Introduction
Malignant breast tumors represent one of the most
commonly occurring cancers in women, and are a leading cause of
cancer-associated mortality (1).
While advances in surgery, radiotherapy, chemotherapy and hormone
replacement therapy have irrefutably enhanced early diagnosis and
treatment, no effective therapy exists for advanced, invasive,
metastatic breast cancer (2). Strong
evidence for the effectiveness of immunotherapy has been provided
in previous reports, and this approach is expected to be effective
in such cases (3). However, the
majority of cancer immunotherapies that have been developed in
experimental animal models and have been tested in clinical trials
have not been effective, although certain treatments have
demonstrated modest clinical effects (4–7). Previous
studies have identified cells of myeloid origin that suppress tumor
immunity, making them an impediment to cancer immunotherapy. These
suppressive myeloid cells were initially described in patients with
cancer six decades ago (8,9), and the importance of their function in
the immune system has begun to be appreciated (10,11).
Accumulating evidence has demonstrated that myeloid-derived
suppressor cells (MDSCs), a population of cells with suppressive
activity, contribute to the negative regulation of immune responses
that occurs in diseases including cancer. MDSCs in mice are
characterized by the expression of cell surface molecules that are
detected by antibodies targeting Gr1 and cluster of differentiation
(CD)11b (12,13). MDSC phenotype variation is consistent
with the idea that these cells belong to a diverse family of cells
in various, intermediate stages of myeloid cell differentiation
(12). In humans, MDSCs are defined
as CD14, CD11b cells or, more specifically, as cells expressing the
common myeloid marker CD33 but lacking markers of mature myeloid
and lymphoid cells and the MHC class II molecule HLA-DR (14). In the present study, CD14−,
CD11b+ and CD33+ cells were considered to be
MDSCs.
In 1986, Mosmann et al (15) described the existence of two types of
T helper (Th) populations; Th1 and Th2. Following T-cell receptor
ligation, Th0 cells differentiate into specific subsets
characterized by their functions and cytokine production profiles.
Th1 lymphocytes are induced by interleukin (IL)-2, tend to produce
IL-12 and interferon (IFN)-γ, and are involved in cellular
immunity. Th2 lymphocytes primarily induce humoral immunity and
produce IL-4, IL-6 and IL-10. The immune function of patients with
cancer, in particular cell-mediated immunity, is known to be
impaired and the Th cell balance during this disease tends to shift
from Th1 to Th2 predominance. In a previous study concerning
gastric and colorectal cancer, the production of IL-12 decreased as
the diseases progressed and production of IFN-γ decreased uniformly
in patients with cancer compared with healthy volunteers (16).
At present, there is a paucity of information
concerning MDSCs in patients with breast cancer, in particular
regarding the relationship of MDSCs with immune status (17). The present study detected MDSCs in
circulating blood from patients with breast cancer and these levels
were analyzed. In addition, MDSCs were also detected in the pleural
effusion of a patient with metastatic breast cancer. Finally, the
effects of chemotherapy on MDSCs were addressed.
Materials and methods
Study subjects
In the present study, a total of 155 patients were
enrolled. Patients were aged between 40 and 84 years (median, 58.0
years) and had histologically confirmed breast cancer that was
treated in the Department of Organ Regulatory Surgery, Fukushima
Medical University (Fukushima, Japan) between January 2011 and June
2016. A total of 110 preoperative patients, including 18 patients
with stage I disease, 39 with stage II, 17 with stage III, and 36
with stage IV cancer; 23 postoperative patients, including 5 with
stage I, 10 with stage II, 7 with stage III, and 1 with stage IV
cancer in accordance with National Comprehensive Cancer Network
(NCCN) Clinical Practice Guidelines in Oncology: Breast Cancer
Screening and Diagnosis (18); 22
recurrent patients that had received a regimen of chemotherapy (6
cycles of 1,000 mg/m2 gemacitabine on days 1 and 8 for
21 days); and 18 healthy volunteers were enrolled. None of the
preoperative patients had received any anticancer treatment. A
total of 177 blood samples were collected from the 155 patients
with breast cancer, including double sampling in recurrent patients
(pre- and post-chemotherapy), and from the 18 healthy volunteers.
Peripheral blood mononuclear cells (PBMCs) were isolated using the
Ficoll density gradient centrifugation method (Ficoll-Hypaque; GE
Healthcare Life Sciences, Chalfont, UK) from 20 ml venous blood
collected in EDTA tubes. Aliquots of PBMCs were cryopreserved in
freezing medium (BLC-1; Juji-Field Co. Ltd, Tokyo, Japan). The
plasma was separated by centrifugation at 1,500 × g for 10 min in a
refrigerated centrifuge at 4°C and kept at −80°C until analysis.
Double samples (pre- and post-chemotherapy) from pleural effusions
were examined. A total of 1×106 cells from 100-ml plural
effusion samples were isolated by centrifugation at 400 × g for 30
min at 4°C using the Ficoll density gradient centrifugation method,
and subjected to flow cytometric analysis as described. The present
study was approved by the Ethics Committee of Fukushima Medical
University (2011–2016). Written informed consent was obtained from
all enrolled patients and healthy donors.
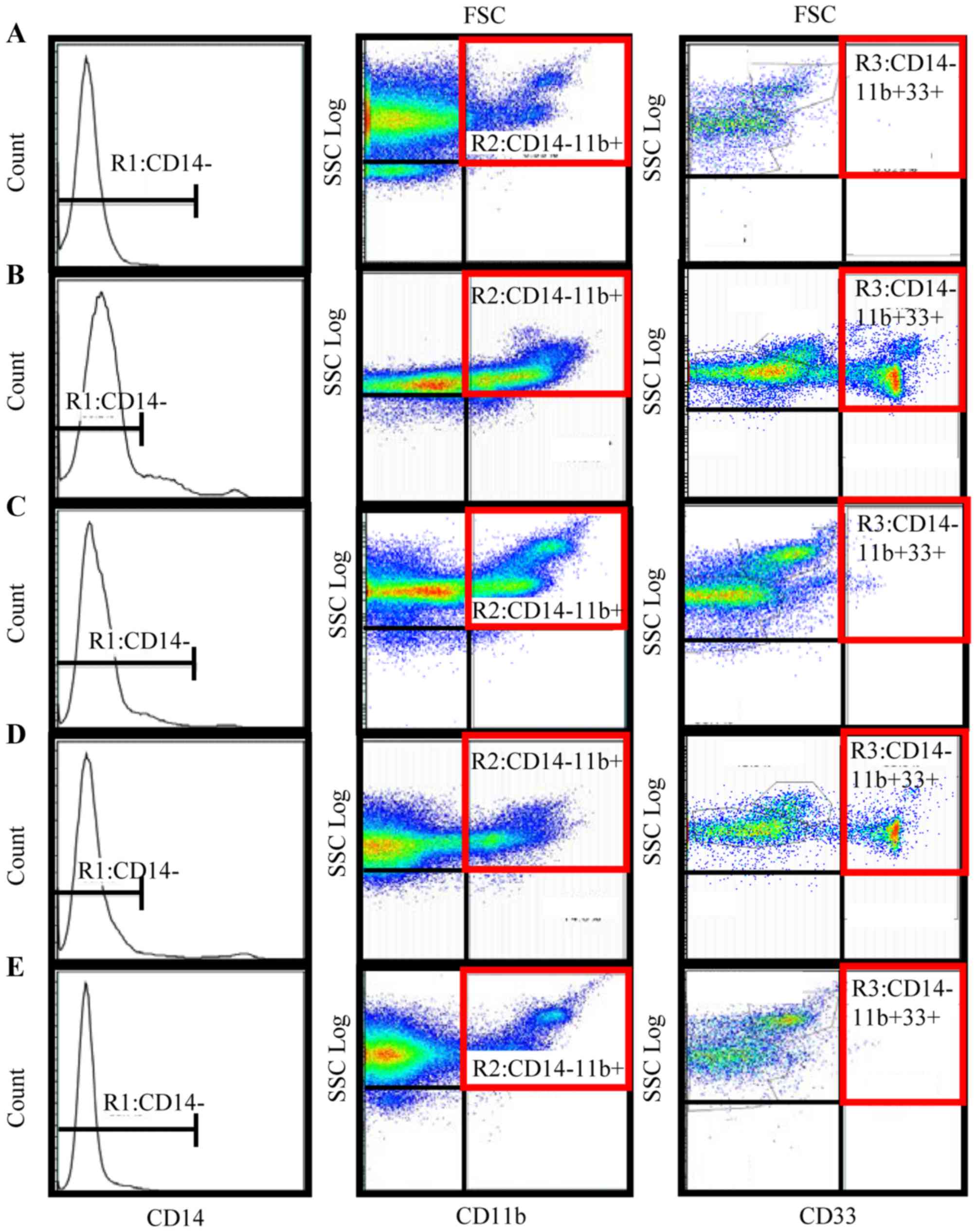
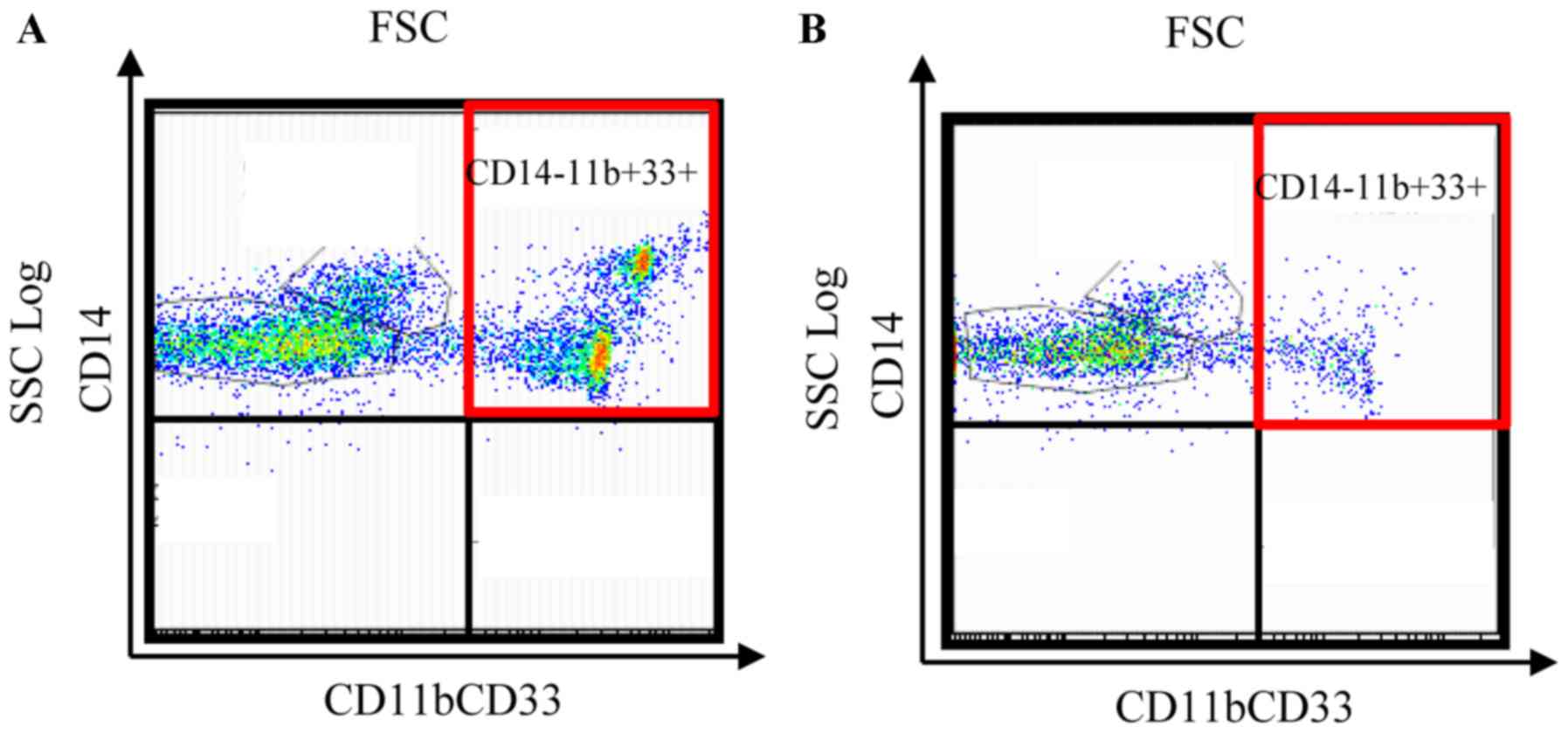
Flow cytometric analysis
A total of 1×106 frozen PBMCs were thawed
rapidly and washed three times with PBS. A three-color flow
cytometric analysis was performed with a cocktail of antibodies,
consisting of fluorescent isothiocyanate (FITC)-conjugated
anti-CD14 (cat. no. ab28061; 20 µl; Abcam, Cambridge, UK),
phycoerythrin (PE)-conjugated anti-CD11b (cat. no. IM-2581 U;
dilution, 0.2 mg/ml; Beckman Coulter, Inc., Brea, CA, USA), and
phycoerythrin cyanin (PC)5.1-conjugated anti-CD33 (cat. no.
FAB1137F; 20 µl; Beckman Coulter, Inc.). Following incubation with
PBS for 30 min at 4°C, samples were washed with
fluorescence-activated cell sorting (FACS) buffer. Pellets were
subsequently resuspended in 800 µl FACS buffer. Data acquisition
and analysis were performed on a FACS Aria II flow cytometer (BD
Biosciences, San Jose, CA, USA; Fig.
1) using Flow Jo v10.2 software (Tree Star, Inc., Ashland, OR,
USA). The labeled cells were first gated (R1) based on their
expression of CD14; R1 was composed of CD14− cells. The
fraction of cells in this population that expressed the myeloid
markers CD11b and CD33 was then determined. Therefore, in the
present study, MDSCs were defined as CD14−,
CD11b+ and CD33+ cells. The percentage of
MDSCs was calculated as a percentage of the total PBMCs.
Cytokine production assay
To assess cytokine production, 1×106
PBMCs were cultured in 1 ml RPMI-1640 medium (Wako Pure Chemical
Industries, Ltd., Osaka, Japan) containing 10% heat-inactivated
fetal calf serum (FCS; Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) and 100 µg/ml phytohemagglutinin (PHA;
Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) for 24 h in 5%
CO2 at 37°C. Subsequently, 1×106 PBMCs were
seeded into a 96-well plate (Costar, Lowell, MA, USA) in the
presence of PHA. Following cultivation, IL-6 and IFN-γ in
supernatants were measured using a Quantikine ELISA kit (Human IL-6
immunoassay, cat. no. D6050; Human IFN-γ immunoassay, cat. no.
DIF50), according to the manufacturer's protocol (R&D Systems,
Inc., Minneapolis, MN, USA).
At the same time, 1×106 PBMCs were
cultured in 1 ml RPMI-1640 medium containing 10% heat-inactivated
FCS and 0.075%/vol of Staphylococcus aureus Cowan1 (SAC;
Sigma-Aldrich; Merck KGaA) for 24 h in 5% CO2 at 37°C.
PBMCs (1×106) were then seeded into a 96-well plate in
the presence of SAC. Following cultivation, IL-12 in supernatant
was measured using a Quantikine ELISA kit (Human IL-12 immunoassay,
cat. no. DP400) according to the manufacturer's protocol (R&D
Systems, Inc.). Absorbance at 450 nm was measured using an ELISA
micro plate reader.
Lymphocyte proliferation assay
Lymphocyte proliferation assays were performed using
A total of 1×106 cells/ml were suspended in RPMI-1640
medium containing 20% fetal bovine serum (FBS; Kojin Bio Co., Ltd.,
Saitama, Japan). Following the addition of 100 µg/ml PHA into the
PBMC culture wells, the culture was kept at 37°C in a 5%
CO2 atmosphere and PHA mitogenesis was observed 3 times
for 80 h by a light microscope (magnification, ×10). A total of 10
µl 3H-thymidine (Japan Radioisotope Association, Tokyo,
Japan) was added to the wells (18.5 Beq/well) for the last 72 h of
incubation. Cells were harvested using an auto cell harvester with
a UniFilter Plate (Bio Tec Co., Ltd. Tokyo, Japan) and
3H-thymidine incorporation was determined using a liquid
scintillation counter (PerkinElmer, Inc., Waltham, MA, USA) and was
expressed as counts per minute (cpm). The stimulation index (SI)
was obtained by calculating total cpm/control cpm. The controls
were PBMCs that had not been subjected to PHA addition.
Statistical analysis
All statistical analyses were performed using Excel
Statics 2012 software for Windows (Social Survey Research
Information Co., Ltd. Tokyo, Japan). The differences between groups
were determined using Student's t-tests. Relationships between two
variables were quantified using Spearman's rank correlation
coefficient tests. All data are presented as the mean ± standard
deviation. P<0.05 was considered to indicate a statistically
significant difference. When measuring overall survival (OS),
follow-up data that were not reached as of the last follow-up date
or at 1,500 days were censored. The prognoses of the patients were
analyzed using Kaplan-Meier method curves and the log-rank test was
used to determine the univariate significance of the variables. In
110 patients with preoperative breast cancer, multivariate Cox
regression analysis of survival was performed according to MDSC
levels, tumor size, molecular subtype of the tumor, Ki-67 status,
lymph node status, and histological grading in accordance with NCCN
Clinical Practice Guidelines in Oncology (18). A Cox proportional-hazards model was
used to simultaneously examine the effects of multiple covariates
on survival. The effect of each individual variable was described
by the hazard ratio, with a 95% confidence interval.
Results
MDSC levels in pre- and post-operative
patients, in patients with recurrent breast cancer, and in patients
with recurrent breast cancer following chemotherapy
MDSCs were successfully detected by flow cytometry.
Representative flow cytometric data was obtained for normal healthy
volunteers (Fig. 1A), preoperative
patients (Fig. 1B), postoperative
patients (Fig. 1C), patients with
recurrent breast cancer (Fig. 1D),
and patients receiving gemcitabine (Fig.
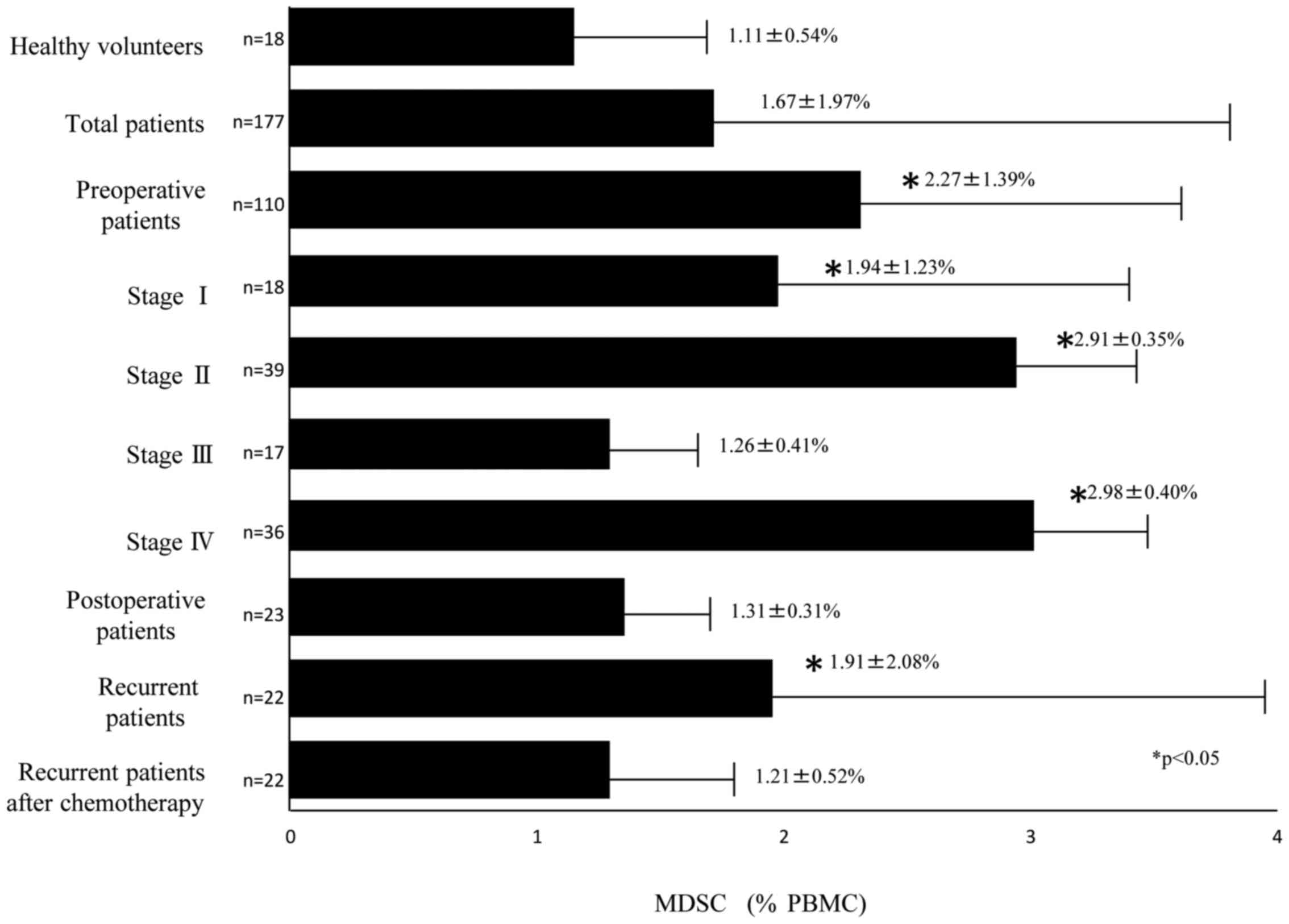
1E). The percentage of MDSCs in the PBMCs of 177 samples from
155 patients with breast cancer and from 18 healthy volunteers was
analyzed. The percentage of MDSCs in the PBMCs from 110
preoperative patients with breast cancer was significantly
increased compared with the 18 healthy volunteers (2.27±1.39 and
1.11±0.54%, respectively; P<0.05; Fig.
2). Of the 110 preoperative patients, the MDSC levels of
patients with stage I, stage II, stage III, and stage IV diseases
were 1.94±1.23, 2.91±0.35, 1.26±0.41 and 2.98±0.40%, respectively,
and those of stage I, stage II, and stage IV were significantly
higher than the levels of healthy volunteers (Fig. 2). The MDSC levels of 23 postoperative
patients, 22 recurrent patients, and 22 recurrent patients who
received chemotherapy were 1.31±0.31, 1.91±2.08, and 1.21±0.52%,
respectively (Fig. 2). The MDSC
levels were also significantly higher in recurrent patients prior
to chemotherapy treatment compared with in healthy volunteers
(P<0.05; Fig. 2). The MDSC levels
of postoperative patients were significantly lower than those of
preoperative patients (P<0.05; Fig.
2) and were equivalent to the range in healthy volunteers. The
MDSC levels of the patients with recurrent breast cancer following
chemotherapy were lower than those in patients with recurrent
breast cancer prior to chemotherapy and were not significantly
different from the levels in healthy volunteers. In summary, the
MDSC levels were increased in preoperative patients, decreased
following removal of the tumor, and increased again with
recurrence. In addition, MDSC levels of patients with recurrent
breast cancer decreased following chemotherapy (Fig. 2).
MDSC levels were correlated with Th2
polarization, malnutrition, inflammation and immune
suppression
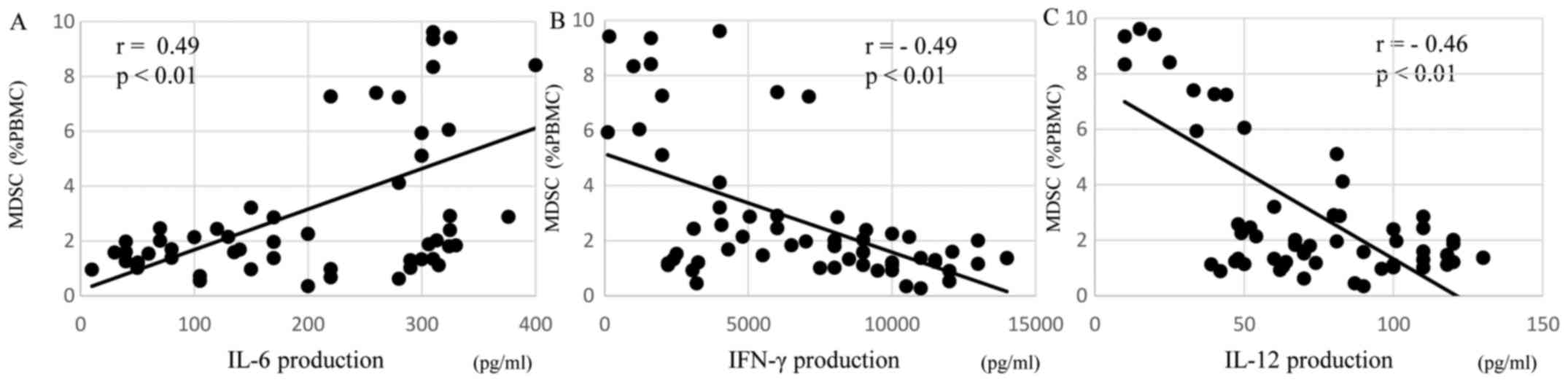
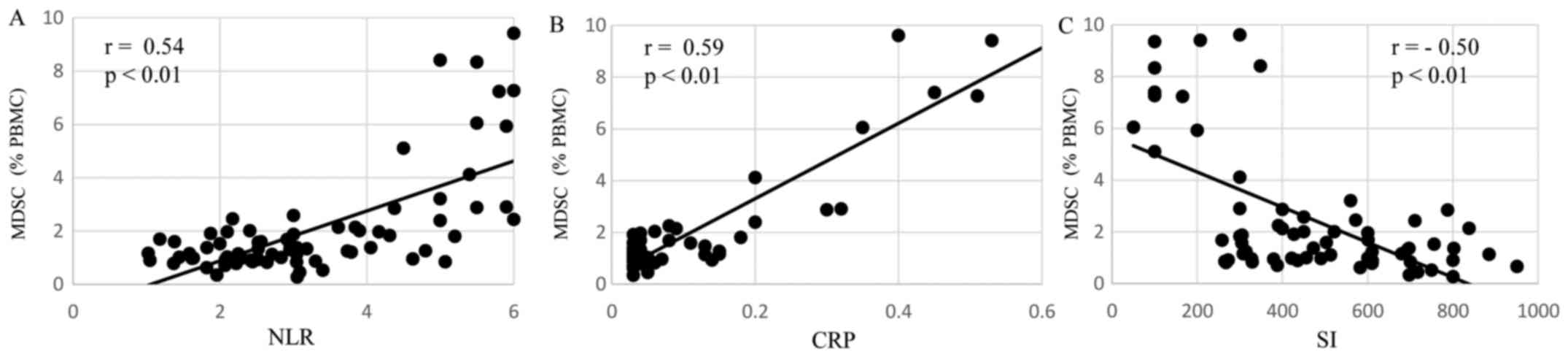
The levels of MDSCs in preoperative patients were
correlated with immune suppression, in particular Th2 polarization,
malnutrition and inflammation. Regarding Th2 polarization, the MDSC
levels of preoperative patients were significantly positively
correlated with IL-6 production (r=0.49, P<0.01; Fig. 3A) and were significantly inversely
correlated with IFN-γ (r=−0.49, P<0.01; Fig. 3B) and IL-12 (r=−0.46, P<0.01;
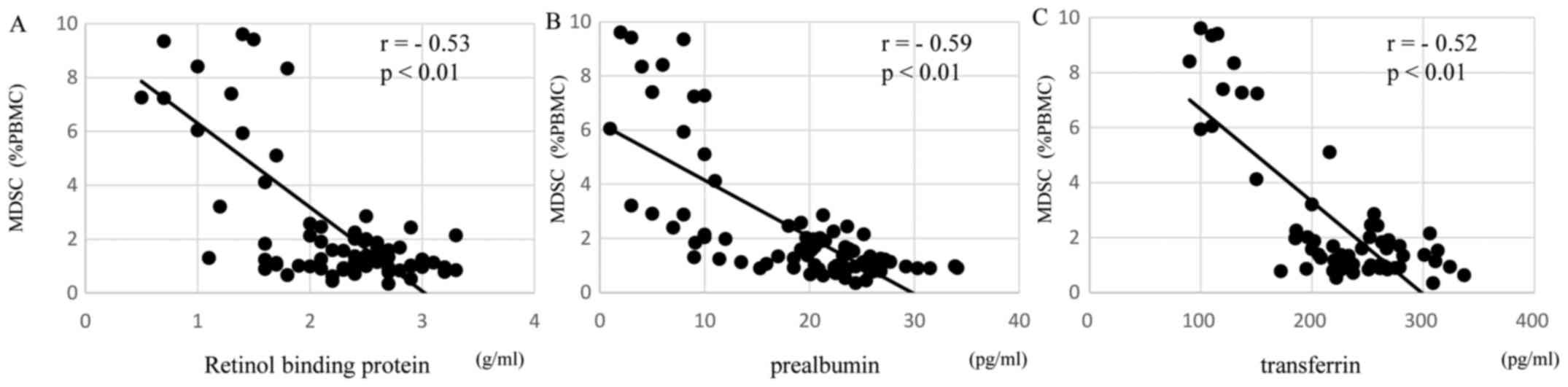
Fig. 3C) production. Regarding
malnutrition, the MDSCs levels of preoperative patients were
significantly negatively correlated with the short turnover
protein: retinol binding protein (r=−0.53, P<0.01; Fig. 4A), prealbumin (r=−0.59, P<0.01;
Fig. 4B), and transferrin (r=−0.52,
P<0.01; Fig. 4C). In terms of
inflammation and the SI, the MDSC levels of preoperative patients
were significantly positively correlated with the
neutrophil/lymphocyte ratio (NLR; r=0.54, P<0.01; Fig. 5A) and C-reactive protein (CRP; r=0.59,
P<0.01; Fig. 5B) and were
significantly negatively correlated with the SI (r=−0.50,
P<0.01; Fig. 5C).
Effect of MDSC levels in patients with
stages I, II, III, and IV breast cancer on overall survival
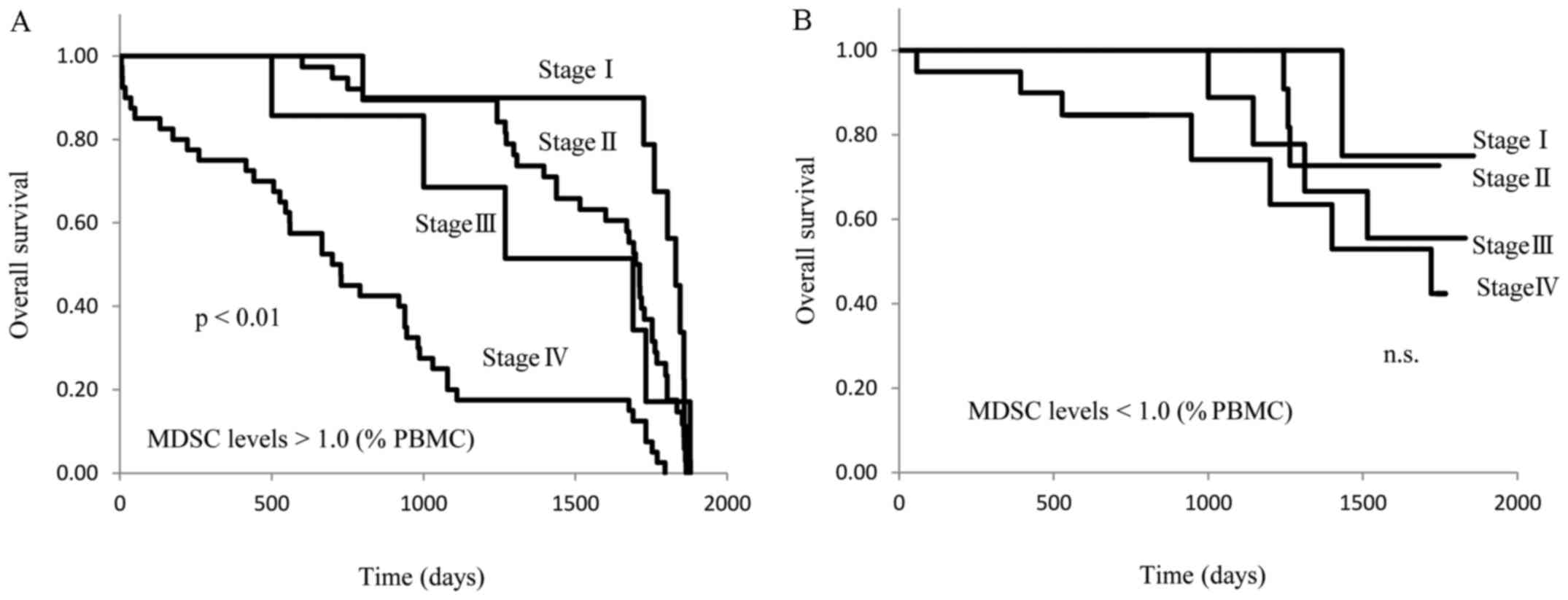
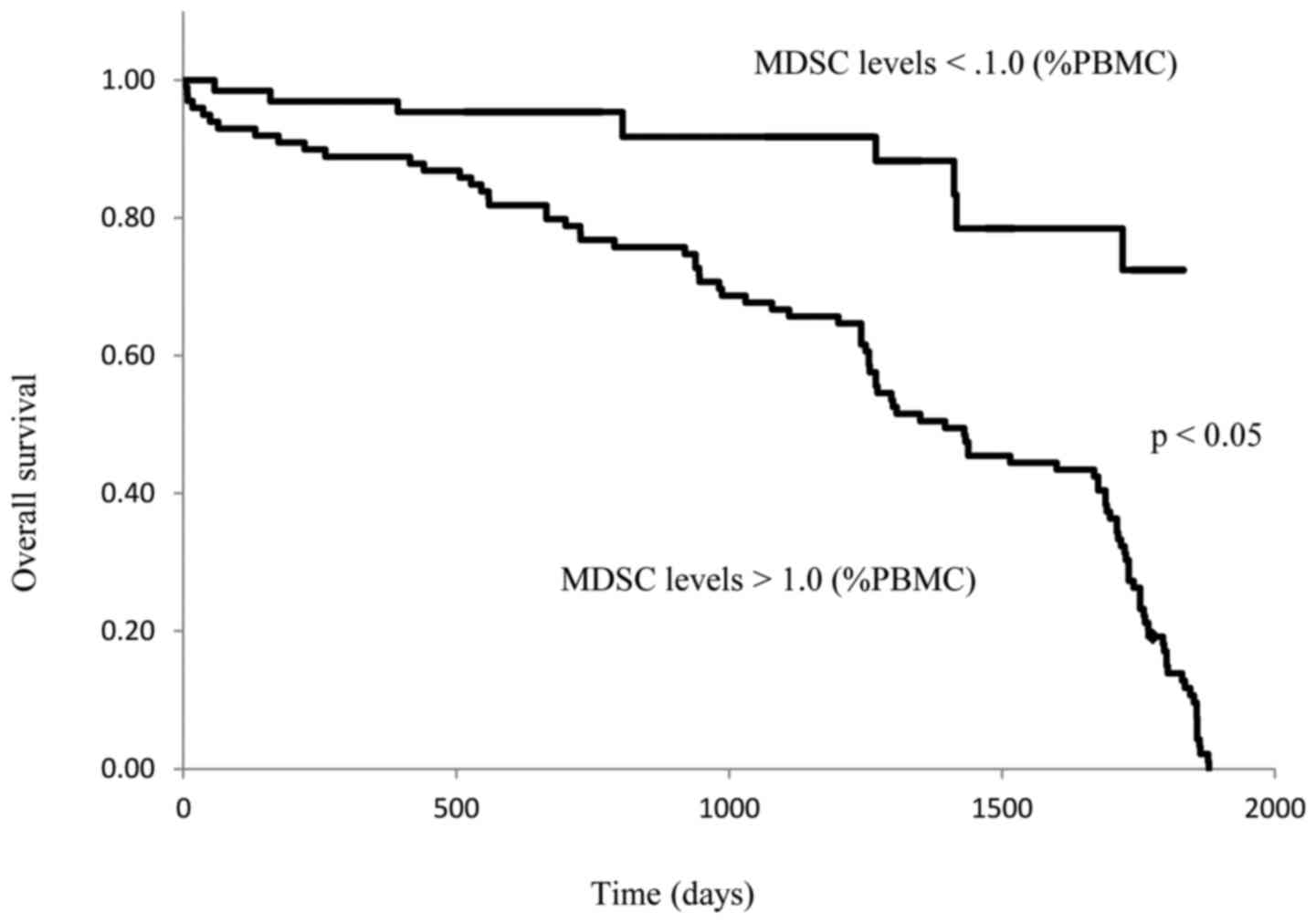
The preoperative patients were separated into 2
groups based on whether their circulating MDSC levels were higher
or lower than 1.0% of total PBMCs. The OS of these 2 groups was
then compared. In patients with MDSC levels >1.0%, the OS of
stage IV disease was significantly shorter than that of stage I,
II, or III disease (P<0.01; Fig.
6A), and no difference in survival was observed between stages
I, II, and III. On the other hand, there were no differences in OS
between stage I–IV breast cancer patients with MDSC levels <1.0%
(Fig. 6B). The OS of stage IV
patients with MDSC levels that were >1.0% was significantly
shorter than that of patients with MDSC levels <1.0% (P<0.05;
Fig. 7).
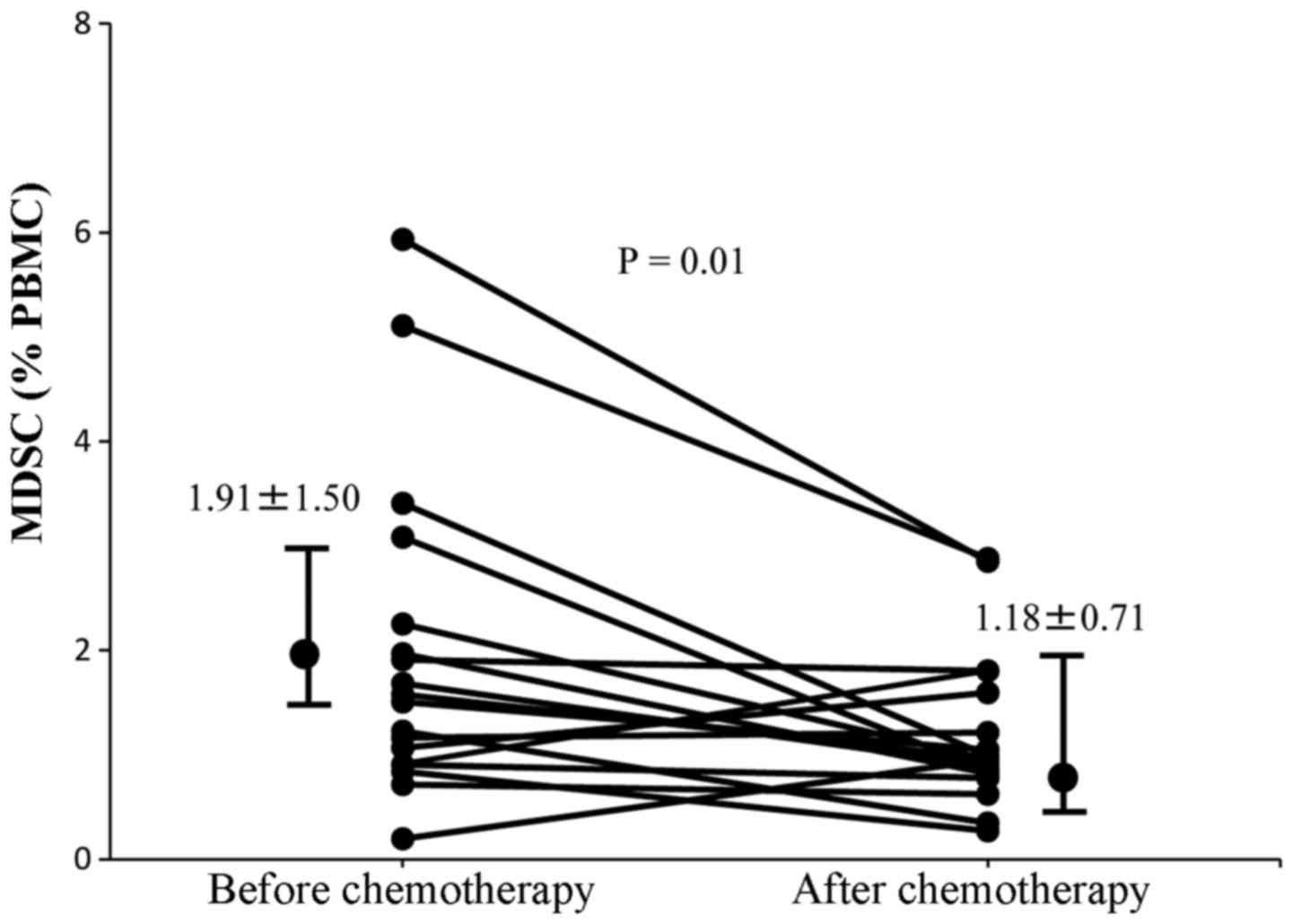
MDSCs and chemotherapy
It has previously been reported that gemcitabine
treatment of tumor-bearing mice significantly inhibited tumor
growth, reduced splenomegaly, and significantly decreased the
proportion of MDSCs in the spleen (19). Patients with recurrent breast cancer
in the present study had received 6 cycles of gemcitabine (1,000
mg/m2). It was therefore determined whether gemcitabine
therapy had altered MDSC levels in these patients. MDSC levels were
analyzed in these patients prior to chemotherapy and 14 days
following the last cycle of chemotherapy. There was a significant
decrease in MDSC levels following chemotherapy compared with those
prior to chemotherapy (1.91±1.50 and 1.18±0.71%, respectively;
P=0.01; Fig. 8).
MDSCs in pleural effusion and the
effect of chemotherapy
A 69-year-old female who had undergone mastectomy
and axillary dissection two years previously was revealed to have
new lung metastasis and pleural effusion. MDSCs were detected in
the pleural effusion using the same experimental procedure as that
described above for PBMCs. The effect of chemotherapy on MDSC
levels was then examined in the pleural effusion of this patient.
MDSC levels in the pleural effusion were decreased from 34.5% prior
to chemotherapy (Fig. 9A) to 11.0%
following 6 cycles of gemcitabine treatment (Fig. 9B). The MDSC levels in the peripheral
blood were also decreased following chemotherapy in this case.
Thus, the level of MDSCs in the pleural effusion and in the PBMCs
decreased in parallel in response to chemotherapy.
Multivariate regression analysis of
survival according to the serum MDSC levels in molecular subtypes
of tumors
The present study then examined whether the
prognostic value of an MDSC level of >1.0% remained
statistically significant in a multivariate analysis in the total
cohort. A multivariate Cox regression model, which included a level
of MDSCs <1.0%, tumor size, molecular subtype of the tumor,
including Luminal A, Luminal B, human epidermal growth factor
receptor 2 or triple negative breast cancer, Ki-67 status, lymph
node status and histological grade was applied. Apart from an MDSC
level of <1.0%, none of the other characteristics were
significantly and independently prognostic in this model (Table I).
 | Table I.Multivariate Cox regression analysis
of survival according to MDSC levels, tumor size, tumor molecular
subtype, Ki-67 status, lymph node status and histological
grade. |
Table I.
Multivariate Cox regression analysis
of survival according to MDSC levels, tumor size, tumor molecular
subtype, Ki-67 status, lymph node status and histological
grade.
| Clinicopathological
characteristic | Number of patients
(n=110) | HR | 95% CI | P-value |
|---|
| MDSCs (% of
PBMCs) |
|
|
|
|
|
<1 | 60 |
|
|
|
| ≥1 | 50 | – | – | <0.05 |
| Tumor size
(mm) |
|
|
|
|
|
<30 | 46 | – | – | – |
|
≥30 | 64 | 1.05 | 0.77–1.21 | <0.10 |
| Molecular
subtype |
|
|
|
|
| Luminal
A | 41 | − | − | − |
| Luminal
B | 27 | 1.26 | 1.14–1.61 | <0.10 |
|
HER2 | 15 | 1.14 | 0.95–1.39 | <0.10 |
|
TNBC | 17 | 1.25 | 1.11–1.58 | <0.10 |
| Ki-67 (%) |
|
|
|
|
|
<50 | 32 | – | – | – |
|
≥50 | 78 | 1.18 | 0.97–1.40 | <0.10 |
| Lymph node
status |
|
|
|
|
| N0 | 52 | – | – | – |
|
≥N1 | 58 | 1.29 | 1.12–1.64 | <0.10 |
| Histological
grade |
|
|
|
|
| G1 | 27 | – | – | – |
|
≥G2 | 83 | 1.21 | 1.12–1.53 | <0.10 |
Discussion
Chronic inflammation is involved in the progression
of malignant diseases and has been reported to be associated with
the immune suppression that is observed in patients with advanced
diseases. MDSCs, which inhibit innate and adaptive immunity, have
been reported to be novel immune suppressor cells that are enhanced
by inflammation and that are present in the blood circulation,
lymph nodes, and tumor tissues in patients with cancer (8,9). MDSC
levels were previously measured in the PBMCs of 222 patients with
esophageal, gastric, colorectal, hepatocellular, cholangiocellular,
pancreatic, breast, ovarian, thyroid and lung cancer using flow
cytometry (20). An additional study
by another investigator provided support for the hypothesis that
MDSC levels are correlated with clinical stage and metastatic
disease burden in patients with breast cancer (21). Diaz-Montero et al (17) reported that the percentage of MDSCs in
the total blood, as measured using flow cytometry, was increased in
patients with later stage breast cancer. In that report, the
average peripheral blood MSDC levels were increased with the
advance of breast cancer and were highest in stage IV patients with
≥3 organ systems involved in the cancer. These authors also
observed that the peripheral blood MDSC levels corresponded to
levels of circulating tumor cells, which are another emerging
prognostic marker (17). The present
study reported that the levels of MDSCs in the circulating
peripheral blood were increased in patients with breast cancer
compared with healthy controls. MDSC levels were significantly
higher in preoperative patients than in healthy volunteers, and
were decreased in postoperative patients compared with preoperative
patients. In addition, MDSC levels were elevated in patients with
recurrent disease to levels that were equivalent to those observed
in preoperative patients. In patients with recurrent breast cancer,
MDSC levels were significantly decreased following chemotherapy.
The MDSC levels in preoperative patients were significantly
positively correlated with IL-6 production and, conversely, were
significantly negatively correlated with the production of IFN-γ
and IL-12. Th1 cells have been reported to be induced by IL-12 and
to produce IFN-γ, and these cells are concerned with cellular
immunocompetence (22). In addition,
IL-12 is known to be a modulator of immune suppression, with
significant potential as a therapeutic agent for metastatic breast
cancer (23). The present study
revealed that MDSC levels were inversely correlated with IL-12
production, which may suggest that MDSCs inhibited IL-12 production
by dendritic cells. Furthermore, the increased production of IL-6
suggested that increased MDSC levels resulted in a Th2-dominant
status. MDSC-produced IL-10 and other suppressive factors
inactivate healthy dendritic cells. Increased levels of MDSCs in
advanced breast cancer may therefore be involved in immune
suppression in these patients through multiple immunological
pathways. MDSC levels in preoperative patients were negatively
correlated with a short turnover protein and with the SI, and were
positively correlated with the NLR and CRP levels. These data
suggested that MDSC levels in these patients in the present study
were correlated not only with immune suppression, but also with
malnutrition and inflammation (24).
When MDSC levels were >1.0%, the prognosis of patients with
stage IV breast cancer was shorter than that of other patients.
However, there was no significant difference between different
stages in the prognosis of patients with MDSC levels <1.0%.
Thus, MDSC counts may be an important prognostic factor for
patients with breast cancer. The results of multivariable analysis
revealed that the risk of a poor prognosis is likely to be more
dependent on MDSCs levels >1%, which were associated with a
higher probability of mortality when adjusted for other potential
prognostic factors. Certain anti-cancer chemotherapeutic agents,
including gemcitabine, have been reported to alter MDSC levels,
resulting in improvement of cellular immunocompetence (17,25). MDSC
levels in the peripheral blood and in the pleural effusion of
patients with metastatic breast cancer have been previously
demonstrated to decrease following chemotherapy with gemcitabine
(26). The results of the present
study were consistent with those of previous studies. Future
studies are expected to investigate novel therapeutic approaches
for controlling immune suppression, malnutrition and chronic
inflammation, through modulation of MDSCs by selective inhibition
using molecular targeting or chemotherapy. Integrative breast
cancer immunotherapies that strategically combine established
therapies with breast cancer vaccines, immune checkpoint blockade
or a combination of the two should result in durable clinical
responses and an increased curative rate (27–29). These
approaches are expected to contribute to the effective augmentation
of cancer immunotherapy.
References
|
1
|
Global Burden of Disease Cancer
Collaboration, ; Fitzmaurice C, Dicker D, Pain A, Hamavid H,
Moradi-Lakeh M, MacIntyre MF, Allen C, Hansen G, Woodbrook R, et
al: The global burden of cancer 2013. JAMA Oncol. 1:505–527. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Reeder JG and Vogel VG: Breast cancer risk
management. Clin Breast Cancer. 7:833–840. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tan PH and Lota AS: Interaction of current
cancer treatments and the immune system: Implications for breast
cancer therapeutics. Expert Opin Pharmacother. 9:2639–2660. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Anderson KS: Tumor vaccines for breast
cancer. Cancer Invest. 27:361–368. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carson WE III and Liang MI: Current
immunotherapeutic strategies in breast cancer. Surg Oncol Clin N
Am. 16:841–860, ix. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rosenberg SA, Yang JC and Restifo NP:
Cancer immunotherapy: Moving beyond current vaccines. Nat Med.
10:909–915. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Curigliano G, Spitaleri G, Dettori M,
Locatelli M, Scarano E and Goldhirsch A: Vaccine immunotherapy in
breast cancer treatment: Promising, but still early. Expert Rev
Anticancer Ther. 7:1225–1241. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gabrilovich DI and Nagaraj S:
Myeloid-derived suppressor cells as regulators of the immune
system. Nat Rev Immunol. 9:162–174. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ostrand-Rosenberg S and Sinha P:
Myeloid-derived suppressor cells: Linking inflammation and cancer.
J Immunol. 182:4499–4506. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zea AH, Rodriguez PC, Atkins MB, Hernandez
C, Signoretti S, Zabaleta J, McDermott D, Quiceno D, Youmans A,
O'Neill A, et al: Arginase-producing myeloid suppressor cells in
renal cell carcinoma patients: A mechanism of tumor evasion. Cancer
Res. 65:3044–3048. 2005.PubMed/NCBI
|
|
11
|
Ochoa AC, Zea AH, Hernandez C and
Rodriguez PC: Arginase, prostaglandins, and myeloid-derived
suppressor cells in renal cell carcinoma. Clin Cancer Res.
13:721s–726s. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kusmartsev S, Nefedova Y, Yoder D and
Gabrilovich DI: Antigen-specific inhibition of CD8+ T cell response
by immature myeloid cells in cancer is mediated by reactive oxygen
species. J Immunol. 172:989–999. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Solito S, Falisi E, Diaz-Montero CM, Doni
A, Pinton L, Rosato A, Francescato S, Basso G, Zanovello P,
Onicescu G, et al: A human promyelocytic-like population is
responsible for the immune suppression mediated by myeloid-derived
suppressor cells. Blood. 118:2254–2265. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Almand B, Clark JI, Nikitina E, van Beynen
J, English NR, Knight SC, Carbone DP and Gabrilovich DI: Increased
production of immature myeloid cells in cancer patients: A
mechanism of immunosuppression in cancer. J Immunol. 166:678–689.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mosmann TR, Cherwinski H, Bond MW, Giedlin
MA and Coffman RL: Two types of murine helper T cell clone. I.
Definition according to profiles of lymphokine activities and
secreted proteins. J Immunol. 136:2348–2357. 1986.PubMed/NCBI
|
|
16
|
Shibata M, Nezu T, Kanou H, Abe H,
Takekawa M and Fukuzawa M: Decreased production of interleukin-12
and type 2 immune responses are marked in cachectic patients with
colorectal and gastric cancer. J Clin Gastroenterol. 34:416–420.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Diaz-Montero CM, Salem ML, Nishimura MI,
Garrett-Mayer E, Cole DJ and Montero AJ: Increased circulating
myeloid-derived suppressor cells correlate with clinical cancer
stage, metastatic tumor burden, and doxorubicin-cyclophosphamide
chemotherapy. Cancer Immunol Immunother. 58:49–59. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bevers TB, Anderson BO, Bonaccio E, Buys
S, Daly MB, Dempsey PJ, Farrar WB, Fleming I, Garber JE, Harris RE,
et al: NCCN clinical practice guidelines in oncology: Breast cancer
screening and diagnosis. J Natl Compr Canc Netw. 7:1060–1096. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Le HK, Graham L, Cha E, Morales JK,
Manjili MH and Bear HD: Gemcitabine directly inhibits myeloid
derived suppressor cells in BALB/c mice bearing 4T1 mammary
carcinoma and augments expansion of T cells from tumor-bearing
mice. Int Immunopharmacol. 9:900–909. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gonda K, Shibata M, Nakamura I, Kenjo A,
Ohtake T, Yasuda M, Suzuki S, Suzuki H, Watanabe T, Fujimori K, et
al: Myeloid-derived suppressor cells in cancer patients. Gan To
Kagaku Ryoho. 39:1797–1799. 2012.(In Japanese). PubMed/NCBI
|
|
21
|
Markowitz J, Wesolowski R, Papenfuss T,
Brooks TR and Carson WE III: Myeloid-derived suppressor cells in
breast cancer. Breast Cancer Res Treat. 140:13–21. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thakur A, Schalk D, Sarkar SH, Al-Khadimi
Z, Sarkar FH and Lum LG: A Th1 cytokine-enriched microenvironment
enhances tumor killing by activated T cells armed with bispecific
antibodies and inhibits the development of myeloid-derived
suppressor cells. Cancer Immunol Immunother. 61:497–509. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Steding CE, Wu ST, Zhang Y, Jeng MH, Elzey
BD and Kao C: The role of interleukin-12 on modulating
myeloid-derived suppressor cells, increasing overall survival and
reducing metastasis. Immunology. 133:221–238. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sinha P, Clements VK, Fulton AM and
Ostrand-Rosenberg S: Prostaglandin E2 promotes tumor progression by
inducing myeloid-derived suppressor cells. Cancer Res.
67:4507–4513. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Panis C, Lemos LG, Victorino VJ, Herrera
AC, Campos FC, Simão AN Colado, Pinge-Filho P, Cecchini AL and
Cecchini R: Immunological effects of taxol and adryamicin in breast
cancer patients. Cancer Immunol Immunother. 61:481–488. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gonda K, Shibata M, Ohtake T, Yasuda M,
Abe N, Watanabe K, Ando J, Okano M, Onozawa H, Tachibana K, et al:
Myeloid-derived suppressor cells in patients with breast cancer.
Gan To Kagaku Ryoho. 39:1363–1368. 2012.(In Japanese). PubMed/NCBI
|
|
27
|
Diaz-Montero CM, Finke J and Montero AJ:
Myeloid-derived suppressor cells in cancer: Therapeutic,
predictive, and prognostic implications. Semin Oncol. 41:174–184.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Emens LA: Breast cancer immunobiology
driving immunotherapy: Vaccines and immune checkpoint blockade.
Expert Rev Anticancer Ther. 12:1597–1611. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
de Coaña Y Pico, Masucci G, Hansson J and
Kiessling R: Myeloid-derived suppressor cells and their role in
CTLA-4 blockade therapy. Cancer Immunol Immunother. 63:977–983.
2014. View Article : Google Scholar : PubMed/NCBI
|