|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yeung TL, Leung CS, Li F, Wong SS and Mok
SC: Targeting stromal-cancer cell crosstalk networks in ovarian
cancer treatment. Biomolecules. 6:32016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Prasad KV, Ao Z, Yoon Y, Wu MX, Rizk M,
Jacquot S and Schlossman SF: CD27, a member of the tumor necrosis
factor receptor family, induces apoptosis and binds to Siva, a
proapoptotic protein. Proc Natl Acad Sci USA. 94:pp. 6346–6351.
1997; View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Py B, Slomianny C, Auberger P, Petit PX
and Benichou S: Siva-1 and an alternative splice form lacking the
death domain, Siva-2, similarly induce apoptosis in T lymphocytes
via a caspase-dependent mitochondrial pathway. J Immunol.
172:4008–4017. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Iorio-Morin C, Germain P, Roy S, Genier S,
Labrecque P and Parent JL: Thromboxane A2 modulates
cisplatin-induced apoptosis through a Siva1-dependent mechanism.
Cell Death Differ. 19:1347–1357. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gudi R, Barkinge J, Hawkins S, Chu F,
Manicassamy S, Sun Z, Duke-Cohan JS and Prasad KV: Siva-1
negatively regulates NF-kappaB activity: Effect on T-cell
receptor-mediated activation-induced cell death (AICD). Oncogene.
25:3458–3462. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shiozaki T, Iwai A, Kawaoka Y, Takada A,
Kida H and Miyazaki T: Requirement for Siva-1 for replication of
influenza A virus through apoptosis induction. J Gen Virol.
92:315–325. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Py B, Bouchet J, Jacquot G, Sol-Foulon N,
Basmaciogullari S, Schwartz O, Biard-Piechaczyk M and Benichou S:
The Siva protein is a novel intracellular ligand of the CD4
receptor that promotes HIV-1 envelope-induced apoptosis in
T-lymphoid cells. Apoptosis. 12:1879–1892. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Van Nostrand JL, Brisac A, Mello SS,
Jacobs SB, Luong R and Attardi LD: The p53 target gene siva enables
non-small cell lung cancer development. Cancer Discov. 5:622–635.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang X, Zha M, Zhao X, Jiang P, Du W, Tam
AY, Mei Y and Wu M: Siva1 inhibits p53 function by acting as an ARF
E3 ubiquitin ligase. Nat Commun. 4:15512013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Du W, Jiang P, Li N, Mei Y, Wang X, Wen L,
Yang X and Wu M: Suppression of p53 activity by Siva1. Cell Death
Differ. 16:1493–1504. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
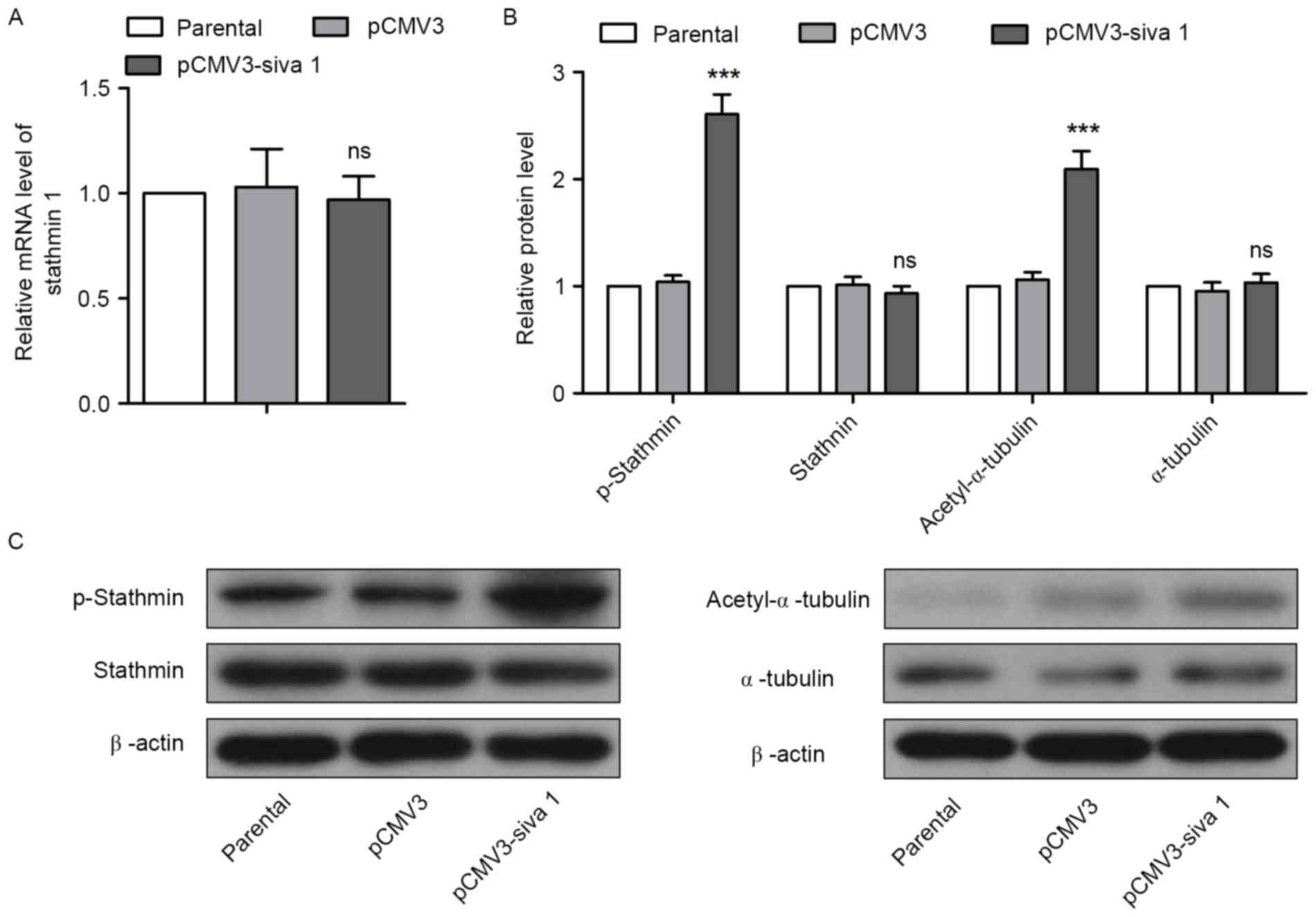
Li N, Jiang P, Du W, Wu Z, Li C, Qiao M,
Yang X and Wu M: Siva1 suppresses epithelial-mesenchymal transition
and metastasis of tumor cells by inhibiting stathmin and
stabilizing microtubules. Proc Natl Acad Sci USA. 108:pp.
12851–12856. 2011; View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wei SH, Lin F, Wang X, Gao P and Zhang HZ:
Prognostic significance of stathmin expression in correlation with
metastasis and clinicopathological characteristics in human ovarian
carcinoma. Acta Histochem. 110:59–65. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ray RM, Bhattacharya S and Johnson LR:
Mdm2 inhibition induces apoptosis in p53 deficient human colon
cancer cells by activating p73- and E2F1-mediated expression of
PUMA and Siva-1. Apoptosis. 16:35–44. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Machado-Neto JA, Lazarini M, Favaro P, de
Melo Campos P, Scopim-Ribeiro R, Junior GC Franchi, Nowill AE, Lima
PR, Costa FF, Benichou S, et al: ANKHD1 silencing inhibits Stathmin
1 activity, cell proliferation and migration of leukemia cells.
Biochim Biophys Acta. 1853:583–593. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gupta KK, Li C, Duan A, Alberico EO, Kim
OV, Alber MS and Goodson HV: Mechanism for the
catastrophe-promoting activity of the microtubule destabilizer
Op18/stathmin. Proc Natl Acad Sci USA. 110:pp. 20449–20454. 2013;
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Alli E, Yang JM and Hait WN: Silencing of
stathmin induces tumor-suppressor function in breast cancer cell
lines harboring mutant p53. Oncogene. 26:1003–1012. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Price DK, Ball JR, Bahrani-Mostafavi Z,
Vachris JC, Kaufman JS, Naumann RW, Higgins RV and Hall JB: The
phosphoprotein Op18/stathmin is differentially expressed in ovarian
cancer. Cancer Invest. 18:722–730. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Roos G, Brattsand G, Landberg G, Marklund
U and Gullberg M: Expression of oncoprotein 18 in human leukemias
and lymphomas. Leukemia. 7:1538–1546. 1993.PubMed/NCBI
|
|
21
|
Mistry SJ, Bank A and Atweh GF: Targeting
stathmin in prostate cancer. Mol Cancer Ther. 4:1821–1829. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kouzu Y, Uzawa K, Koike H, Saito K,
Nakashima D, Higo M, Endo Y, Kasamatsu A, Shiiba M, Bukawa H, et
al: Overexpression of stathmin in oral squamous-cell carcinoma:
Correlation with tumour progression and poor prognosis. Br J
Cancer. 94:717–723. 2006.PubMed/NCBI
|
|
23
|
Xi W, Rui W, Fang L, Ke D, Ping G and
Hui-Zhong Z: Expression of stathmin/op18 as a significant
prognostic factor for cervical carcinoma patients. J Cancer Res
Clin Oncol. 135:837–846. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kuo MF, Wang HS, Kuo QT, Shun CT, Hsu HC,
Yang SH and Yuan RH: High expression of stathmin protein predicts a
fulminant course in medulloblastoma. J Neurosurg Pediatr. 4:74–80.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Schulze E, Asai DJ, Bulinski JC and
Kirschner M: Posttranslational modification and microtubule
stability. J Cell Biol. 105:2167–2177. 1987. View Article : Google Scholar : PubMed/NCBI
|