Introduction
Dermatofibrosarcoma protuberans (DFSP) is a rare,
slow-growing, low-grade tumor of putative dermal fibroblastic
origin. All DFSP recurrence is in situ and it rarely
metastasizes. It usually involves the trunk and extremities,
although tumors may occur in any part of the body in children and
adults. The incidence rate is reported to be ~5/1,000,000 people
annually (1–4). According to a previous study, the sex
distribution is approximately equal, with a slight female
predominance (4). The appearance of
the tumor depends on the stage of the disease, since the tumor
progresses slowly over a long period of time prior to entering a
rapid growth phase (5). Genetically,
DFSP is characterized by a reciprocal translocation
t(17;22)(q22;q13), or more often as a supernumerary ring chromosome
involving chromosomes 17 and 22. This translocation mechanism
results in the transcriptional upregulation of the platelet derived
growth factor subunit B (PDGFB) gene, in the form of a
collagen type I α 1 chain-PDGFB fusion oncogene (1,2,5). Patients often ignore these tumors due to
their slow growth. DFSP breast involvement is rare, and is often
misdiagnosed as a benign breast tumor, which delays treatment
(3–5).
In the present study, a case report of a woman with locally
advanced DFSP of the breast is discussed.
Case report
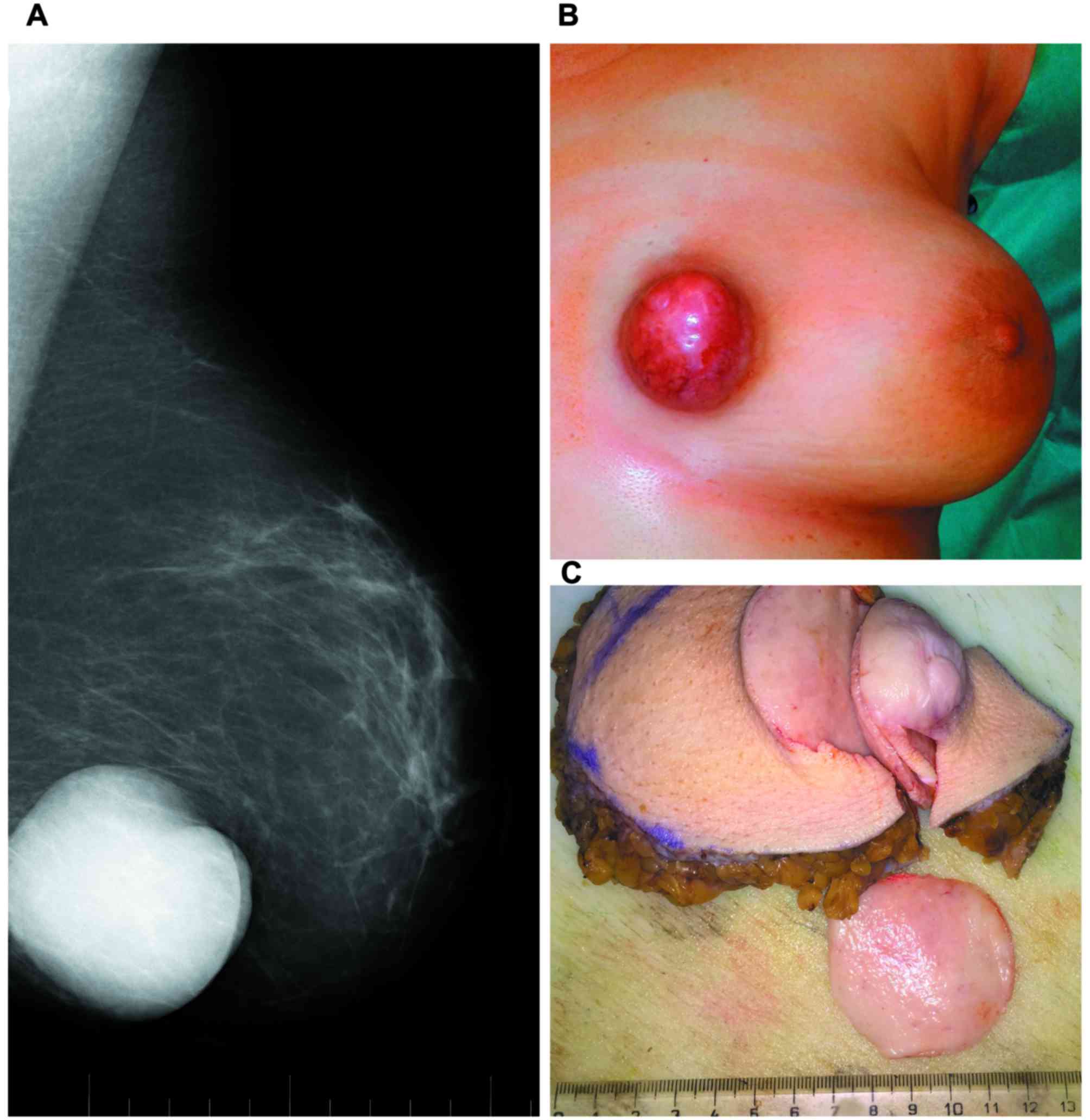
A 43-year-old Caucasian premenopausal woman with no
previous medical history was referred to the Breast Unit of the
Second Department of Gynecology and Obstetrics at the University
Hospital of Bratislava (Bratislava, Slovakia) in May 2016, due to
the growth of a lump in the left breast. Physical examination
revealed a superficial skin-infiltrating, prominent 6-cm lump
located at the border of the medial quadrants of the left breast
(Fig. 1). The lump was painless and
not adherent to the deep layers. Mammography suggested a
circumscribed round and partially lobulated radiopaque lesion with
sharp contours. The patient underwent wide excision of the tumor
with sentinel lymphadenectomy. Gross examination revealed a
12.0×9.0×8.0-cm segment of breast tissue with an unencapsulated
circumscribed 6.2×6.2×5.0-cm tumor with suspicious skin
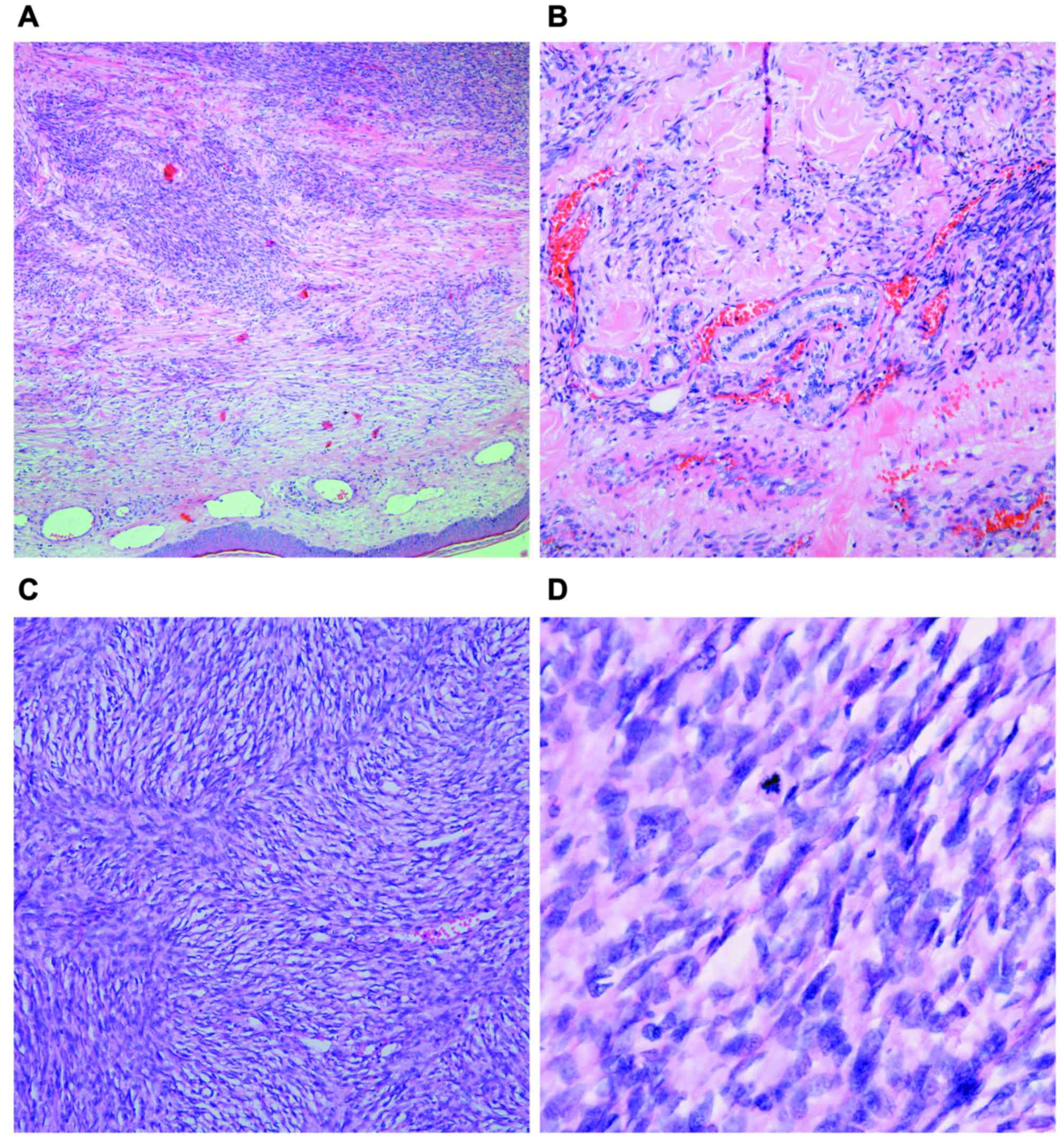
infiltration. Histologically, it was defined as a low-grade
mesenchymal tumor that had fish-bone arrayed spindled fibroblastic
cells with low/medium nuclear polymorphism, thin-walled vessels
without an epithelial component and high mitotic activity (10–12
mitotic figures/10 high-power fields). A prominent storiform
cellular pattern was present (Fig.
2). The nine sentinel lymph nodes tested negative for
metastases. The patient provided written informed consent with
medical procedures, photographs and publication of results.
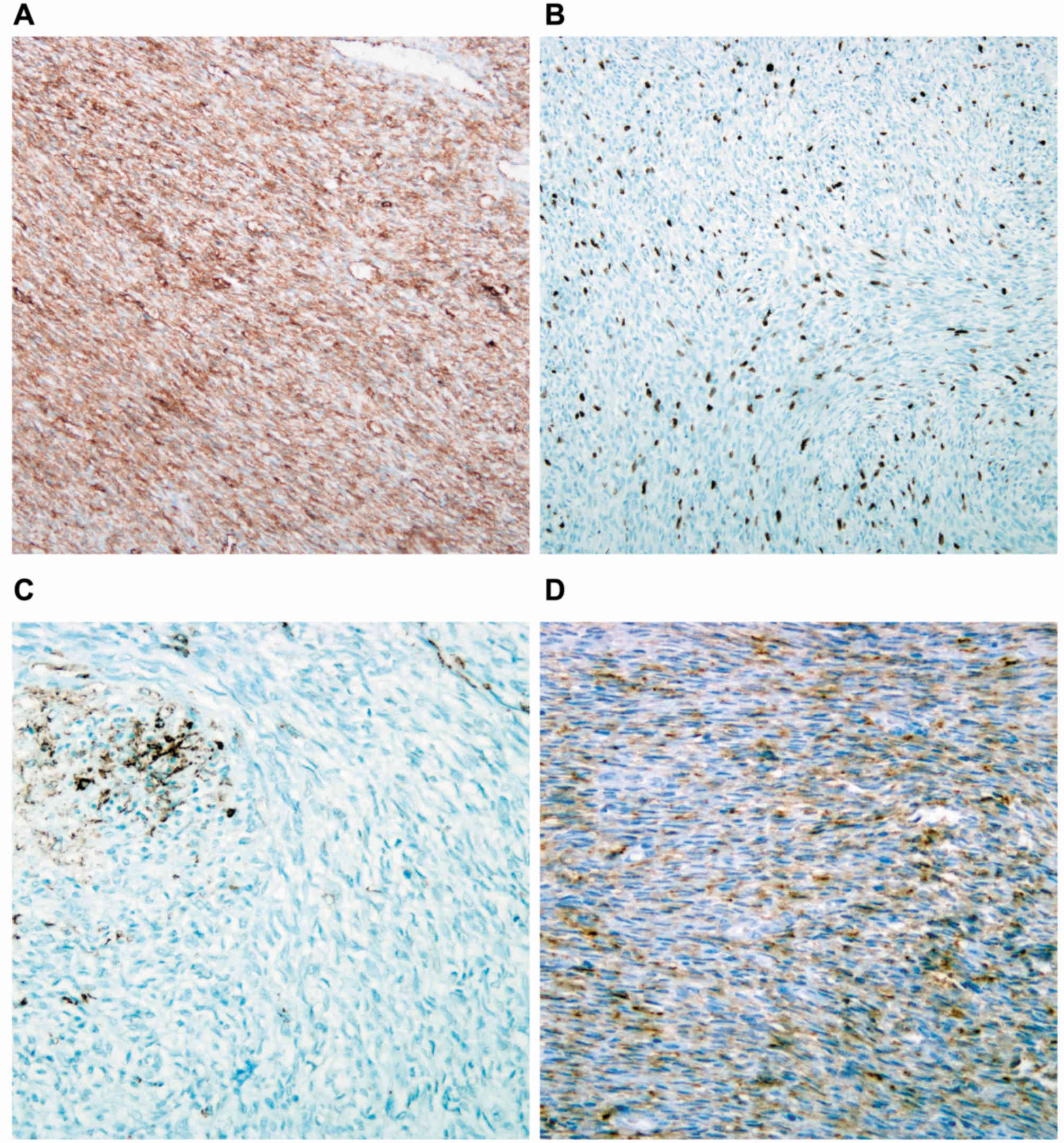
Immunohistochemical (IHC) analysis of the tumor with
anti-cluster of differentiation (CD)34 (mouse monoclonal antibody;
clone QBEud/10; cat. no., 790-2927; Ventana Medical Systems, Inc.,
Tucson, USA; ready to use; incubation time 24 min at 36°C) and
anti-CD10 (mouse monoclonal antibody; clone 56C6; cat. no.,
CMC11021040; Cell Marque™, Rocklin, USA; dilution 1:100; incubation
time 32 min at 36°C) was provided as specified elsewhere (5). It demonstrated positive results
(Fig. 3). The tissue was negative for
cytokeratins (CK)AE1/3 (anti-Pan Keratin (AE1/AE3/PCK26) primary
mouse antibody; cat. no., 760-2135; Ventana Medical Systems, Inc.;
ready to use; incubation 24 min at 36°C), cytokeratin 7
(Novocastra™ liquid mouse monoclonal antibody; clone RN7; cat. no.,
NCL-L-CK7-560; Leica Biosystems GmbH, Nussloch, Germany; dilution
1:300, incubation 36 min at 25°C), cytokeratins 8/18 (mouse
monoclonal antibodies; clone B22.1 & B23.1; cat. no.,
CMC81829040; Cell Marque™; dilution 1:500; incubation time 36 min
at 36°C), cytokeratin 19 (monoclonal mouse antibody; clone RCK108;
cat. no., M0888; Dako A/S; Agilent Technologies, Inc., Santa Clara,
CA, USA; dilution 1:100; incubation time 32 min at 36°C), S100
protein (mouse monoclonal antibody; clone 4C4.9; cat. no.,
CMC33021050; Cell Marque™; dilution 1:200; incubation time 16 min,
36°C), desmin filament (mouse monoclonal antibody; clone D33; cat.
no., 243M-18, Cell Marque™; dilution 1:100; incubation time 36 min
at 36°C), epithelial membrane antigen (EMA; mouse monoclonal
antibody; clone E29; cat. no., CMC24729021; Cell Marque™; dilution
1:200; incubation time 32 min at 36°C), estrogen and progesterone
receptors (rabbit monoclonal primary antibodies; clones SP1 and
1E2; cat. nos., 790-4324 and 790-2223; Ventana Medical Systems,
Inc.; ready to use; incubation time 32 min at 36°C) and cytoplasmic
staining with h-caldesmon (mouse primary monoclonal antibody; clone
h-CD; cat. no., M3557; Dako A/S; Agilent Technologies, Inc.;
dilution 1:200; incubation time 28 min at 36°C). In addition, the
tumor was negative for apoptosis regulator B cell lymphoma-2
(anti-bcl-2 primary mouse monoclonal antibody; clone 124; cat. no.,
790-4464; Ventana Medical Systems, Inc.; ready to use; incubation
time 24 min at 36°C), tumor protein p53 (anti-p53 primary antibody;
clone DO-7; cat. no., 790-2912; ready to use; incubation time 32
min at 36°C), cell surface glycoprotein CD99 (Dako CD99 mouse
monoclonal antibody; clone 12E7; cat. no., M3601; Dako A/S; Agilent
Technologies, Inc.; dilution 1:200; incubation time 24 min at
36°C), cell adhesion molecule CD31 (anti-human CD31 mouse
monoclonal antibody; clone JC70A; cat. no., M0823, Dako A/S;
Agilent Technologies, Inc.; dilution 1:200; incubation time 36 min
at 36°C) and stem cell factor receptor CD117 (c-kit rabbit
monoclonal primary antibody; clone YR145; cat. no., 117-R1; Cell
Marque™; dilution 1:800; incubation time 28 min at 36°C). The IHC
procedures were carried out on the BenchMark XT fully-automated
IHC/ISH staining slide system (Ventana Medical Systems, Inc.). The
Ki67 proliferation index, evaluated according to the protocol of
Knutsvik et al (6), was 10%
(Fig. 3). A differential diagnosis of
a solid fibrous tumor, dermatofibrosarcoma protuberans, or a
spindle cell pleomorphic lipoma was considered, and the case was
referred to a breast pathology specialist (Z.K.). Additional
cytogenetic evaluations of collagen type I α 1 chain
(COL1A1)/platelet derived growth factor subunit B
(PDGFB) gene translocation were performed (P.G.).
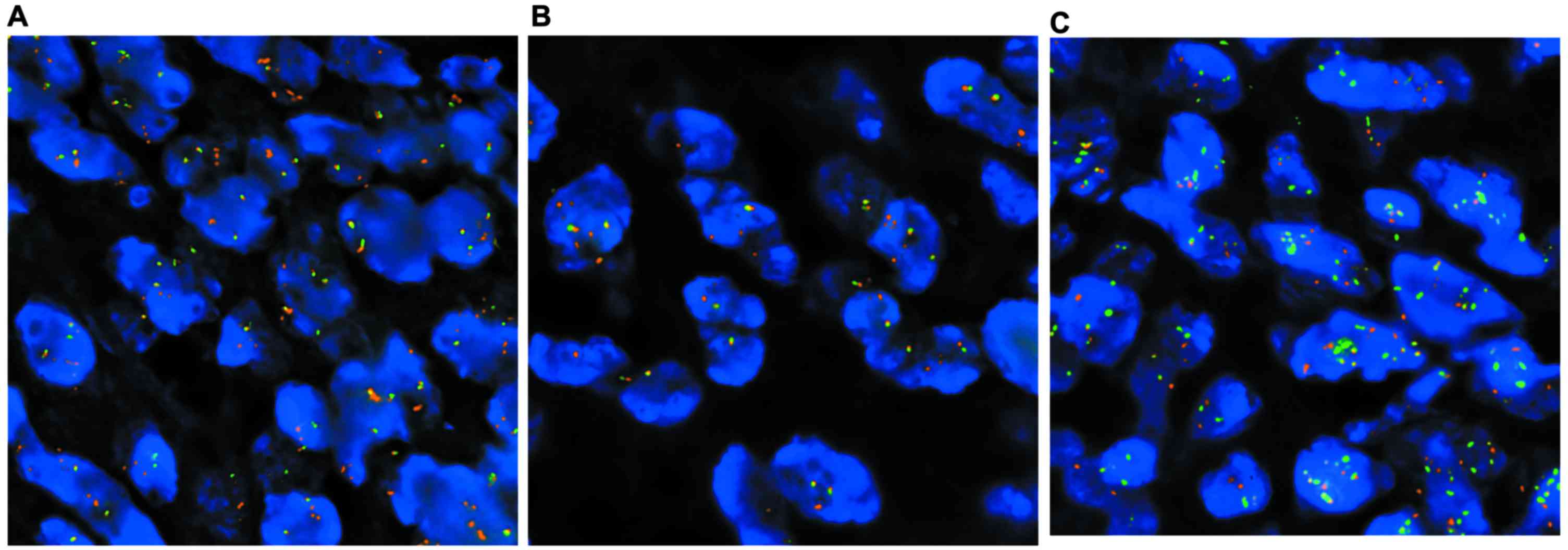
Fluorescence in situ hybridization
(FISH)
The molecular cytogenetic detection of
t(17;22)(q22;q13) was performed in formalin-fixed paraffin-embedded
(FFPE) tissues via FISH. Tissue was fixed in 10% formalin at
room temperature for 24 h. Sections of FFPE tissue measuring 4 µm
in thickness were placed on positively charged slides. Hematoxylin
and eosin stained slides were examined to determine areas for cell
counting. The unstained slides were routinely deparaffinized in
xylene, incubated in 1X Target Retrieval Solution Citrate (pH 6;
Dako; Agilent Technologies, Inc., Santa Clara, CA, USA) for 40 min
at 95°C, then digested in 0.5 mg/ml pepsin solution (Sigma Aldrich;
Merck KGaA, Darmstadt, Germany) in 0.01 M HCl at 37°C for 25 min. A
total of 10 µl factory premixed probes ZytoLight® SPEC
COL1A1 Dual Color Break Apart Probe, ZytoLight® SPEC
PDGFB Dual Color Break Apart Probe and ZytoLight® SPEC
COL1A1/PDGFB Dual Color Dual Fusion Probe (ZytoVision GmbH,
Bremerhaven, Germany) were applied on specimens separately. The
slides were incubated using a ThermoBrite instrument (StatSpin/Iris
Sample Processing, Westwood, MA, USA) at 85°C for 8 min and then
37°C for 16 h. Subsequently, slides were washed in 2X SSC/0.3%
NP-40 solution at 72°C for 2 min and counterstained with DAPI
(Abbott Molecular, IL, USA). This analysis revealed COL1A1/PDGFB
fusion and confirmed the diagnosis of DFSP (Fig. 4). Following extensive serial
sectioning of the tumor and immunohistochemistry, no signs of
malignant transformation to a low-grade fibrosarcoma were
identified. The patient has been followed up and has continued
without clinical signs of disease recurrence. At the time of
writing the present report, it had been >6 months since the
initial surgery and the patient had remained disease free.
Discussion
DFSP was first described by Darier and Ferrand
(7) in 1924, and was termed by
Hoffmann (8) in 1925. In 1962, Taylor
and Helwig (9) described, in a review
of 115 cases, the histologic characteristics of the neoplasia in
detail, and characterized it as a fibroblastic growth appearing as
a low-grade sarcoma. DFSP typically occurs in the dermis and
subcutis rather than in deeper soft tissue. Due to the rarity of
breast DFSP cases, this condition is difficult to diagnose.
Conventional mammography usually reveals a subcutaneous oval mass
with smooth, well-defined margins (2–10).
Magnetic resonance imaging (MRI) may be necessary for the
localization and differential diagnosis of DFSP, and is
particularly useful when primary DFSP is located in areas other
than the head, neck and upper part of the thorax (10–13). Chen
et al (10) described the MRI
appearance of DFSP in a male breast as a well-defined lesion that
has prolonged T1 and T2 relaxation times. On T1-weighted imaging,
the tumor was isointense, slightly hypointense or hyperintense
compared with that in skeletal muscle. In a review by Millare et
al (12), all 14 MRI T1-imaged
lesions were demonstrated to be isointense compared with those in
muscle tissue. In a study by Jiang et al (2), targeted ultrasound of the breast
revealed a hypoechoic mass lesion with irregular borders and no
peripheral or internal blood flow. As DFSP metastasizes in 2–5% of
cases, extensive evaluations with computed tomography scans and
laboratory tests are not usually recommended (5,13).
Generally, imaging results for DFSP are nonspecific, but they may
aid in defining the diagnosis in an appropriate clinical setting
(11–13).
Histologic classification recognizes several
subtypes of DFSP: Pigmented (Bednar tumor), giant cell
fibroblastoma-like, atrophic, sclerosing, granular cell variant,
fibrosarcomatous and myxoid DFSP (5).
A definitive diagnosis of DFSP is usually established on the basis
of routine histopathological and immunohistochemical features.
Immunohistochemical expression of CD34 has been considered as a
diagnostic marker for DFSP. CD34 is expressed in 80–100% of DFSP
tumors (5,8,14,15). Factor XIIIa is useful in the
differential diagnosis between DFSP and cellular fibrous
histiocytoma (15). Novel
immunohistochemical markers have been identified for use in
differential diagnosis, including stromelysin III, apolipoprotein
D, nestin and CD163 (5,16). Despite the presence of a
fibrosarcomatous component in DFSP, DFSP differs from breast
sarcoma in its cutaneous derivation (15–19).
Fine-needle aspiration cytology has low diagnostic accuracy for
mesenchymal breast tumor. Core biopsy is considered the optimal
procedure for diagnosing such tumors, though adjunctive
immunohistochemical analysis is often required (18–21).
However, a diagnosis from a core biopsy is often difficult. The
differential diagnosis of solitary fibrous tumors (SFTs) is
expansive, and a diagnosis based on core biopsy specimens can be
challenging, since certain distinctive features of SFT, including
alternating cellular and hypocellular architecture, and vascular
pattern, may not be appreciable (15,19,21).
Genetically, DFSP is characterized by a reciprocal
translocation t(17;22)(q22;q13), or more often, as a supernumerary
ring chromosome involving chromosomes 17 and 22 (21–23). These
chromosomal rearrangements result in the fusion of the
COL1A1 gene in chromosome bands 17q21 and 33 with the
PDGFB gene in chromosome 22q13 (22). The main consequence of the
t(17;22)(q22;q13) translocation is the overproduction of PDGFB by
tumor cells, which leads to a constitutive activation of the PDGFB
receptor, which is a type III tyrosine kinase receptor (23). The t(17;22)(q22;q13) translocation can
be detected either by FISH on interphase nuclei and/or by multiplex
reverse transcription-polymerase chain reaction, which can be used
to detect COL1A1/PDGFB fusion transcripts (5,21–24).
Complete surgical resection is accepted as the
optimal local treatment for DFSP. However, the minimum resection
margin required to achieve local control remains undefined
(25–27). When DFSP has been excised with close
margins, the local recurrence rates range between 26 and 60%.
Following wide local excision (2–3 cm), reported local recurrence
rates are lower (0–30%) (25–27). Farma et al (26) suggested that with the use of a
standardized surgical approach, including a meticulous pathological
evaluation of margins, a low recurrence rate (1%) was achievable
with relatively narrow margins (median size, 2 cm), allowing
primary closure in 69% of patients. DFSP is considered to be
radiosensitive, although the role of adjuvant radiotherapy in
treating this neoplasm remains uncertain (28).
As mentioned above, the main consequence of the
t(17;22)(q22;q13) in DFSP is the overproduction of PDGFB by the
tumor cells, which leads to the constitutive activation of the
PDGFB receptor (5,22). The PDGFB receptor has tyrosine kinase
activity and activates various intracellular signaling pathways
(5,21–24).
Imatinib mesylate (STI571; Gleevec®; Novartis
International AG, Basel, Switzerland), a tyrosine kinase inhibitor,
was used in the Imatinib Target Exploration Consortium Study B2225
(24), where 10 assessable patients
were treated with the drug. The results demonstrated that imatinib
may assist in disease control in patients with locally advanced or
metastatic disease. In 4 patients, imatinib therapy produced
substantial regression of locally advanced tumors prior to surgical
resection. However, fibrosarcomatous variants of DFSP lacking
t(17;22) may not respond to imatinib (22,24,27,29).
Fields et al (27) analyzed
the therapy results from 244 patients with DFSP following a median
follow-up of 50 months. It was concluded that primary or recurrent
treatment of DFSP should be excision with negative margins, which
should result in low recurrence rates and infrequent metastatic
spread. Multimodality treatment, particularly the use of tyrosine
kinase inhibitors, could be effective, but should not be considered
as curative (5,18,21,24–29).
DFSP follow-ups subsequent to surgery are recommended for a minimum
of 3 years, in 6-month intervals (18).
In conclusion, DFSP is a rare breast neoplasm.
Despite its classification as a tumor of intermediate malignancy
with a limited potential for metastasis, DFSP does possess the
potential for aggressive local behavior. Complete surgical
resection is accepted as the optimal local treatment for DFSP.
Imatinib may assist in disease control in patients with locally
advanced or metastatic disease. Due to the rare involvement of the
breast in patients with DFSP, the present study reports this unique
case with the clinical features and histological and cytogenetic
findings.
References
|
1
|
Lemm D, Mügge LO, Mentzel T and Höffken K:
Current treatment options in dermatofibrosarcoma protuberans. J
Cancer Res Clin Oncol. 135:653–665. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jiang J, Huang Z, Wang LH, Shen SD and Lu
H: Dermatofibrosarcoma protuberans of the breast: A case report.
Oncol Lett. 8:1202–1204. 2014.PubMed/NCBI
|
|
3
|
Sin FN and Wong KW: Dermatofibrosarcoma
protuberans of the breast: A case report. Clin Imaging. 35:398–400.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Criscione VD and Weinstock MA: Descriptive
epidemiology of dermatofibrosarcoma protuberans in the United
States, 1973 to 2002. J Am Acad Dermatol. 56:968–973. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Llombart B, Serra-Guillén C, Monteagudo C,
López Guerrero JA and Sanmartín O: Dermatofibrosarcoma protuberans:
A comprehensive review and update on diagnosis and management.
Semin Diagn Pathol. 30:13–28. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Knutsvik G, Stefansson IM, Azis S, Arnes
J, Eide J, Collett K and Akslen L: Evaluation of Ki67 expression
across distinct categories of breast cancer specimens: A
population-based study of matched surgical specimens, core needle
biopsies and tissue microarrays. PLoS One. 9:e1121212014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Darier S and Ferrand M: Recurrent or
progressive dermatofibromas and fibrosarcoma of the skin. Ann
Dermatol Venerol. 5:545–562. 1924.(In French).
|
|
8
|
Hoffman E: Ueber das knollentribende
Fibrosarkom der Haut (dermatofibrosarcoma protuberans). Dermatol Z.
43:1–286. 1925.(In German). View Article : Google Scholar
|
|
9
|
Taylor HB and Helwig EB:
Dermatofibrosarcoma protuberans. A study of 115 cases. Cancer.
15:717–725. 1962. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen X, Chen YH, Zhang YL, Guo YM, Bai ZL
and Zhao X: Magnetic resonance imaging and mammographic appearance
of dermatofibrosarcoma protuberans in a male breast: A case report
and literature review. J Med Case Rep. 3:82462009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Serra-Guillén C, Sanmartín O, Llombart B,
Nagore E, Deltoro C, Martín I, Borella-Estrada R, Requena C,
Martorell-Calatayud A, Cervera J and Guillén C: Correlation between
preoperative magnetic resonance imaging and surgical margins with
modified Mohs for dermatofibrosarcoma protuberans. Dermatol Surg.
37:1638–1645. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Millare GG, Guha-Thakurta N, Sturgis EM,
El-Naggar AK and Debnam JM: Imaging findings of head and neck
dermatofibrosarcoma protuberans. AJNR Am J Neuroradiol. 35:373–378.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang L, Liu QY, Cao Y, Zhong JS and Zhang
WD: Dermatofibrosarcoma protuberans: Computed tomography and
magnetic resonance imaging findings. Medicine (Baltimore).
94:e10012015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chang GK, Jacobs IA and Salti GI: Outcomes
of surgery for dermatofibrosarcoma protuberans. Eur J Surg Oncol.
30:341–345. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li N, McNiff J, Hui P, Manfioletti G and
Tallini G: Differential expression of HMGA1 and HMGA2 in
dermatofibroma and dermatofibrosarcoma protuberans: Potential
diagnostic applications and comparison with histologic findings,
CD34, and factor XIIIa immunoreactivity. Am J Dermatopathol.
26:267–272. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Thway K, Ng W, Noujaim J, Jones RL and
Fisher C: The current status of solitary fibrous tumor: Diagnostic
features, variants and genetics. Int J Surg Pathol. 24:281–292.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Stacchiotti S, Pedeutour F, Negri T, Conca
E, Marrari A, Palassini E, Collini P, Keslair F, Morosi C, Gronchi
A, et al: Dermatofibrosarcoma protuberans-derived fibrosarcoma:
Clinical history, biological profile and sensitivity to imatinib.
Int J Cancer. 129:1761–1772. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kuzel P, Mahmood MN, Metelitsa AI and
Salopek TG: A clinicopathologic review of a case series of
dermatofibrosarcoma protuberans with fibrosarcomatous
differentiation. J Cutan Med Surg. 19:28–34. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lim SZ, Ong KW, Tee Tan BK, Selvarajan S
and Tan P Hoon: Sarcoma of the breast: An update on a rare entity.
J Clin Pathol. 69:373–381. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Al Barwani AS, Taif S, Al Mazrouai RA, Al
Muzahmi KS and Alrawi A: Dermatofibrosarcoma protuberans: Insights
into a rare soft tissue tumor. J Clin Imaging Sci. 6:162016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Llombart B, Monteagudo C, Sanmartín O,
López-Guerrero JA, Serra-Guillén C, Poveda A, Jorda E,
Fernandez-Serra A, Pellín A, Guillén C and Llombart-Bosch A:
Dermatofibrosarcoma protuberans: A clinicopathological,
immunohistochemical, genetic (COL1A1-PDGFB), and therapeutic study
of low-grade versus high-grade (fibrosarcomatous) tumors. J Am Acad
Dermatol. 65:564–575. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Simon MP, Navarro M, Roux D and Pouysségur
J: Structural and functional analysis of a chimeric protein
COL1A1-PDGFB generated by the translocation t(17; 22)(q22;q13.1) in
dematofibrosarcoma protubrans (DP). Oncogene. 20:2965–2975. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Giacchero D, Maire G, Nuin PA, Berthier F,
Ebran N, Carlotti A, Celerier P, Coindre JM, Esteve E, Fraitag S,
et al: No correlation between the molecular subtype of COL1A1-PDGFB
fusion gene and the clinicohistopathological features of
dermatofibrosarcoma protuberans. J Invest Dermatol. 130:904–907.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
McArthur GA, Demetri GD, van Oosterom A,
Heinrich MC, Debiec-Rychter M, Corless CL, Nikolova Z, Dimitrijevic
S and Fletcher JA: Molecular and clinical analysis of locally
advanced dermatofibrosarcoma protuberans treated with imatinib:
Imatinib target exploration consortium study B2225. J Clin Oncol.
23:866–873. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Snow SN, Gordon EM, Larson PO, Bagheri MM,
Bentz ML and Sable DB: Dermatofibrosarcoma protuberans: A report on
29 patients treated by Mohs micrographic surgery with long-term
follow-up and review of the literature. Cancer. 101:28–38. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Farma JM, Ammori JB, Zager JS, Marzban SS,
Bui MM, Bichakjian CK, Johnson TM, Lowe L, Sabel MS, Wong SL, et
al: Dermatofibrosarcoma protuberans: How wide should we resect? Ann
Surg Oncol. 17:2112–2118. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fields RC, Hameed M, Qin LX, Moraco N, Jia
X, Maki RG, Singer S and Brennan MF: Dermatofibrosarcoma
protuberans (DFSP): Predictors of recurrence and the use of
systemic therapy. Ann Surg Oncol. 18:328–336. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Williams N, Morris CG, Kirwan JM, Dagan R
and Mendenhall WM: Radiotherapy for dermatofibrosarcoma
protuberans. Am J Clin Oncol. 37:430–432. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Eilers G, Czaplinski JT, Mayeda M, Bahri
N, Tao D, Zhu M, Hornick JL, Lindeman NI, Sicinska E, Wagner AJ, et
al: CDKN2A/p16 Loss implicates CDK4 as a therapeutic target in
imatinib-resistant dermatofibrosarcoma protuberans. Mol Cancer
Ther. 14:1346–1353. 2015. View Article : Google Scholar : PubMed/NCBI
|