|
1
|
Modlin IM, Oberg K, Chung DC, Jensen RT,
de Herder WW, Thakker RV, Caplin M, Fave G Delle, Kaltsas GA,
Krenning EP, et al: Gastroenteropancreatic neuroendocrine tumours.
Lancet Oncol. 9:61–72. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
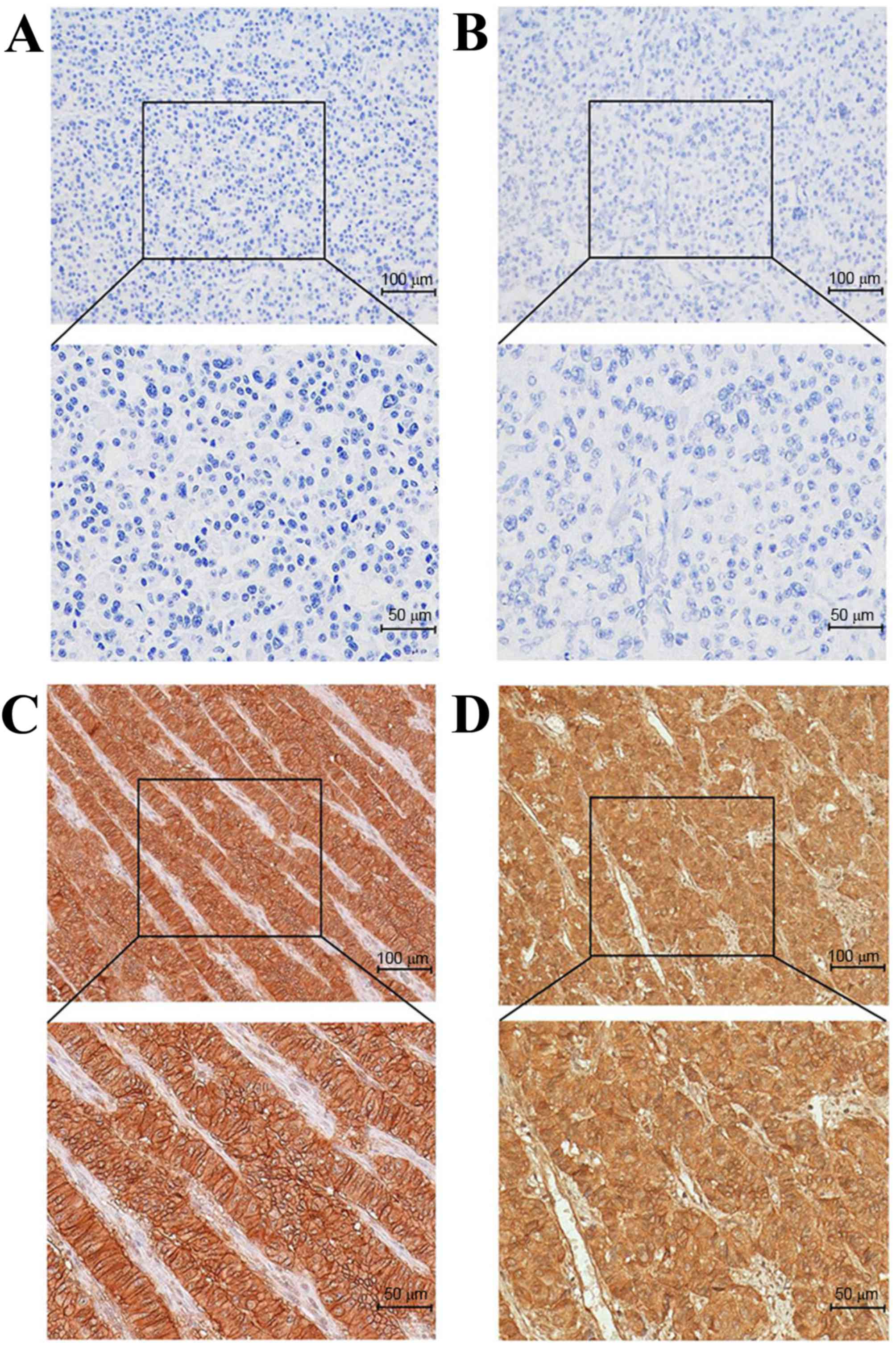
Papotti M, Bongiovanni M, Volante M, Allìa
E, Landolfi S, Helboe L, Schindler M, Cole SL and Bussolati G:
Expression of somatostatin receptor types 1–5 in 81 cases of
gastrointestinal and pancreatic endocrine tumors. A correlative
immunohistochemical and reverse-transcriptase polymerase chain
reaction analysis. Virchows Arch. 440:461–475. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kulaksiz H, Eissele R, Rössler D, Schulz
S, Höllt V, Cetin Y and Arnold R: Identification of somatostatin
receptor subtypes 1, 2a, 3 and 5 in neuroendocrine tumours with
subtype specific antibodies. Gut. 50:52–60. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Korner M, Eltschinger V, Waser B,
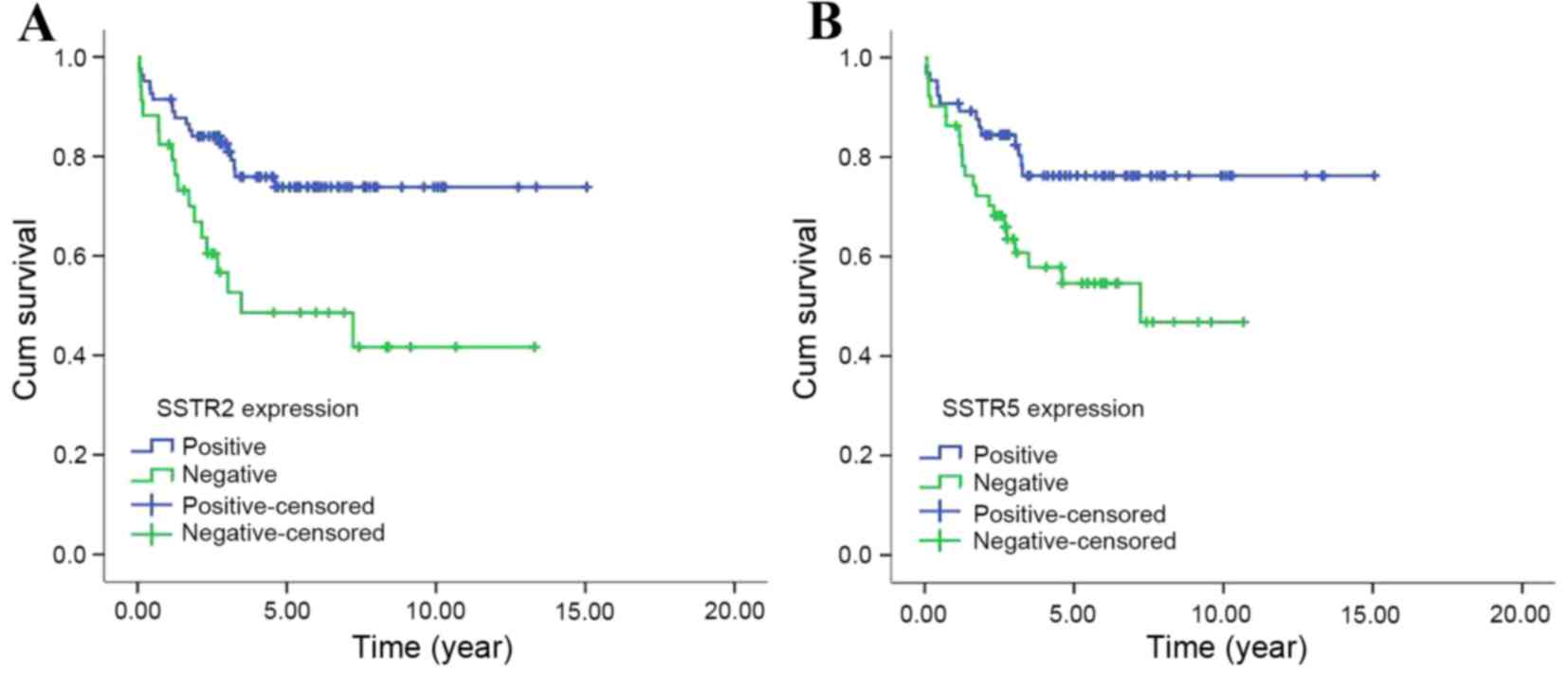
Schonbrunn A and Reubi JC: Value of immunohistochemistry for
somatostatin receptor subtype sst2a in cancer tissues: Lessons from
the comparison of anti-sst2a antibodies with somatostatin receptor
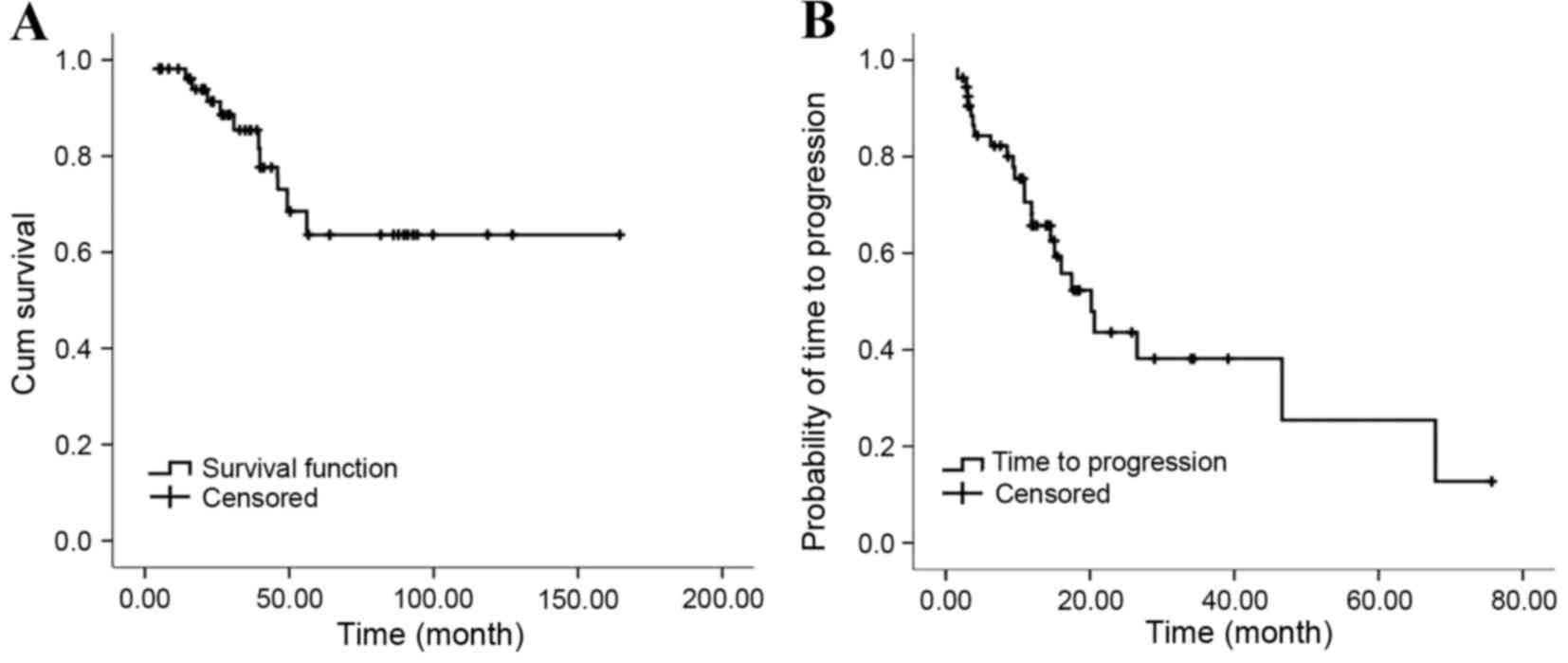
autoradiography. Am J Surg Pathol. 29:1642–1651. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zamora V, Cabanne A, Salanova R, Bestani
C, Domenichini E, Marmissolle F, Giacomi N, O'Connor J, Méndez G
and Roca E: Buenos Aires and La Plata Argentina Argentum Working
Group: Immunohistochemical expression of somatostatin receptors in
digestive endocrine tumours. Dig Liver Dis. 42:220–225. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Volante M, Brizzi MP, Faggiano A, La Rosa
S, Rapa I, Ferrero A, Mansueto G, Righi L, Garancini S, Capella C,
et al: Somatostatin receptor type 2a immunohistochemistry in
neuroendocrine tumors: A proposal of scoring system correlated with
somatostatin receptor scintigraphy. Mod Pathol. 20:1172–1182. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hofland LJ and Lamberts SW: The
pathophysiological consequences of somatostatin receptor
internalization and resistance. Endocr Rev. 24:28–47. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Oberg KE, Reubi JC, Kwekkeboom DJ and
Krenning EP: Role of somatostatins in gastroenteropancreatic
neuroendocrine tumor development and therapy. Gastroenterology.
139:742–753, 753.e1. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Oberg K: Future aspects of
somatostatin-receptor-mediated therapy. Neuroendocrinology.
80:(Suppl 1). S57–S61. 2004. View Article : Google Scholar
|
|
10
|
Appetecchia M and Baldelli R: Somatostatin
analogues in the treatment of gastroenteropancreatic neuroendocrine
tumours, current aspects and new perspectives. J Exp Clin Cancer
Res. 29:192010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rinke A, Müller HH, Schade-Brittinger C,
Klose KJ, Barth P, Wied M, Mayer C, Aminossadati B, Pape UF, Bläker
M, et al: Placebo-controlled, double-blind, prospective, randomized
study on the effect of octreotide lar in the control of tumor
growth in patients with metastatic neuroendocrine midgut tumors: A
report from the promid study group. J Clin Oncol. 27:4656–4663.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Caplin ME, Pavel M, Ćwikła JB, Phan AT,
Raderer M, Sedláčková E, Cadiot G, Wolin EM, Capdevila J, Wall L,
et al: Lanreotide in metastatic enteropancreatic neuroendocrine
tumors. N Engl J Med. 371:224–233. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lim T, Lee J, Kim JJ, Lee JK, Lee KT, Kim
YH, Kim KW, Kim S, Sohn TS, Choi DW, et al: Gastroenteropancreatic
neuroendocrine tumors: Incidence and treatment outcome in a single
institution in korea. Asia Pac J Clin Oncol. 7:293–299. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hauso O, Gustafsson BI, Kidd M, Waldum HL,
Drozdov I, Chan AK and Modlin IM: Neuroendocrine tumor
epidemiology: Contrasting norway and north america. Cancer.
113:2655–2664. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yao JC, Hassan M, Phan A, Dagohoy C, Leary
C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A and Evans
DB: One hundred years after ‘carcinoid’: Epidemiology of and
prognostic factors for neuroendocrine tumors in 35,825 cases in the
united states. J Clin Oncol. 26:3063–3072. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang YH, Lin Y, Xue L, Wang JH, Chen MH
and Chen J: Relationship between clinical characteristics and
survival of gastroenteropancreatic neuroendocrine neoplasms: A
single-institution analysis (1995–2012) in south china. BMC Endocr
Disord. 12:302012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ito T, Okusaka T, Nishida T, Yamao K,
Igarashi H, Morizane C, Kondo S, Mizuno N, Hara K, Sawaki A, et al:
Phase ii study of sunitinib in japanese patients with unresectable
or metastatic, well-differentiated pancreatic neuroendocrine tumor.
Invest New Drugs. 31:1265–1274. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Raymond E, Dahan L, Raoul JL, Bang YJ,
Borbath I, Lombard-Bohas C, Valle J, Metrakos P, Smith D, Vinik A,
et al: Sunitinib malate for the treatment of pancreatic
neuroendocrine tumors. N Engl J Med. 364:501–513. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bosman F, Carneiro F, Hruban R and Theise
N: Who classification of tumours of the digestive system. 4th. IARC
Press; PA: 2010
|
|
20
|
Rindi G, Klöppel G, Alhman H, Caplin M,
Couvelard A, de Herder WW, Erikssson B, Falchetti A, Falconi M,
Komminoth P, et al: Tnm staging of foregut (neuro)endocrine tumors:
A consensus proposal including a grading system. Virchows Arch.
449:395–401. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rindi G, Klöppel G, Couvelard A, Komminoth
P, Körner M, Lopes JM, McNicol AM, Nilsson O, Perren A, Scarpa A,
et al: Tnm staging of midgut and hindgut (neuro) endocrine tumors:
A consensus proposal including a grading system. Virchows Arch.
451:757–762. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen AP, Setser A, Anadkat MJ, Cotliar J,
Olsen EA, Garden BC and Lacouture ME: Grading dermatologic adverse
events of cancer treatments: The common terminology criteria for
adverse events version 4.0. J Am Acad Dermatol. 67:1025–1039. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Diakatou E, Kaltsas G, Tzivras M, Kanakis
G, Papaliodi E and Kontogeorgos G: Somatostatin and dopamine
receptor profile of gastroenteropancreatic neuroendocrine tumors:
An immunohistochemical study. Endocr Pathol. 22:24–30. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
van Adrichem RC, Kamp K, van Deurzen CH,
Biermann K, Feelders RA, Franssen GJ, Kwekkeboom DJ, Hofland LJ and
de Herder WW: Is there an additional value of somatostatin receptor
subtype 2a immunohistochemistry over somatostatin receptor
scintigraphy uptake in predicting gastroenteropancreatic
neuroendocrine tumor response? Neuroendocrinology. 103:560–566.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sclafani F, Carnaghi C, Di Tommaso L,
Rodari M, Destro A, Rimassa L, Giordano L, Chiti A, Roncalli M and
Santoro A: Detection of somatostatin receptor subtypes 2 and 5 by
somatostatin receptor scintigraphy and immunohistochemistry:
Clinical implications in the diagnostic and therapeutic management
of gastroenteropancreatic neuroendocrine tumors. Tumori.
97:620–628. 2011.PubMed/NCBI
|
|
27
|
Yerci O, Sehitoglu I, Ugras N, Cubukcu E,
Yuce S, Bedir R and Cure E: Somatostatin receptor 2 and 5
expressions in gastroenteropancreatic neuroendocrine tumors in
turkey. Asian Pac J Cancer Prev. 16:4377–4381. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Nasir A, Stridsberg M, Strosberg J, Su PH,
Livingston S, Malik HA, Kelley ST, Centeno BA, Coppola D, Malafa
ME, et al: Somatostatin receptor profiling in hepatic metastases
from small intestinal and pancreatic neuroendocrine neoplasms:
Immunohistochemical approach with potential clinical utility.
Cancer Control. 13:52–60. 2006.PubMed/NCBI
|
|
29
|
Srirajaskanthan R, Watkins J, Marelli L,
Khan K and Caplin ME: Expression of somatostatin and dopamine 2
receptors in neuroendocrine tumours and the potential role for new
biotherapies. Neuroendocrinology. 89:308–314. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Okuwaki K, Kida M, Mikami T, Yamauchi H,
Imaizumi H, Miyazawa S, Iwai T, Takezawa M, Saegusa M, Watanabe M
and Koizumi W: Clinicopathologic characteristics of pancreatic
neuroendocrine tumors and relation of somatostatin receptor type 2a
to outcomes. Cancer. 119:4094–4102. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kaemmerer D, Trager T, Hoffmeister M,
Sipos B, Hommann M, Sänger J, Schulz S and Lupp A: Inverse
expression of somatostatin and cxcr4 chemokine receptors in
gastroenteropancreatic neuroendocrine neoplasms of different
malignancy. Oncotarget. 6:27566–27579. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Corleto VD, Falconi M, Panzuto F, Milione
M, De Luca O, Perri P, Cannizzaro R, Bordi C, Pederzoli P, Scarpa A
and Fave G Delle: Somatostatin receptor subtypes 2 and 5 are
associated with better survival in well-differentiated endocrine
carcinomas. Neuroendocrinology. 89:223–230. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Jann H, Denecke T, Koch M, Pape UF,
Wiedenmann B and Pavel M: Impact of octreotide long-acting release
on tumour growth control as a first-line treatment in
neuroendocrine tumours of pancreatic origin. Neuroendocrinology.
98:137–143. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Broder MS, Beenhouwer D, Strosberg JR,
Neary MP and Cherepanov D: Gastrointestinal neuroendocrine tumors
treated with high dose octreotide-lar: A systematic literature
review. World J Gastroenterol. 21:1945–1955. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Welin SV, Janson ET, Sundin A, Stridsberg
M, Lavenius E, Granberg D, Skogseid B, Oberg KE and Eriksson BK:
High-dose treatment with a long-acting somatostatin analogue in
patients with advanced midgut carcinoid tumours. Eur J Endocrinol.
151:107–112. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ferolla P, Faggiano A, Grimaldi F, Ferone
D, Scarpelli G, Ramundo V, Severino R, Bellucci MC, Camera LM,
Lombardi G, et al: Shortened interval of long-acting octreotide
administration is effective in patients with well-differentiated
neuroendocrine carcinomas in progression on standard doses. J
Endocrinol Invest. 35:326–331. 2012.PubMed/NCBI
|
|
37
|
Baldelli R, Barnabei A, Rizza L, Isidori
AM, Rota F, Di Giacinto P, Paoloni A, Torino F, Corsello SM, Lenzi
A and Appetecchia M: Somatostatin analogs therapy in
gastroenteropancreatic neuroendocrine tumors: Current aspects and
new perspectives. Front Endocrinol (Lausanne). 5:72014.PubMed/NCBI
|
|
38
|
Yao JC, Shah MH, Ito T, Bohas CL, Wolin
EM, Van Cutsem E, Hobday TJ, Okusaka T, Capdevila J, de Vries EG,
et al: Everolimus for advanced pancreatic neuroendocrine tumors. N
Engl J Med. 364:514–523. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kouvaraki MA, Ajani JA, Hoff P, Wolff R,
Evans DB, Lozano R and Yao JC: Fluorouracil, doxorubicin and
streptozocin in the treatment of patients with locally advanced and
metastatic pancreatic endocrine carcinomas. J Clin Oncol.
22:4762–4771. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Sun W, Lipsitz S, Catalano P, Mailliard JA
and Haller DG: Eastern Cooperative Oncology Group: Phase ii/iii
study of doxorubicin with fluorouracil compared with streptozocin
with fluorouracil or dacarbazine in the treatment of advanced
carcinoid tumors: Eastern cooperative oncology group study e1281. J
Clin Oncol. 23:4897–4904. 2005. View Article : Google Scholar : PubMed/NCBI
|