|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sepiashvili L, Hui A, Ignatchenko V, Shi
W, Su S, Xu W, Huang SH, O'Sullivan B, Waldron J, Irish JC, et al:
Potentially novel candidate biomarkers for head and neck squamous
cell carcinoma identified using an integrated cell line-based
discovery strategy. Mol Cell Proteomics. 11:1404–1415. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hashibe M, Brennan P, Benhamou S,
Castellsague X, Chen C, Curado MP, Dal Maso L, Daudt AW, Fabianova
E, Fernandez L, et al: Alcohol drinking in never users of tobacco,
cigarette smoking in never drinkers, and the risk of head and neck
cancer: Pooled analysis in the International Head and Neck Cancer
Epidemiology Consortium. J Natl Cancer Inst. 99:777–789. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hashibe M, Brennan P, Chuang SC, Boccia S,
Castellsague X, Chen C, Curado MP, Dal Maso L, Daudt AW, Fabianova
E, et al: Interaction between tobacco and alcohol use and the risk
of head and neck cancer: Pooled analysis in the international head
and neck cancer epidemiology consortium. Cancer Epidemiol
Biomarkers Prev. 18:541–550. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ang KK and Sturgis EM: Human
papillomavirus as a marker of the natural history and response to
therapy of head and neck squamous cell carcinoma. Semin Radiat
Oncol. 22:128–142. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Romanitan M, Näsman A, Ramqvist T,
Dahlstrand H, Polykretis L, Vogiatzis P, Vamvakas P, Tasopoulos G,
Valavanis C, Arapantoni-Dadioti P, et al: Human papillomavirus
frequency in oral and oropharyngeal cancer in Greece. Anticancer
Res. 28:2077–2080. 2008.PubMed/NCBI
|
|
7
|
Dayyani F, Etzel CJ, Liu M, Ho CH, Lippman
SM and Tsao AS: Meta-analysis of the impact of human papillomavirus
(HPV) on cancer risk and overall survival in head and neck squamous
cell carcinomas (HNSCC). Head Neck Oncol. 2:152010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lopez-Ocejo O, Viloria-Petit A,
Bequet-Romero M, Mukhopadhyay D, Rak J and Kerbel RS: Oncogenes and
tumor angiogenesis: The HPV-16 E6 oncoprotein activates the
vascular endothelial growth factor (VEGF) gene promoter in a p53
independent manner. Oncogene. 19:4611–4620. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gillison ML, Castellsagué X, Chaturvedi A,
Goodman MT, Snijders P, Tommasino M, Arbyn M and Franceschi S:
Eurogin Roadmap: Comparative epidemiology of HPV infection and
associated cancers of the head and neck and cervix. Int J Cancer.
134:497–507. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dok R and Nuyts S: HPV positive head and
neck cancers: Molecular pathogenesis and evolving treatment
strategies. Cancers (Basel). 8:pii: E41. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Doorbar J: Molecular biology of human
papillomavirus infection and cervical cancer. Clin Sci (Lond).
110:525–541. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sturgis EM and Ang KK: The epidemic of
HPV-associated oropharyngeal cancer is here: Is it time to change
our treatment paradigms? J Natl Compr Canc Netw. 9:665–673.
2011.PubMed/NCBI
|
|
13
|
O'Sullivan B, Huang SH, Perez-Ordonez B,
Massey C, Siu LL, Weinreb I, Hope A, Kim J, Bayley AJ, Cummings B,
et al: Outcomes of HPV-related oropharyngeal cancer patients
treated by radiotherapy alone using altered fractionation.
Radiother Oncol. 103:49–56. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Park CC, Bissell MJ and Barcellos-Hoff MH:
The influence of the microenvironment on the malignant phenotype.
Mol Med Today. 6:324–329. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Aderhold C, Umbreit C, Faber A, Birk R,
Sommer JU, Hörmann K and Schultz JD: Matrix metalloproteinase-2 and
−14 in p16-positive and -negative HNSCC after exposure To 5-FU and
docetaxel in vitro. Anticancer Res. 34:4929–4937. 2014.PubMed/NCBI
|
|
16
|
Curry JM, Sprandio J, Cognetti D,
Luginbuhl A, Bar-ad V, Pribitkin E and Tuluc M: Tumor
microenvironment in head and neck squamous cell carcinoma. Semin
Oncol. 41:217–234. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jimenez L, Sharma VP, Condeelis J, Harris
T, Ow TJ, Prystowsky MB, Childs G and Segall JE: MicroRNA-375
suppresses extracellular matrix degradation and invadopodial
activity in head and neck squamous cell carcinoma. Arch Pathol Lab
Med. 139:1349–1361. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rosenthal EL and Matrisian LM: Matrix
metalloproteases in head and neck cancer. Head Neck. 28:639–648.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nelson AR, Fingleton B, Rothenberg ML and
Matrisian LM: Matrix metalloproteinases: Biologic activity and
clinical implications. J Clin Oncol. 18:1135–1149. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ravanti L and Kähäri VM: Matrix
metalloproteinases in wound repair (review). Int J Mol Med.
6:391–407. 2000.PubMed/NCBI
|
|
21
|
Monsky WL, Kelly T, Lin CY, Yeh Y,
Stetler-Stevenson WG, Mueller SC and Chen WT: Binding and
localization of M(r) 72,000 matrix metalloproteinase at cell
surface invadopodia. Cancer Res. 53:3159–3164. 1993.PubMed/NCBI
|
|
22
|
Rundhaug JE: Matrix metalloproteinases,
angiogenesis, and cancer: Commentary re: A. C. Lockhart et
al: Reduction of wound angiogenesis in patients treated with
BMS-275291, a broad spectrum matrix metalloproteinase inhibitor.
Clin. Cancer Res., 9: 00-00, 2003. Clin Cancer Res. 9:551–554.
2003.PubMed/NCBI
|
|
23
|
Koontongkaew S, Amornphimoltham P,
Monthanpisut P, Saensuk T and Leelakriangsak M: Fibroblasts and
extracellular matrix differently modulate MMP activation by primary
and metastatic head and neck cancer cells. Med Oncol. 29:690–703.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Koontongkaew S: The tumor microenvironment
contribution to development, growth, invasion and metastasis of
head and neck squamous cell carcinomas. J Cancer. 4:66–83. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ferrara N, Gerber HP and LeCouter J: The
biology of VEGF and its receptors. Nat Med. 9:669–676. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Folkman J: The role of angiogenesis in
tumor growth. Semin Cancer Biol. 3:65–71. 1992.PubMed/NCBI
|
|
27
|
Hsu HW, Wall NR, Hsueh CT, Kim S, Ferris
RL, Chen CS and Mirshahidi S: Combination antiangiogenic therapy
and radiation in head and neck cancers. Oral Oncol. 50:19–26. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mineta H, Miura K, Ogino T, Takebayashi S,
Misawa K, Ueda Y, Suzuki I, Dictor M, Borg A and Wennerberg J:
Prognostic value of vascular endothelial growth factor (VEGF) in
head and neck squamous cell carcinomas. Br J Cancer. 83:775–781.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Argiris A, Lee SC, Feinstein T, Thomas S,
Branstetter BF IV, Seethala R, Wang L, Gooding W, Grandis JR and
Ferris RL: Serum biomarkers as potential predictors of antitumor
activity of cetuximab-containing therapy for locally advanced head
and neck cancer. Oral Oncol. 47:961–966. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
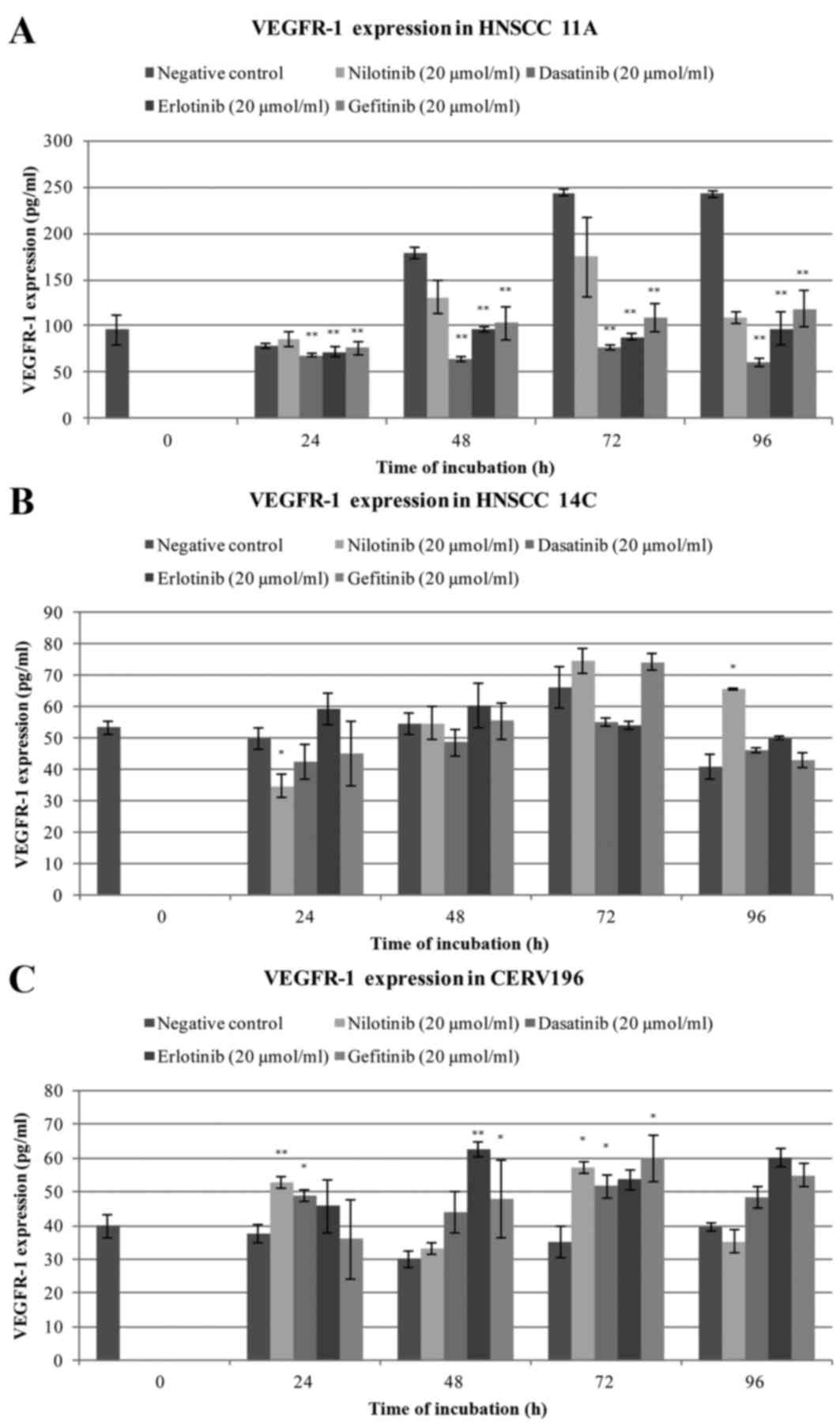
Aderhold C, Faber A, Umbreit C,
Chakraborty A, Bockmayer A, Birk R, Sommer JU, Hörmann K and
Schultz JD: Small molecules alter VEGFR and PTEN expression in
HPV-positive and -negative SCC: New hope for targeted-therapy.
Anticancer Res. 35:1389–1399. 2015.PubMed/NCBI
|
|
31
|
Kramer B, Hock C, Birk R, Sauter A, Stuck
BA, Hörmann K, Schultz JD and Aderhold C: Targeted therapies in
HPV-positive and -negative HNSCC-alteration of EGFR and VEGFR-2
expression in vitro. Anticancer Res. 36:2799–2807. 2016.PubMed/NCBI
|
|
32
|
Cabebe E and Wakelee H: Role of
anti-angiogenesis agents in treating NSCLC: Focus on bevacizumab
and VEGFR tyrosine kinase inhibitors. Curr Treat Options Oncol.
8:15–27. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Van Limbergen EJ, Zabrocki P, Porcu M,
Hauben E, Cools J and Nuyts S: FLT1 kinase is a mediator of
radioresistance and survival in head and neck squamous cell
carcinoma. Acta Oncol. 53:637–645. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Le Buanec H, D'Anna R, Lachgar A, Zagury
JF, Bernard J, Ittelé D, d'Alessio P, Hallez S, Giannouli C, Burny
A, et al: HPV-16 E7 but not E6 oncogenic protein triggers both
cellular immunosuppression and angiogenic processes. Biomed
Pharmacother. 53:424–431. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
No JH, Jo H, Kim SH, Park IA, Kang D, Han
SS, Kim JW, Park NH, Kang SB and Song YS: Expression of vascular
endothelial growth factor and hypoxia inducible factor-1alpha in
cervical neoplasia. Ann N Y Acad Sci. 1171:105–110. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ward WH, Cook PN, Slater AM, Davies DH,
Holdgate GA and Green LR: Epidermal growth factor receptor tyrosine
kinase. Investigation of catalytic mechanism, structure-based
searching and discovery of a potent inhibitor. Biochem Pharmacol.
48:659–666. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Bareschino MA, Schettino C, Troiani T,
Martinelli E, Morgillo F and Ciardiello F: Erlotinib in cancer
treatment. Ann Oncol. 18:(Suppl 6). vi35–vi41. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Gridelli C, Bareschino MA, Schettino C,
Rossi A, Maione P and Ciardiello F: Erlotinib in non-small cell
lung cancer treatment: Current status and future development. The
Oncologist. 12:840–849. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hirata A, Ogawa S, Kometani T, Kuwano T,
Naito S, Kuwano M and Ono M: ZD1839 (Iressa) induces antiangiogenic
effects through inhibition of epidermal growth factor receptor
tyrosine kinase. Cancer Res. 62:2554–2560. 2002.PubMed/NCBI
|
|
40
|
Wakeling AE: Inhibitors of growth factor
signalling. Endocr Relat Cancer. 12:(Suppl 1). S183–S187. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Toda D, Ota T, Tsukuda K, Watanabe K,
Fujiyama T, Murakami M, Naito M and Shimizu N: Gefitinib decreases
the synthesis of matrix metalloproteinase and the adhesion to
extracellular matrix proteins of colon cancer cells. Anticancer
Res. 26:129–134. 2006.PubMed/NCBI
|
|
42
|
Kantarjian H, Giles F, Wunderle L, Bhalla
K, O'Brien S, Wassmann B, Tanaka C, Manley P, Rae P, Mietlowski W,
et al: Nilotinib in imatinib-resistant CML and Philadelphia
chromosome-positive ALL. N Engl J Med. 354:2542–2551. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Manley PW, Drueckes P, Fendrich G, Furet
P, Liebetanz J, Martiny-Baron G, Mestan J, Trappe J, Wartmann M and
Fabbro D: Extended kinase profile and properties of the protein
kinase inhibitor nilotinib. Biochim Biophys Acta. 1804:445–453.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
le Coutre P, Schwarz M and Kim TD: New
developments in tyrosine kinase inhibitor therapy for newly
diagnosed chronic myeloid leukemia. Clin Cancer Res. 16:1771–1780.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Bromann PA, Korkaya H and Courtneidge SA:
The interplay between Src family kinases and receptor tyrosine
kinases. Oncogene. 23:7957–7968. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Willis AL, Sabeh F, Li XY and Weiss SJ:
Extracellular matrix determinants and the regulation of cancer cell
invasion stratagems. J Microsc. 251:250–260. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Yao J, Xiong S, Klos K, Nguyen N, Grijalva
R, Li P and Yu D: Multiple signaling pathways involved in
activation of matrix metalloproteinase-9 (MMP-9) by heregulin-beta1
in human breast cancer cells. Oncogene. 20:8066–8074. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zuo JH, Zhu W, Li MY, Li XH, Yi H, Zeng
GQ, Wan XX, He QY, Li JH, Qu JQ, et al: Activation of EGFR promotes
squamous carcinoma SCC10A cell migration and invasion via inducing
EMT-like phenotype change and MMP-9-mediated degradation of
E-cadherin. J Cell Biochem. 112:2508–2517. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhang YQ, Wei XL, Liang YK, Chen WL, Zhang
F, Bai JW, Qiu SQ, Du CW, Huang WH and Zhang GJ: Over-expressed
twist associates with markers of epithelial mesenchymal transition
and predicts poor prognosis in breast cancers via ERK and Akt
activation. PLoS One. 10:e01358512015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhao L, Geng H, Liang ZF, Zhang ZQ, Zhang
T, Yu DX and Zhong CY: Benzidine induces epithelial-mesenchymal
transition in human uroepithelial cells through ERK1/2 pathway.
Biochem Biophys Res Commun. 459:643–649. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Qiao B, Johnson NW and Gao J:
Epithelial-mesenchymal transition in oral squamous cell carcinoma
triggered by transforming growth factor-beta1 is Snail
family-dependent and correlates with matrix metalloproteinase-2 and
−9 expressions. Int J Oncol. 37:663–668. 2010.PubMed/NCBI
|
|
52
|
Liu Z and Klominek J: Inhibition of
proliferation, migration, and matrix metalloprotease production in
malignant mesothelioma cells by tyrosine kinase inhibitors.
Neoplasia. 6:705–712. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Normanno N and Gullick WJ: Epidermal
growth factor receptor tyrosine kinase inhibitors and bone
metastases: Different mechanisms of action for a novel therapeutic
application? Endocr Relat Cancer. 13:3–6. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Lee EJ, Whang JH, Jeon NK and Kim J: The
epidermal growth factor receptor tyrosine kinase inhibitor ZD1839
(Iressa) suppresses proliferation and invasion of human oral
squamous carcinoma cells via p53 independent and MMP, uPAR
dependent mechanism. Ann N Y Acad Sci. 1095:113–128. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Li S, Zhang Z, Xue J, Guo X, Liang S and
Liu A: Effect of hypoxia on DDR1 expression in pituitary adenomas.
Med Sci Monit. 21:2433–2438. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kilarski WW, Jura N and Gerwins P:
Inactivation of Src family kinases inhibits angiogenesis in vivo:
Implications for a mechanism involving organization of the actin
cytoskeleton. Exp Cell Res. 291:70–82. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Liang W, Kujawski M, Wu J, Lu J, Herrmann
A, Loera S, Yen Y, Lee F, Yu H, Wen W and Jove R: Antitumor
activity of targeting SRC kinases in endothelial and myeloid cell
compartments of the tumor microenvironment. Clin Cancer Res.
16:924–935. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhu D, Ye M and Zhang W: E6/E7
oncoproteins of high risk HPV-16 upregulate MT1-MMP, MMP-2 and
MMP-9 and promote the migration of cervical cancer cells. Int J
Clin Exp Pathol. 8:4981–4989. 2015.PubMed/NCBI
|
|
59
|
Hu Z, Müller S, Qian G, Xu J, Kim S, Chen
Z, Jiang N, Wang D, Zhang H, Saba NF, et al: Human papillomavirus
16 oncoprotein regulates the translocation of β-catenin via the
activation of epidermal growth factor receptor. Cancer.
121:214–225. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Schwartz JD, Rowinsky EK, Youssoufian H,
Pytowski B and Wu Y: Vascular endothelial growth factor receptor-1
in human cancer: Concise review and rationale for development of
IMC-18F1 (Human antibody targeting vascular endothelial growth
factor receptor-1). Cancer. 116:(4 Suppl). S1027–S1032. 2010.
View Article : Google Scholar
|
|
61
|
Mayer EL and Krop IE: Advances in
targeting SRC in the treatment of breast cancer and other solid
malignancies. Clin Cancer Res. 16:3526–3532. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Kanda S, Miyata Y, Kanetake H and
Smithgall TE: Non-receptor protein-tyrosine kinases as molecular
targets for antiangiogenic therapy (Review). Int J Mol Med.
20:113–121. 2007.PubMed/NCBI
|
|
63
|
Argiris A, Kotsakis AP, Hoang T, Worden
FP, Savvides P, Gibson MK, Gyanchandani R, Blumenschein GR Jr, Chen
HX, Grandis JR, et al: Cetuximab and bevacizumab: Preclinical data
and phase II trial in recurrent or metastatic squamous cell
carcinoma of the head and neck. Ann Oncol. 24:220–225. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Cohen EE, Davis DW, Karrison TG, Seiwert
TY, Wong SJ, Nattam S, Kozloff MF, Clark JI, Yan DH, Liu W, et al:
Erlotinib and bevacizumab in patients with recurrent or metastatic
squamous-cell carcinoma of the head and neck: A phase I/II study.
Lancet Oncol. 10:247–257. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Tabernero J: The role of VEGF and EGFR
inhibition: Implications for combining anti-VEGF and anti-EGFR
agents. Mol Cancer Res. 5:203–220. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Dias JD, Guse K, Nokisalmi P, Eriksson M,
Chen DT, Diaconu I, Tenhunen M, Liikanen I, Grénman R, Savontaus M,
et al: Multimodal approach using oncolytic adenovirus, cetuximab,
chemotherapy and radiotherapy in HNSCC low passage tumour cell
cultures. Eur J Cancer. 46:625–635. 2010. View Article : Google Scholar : PubMed/NCBI
|