Introduction
Eosinophilic lung diseases, which comprise a varied
group of pulmonary diseases, are characterized by eosinophilic
infiltration of the interstitium of the lung, airways or alveoli
(1). They were originally described
as pulmonary infiltration with eosinophilia syndromes, and were
classified by the observation of lung infiltrates associated with
peripheral blood eosinophilia on chest radiographs (2). Currently, the detection of eosinophilic
lung disease may be based on the observation of lung tissue
eosinophilia on lung biopsy, bronchoalveolar lavage (BAL)
eosinophilia or pulmonary disease with blood eosinophilia. Primary
lung mucosa-associated lymphoid tissue (MALT) lymphoma is a rare
distinct entity. The outcome is generally favourable in the
majority of cases, with a 5-year overall survival of >80% or
>10 years (3). Generally, these
cases are difficult to diagnose accurately due to their nonspecific
clinical and radiological presentation (3). The present study reports a rare case of
MALT lymphoma, which was initially misdiagnosed as eosinophilic
pneumonia.
Case report
A 49-year-old woman was referred to Drum Tower
Hospital (Nanjing, China) in December 2012, presenting with a
2-month history of low-grade fever and a non-productive cough. The
patient was a non-smoker, had not recently travelled abroad and did
not own any domestic pets. The patient also denied any history of
allergic conditions. Her vital signs were stable at initial
examination; the patient was afebrile and oxygen saturation was 95%
in ambient air. On physical examination, auscultation of the lungs
detected slight coarse crackles at the right base. The remainder of
the examination was unremarkable. Laboratory tests identified
hypereosinophilia [white cell count: 7,200 cells/µl (normal range,
4,000–10,000 cells/µl), comprising 44.1% eosinophils (normal range,
0.5–5.0%), 33.3% neutrophils (normal range, 51.0–75.0%) and 15.6%
lymphocytes (normal range, 20.0–40.0%)]. Blood chemistry analysis
did not provide any remarkable data. The patient was negative for
antinuclear, antineutrophil cytoplasmic and antiparasitic
antibodies in immunofluorescence assays. A comprehensive metabolic
profile was normal and urine analysis did not identify any
sediment. Arterial blood gas analysis was as follows: pH, 7.444
(normal range, 7.350–7.450); PaO2, 73 mmHg (normal
range, 80–100 mmHg); and PaCO2, 37.1 mmHg (normal range,
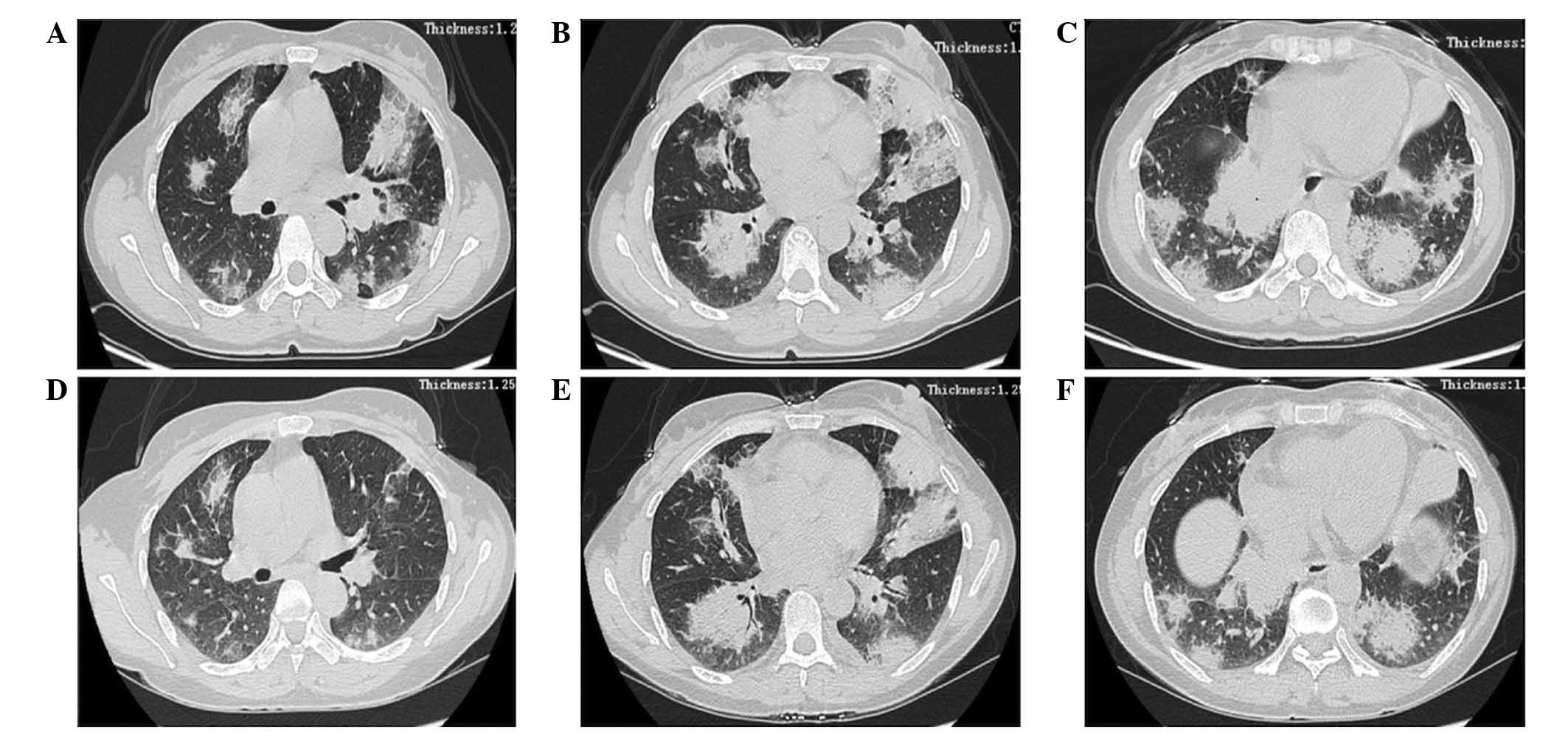
35.0–45.0 mmHg) in room air. High-resolution chest computed
tomography (CT; LightSpeed; GE Healthcare Life Sciences, Chalfont,
UK) revealed no pleural effusion or pulmonary edema, but did
identify diffuse, non-segmental areas of patchy (or airspace)
consolidation with peripheral predominance (Fig. 1A-C). Lung spirometry was performed and
the forced expiratory volume of 1 sec (FEV1), forced vital capacity
(FVC) and their ratio (FEV1/FVC) were determined to be 81.3, 84.3
and 96.9% of the predicted values, respectively. In addition,
carbon monoxide diffusion was 57.7% of the predicted value.
On day 4 of hospitalization, bronchoscopy with a
transbronchial lung biopsy (TBLB) was performed from the left
lingular lobe and the right middle lobe spur. In addition, BAL was
performed on the right middle lobe. The percentage of eosinophils
observed in the fluid obtained from BAL was 64%. Based on these
observations, the patient was diagnosed with eosinophilic
pneumonia. Corticosteroids (40 mg/day methylprednisolone) were
administered for 3 days, followed by oral administration of
prednisolone (30 mg/day), which resulted in immediate improvement,
with the eosinophil count rapidly decreasing from 44.1% to a normal
level within 3 days. The patient was discharged and instructed to
gradually reduce the dose of prednisolone to 20 mg. However, 6
months after the initiation of treatment, the abnormal shadow
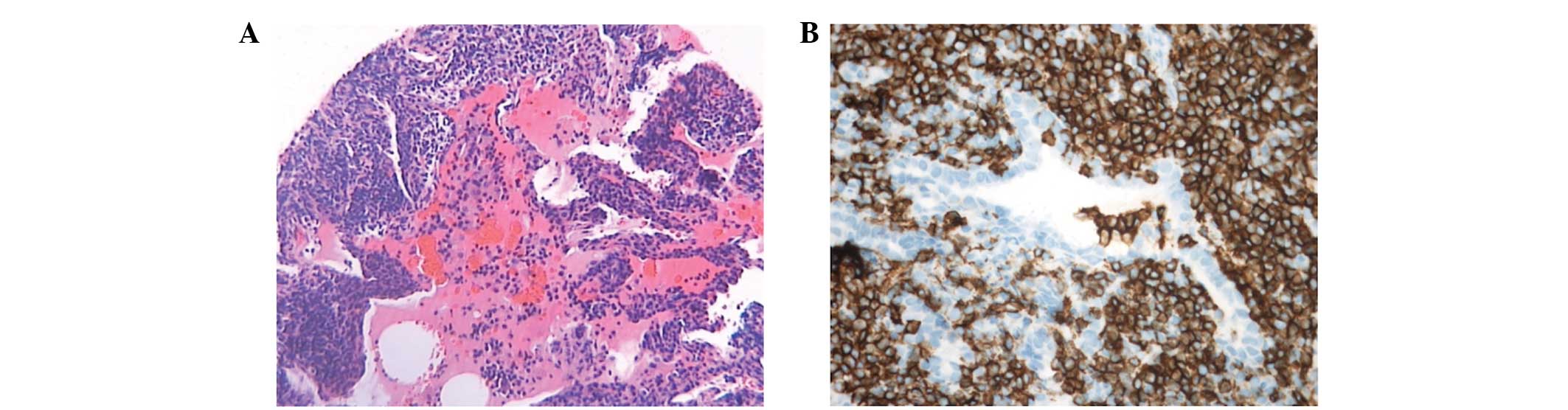
observed on CT scans of the chest had not diminished (Fig. 1D-F). CT-guided needle biopsy of the
lung was performed. Tissue samples were fixed in 10% neutral
formaldehyde solution (Sigma-Aldrich China, Inc., Shanghai, China),
dehydrated, embedded in paraffin (Leica Biosystems, Shanghai,
China), and conventionally stained with hematoxylin and eosin.
Microscopic examination (BX41; Olympus Corporation, Tokyo, Japan)
of the specimen revealed an intense lymphoid infiltrate, which
primarily consisted of B cells (Fig.
2A). Deparaffinized sections of patient tissue samples were
washed with phosphate-buffered saline (PBS) three times for 5 min
each. In order to block the endogenous peroxidase activity, the
sections were incubated in PBS that contained 3%
H2O2 for 10 min, and then immersed in 10%
sheep serum for 30 min, prior to be incubated overnight with
specific antibodies against cluster of differentiation (CD)3 (clone
PS1; mouse anti-human monoclonal antibody; dilution, 1:100; PA0553;
Novo castra; Leica Biosystems), CD5 (clone 4C7; mouse anti-human
monoclonal antibody; dilution, 1:100; M3641; Dako, Glostrup,
Denmark), CD20 (clone L26; mouse anti-human monoclonal antibody;
dilution, 1:500; M0755; Dako) and CD79a (clone JCB117; mouse
anti-human monoclonal antibody; dilution, 1:150; M7050; Dako). The
sections were washed and stained according to the manufacturer's
protocol. Immunohistochemical analysis demonstrated that the lesion
was positive for B cell markers, including cluster of
differentiation (CD)20, CD79a and B cell lymphoma 2, and negative
for T cell markers, including CD5 and CD3 (Fig. 2B). These findings were consistent with
a diagnosis of MALT lymphoma. Thus, the patient was referred to the
Department of Hematology of Drum Tower Hospital, where the patient
was treated with 6 cycles of R-CHOP (rituximab, cyclophosphamide,
doxorubicin, vincristine and prednisone). The patient was followed
up 30 months, and continues to be stable at present.
Discussion
Pulmonary eosinophilic infiltrates are a
heterogeneous group of pulmonary disorders that are accompanied by
characteristics of eosinophilia and lung disease in the peripheral
blood, pulmonary interstitium or BAL fluid. Radiological and
clinical presentations of these disorders may include chronic or
acute eosinophilic pneumonia, allergic bronchopulmonary
aspergillosis, simple pulmonary eosinophilia and pulmonary
eosinophilia associated with a systemic disease, such as
hypereosinophilic syndrome or Churg-Strauss syndrome (1). A diagnosis of eosinophilic lung disease
may be determined by the identification of any of the following:
Tissue eosinophilia confirmed at open biopsy or TBLB, increased
eosinophils in BAL fluid, or pulmonary opacities with peripheral
eosinophilia (4).
In the present case, a CT scan of the chest at
admission demonstrated infiltrations in each lung with blood
eosinophilia, and BAL fluid analysis identified a significant
increase in the percentage of eosinophils. At admission, the
clinical course of the patient and the BAL fluid results
corresponded with a diagnosis of chronic eosinophilic pneumonia;
thus, video-assisted thoracoscopic (VATS) lung biopsy or CT-guided
percutaneous lung biopsy were not performed. As it is not possible
to diagnose malignant lymphoma from BAL fluid analysis (3), this disease may have gone undetected at
the time of referral.
Eosinophilic pneumonia may present as an early
manifestation of lymphoma (4); thus,
patients must be carefully monitored for any signs of deterioration
in their clinical condition. Tissue eosinophilia is often observed
in Hodgkin's disease and non-Hodgkin's lymphoma of T cell origin
(5,6).
However, eosinophilia is rarely observed in non-Hodgkin's lymphoma
of B cell origin (3). There have been
a limited number of cases of chronic eosinophilic pneumonia
occurring prior to lymphoma (histiocytic type) and malignant
histiocytosis (7,8), and pulmonary MALT lymphoma is extremely
rare (3).
The physical signs and symptoms of pulmonary MALT
lymphoma are highly heterogeneous. Symptomatic patients may present
with hemoptysis, a cough, chest pain, sputum and/or moderate fever
(3). The disease is characterized by
indolent lesions, and patients often have a good prognosis
(3). Additionally, the radiographical
appearance of pulmonary MALT lymphoma is highly diverse (9). McCulloch et al (10) observed that MALT lymphoma lesions were
typically multifocal and composed of poorly-defined nodules
containing air bronchograms. The same study also reported the
presence of focal lobar consolidation (10). Mediastinal lymphadenopathy and pleural
reaction are uncommon (10). Bae
et al (11) assessed the
radiological appearance of 21 cases of MALT lymphoma. It was
determined that multiple or single nodules, or areas of
consolidation were the predominant radiographical abnormalities
observed (11). In the current case,
the major radiographical abnormality observed was described as
multiple, patchy (or airspace) consolidations. Due to the
poorly-defined clinical and imaging features of this disease, the
majority of cases are initially misdiagnosed as pneumonia,
pulmonary tuberculosis, organizing pneumonia or interstitial lung
disease, and the diagnosis of primary pulmonary lymphoma is a
common clinical challenge (11).
A diagnosis of pulmonary MALT lymphoma may only be
confirmed by pathological methods. Open thoracotomy, or CT-guided
percutaneous or VATS lung biopsies are the most commonly used
methods to obtain samples. CT-guided percutaneous needle biopsy
minimizes the requirement for open biopsy, and has therefore become
an important diagnostic tool (3). A
final diagnosis of primary pulmonary lymphoma requires a tissue
sample obtained through invasive procedures. CT-guided core-needle
biopsy is also widely used in the classification and diagnosis of
malignant lymphomas.
In conclusion, the present study described an
extremely rare case of malignant lymphoma, which was initially
misdiagnosed as eosinophilic pneumonia. If a patient is not
responsive to treatment, an alternative diagnosis should be
considered and invasive procedures, including CT-guided
percutaneous lung biopsies, open thoracotomy or a VATS lung biopsy,
should be performed to provide an accurate diagnosis.
References
|
1
|
Bhatt NY and Allen JN: Update on
eosinophilic lung diseases. Semin Respir Crit Care Med. 33:555–571.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mann B: Eosinophilic lung disease. Clin
Med Circ Respirat Pulm Med. 2:99–108. 2008.
|
|
3
|
Cadranel J, Wislez M and Antoine M:
Primary pulmonary lymphoma. Eur Respir J. 20:750–762. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jeong YJ, Kim KI, Seo IJ, Lee CH, Lee KN,
Kim KN, Kim JS and Kwon WJ: Eosinophilic lung diseases: A clinical,
radiologic, and pathologic overview. Radiographics. 27:617–639.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Thiruchelvam JK, Penfold CN and Akhtar S:
Chronic eosinophilic pneumonia associated with T-cell lymphoma. Int
J Oral Maxillofac Surg. 31:112–114. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kunimasa K, Arita M, Arai Y, Uchino K,
Iwasaku M, Jo T, Konishi S and Ishida T: Peripheral T-cell lymphoma
not otherwise specified (PTCL-NOS) in a patient with
hypereosinophilic syndrome showing multiple nodules on chest
computed tomography. Intern Med. 50:2417–2421. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Watanabe K, Shinbo T, Kojima M, Naito M,
Tanahashi N and Nara M: B-cell lymphoma associated with
eosinophilia. Cancer. 64:1682–1685. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fujii M, Tanimoto Y, Kiguchi T, Takehara
H, Fujimori Y, Teshima T, Kanehiro A, Shinagawa K, Tada S and
Kataoka M: Pulmonary infiltration with eosinophilia syndrome
complicated with non-Hodgkin's lymphoma of B cell lineage. Allergol
Int. 52:161–164. 2003. View Article : Google Scholar
|
|
9
|
Hare SS, Souza CA, Bain G, Seely JM Frcpc,
Gomes MM and Quigley M: The radiological spectrum of pulmonary
lymphoproliferative disease. Br J Radiol. 85:848–864. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McCulloch GL, Sinnatamby R, Stewart S,
Goddard M and Flower CD: High-resolution computed tomographic
appearance of MALToma of the lung. Eur Radiol. 8:1669–1673. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bae YA, Lee KS, Han J, Ko YH, Kim BT,
Chung MJ and Kim TS: Marginal zone B-cell lymphoma of
bronchus-associated lymphoid tissue: Imaging findings in 21
patients. Chest. 133:433–440. 2008. View Article : Google Scholar : PubMed/NCBI
|