgR antibody (1E2; 790–2223, Ventana Medical
Systems, pre-diluted), rabbit monoclonal anti-HER2 antibody (4B5;
790–2991, Ventana Medical Systems, pre-diluted), and mouse
monoclonal anti-Ki67 antibody (MIB-1; M7240, Dako, 1:80). IHC
staining was performed according to the ultraView Universal DAB
Detection Kit (760–500, Ventana Medical Systems) manufacturer's
instructions.
Follow-up evaluation
All patients were followed up from the day of
surgery. Follow-up care plans included clinical breast and regional
lymph node examinations by visual and touch inspection every 3
months and yearly mammograms. Recurrence was defined as any
unequivocal occurrence of new cancer foci in a hitherto
disease-free patient. The site of the first cancer recurrence and
the interval between surgery and recurrence were determined.
Recurrence-free intervals (RFI) were calculated as the amount of
elapsed time between the date of surgery and that of the first
confirmation of cancer recurrence or the last clinical contact
attesting to disease-free status.
Statistical analysis
Data are presented as number of patients (with
percentages) or as means, unless otherwise stated. Frequencies were
compared using the χ2 test for categorical variables,
and small samples were assessed using Fisher's exact test. The
duration of the RFI was determined using Kaplan-Meier analyses, and
differences in RFI were assessed using the log-rank test. Cox's
proportional hazards model was used for univariate and multivariate
analyses of prognostic values. Multivariate analyses included
variables determined to have P<0.05 in the univariate analyses;
P<0.05 was considered to indicate statistical significance in
all tests. Data were statistically analyzed using SPSS software
version 10.5 (SPSS Inc., Chicago, IL, USA) (23).
Results
Patient's characteristics
Table I shows the
clinicopathological characteristics of the 184 patients enrolled in
this study. Among these patients, the median age was 64 years
(range, 50–91 years), 130 patients (70.7%) had pT1 status, 40
(21.7%) had positive nodal status, and 89% of the tumors were
histopathologically diagnosed (by hematoxylin and eosin staining)
as invasive ductal carcinoma. Over 80% of the tumors were PgR+
(83.7%), the median Ki-67 labeling index was 16.3% (range,
0.0–60.0%) and 53 (28.8%) patients had received adjuvant
chemotherapy. Anastrozole treatment had been administered in 96
(52.2%) cases, whilst 84 (45.7%) patients had been treated with
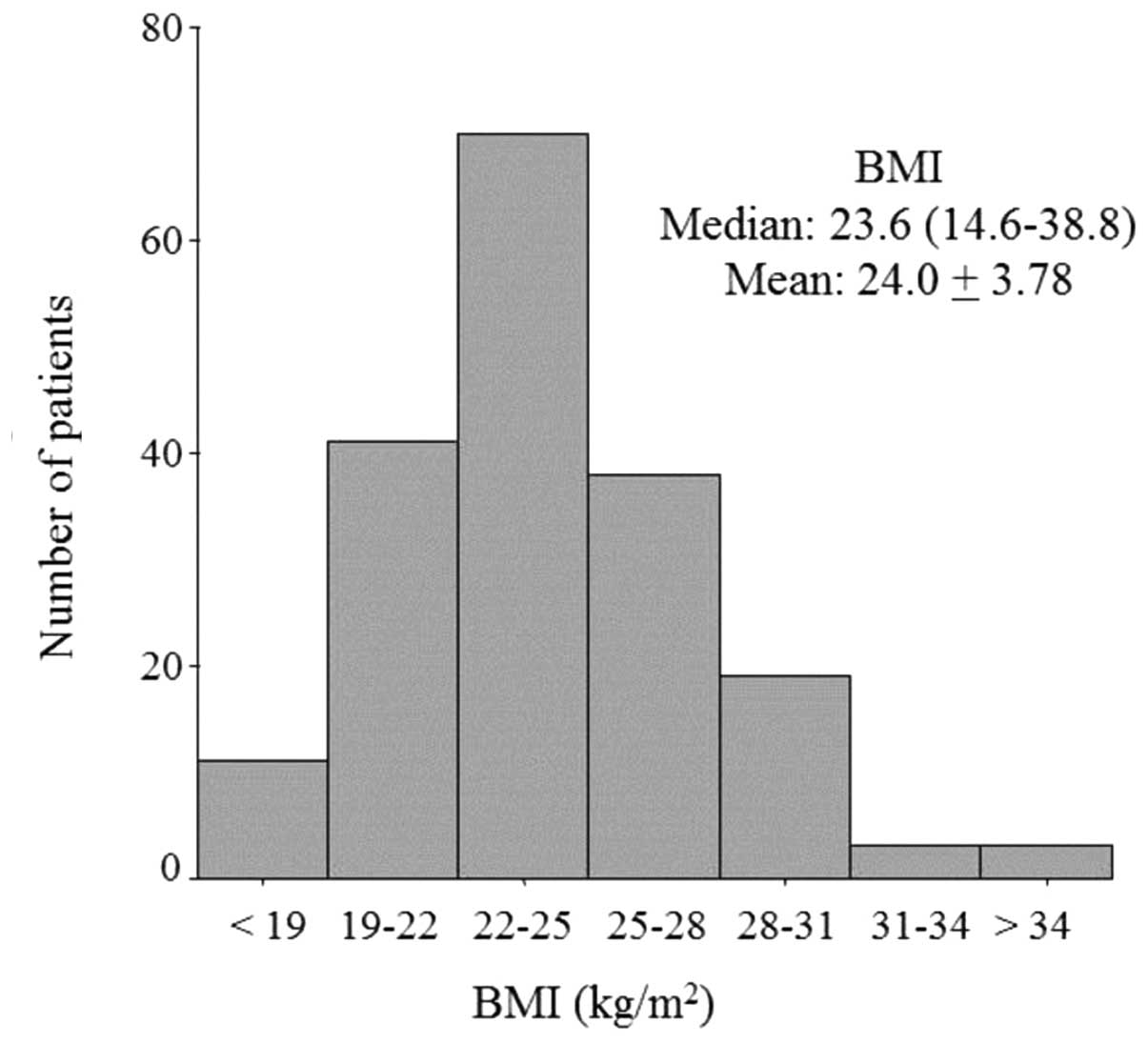
letrozole. Fig. 2 shows the
distribution of patients according to BMI (median, 23.6
kg/m2; range, 14.6–38.8 kg/m2). Two thirds of
these patients were underweight or of normal weight (n=120), and
one third was overweight (n=52) or obese (n=12) (Fig. 2).
 | Table I.Patient's characteristics (n=184). |
Table I.
Patient's characteristics (n=184).
| Variable | Value |
|---|
| Age, years; median
(range) | 64.0
(50–91) |
| Body mass index,
kg/m2; median (range) | 23.6 (14.6–38.8) |
| Histology, n (%) |
|
| Invasive
ductal carcinoma | 164
(89.1) |
| Invasive
lobular carcinoma |
4 (2.2) |
|
Other | 16
(8.7) |
| pT stage, n
(%) |
|
| T1 | 130
(70.7) |
| T2 | 49
(26.6) |
| T3 |
1 (0.5) |
| T4 |
4 (2.2) |
| Nodal status, n
(%) |
|
|
Negative | 144
(78.3) |
|
Positive | 40
(21.7) |
| Nuclear grade, n
(%) |
|
| I | 25
(13.6) |
| II | 132
(71.7) |
|
III | 22
(12.0) |
|
Unknown |
5 (2.7) |
| Lymphovascular
invasion, n (%) |
|
|
Negative | 30
(16.3) |
|
Positive | 154
(83.7) |
| Progesterone
receptor, n (%) |
|
|
Negative | 30
(16.3) |
|
Positive | 154
(83.7) |
| Ki-67 labeling
index, %; median (range) | 16.3
(0.3–60.0) |
| Type of surgery, n
(%) |
|
|
Breast-conserving surgery | 137
(74.5) |
|
Modified radical
mastectomy | 47
(25.5) |
| Endocrine therapy,
n (%) |
|
|
Anastrozole | 96
(52.2) |
|
Letrozole | 84
(45.7) |
|
Exemestane |
4 (2.1) |
| Chemotherapy, n
(%) |
|
|
Yes | 53
(28.8) |
| No | 131
(71.2) |
| Recurrence, n
(%) |
|
| Local
recurrence | 5
(2.7) |
| Distant
metastasis | 11
(6.0) |
Regression analyses of RFI
Breast cancer recurred in 16 patients during the
follow-up period. The variables included in the univariate analysis
of RFI in the 184 patients were BMI, tumor size, nodal status,
nuclear grade, lymphovascular invasion status, PgR status, Ki-67
labeling index and chemotherapy. A high BMI, positive nodal status,
negative PgR status and high Ki-67 labeling index were
significantly associated with a short RFI (P=0.048, 0.007, 0.027,
and 0.012, respectively).. Multivariate analysis, which included
BMI, nodal status, PgR status and Ki-67 labeling index, identified
positive nodal status as an independent prognostic factor for RFI
[hazard ratio, 3.27; 95% confidence interval, 1.20–8.90; P=0.020]
(Table II).
 | Table II.Univariate and multivariate analyses
of recurrence-free interval. |
Table II.
Univariate and multivariate analyses
of recurrence-free interval.
| A, Univariate
analysis |
|
|
|
|---|
|
|---|
| Variable | Value | HR (95% CI) | P-value |
|---|
| BMI | ≥25
kg/m2 | 2.71
(1.01–7.29) | 0.048 |
| T stage | T2/3/4 | 1.62
(0.60–4.35) | 0.349 |
| Nodal status | Positive | 3.84
(1.44–10.25) | 0.007 |
| Nuclear grade | III | 2.11
(0.60–7.48) | 0.248 |
| Lymphovascular
invasion | Positive | 26.9
(0.08–8837.97) | 0.265 |
| Progesterone
receptor status | Negative | 3.13
(1.13–8.65) | 0.027 |
| Ki-67 labeling
index | ≥20% | 4.24
(1.37–13.20) | 0.012 |
| Chemotherapy | Yes | 1.57
(0.5714.33) | 0.381 |
|
| B, Multivariate
analysis |
|
|
|
|
| Variable | Value | HR (95% CI) | P-value |
|
| BMI | ≥25
kg/m2 | 1.04
(0.90–1.19) | 0.610 |
| Nodal status | Positive | 3.27
(1.20–8.90) | 0.020 |
| Progesterone
receptor status | Negative | 2.62
(0.88–7.84) | 0.085 |
| Ki-67 labeling
index | ≥20% | 0.29
(0.83–9.33) | 0.097 |
Impact of PgR/BMI status on
clinicopathological factors and prognosis
Considering the mechanism of action of aromatase
inhibitors, the impact of PgR/BMI status on prognosis was analyzed.
A significantly shorter RFI was observed in patients with
PgR-negative tumors and/or BMI-H compared with that of PgR-positive
tumors and low BMI (PgR+/BMI-L; P=0.003) (Fig. 3).
Tumors were significantly larger and the Ki-67
labeling index was higher in the ‘unfavorable’ PgR- or BMI-H group,
than in the ‘favorable’ PgR+/BMI-L group (P=0.024 and <0.001,
respectively). Nodal status was not associated with the combined
PgR/BMI status (P=0.721; Table
III).
 | Table III.Clinicopathological implications of
combined PgR/BMI status in postmenopausal patients with ER+/HER2-
breast cancer. |
Table III.
Clinicopathological implications of
combined PgR/BMI status in postmenopausal patients with ER+/HER2-
breast cancer.
|
| PgR+/BMI-L | PgR- and/or
BMI-H |
|
|---|
| Variable | (n=98) | (n=86) | P-value |
|---|
| Age, years; mean ±
SD | 65.7±8.5 | 65.2±8.3 | 0.705 |
| T stage, n (%) |
|
| 0.024 |
| T1 | 76 (77.6) | 53 (61.6) |
|
|
T2,T3,T4 | 22 (22.4) | 33 (38.4) |
|
| Nodal status, n
(%) |
|
| 0.721 |
|
Negative | 78 (79.6) | 66 (76.7) |
|
|
Positive | 20 (20.4) | 20 (23.3) |
|
| Nuclear grade, n
(%) |
|
| 0.113 |
|
I/II | 87 (91.6) | 70 (83.3) |
|
III | 8
(8.4) | 14 (16.7) |
|
| Lymphovascular
invasion, n (%) |
|
| 0.239 |
|
Negative | 19 (19.4) | 11 (12.8) |
|
|
Positive | 79 (80.6) | 75 (87.2) |
|
| Ki-67 labeling
index,%; mean ± SD | 16.3±10.3 | 23.4±14.4 | <0.001 |
| Type of surgery, n
(%) |
|
| 0.503 |
|
Breast-conserving surgery | 75 (76.5) | 62 (72.1) |
|
|
Modified radical
mastectomy | 23 (23.5) | 24 (27.9) |
|
| Endocrine therapy,
n (%) |
|
|
|
|
Anastrozole | 53 (54.1) | 43 (50.0) | 0.649 |
|
Letrozole | 43 (43.9) | 41 (47.7) |
|
|
Exemestane | 2
(2.0) | 2
(2.4) |
|
| Chemotherapy, n
(%) |
|
| 0.516 |
|
Yes | 72 (73.5) | 59 (68.6) |
|
| No | 26 (26.5) | 86 (31.4) |
|
| Recurrence, n
(%) |
|
| 1.00 |
| Local
recurrence | 1
(33.3) | 4
(30.8) |
|
| Distant
recurrence | 2
(66.7) | 9
(69.2) |
|
Multivariate analysis of combined PgR/BMI status,
nodal status and the Ki-67 labeling index using the Cox
proportional hazards regression model identified PgR- or BMI-H and
positive nodal status as independent prognostic factors (P=0.012
and 0.020, respectively) (Table
IV).
 | Table IV.Univariate and multivariate analyses
of recurrence-free interval (combined PgR/BMI status). |
Table IV.
Univariate and multivariate analyses
of recurrence-free interval (combined PgR/BMI status).
| A, Univariate
analysis |
|
|
|
|---|
| Variable | Value | HR (95% CI) | P-value |
|
| PgR/BMI | PgR- and/or
BMI-H | 5.40
(1.54–18.91) | 0.009 |
|
| B, Multivariate
analysis |
|
|
|
|
| Variable | Value | HR (95% CI) | P-value |
|
| PgR/BMI | PgR- and/or
BMI-H | 5.07
(1.43–18.00) | 0.012 |
| Nodal status | Positive | 3.40
(1.22–9.52) | 0.020 |
| Ki-67 labeling
index | ≥20% | 1.28
(0.39–4.25) | 0.682 |
Discussion
The current study described a series of 184
postmenopausal patients with ER+ and HER2- breast cancer who were
treated with adjuvant aromatase inhibitor therapy. The results
reveal the importance of combining PgR status with BMI into a
single prognostic factor. To our knowledge, this is the first
report to demonstrate an association between PgR/BMI status and the
outcome of adjuvant aromatase inhibitor therapy for postmenopausal
patients with breast cancer.
Three randomized trials in the adjuvant setting of
postmenopausal breast cancer have examined the role of BMI in the
relative effectiveness of aromatase inhibitors vs. tamoxifen: The
Arimidex, Tamoxifen, Alone or in Combination (ATAC) trial (24); the Breast International Group (BIG)
1–98 trial (25); and the Tamoxifen
Exemestane Adjuvant Multinational (TEAM) trial (26). In the three trials, an aromatase
inhibitor was associated with improved outcomes compared with that
of tamoxifen at all BMI values. Notably, BMI did not significantly
interact with letrozole (vs. tamoxifen) in the BIG 1–98 trial
(25), whereas the ATAC investigators
concluded that the relative benefit of anastrozole (vs. tamoxifen)
may be more pronounced in women of a lower weight (24). These findings do not support the
notion that BMI can predict the benefit of aromatase inhibitors
(vs. tamoxifen) as adjuvant therapies in postmenopausal patients
with breast cancer (27). Sendur
et al (28) reported similar
findings from a retrospective analysis. The study showed that the
one- and three-year disease-free survival and three-year overall
survival rates following treatment with aromatase inhibitors were
similar among patients who were overweight, obese and of normal
weight. They concluded that BMI does not negatively impact the
outcomes of ER+ breast cancer in postmenopausal patients. The
current finding that BMI did not reach statistical significance for
RFI in multivariate analysis supported those of Sendur et al
(28).
A number of studies have identified an association
between levels of endogenous sex hormones and BMI in postmenopausal
women (29–31). The conversion of androstenedione to
estrone or estradiol by aromatase in adipose tissue is a major
source of estrogen in postmenopausal women (9–11). A high
BMI leads to elevated serum estradiol concentrations. The
association between plasma estrogen levels and BMI in
postmenopausal women with breast cancer treated with aromatase
inhibitors has also been investigated in numerous studies (32–35),
however, the results are inconsistent. Among them, the ALIQUOT
study (Anastrozole vs. Letrozole, an Investigation of Quality Of
Life and Tolerability) identified a relationship between poorly
suppressed levels of plasma estradiol and estrone sulfate and a
high BMI during treatment with aromatase inhibitors (36). Although the effects of BMI on clinical
outcomes and on estrogen levels in postmenopausal women with breast
cancer treated with aromatase inhibitors have not yet been
clarified, it is clear that a high BMI is not advantageous to the
outcome of such treatment.
Meanwhile, the molecular mechanisms of PgR remain
largely unknown. The PgR is synthesized by tumor cells following
stimulation by estrogens through interaction with the ER. The ER
pathway targets PgR, the presence of which reflects a functional ER
pathway (37,38). In theory, PgR may be a better
indicator of hormonal dependence. The St. Gallen international
expert consensus on primary therapy for early breast cancer 2013
has recently adopted PgR status to define more endocrine-sensitive
subgroups (17). The results of the
present study showed that PgR- and/or BMI-H when associated with a
high Ki-67 labeling index was an independent predictor of a poor
prognosis in addition to being a more significant predictor than
positive nodal status. Conversely, PgR+ tumors together with BMI-L
indicated highly sensitive endocrine tumors and low levels of
plasma estrogen, which may be a good indication for therapy with
aromatase inhibitors. Combined PgR/BMI status could thus
theoretically lead to better outcomes. However, this notion must be
addressed by evaluating aromatization and estrogen levels during
treatment in future studies.
The limitations of the present study include the
small sample cohort, the retrospective design, the single
institution and the short follow-up period. Furthermore, baseline
values composed the only available information about BMI, which did
not reflect weight changes during follow-up. Nonetheless, a clear
statistical difference was identified between PgR/BMI statuses. A
prospective analysis of PgR and BMI is required to assess its role
as a biomarker of outcomes among patients with ER+/HER2- breast
cancer.
In conclusion, the present retrospective analysis
demonstrated that PgR/BMI status may serve as a useful prognostic
factor in postmenopausal women with ER+ and HER2- breast cancer
treated with adjuvant aromatase inhibitors. PgR and BMI may be an
important consideration when customizing adjuvant treatment
strategies.
Abbreviations:
|
BMI
|
body mass index
|
|
CI
|
confidence interval
|
|
ER
|
estrogen receptor
|
|
HER2
|
human epidermal growth factor receptor
type 2
|
|
HR
|
hazard ratio
|
|
PgR
|
progesterone receptor
|
|
RFI
|
recurrence-free interval
|
References
|
1
|
Iwase H: Current topics and perspectives
on the use of aromatase inhibitors in the treatment of breast
cancer. Breast Cancer. 15:278–290. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Burstein HJ, Prestrud AA, Seidenfeld J,
Anderson H, Buchholz TA, Davidson NE, Gelmon KE, Giordano SH, Hudis
CA, Malin J, et al: American society of clinical oncology clinical
practice guideline: Update on adjuvant endocrine therapy for women
with hormone receptor-positive breast cancer. J Clin Oncol.
28:3784–3796. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cardoso F, Harbeck N, Fallowfield L,
Kyriakides S and Senkus E: ESMO Guidelines Working Group: Locally
recurrent or metastatic breast cancer: ESMO Clinical Practice
Guidelines for diagnosis, treatment and follow-up. Ann Oncol.
21(Suppl 7): vii11–vii19. 2012.
|
|
4
|
Dowsett M, Allred C, Knox J, Quinn E,
Salter J, Wale C, Cuzick J, Houghton J, Williams N, Mallon E, et
al: Relationship between quantitative estrogen and progesterone
receptor expression and human epidermal growth factor receptor 2
(HER-2) status with recurrence in the arimidex, tamoxifen, alone or
in combination trial. J Clin Oncol. 26:1059–1065. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Viale G, Regan MM, Dell'Orto P,
Mastropasqua MG, Maiorano E, Rasmussen BB, MacGrogan G, Forbes JF,
Paridaens RJ, Colleoni M, et al: Which patients benefit most from
adjuvant aromatase inhibitors? Results using a composite measure of
prognostic risk in the BIG 1–98 randomized trial. Ann Oncol.
22:2201–2207. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bartlett JM, Brookes CL, Robson T, van de
Velde CJ, Billingham LJ, Campbell FM, Grant M, Hasenburg A, Hille
ET, Kay C, et al: Estrogen receptor and progesterone receptor as
predictive biomarkers of response to endocrine therapy: A
prospectively powered pathology study in the tamoxifen and
exemestane adjuvant multinational trial. J Clin Oncol.
29:1531–1538. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Horwitz KB and McGuire WL: Oestrogen
control of progesterone receptor in human breast cancer:
correlation with nuclear processing of oestrogen receptor. J Biol
Chem. 253:2223–2228. 1978.PubMed/NCBI
|
|
8
|
Dowsett M, Houghton J, Iden C, Salter J,
Farndon J, A'Hern R, Sainsbury R and Baum M: Benefit from adjuvant
tamoxifen therapy in primary breast cancer patients according
oestrogen receptor, progesterone receptor, EGF receptor and HER2
status. Ann Oncol. 17:818–826. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yamashita H, Iwase H, Toyama T, Takahashi
S, Sugiura H, Yoshimoto N, Endo Y, Fujii Y and Kobayashi S:
Estrogen receptor-positive breast cancer in Japanese women: Trends
in incidence, characteristics and prognosis. Ann Oncol.
22:1318–1325. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Berclaz G, Li S, Price KN, Coates AS,
Castiglione-Gertsch M, Rudenstam CM, Holmberg SB, Lindtner J, Erien
D, Collins J, et al: Body mass index as a prognostic feature in
operable breast cancer: The international breast cancer study group
experience. Ann Oncol. 15:875–884. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Elliot KM, Dent J, Stanczyk FZ, Woodley L,
Coombes RC, Purohit A and Palmieri C: Effects of aromatase
inhibitors and body mass index on steroid hormone levels in women
with early and advanced breast cancer. Br J Surg. 101:939–948.
2014. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Slamon DJ, Leyland-Jones B, Shak S, Fuchs
H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M,
et al: Use of chemotherapy plus a monoclonal antibody against HER2
for metastatic breast cancer that overexpresses HER2. N Engl J Med.
344:783–792. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Goldhirsch A, Glick JH, Gelber RD, Coates
AS, Thürlimann B and Senn HJ: Panel members: Meeting highlights:
International expert consensus on the primary therapy of early
breast cancer 2005. Ann Oncol. 16:1569–1583. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goldhirsch A, Wood WC, Gelber RD, Coates
AS, Thürlimann B and Senn HJ: 10th St. Gallen conference: Progress
and promise: Highlights of the international expert consensus on
the primary therapy of early breast cancer 2007. Ann Oncol.
18:1133–1144. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Goldhirsch A, Ingle JN, Gelber RD, Coates
AS, Thürlimann B and Senn HJ: Panel members: Thresholds for
therapies: Highlights of the St Gallen international expert
consensus on the primary therapy of early breast cancer 2009. Ann
Oncol. 20:1319–1329. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Goldhirsch A, Wood WC, Coates AS, Gelber
RD, Thürlimann B and Senn HJ: Panel members: Strategies for
subtypes-dealing with the diversity of breast cancer: Highlights of
the St. Gallen International expert consensus on the primary
therapy of early breast cancer 2011. Ann Oncol. 22:1736–1747. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Goldhirsch A, Winer EP, Coates AS, Gelber
RD, Piccart-Gebhart M, Thürlimann B and Senn HJ: Panel members:
Personalizing the treatment of women with early breast cancer:
Highlights of the St Gallen international expert consensus on the
primary therapy of early breast cancer 2013. Ann Oncol.
24:2206–2223. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
National Comprehensive Cancer Network:
NCCN Guidelines - Breast Cancer. http://www.nccn.org/professionals/physician_gls/f_guidelines.aspAccessed.
April 1st–2012
|
|
19
|
WHO Expert Consultation: Appropriate
body-mass index for Asian populations and its implications for
policy and intervention strategies. Lancet. 363:157–163. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
The Japanese Breast Cancer Society:
General rules for clinical and pathological recording of breast
cancer (16th). Kanehara, Tokyo: 2008.
|
|
21
|
Allred DC, Harvey JM, Berardo M and Clark
GM: Prognostic and predictive factors in breast cancer by
immunohistochemical analysis. Mod Pathol. 11:155–168.
1998.PubMed/NCBI
|
|
22
|
Kai K, Nishimura R, Arima N, Miyayama H
and Iwase H: p53 expression status is a significant molecular
marker in predicting the time to endocrine therapy failure in
recurrent breast cancer: A cohort study. Int J Clin Oncol.
11:426–433. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ohara M, Shigematsu H, Tsutani Y, Emi A,
Masumoto N, Ozaki S, Kadoya T and Okada M: Role of FDG-PET/CT in
evaluating surgical outcomes of operable breast cancer-usefulness
for malignant grade of triple-negative breast cancer. Breast.
22:958–963. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sestak I, Distler W, Forbes JF, Dowsett M,
Howell A and Cuzick J: Effect of body mass index on recurrences in
tamoxifen and anastrozole treated women: An exploratory analysis
from the ATAC trial. J Clin Oncol. 28:3411–3415. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ewertz M, Gray KP, Regan MM, Ejlertsen B,
Price KN, Thürlimann B, Bonnefoi H, Forbes JF, Paridaens RJ,
Rabaglio M, et al: Obesity and risk of recurrence or death after
adjuvant endocrine therapy with letrozole or tamoxifen in the
breast international group 1–98 trial. J Clin Oncol. 30:3967–3975.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Seynaeve C, Hille E, Hasenburg A, Rea D,
Markopoulos C, Hozumi Y, Putter H, Nortier H, van Nes J, Dirix L
and van de Velde C: Impact of body mass index (BMI) on the efficacy
of adjuvant endocrine therapy in postmenopausal hormone sensitive
breast cancer (BC) patients; Exploratory analysis from the TEAM
study. Cancer Res. 70:Abstract S2–S3. 2010. View Article : Google Scholar
|
|
27
|
Goodwin PJ: Obesity and endocrine therapy:
Host factors and breast cancer outcome. Breast. 22(Suppl 2):
S44–S47. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sendur MA, Aksoy S, Zengin N and Altundag
K: Efficacy of adjuvant aromatase inhibitor in hormone
receptor-positive postmenopausal breast cancer patients according
to the body mass index. Br J Cancer. 107:1815–1819. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hankinson SE, Willett WC, Manson JE,
Hunter DJ, Colditz GA, Stampfer MJ, Longcope C and Speizer FE:
Alcohol, height and adiposity in relation to estrogen and prolactin
levels in postmenopausal women. J Natl Cancer Inst. 87:1297–1302.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Mahabir S, Baer DJ, Johnson LL, Hartman
TJ, Dorgan JF, Campbell WS, Clevidence BA and Taylor PR: Usefulness
of body mass index as a sufficient adiposity measurement for sex
hormone concentration associations in postmenopausal women. Cancer
Epidemiol Biomarkers Prev. 15:2502–2507. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
McTiernan A, Rajan KB, Tworoger SS, Irwin
M, Bernstein L, Baumgartner R, Gilliland F, Stanczyk FZ, Yasui Y
and Ballard-Barbash R: Adiposity and sex hormones in postmenopausal
breast cancer survivors. J Clin Oncol. 21:1961–1966. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Folkerd EJ, Dixon JM, Renshaw L, A'Hern RP
and Dowsett M: Suppression of plasma estrogen levels by letrozole
and anastrozole is related to body mass index in patients with
breast cancer. J Clin Oncol. 30:2977–2980. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Pfeiler G, Königsberg R, Hadji P, Fitzal
F, Maroske M, Dressel-Ban G, Zellinger J, Exner R, Seifert M,
Singer C, et al: Impact of body mass index on estradiol depletion
by aromatase inhibitors in postmenopausal women with early breast
cancer. Br J Cancer. 109:1522–1527. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sini V, Lunardi G, Cirillo M, Turazza M,
Bighin C, Giraudi S, Levaggi A, Piccioli P, Bisagni G, Gnoni R, et
al: Body mass index and circulating oestrone sulphate in women
treated with adjuvant letrozole. Br J Cancer. 110:1133–1138. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lønning PE, Haynes BP and Dowsett M:
Relationship of body mass index with aromatisation and plasma and
tissue oestrogen levels in postmenopausal breast cancer patients
treated with aromatase inhibitors. Eur J Cancer. 50:1055–1064.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Folkerd EJ, Dixon JM, Renshaw L, A'Hern RP
and Dowsett M: Suppression of plasma estrogen levels by letrozole
and anastrozole is related to body mass index in patients with
breast cancer. J Clin Oncol. 30:2977–2988. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Arafah BM, Finegan HM, Roe J, Manni A and
Pearson OH: Hormone dependency in N-nitrosomethylurea-induced rat
mammary tumors. Endocrinology. 111:584–588. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Brisken C: Progesterone signalling in
breast cancer: A neglected hormone coming into the limelight. Nat
Rev Cancer. 13:385–396. 2013. View
Article : Google Scholar : PubMed/NCBI
|