Introduction
Among tumors of the major salivary glands, tumors of
the sublingual gland are rare, accounting for <0.5% of cases
(1). Although mucoepidermoid
carcinoma (MEC) is one of the most common malignant salivary gland
neoplasms, and ~50% of MECs occur in the major salivary glands,
including the parotid or submandibular gland (2,3), MEC of
the sublingual gland is a relatively rare disease.
MEC is a malignant epithelial neoplasm that was
first described by Stewart et al in 1945 (4). MEC is the most common malignant salivary
gland tumor among cases reviewed at the Armed Forces Institute of
Pathology since 1970 and other treatment centers in the United
States (2). In addition, the
frequencies are comparable to those studies from other countries
(2).
MEC is histologically characterized by the presence
of mucinous, intermediate and squamoid cells, while clear, columnar
and oncocytic cells are less commonly observed (3,5).
Typically, the pathological diagnosis of MEC is relatively easy;
however, definitive diagnosis may be challenging when the tumor is
composed of less common cell types (5). MEC is sub-classified into low,
intermediate and high grades on the basis of its histological
features (2,3,5,6).
No chemical carcinogens or oncogenic viruses are
associated with MEC (6). However,
prior exposure to radiation is a contributing factor for MEC
(7).
Prognosis depends on clinical stage, site, grading
and adequacy of surgical excision (5). Low grade tumors exhibit excellent
prognoses, however; high grade tumors demonstrate metastasis to the
regional lymph nodes and distant sites including lungs, bone, and
brain (5).
Mastermind-like transcriptional coactivator 2
(MAML2) gene translocation is observed in more than half of
all cases of MEC, and is a useful diagnostic marker (8,9). The
present study reports a case of MEC occurring in the sublingual
gland of a 76-year-old female. A review of the relevant literature
is also presented.
Case report
A 76-year old Japanese woman suffering from
Parkinson's disease presented at Kurume University Hospital
(Kurume, Japan) in April 2016 due to a mass in her left
submandibular region. Upon examination, a soft mass was palpable.
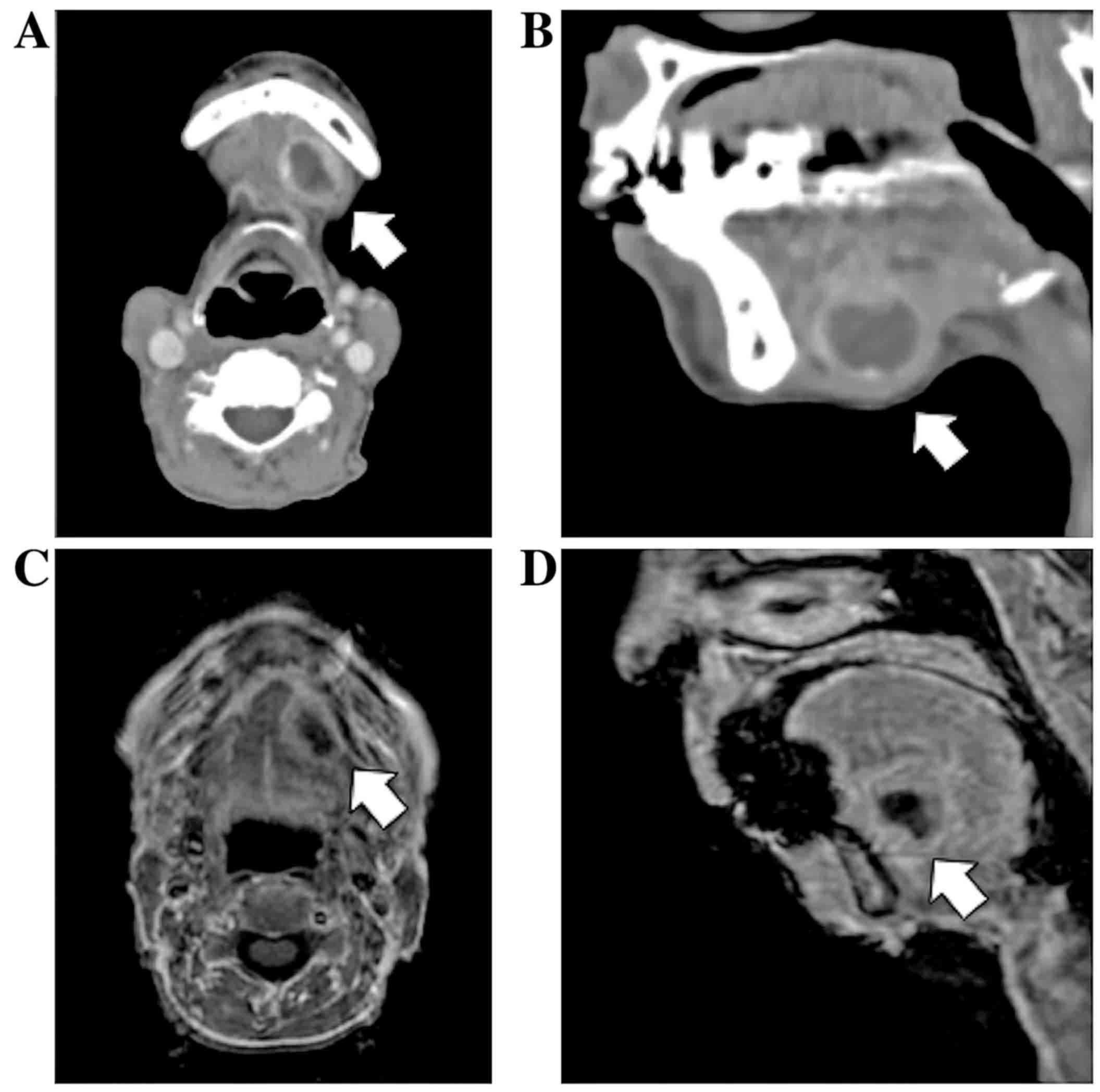
Contrast-enhanced computed tomography (CT) scans (Fig. 1A and B) and a magnetic resonance
imaging (MRI) examination (Fig. 1C and
D) revealed a cystic mass originating from the sublingual gland
in the floor of the oral cavity. Fine-needle aspiration cytology
was performed, which revealed only inflammatory cells, including
histiocytes, lymphocytes and neutrophils, with no epithelial
component. The tumor was removed percutaneously.
The sublingual gland tumor was encapsulated and did
not adhere to the surrounding tissue. Macroscopically, the tumor
was 20 mm in diameter and contained black fluid (Fig. 2). Tissue preparation and staining were
performed as follows: Paraffin-embedded tissue samples were cut at
4 µm and examined on a coated glass slides, and then labeled with
antibodies using the BenchMark ULTRA (Ventana Automated Systems,
Inc., Tucson, AZ, USA) and Bond-III autostainer (Leica
Microsystems, Ltd., Milton Keynes, UK).
Primary antibodies were as follows: Endomysial
antibody (EMA; cat no. 1504; ready to use; clone E29/EP1), S100
protein (cat no. N1573; ready to use) (both from DakoCytomation;
Agilent Technologies, Inc., Santa Clara, CA, USA), mitochondria
(cat no. 6280-0004; 1:500; clone AE1; Biogenesis; Morphosys AG,
Poole, UK), p63 (cat no. M7247; 1:100, clone 4A4; DakoCytomation;
Agilent Technologies, Inc.), and p40 (cat no. PC373; 1:500, clone
5–17; Calbiochem; Merck KGaA, Darmstadt, Germany).
For p63 and p40, BenchMark ULTRA was used. Briefly,
each slide was heat-treated at 99°C using Ventana CC1 retrieval
solution (Ventana Automated Systems, Inc.) for 30 min, and
incubated at room temperature with each antibody for 30 min. This
automated system used the streptavidin-biotin complex method with
3,3′ diaminobenzidine (DAB) as the chromogen (Ventana UltraVIEW DAB
detection kit; Ventana Automated Systems, Inc.). Immunostaining
with EMA, S100 protein and mitochondria were performed on the same
fully automated Bond-III system using on-board heat-induced antigen
retrieval with epitope retrieval solution 2 (pH 9.0) for 5 min and
a Refine polymer detection system (Leica Microsystems, Ltd.). DAB
was used as the chromogen in all these immunostainings.
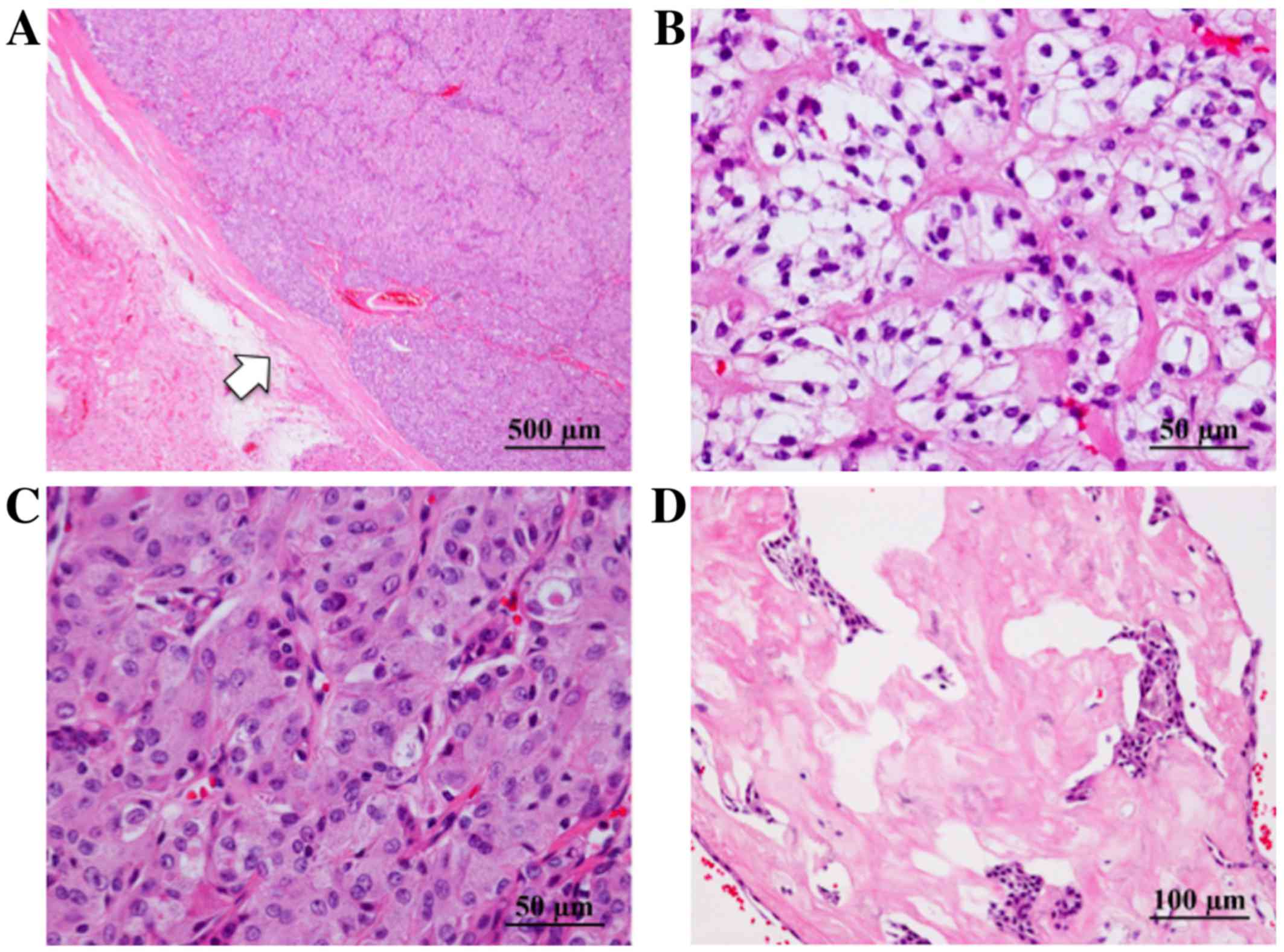
Histological evaluation revealed that the tumor was
encapsulated by fibrous tissue (Fig.
3A) and composed of cells with clear (Fig. 3B) or granular eosinophilic cytoplasm
(Fig. 3C), proliferating in solid
patterns. Individual cells had subtle nuclear atypia. Hyalinized
stroma was observed (Fig. 3D). A
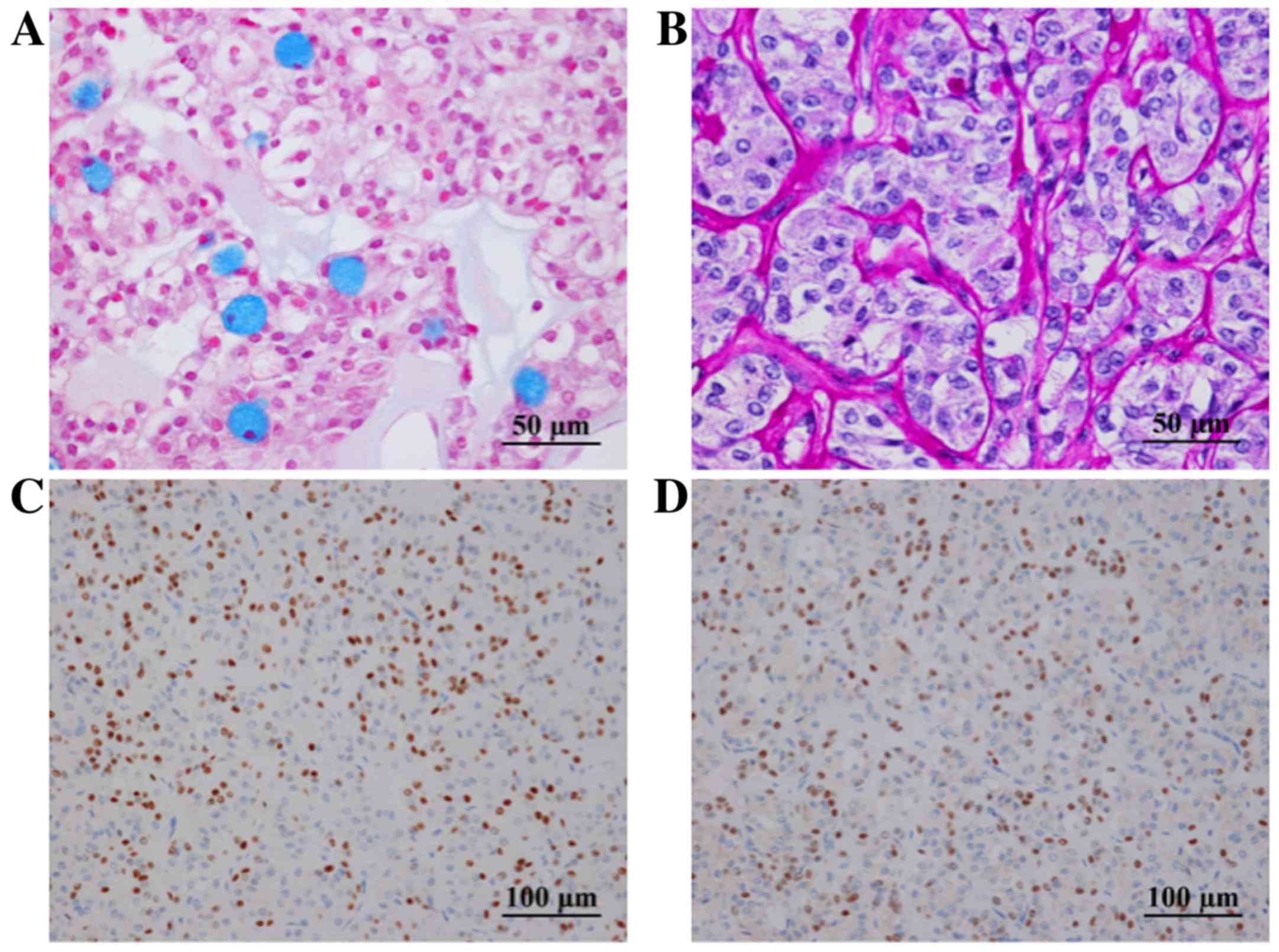
small number of mucinous cells were observed in the tumor following
alcian blue (Fig. 4A) and periodic
acid-Schiff (PAS) staining. Diastase-resistant PAS-positive
granules were observed in the cytoplasm of the tumor cells
(Fig. 4B), and were interpreted as
fine hyaline globules. Immunoreactivity for p63 (Fig. 4C) and p40 (Fig. 4D) was found in the tumor cells.
However, S-100 protein and epithelial membrane antigen (EMA) were
not detected. A positive reaction for mitochondria was observed to
be scattered in individual cells, indicating that the tumor was
unlikely to be oncocytoma or oncocytic carcinoma in differential
diagnosis.
Since there was no indication of perineural
invasion, necrosis, mitoses or anaplasticity, the tumor was
considered a low-grade malignancy according the grading scale
proposed by Goode et al (10).
Although microinvasion into the surrounding fibrous capsule was
observed, no vascular invasion was confirmed by Elastica van Gieson
and D2-40 staining.
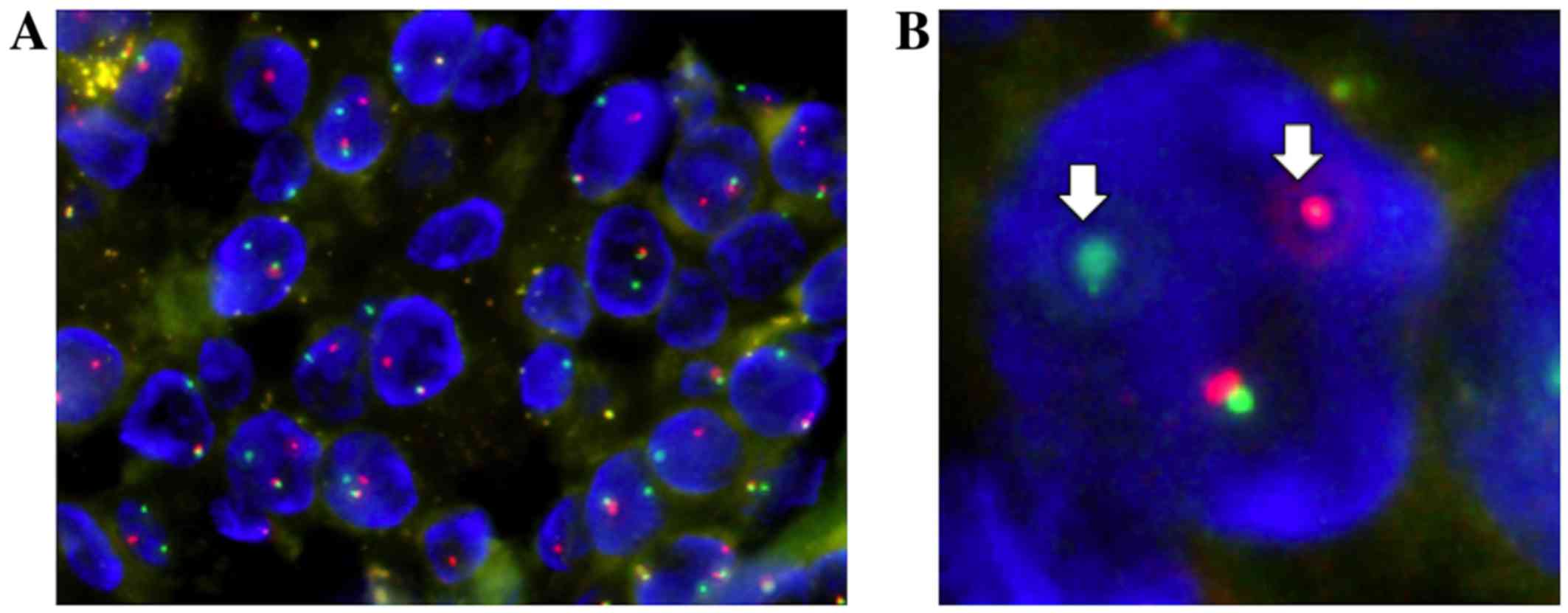
Fluorescence in situ hybridization (FISH)
analysis for a MAML2 (11q21) gene translocation was
performed using a ZytoLight® SPEC MAML2 Dual Color Break
Apart Probe (ZytoVision GmbH, Bremerhaven, Germany). FISH analysis
detected a split signal in the MAML2 gene, with a rate of
83% of the counted nuclei in the tumor cells (Fig. 5). Based on these findings, a final
diagnosis of low-grade MEC was determined.
Following the complete surgical removal of the
tumor, fludeoxyglucose-positron emission tomography (PET) revealed
no other metastatic lesions. As histological evaluation
demonstrated clear margins, and the MEC was determined to be a
low-grade type, no additional treatment was performed. During the
6-month postoperative course, no evidence of local recurrence or
distant metastasis was observed, and the patient remains relatively
well thus far.
The present study was approved by the ethics
committee of Kurume University (approval no. 17003) and written
informed consent was obtained.
Discussion
Tumors of the sublingual gland are uncommon, and MEC
of the sublingual gland is even more rare. To date, only three such
cases have been reported in the English literature (11–13). In
one case, bone formation was observed within the tumor (12). To the best of our knowledge, there
have been no reports of MEC of the sublingual gland with confirmed
MAML2 gene translocation.
MEC is typically composed of mucinous, squamoid and
intermediate cells. Clear cells, oncocytic cells and columnar cells
are occasionally present and prominent (2,5). Since MEC
exhibits various histological structures composed of these cell
types, it is occasionally difficult to differentiate MEC from other
types of tumor, such as clear cell, oncocytic and squamous cell
carcinomas (2,5).
In the present case, the tumor was composed of cells
with granular eosinophilic or clear cytoplasm, and a mucinous cell
component was also observed in a limited area. Therefore, it was
difficult to determine a diagnosis of MEC based solely on
morphological observation. Immunohistochemical staining for p40 and
p63, as well as mucin staining, aided the diagnosis.
Immunohistochemically, the tumor cells were negative for S-100
protein, a representative myoepithelial marker. p40 and p63
(14), which are myoepithelial as
well as squamous cell markers (15),
were positively expressed in the tumor cells, indicating that the
tumor had features of squamous and/or squamoid differentiation. The
presence of mucinous cells meant that the tumor was less likely to
be an oncocytic or clear cell carcinoma. However, mucinous cells
are not only detected in MEC, but also in various other tumors with
mucinous metaplasia (2).
As the tumor in the present case was histologically
composed of cells with granular eosinophilic or clear cytoplasm,
the differential diagnoses included benign and malignant tumors
with oncocytic or clear cytoplasm, such as oncocytoma, acinic cell
carcinoma, mammary analogue secretory carcinoma of the salivary
gland, epithelial-myoepithelial carcinoma and clear cell carcinoma.
The small number of mucinous cells identified in the tumor
indicated the possibility of MEC rather than other salivary gland
tumors; however, as the tumor occurred at an unusual site, FISH
analysis was performed to confirm this diagnosis. FISH analysis for
a MAML2 gene translocation is a useful supplemental method
for cases where the diagnosis of MEC is uncertain.
MAML2 gene translocation is a specific gene
rearrangement present in MEC tumors, and FISH analysis of the
MAML2 gene is therefore useful for the screening of MEC
(8,9).
Noda et al (8) reported that
MAML2 gene translocation was detected in ~65% of primary
MECs, and that the cut-off value for the split signal in
MAML genes is >7%. In the present case, the rate of
MAML split signal detection was 83%, and the tumor was
therefore considered to have MAML2 gene translocation.
The majority of MECs with MAML2 gene
translocation are histologically classified as low-grade (8), as demonstrated by the present case.
MAML2 gene translocation is typically detected in MECs that
are predominantly composed of epidermoid, intermediate and mucinous
cells; however, there have been a few reports of clear cell or
oncocytic variants of MEC harboring a MAML2 gene split
(16,17).
The MAML2 gene translocation is an oncogenic
event that underlies the development of MEC (18). Therefore, MAML2 gene
translocation may be observed in various types of cells in MEC.
Tumor cells with a granular eosinophilic or clear cytoplasm may
indicate oncogenesis as the degree of MAML2 gene
translocation is high in the tumor.
Although FISH analysis for a MAML2 gene
translocation is not routinely performed to diagnose MEC, its use
in unusual cases may aid in determining an accurate diagnosis. The
MAML2 gene and other molecular biomarkers have been
identified to form the basis for the development of novel
therapeutic strategies (19). Noda
et al (8) reported that
MAML2 gene translocation is associated with a favorable
prognosis in cases of MEC. However, a more recent study reported
that MAML2 gene status has no association with the prognosis
of MEC (20). As the association
between MAML2 status and prognosis is controversial,
MAML2 status in MEC must be investigated in a larger cohort
of patients in order to determine its precise roles. MAML2
gene translocation may also aid the prediction of prognoses and
selection of optimal treatments.
The 5-year survival rates of low-grade and
high-grade MEC are 97 and 27%, respectively (21). Therefore, it is important to determine
the histological grade of this malignancy, as this influences the
clinical features and prognosis (22). MEC may be classified into three grades
according to its pathological features, including cystic
components, perineural invasion, necrosis, mitoses and
anaplasticity (2,3,5,10). As the tumor in the present case lacked
any of these features, it was categorized as a low-grade
malignancy.
Surgical resection of the primary tumor is the
standard treatment for all grades of MEC. The majority of cases of
high-grade MEC tend to metastasize, and selective neck dissection
during initial surgery is therefore recommended (22). In addition, adjuvant radiotherapy is
recommended in cases of high-grade MEC (22). By contrast, low-grade MEC is less
aggressive; thus, surgical resection alone is usually sufficient,
as in the present case. However, there is a potential risk of local
metastasis in low-grade MEC, and this occurs in ~4% of cases
(10). Therefore, careful clinical
follow-up is recommended.
Previous reports have described the utility of
PET/CT for MECs of the lung or bronchi (23,24), and
one report described the assessment of low-grade MEC with
high-resolution PET/CT (24). It is
unclear whether FDG accumulates in low-grade MEC. However, we
suggest that PET/CT combined with CT and MRI could be used as a
supplemental examination, as the prognosis and the frequency of
metastasis in MECs of the sublingual gland are unclear. The precise
roles of PET/CT for salivary gland MECs must be investigated in a
larger patient cohort.
In summary, the combined use of
immunohistochemistry, FISH analysis of MAML2 gene
translocation and histological observation is a useful and reliable
examination technique for the accurate diagnosis of atypical MEC.
To the best of our knowledge, this is the first report of MEC of
the sublingual gland with MAML2 gene translocation confirmed
by FISH.
References
|
1
|
Eveson JW and Cawson RA: Salivary gland
tumours. A review of 2410 cases with particular reference to
histological types, site, age and sex distribution. J Pathol.
146:51–58. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gary LE and Paul LA: Tumor of the salivary
glandsAFIP Atlas of Tumor Pathology Series 4. AFIP ARP; Washington:
pp. 173–196. 2008
|
|
3
|
Goode RK and El-Naggar AK: Mucoepidermoid
carcinoma. In: World Health Organization Classification of
TumorsPathology and Genetics of Head and Neck Tumors. Barnes L,
Evenson JW, Reichart P and Sidransky D: IARC Press; Lyon: pp.
219–220. 2005
|
|
4
|
Stewart FW, Foote FW and Becker WF:
Muco-epidermoid tumors of salivary glands. Am J Surg. 122:820–844.
1945.
|
|
5
|
John WE and Lester DRT: Malignant
neoplasms of the salivary glandsHead and Neck Pathology. Lester
DRT: 2nd. Elsevier Sauners; Philadelphia: pp. 270–277. 2013
|
|
6
|
Luna MA: Salivary mucoepidermoid
carcinoma: Revisited. Adv Anat Pathol. 13:293–307. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Whatley WS, Thompson JW and Rao B:
Salivary gland tumors in survivors of childhood cancer. Otolaryngol
Head Neck Surg. 134:385–388. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Noda H, Okamura Y, Nakayama T, Miyabe S,
Fujiyoshi Y, Hattori H, Shimozato K and Inagaki H:
Clinicopathological significance of MAML2 gene split in
mucoepidermoid carcinoma. Cancer Sci. 104:85–92. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fehr A, Röser K, Heidorn K, Hallas C,
Löning T and Bullerdiek J: A new type of MAMAL2 fusion in
mucoepidermoid carcinoma. Genes Chromosomes Cancer. 47:203–206.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Goode RK, Alclair PL and Ellis GL:
Mucoepidermoid carcinoma of the major salivary glands. Clinical and
histopathologic analysis of 234 cases with evaluation of grading
criteria. Cancer. 82:1217–1224. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kumar AN, Nair PP, Thomas S, Raman PS and
Bhambal A: Mucoepidemoid carcinoma of sublingual gland: A malignant
neoplasm in an uncommon region. BMJ Case Rep May.
2011:bcr02201138642011.
|
|
12
|
Murase Y, Kawano S, Kiyoshima T, Goto Y,
Matsubara R, Chikui T, Yoshiga D and Nakamura S: Case of
mucoepidermoid carcinoma of the sublingual gland accompanied with
extensive dystrophic calcification and intratumoral bone formation.
Head Neck. 37:E161–E164. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sumanth KN, Mainali A, Ongole R and Pai
MR: Mucoepidermoid carcinoma: ‘A Mimicker’? J Nepal Dent Assoc.
10:31–34. 2009.
|
|
14
|
Furuse C, Sousa SO, Nunes FD, Magalhães MH
and Araújo VC: Myoepithelial cell markers in salivary gland
neoplasms. Int J Surg Pathol. 13:57–65. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Owosho AA, Aguilar CE and Seethala RR:
Comparison of p63 and p40 (ΔNp63) as basal, squamoid, and
myoepithelial markers in salivary gland tumors. Appl
Immunohistochem Mol Morphol. 24:501–508. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tajima S, Namiki I and Koda K: A clear
cell variant of mucoepidermoid carcinoma harboring CRTC1-MAML2
fusion gene found in buccal mucosa: Report of a case showing a
large clear cell component and lacking typical epidermoid cells and
intermediate cells. Med Mol Morphol. 50:117–121. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fujimaki M, Fukumura Y, Saito T, Mitani K,
Uchida S, Yokoyama J, Yao T and Ikeda K: Oncocytic mucoepidermoid
carcinoma of the parotid gland with CRTC1-MAML2 fusion transcript:
Report of a case with review of literature. Hum Pathol.
42:2052–2055. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wu L, Liu J, Gao P, Nakamura M, Cao Y,
Shen H and Griffin JD: Transforming activity of MECT1-MAML2 fusion
oncoprotein is mediated by constitutive CREB activation. EMBO J.
24:2391–2402. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Stenman G, Persson F and Andersson MK:
Diagnostic and therapeutic implications of new molecular biomarkers
in salivary gland cancers. Oral Oncol. 50:683–690. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Seethala RR and Chiosea SI: MAML2 status
in mucoepidermoid carcinoma can no longer be considered a
prognostic marker. Am J Surg Pathol. 40:1151–1153. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Spiro RH, Huvos AG, Berk R and Strong EW:
Mucoepidermoid carcinoma of salivary gland origin. A
clinicopathologic study of 367 cases. Am J Surg. 136:461–468. 1978.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nance MA, Seethala RR, Wang Y, Chiosea SI,
Myers EN, Johnson JT and Lai SY: Treatment and survival outcomes
based on histologic grading in patients with head and neck
mucoepidermoid carcinoma. Cancer. 113:2082–2089. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Elnayal A, Moran CA, Fox PS, Mawlawi O,
Swisher SG and Marom EM: Primary salivary gland-type lung cancer:
Imaging and clinical predictors of outcome. AJR Am J Roentgenol.
201:W57–W63. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ishizumi T, Tateishi U, Watanabe S, Maeda
T and Arai Y: F-18 FDG PET/CT imaging of low-grade mucoepidermoid
carcinoma of the bronchus. Ann Nucl Med. 21:299–302. 2007.
View Article : Google Scholar : PubMed/NCBI
|