Introduction
A thyroglossal duct cyst (TGDC) is a common
congenital anomaly that primarily consists of benign lesions
(1). Carcinoma arising from a TGDC is
rare, accounting for ~1% of all TGDC cases (2). TGDC associated with carcinoma typically
presents as a painless mass in the mid-neck (2). It is often difficult to differentiate
TGDC carcinoma from other diseases based on clinical presentation
alone; thus, pathological analysis is required for an accurate
diagnosis. The most common subtype of carcinoma arising from a TGDC
is papillary carcinoma, followed by the less prevalent squamous
cell carcinoma (2). TGDC associated
with adenosquamous carcinoma is extremely rare, and only one case
has been reported in literature to date (3). The current case describes a patient with
adenosquamous carcinoma arising in a TGDC, which presented as a
lateral neck mass, and is followed by a discussion of the diagnosis
and subsequent management of the disease.
Case report
A 77-year-old man presented to the Department of
Otolaryngology of Kaohsiung Veterans General Hospital (Kaohsiung,
Taiwan) with a large mass in the left mid-neck. The patient visited
a regional hospital 2 months prior to admission due to hoarseness.
On physical examination, a painless neck mass was detected
incidentally, and the patient was subsequently referred to the
Department of Otolaryngology of Kaohsiung Veterans General
Hospital.
Physical examination identified a soft, ballotable,
mobile mass that measured ~5×6 cm in size. A fiberoptic endoscopy
was performed, but no lesion was observed in the upper
aerodigestive tract, except for one small polyp-like lesion in the
anterior third of the right vocal cord. Fine-needle aspiration
(FNA) was performed on the neck mass, and ~30 ml of aspirated brown
fluid was sent for cytology. A large number of histiocytes were
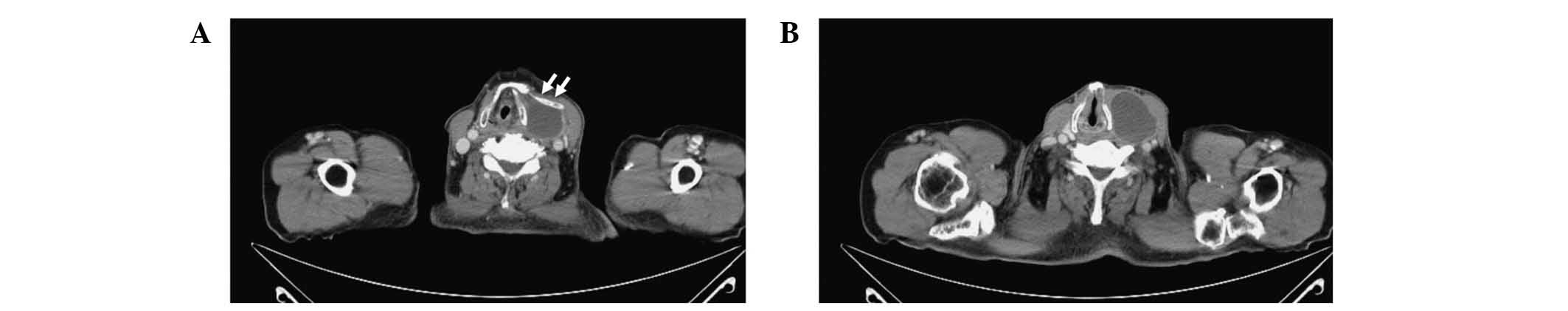
reported, without any presence of malignant cells. Computed
tomography (CT; Brilliance 64 Slice CT; Philips, Amsterdam,
Netherlands) demonstrated a cystic lesion of 41×34 mm in size,
which was located in the left lobe of the thyroid gland (Fig. 1), thus a thyroid cyst was suspected.
An additional hyoid bone, which was adjacent to the upper side of
the cystic lesion, was also identified by CT.
The patient was admitted to the hospital, and
initially underwent microscopic laryngeal surgery to remove the
right vocal polyp. The vocal lesion showed edema, proliferation of
fibroblasts, hyalinization of stroma and dilated blood vessels in
the lamina propia. The vocal lesion was covered with an intact
squamous epithelium and had no evidence of neoplasia. Therefore,
vocal polyp was diagnosed.
A subtotal thyroidectomy of the left lobe of the
thyroid gland was performed 1 week later. During surgery, it was
observed that the cystic lesion was separated from the left lobe of
the thyroid gland. The lesion had clear margins to the surrounding
tissues, however, the upper side of the cyst was adhered to the
additional hyoid bone. Therefore, the cyst and the additional hyoid
bone were completely removed. There were a small number of dark,
firm lymph nodes, with the largest one (measuring 1.3 cm in size)
located in the left levels II and III of the neck. Frozen section
analysis of the lymph nodes revealed reactive hyperplasia. Briefly,
tissues were embedded in optimal cutting temperature compound
(Shandon Cryomatrix; Thermo Fisher Scientific Inc., Waltham, MA,
USA) and frozen rapidly. They were sectioned with a thickness of 5
µm using a HM400 microtome (Microm UK Ltd., Bicester, UK) and
stained with hematoxylin and eosin (Scharlab SL, Barcelona, Spain).
Microscopic examination revealed enlarged lymph nodes with
hyperplasia of germinal centers, polymorphous follicles and intact
mantle zones. Reactive hyperplasia was diagnosed accordingly.
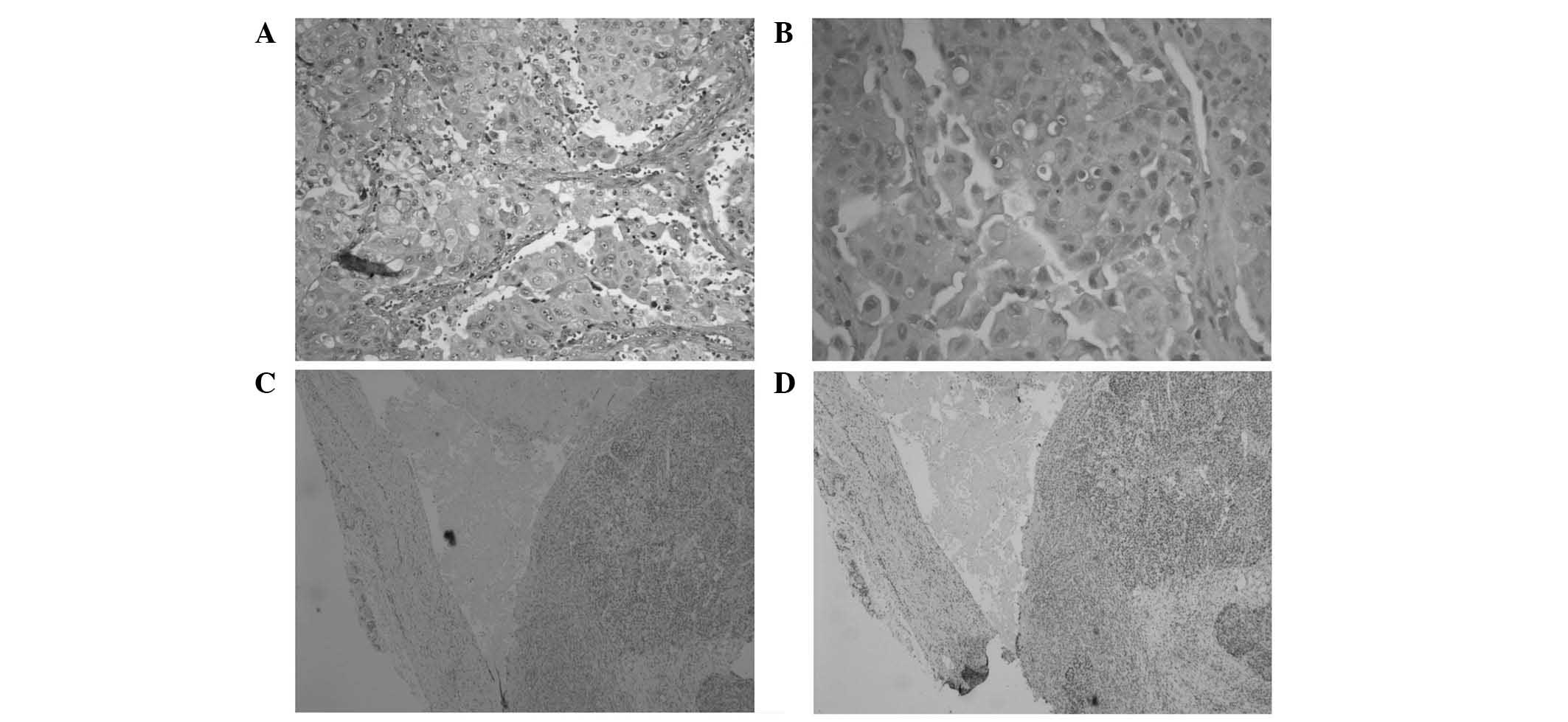
Gross examination of the cyst detected a high
content of a brown fluid. Microscopically (Eclipse 50i; Nikon
Corporation, Tokyo, Japan), the cyst was lined by squamous and
respiratory epithelium. Poorly-differentiated, neoplastic squamous
cells were identified in a glandular formation, which displayed
hyperchromatic and pleomorphic nuclei (Fig. 2). Mucin secretion was identified by
mucicarmine histochemical staining. Briefly, the tissues were fixed
in buffered formalin (Tonyar Biotech, Inc., Taoyuan, Taiwan) and
then embedded in paraffin (Leica Biosystems, Wetzlar, Germany).
They were sectioned with the thickness of 4 µm and stained with
hematoxylin and eosin stain (Scharlab SL). Immunostaining was
performed for paired box 8 (PAX-8; clone, ZR-1; rabbit anti-human
monoclonal antibody; dilution, 1:50; catalog no., Z2202; Zeta
Corporation, Arcadia, CA, USA) and thyroid transcription factor-1
(TTF-1; clone, SPT24; mouse anti-human monoclonal antibody;
dilution, 1:200; catalog no., TTF-1-L-CE; Novocastra; Leica
Microsystems GmbH, Wetzlar, Germany). The tumor cells were negative
for PAX-8 and TTF-1 immunostaining.
Based on the aforementioned analyses, the final
diagnosis was confirmed as adenosquamous carcinoma arising from a
TGDC. Due to the old age of the patient and the large size of the
tumor, a total thyroidectomy was performed 3 weeks following the
first operation. Pathologically, no synchronous neoplastic lesion
was detected in the thyroid gland. The patient was subsequently
discharged and was followed-up every 2 weeks during the first 2
months and then every 2 months. The patient remains alive without
signs of recurrence.
Discussion
TGDC develops when the tract that forms during the
descent of the primordial thyroid gland fails to undergo involution
(2). This disease is the most common
anomaly of thyroid gland development, with an estimated prevalence
of ~7% (1). The majority of TGDCs are
benign. Carcinoma arising from a TGDC is uncommon, and occurs in
~1% of all TGDC cases (2). Papillary
carcinoma is the most common carcinoma to arise from a TGDC, with
an incidence of ~80% of TGDC cases, whilst squamous cell carcinoma
is less common, with an incidence of 6% of all TGDC carcinoma cases
(2). Adenosquamous carcinoma
associated with a TGDC is extremely rare, with only one case
currently reported in the literature (3).
The clinical presentation of TGDC is typically a
mobile, painless neck swelling in the midline (4). However, the patient of the current case
presented with an asymptomatic neck mass in the lateral neck, which
is an atypical location for TGDC. Furthermore, the lesion occurred
in proximity to the additional hyoid bone. The symptoms associated
with TGDC carcinoma are similar to the those exhibited by a benign
TGDC (2). Suspicions of malignancy
should be raised if the lesion is hard, fixed, irregular or has
undergone recent change (5). However,
carcinoma of a TGDC often lacks the aforementioned features, and
prior to surgery, it is generally difficult to differentiate such a
lesion from a benign TGDC (2). If a
reliable diagnosis of TGDC carcinoma can be made preoperatively, a
more appropriate surgical intervention may be planned (3). Thus, FNA is considered to be important
for preoperative assessment of TGDC (6). However, the present case did not exhibit
malignant features, and FNA did not detect any malignant cells,
with the final diagnosis being confirmed during pathology.
The treatment of carcinoma arising from a TGDC
primarily depends on surgery. The Sistrunk procedure is considered
to be adequate for the majority of patients with a clinically and
radiologically normal thyroid gland (7). Synchronous neoplastic lesions in the
thyroid gland were identified in ~30% of TGDC carcinoma patients
(7). Patel et al (7) suggests that a total thyroidectomy and
Sistrunk procedure should be reserved for patients older than 45
years, with a tumor size of >4 cm, soft tissue extension or with
nodal or distant metastasis. Squamous cell carcinoma arising from a
TGDC is rare, and is associated with a poor prognosis. Only 24
cases of squamous cell carcinoma arising from a TGDC have currently
been reported in the literature (Table
I) (5,6,8–29). The median age at presentation is 57.2
years, and the male-to-female ratio is 13/9. The majority of these
cases were treated with wide local excision and postoperative
radiotherapy. A total of 15 cases reported no evidence of
recurrence during follow-up, and 4 cases succumbed to the disease,
not including Lustmann et al (19), who succumbed to pneumonia. Local
recurrence is common, and was previously reported to occur up to 13
years following the initial treatment (10,30).
Therefore, Hanna (30) suggested that
wide excision should be performed on localized lesions, and
postoperative radiotherapy should be performed on lesions that are
larger in size, present extensive nodal disease or exhibit positive
surgical margins. To the best of our knowledge, the present case is
the second reported case of adenosquamous carcinoma arising from a
TGDC. A consensus for the management of this disease has not yet
been established, primarily due to the limited available data. A
previous study reported that adenosquamous carcinoma of the thyroid
gland behaves in a similar aggressive manner to that of anaplastic
carcinoma (31). Therefore, it is
assumed that patients with TGDC adenosquamous carcinoma may
experience a poor prognosis and high local recurrence rate. Due to
the old age of the patient and the large tumor size, a more
aggressive treatment plan, including the Sistrunk procedure and
radical thyroidectomy, was selected for the present case. Pathology
demonstrated a clear surgical margin and no malignancy in the
thyroid gland or sampled lymph nodes. Therefore, no further
treatment was required, with the patient undergoing long-term
follow-up alone. Further observation of the clinical course and
nature of such tumors is necessary for the improvement of available
treatment.
 | Table I.Cases of squamous cell carcinoma
arising from a thyroglossal duct cyst. |
Table I.
Cases of squamous cell carcinoma
arising from a thyroglossal duct cyst.
| Author, year | Age,
years/gender | Therapy | Follow-up | Prognosis | Refs. |
|---|
| Ferrer et al,
2000 | 49/M | Surgery and adjuvant
radiotherapy | 52 months | NED at 52 months | (5) |
| Ranieri et al,
1996 | 68/M | Surgery and adjuvant
radiotherapy | 22 months | NED at 22 months | (6) |
| Clute and Smith,
1929 | 56/M | Surgery and adjuvant
radiotherapy | 15 months | Succumbed at 15
months | (8) |
| Nachlas, 1950 | NA | Surgery | NA | NA | (9) |
| Dalgaard and
Wetteland, 1956 | 44/F | Surgery | 28 years | Local recurrence 13
years post-surgery, NED 15 years after second surgery | (10) |
| Ruppmann and
Georgsson, 1966 | 51/F | Surgery | NA | Local recurrence, NED
1 year after last surgery | (11) |
| Shepard and
Rosenfeld, 1968 | 28/F | Surgery and adjuvant
radiotherapy | 4 years | Local recurrence,
succumbed at 4 years | (12) |
| Mobini et al,
1974 | 50/F | Surgery and adjuvant
radiotherapy | 2 years | NED at 2 years | (13) |
| Saharia, 1975 | 81/F | Surgery | 3 years | NED at 3 years | (14) |
| Benveniste et
al, 1980 | 75/M | Surgery and adjuvant
radiotherapy | 7 months | NED at 7 months | (15) |
| White and Talbert,
1982 | 61/M | Surgery | NA | NED | (16) |
| Ronan et al,
1986 | 19/F | Surgery | NA | NA | (17) |
| Bosch et al,
1986 | 54/M | Surgery and adjuvant
radiotherapy | 7 months | Local recurrence,
succumbed at 7 months | (18) |
| Lustmann et
al, 1989 | 80/F | Surgery and adjuvant
radiotherapy | 6 months | Local recurrence,
succumbed to pneumonia | (19) |
| Colloby et al,
1989 | 67/M | Surgery | 6 months | NED at 6 months | (20) |
| Yanagisawa et
al, 1992 | 65/M | Surgery and adjuvant
radiotherapy | 18 months | NED at 18 months | (21) |
| Virno et al,
1993 | 68/M | Surgery and adjuvant
radiotherapy | 1 year | NED at 1 year | (22) |
| Boswell et al,
1994 | 65/F | Surgery | 11 years | NED at 11 years | (23) |
| Bardales et
al, 1996 | 50/M | Surgery and adjuvant
radiotherapy | 36 months | NED at 36 months | (24) |
| Kwan et al,
1996 | 38/M | Surgery and adjuvant
radiotherapy | 3 years | NED at 3 years | (25) |
| Hama et al,
1997 | 57/M | Neoadjuvant
radiotherapy and surgery | 7 years | NED at 7 years | (26) |
| El Bakkouri et
al, 2004 | 55/F | Incomplete
operation due to carotid artery and larynx involvement, adjuvant
radiotherapy and palliative chemotherapy | 2 years | Local
progression | (27) |
| Iakovou et
al, 2011 | 78/M | Surgery | NA | NA | (28) |
| Yü et al,
2012 | NA | Surgery | 7 months | Recurrence at 2
months, succumbed at 7 months | (29) |
In conclusion, the current study described a rare
case of adenosquamous carcinoma arising from a TGDC, which
presented as a painless lateral neck mass. The patient lacked
clinical features that would indicate a malignant lesion, including
a hard, fixed or rapidly growing mass. The diagnosis of this
disease is primarily based on pathological findings, resulting in a
challenging preoperative planning of adequate surgery. The
preferred treatment for TGDC carcinoma is the Sistrunk procedure,
whilst other available treatment options include postoperative
radiotherapy or a total thyroidectomy (7). Local recurrence of the disease has been
reported to occur numerous years following initial treatment;
therefore, long-term follow-up is necessary.
The present case showed that the presentation of
TGDC adenosquamous carcinoma may be variable and challenging to
diagnose by preoperative imaging or fine-needle aspiration
cytology. The tumor had distinct margins, which made made the
complete resection by the Sistrunk procedure possible. Further
studies are required to delineate the long-term prognosis and best
treatment strategies for TGDC.
References
|
1
|
Ellis PD and van Nostrand AW: The applied
anatomy of thyroglossal tract remnants. Laryngoscope. 87:765–770.
1977. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Motamed M and McGlashan JA: Thyroglossal
duct carcinoma. Curr Opin Otolaryngol Head Neck Surg. 12:106–109.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kinoshita N, Abe K, Sainoo Y, Kumagami H,
Takahashi H and Hayashi T: Adenosquamous carcinoma arising in a
thyroglossal duct cyst: Report of a case. Surg Today. 41:533–536.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mondin V, Ferlito A, Muzzi E, Silver CE,
Fagan JJ, Devaney KO and Rinaldo A: Thyroglossal duct cyst:
Personal experience and literature review. Auris Nasus Larynx.
35:11–25. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ferrer C, Ferrández A, Dualde D, Rodriguez
M, Ferrer E, Pinazo J and Sancho R: Squamous cell carcinoma of the
thyroglossal duct cyst: Report of a new case and literature review.
J Otolaryngol. 29:311–314. 2000.PubMed/NCBI
|
|
6
|
Ranieri E, D'Andrea MR and Vecchione A:
Fine needle aspiration cytology of squamous cell carcinoma arising
in a thyroglossal duct cyst. A case report. Acta Cytol. 40:747–750.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Patel SG, Escrig M, Shaha AR, Singh B and
Shah JP: Management of well-differentiated thyroid carcinoma
presenting within a thyroglossal duct cyst. J Surg Oncol.
79:134–141. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Clute HM and Smith LW: Cancer of the
thyroid gland. Arch Surg. 18:1–20. 1929. View Article : Google Scholar
|
|
9
|
Nachlas NE: Thyroglossal duct cysts. Ann
Otol Rhinol Laryngol. 59:381–390. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dalgaard JB and Wetteland P: Aberrant
thyroid tissue. II. Thyroglossal anomalies; a follow-up study of 58
cases. Acta Chir Scand. 111:444–455. 1956.PubMed/NCBI
|
|
11
|
Ruppmann E and Georgsson G: Squamous
carcinoma of the thyroglossal duct. Ger Med Mon. 11:442–447.
1966.PubMed/NCBI
|
|
12
|
Shepard GH and Rosenfeld L: Carcinoma of
thyroglossal duct remnants. Review of the literature and addition
of two cases. Am J Surg. 116:125–129. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mobini J, Krouse TB and Klinghoffer JF:
Squamous cell carcinoma arising in a thyroglossal duct cyst. Am
Surg. 40:290–294. 1974.PubMed/NCBI
|
|
14
|
Saharia PC: Carcinoma arising in
thyroglossal duct remnant: Case reports and review of the
literature. Br J Surg. 62:689–691. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Benveniste GL, Hunter R and Cook MG:
Squamous carcinoma of thyroglossal duct remnants: A case report and
review of the literature. Aust N Z J Surg. 50:53–55. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
White IL and Talbert WM: Squamous cell
carcinoma arising in thyroglossal duct remnant cyst epithelium.
Otolaryngol Head Neck Surg. 90:25–31. 1982.PubMed/NCBI
|
|
17
|
Ronan SG, Deutsch E and Ghosh L:
Thyroglossal duct carcinomas: Light and electron microscopic
studies. Head Neck Surg. 8:222–225. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bosch JL, Kummer EW and Hohmann FR:
Carcinoma of the thyroglossal duct. Neth J Surg. 38:36–40.
1986.PubMed/NCBI
|
|
19
|
Lustmann J, Benoliel R and Zeltser R:
Squamous cell carcinoma arising in a thyroglossal duct cyst in the
tongue. J Oral Maxillofac Surg. 47:81–85. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Colloby PS, Sinha M, Holl-Allen RT and
Crocker J: Squamous cell carcinoma in a thyroglossal cyst remnant:
A case report and review of the literature. World J Surg.
13:137–139. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yanagisawa K, Eisen RN and Sasaki CT:
Squamous cell carcinoma arising in a thyroglossal duct cyst. Arch
Otolaryngol Head Neck Surg. 118:538–541. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Virno VA, Mazzocconi G and Caprio G:
Carcinoma a cellule squamose del dotto tireoglosso. Caso Clinico G
Chir. 14:351–353. 1993.(In Italian).
|
|
23
|
Boswell WC, Zoller M, Williams JS, Lord SA
and Check W: Thyroglossal duct carcinoma. Am Surg. 60:650–655.
1994.PubMed/NCBI
|
|
24
|
Bardales RH, Suhrland MJ, Korourian S,
Schaefer RF, Hanna EY and Stanley MW: Cytologic findings in
thyroglossal duct carcinoma. Am J Clin Pathol. 106:615–619. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kwan WB, Liu FF, Banerjee D, Rotstein LE
and Tsang RW: Concurrent papillary and squamous carcinoma in a
thyroglossal duct cyst: A case report. Can J Surg. 39:328–332.
1996.PubMed/NCBI
|
|
26
|
Hama Y, Sugenoya A, Kobayashi S, Itoh N
and Amano J: Squamous cell carcinoma arising from thyroglossal duct
remnants: Report of a case and results of immunohistochemical
studies. Surg Today. 27:1077–1081. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
El Bakkouri W, Racy E, Vereecke A,
Gauthier A, Quillard J, Bobin S and Portier F: Squamous cell
carcinoma in a thyroglossal duct cyst. Ann Otolaryngol Chir
Cervicofac. 121:303–305. 2004.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Iakovou I, Konstantinidis I, Doumas A,
Nikolaidis V, Karatzas N and Efstratiou I: Squamous cell carcinoma
in a thyroglossal duct cyst and 99mTc-MIBI findings. Hell J Nucl
Med. 14:62–64. 2011.PubMed/NCBI
|
|
29
|
Yü Y, Wang XL, Xu ZG, Liu SY and Wang JY:
Management of thyroglossal duct carcinoma: Report of five cases.
Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 47:1013–1016.
2012.(In Chinese). PubMed/NCBI
|
|
30
|
Hanna E: Squamous cell carcinoma in a
thyroglossal duct cyst (TGDC): Clinical presentation, diagnosis,
and management. Am J Otolaryngol. 17:353–357. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nicolaides AR, Evans Rhys P and Fisher C:
Adenosquamous carcinoma of the thyroid gland. J Laryngol Otol.
103:978–979. 1989. View Article : Google Scholar : PubMed/NCBI
|