Introduction
Intraspinal tumors are common neurogenic tumors,
accounting for approximately 15% of central nervous system tumors
(1). Intraspinal tumors refer
collectively to the primary tumors and metastatic tumors that grow
in the spinal canal or spinal cord or adjacent tissue structures to
spine (such as the spinal dura mater, nerve roots, blood vessels
and intraspinal adipose tissue). Intrathecal tumors include the
primary tumors and secondary tumors. The primary intraspinal tumors
refer to all tumors originated in intraspinal tissue, and secondary
intraspinal tumors refer to tumors originated in adjacent tissues
outside spinal canal and spread into spinal canal, and malignant
tumors originated in distal sites and spread into spinal canal via
metastasis, among which neurilemmoma is a kind of common benign
tumor in spinal canal (2,3), and due to the slow tumor growth, hidden
onset and no specific symptoms and signs, its early diagnosis is
more difficult, and some patients are not treated until they are
paralyzed. In particular, its initial manifestation in the early
stage is the radiating pain caused by affecting the nerve root, so
it is often misdiagnosed as coronary heart disease, cholecystitis
and appendicitis, and patients even receive the wrong operation,
seriously affecting the patient's operative prognosis (4). Thus, the early diagnosis and early
surgery are essential. Twenty-seven patients with intraspinal
neurilemmoma were admitted to the Second People's Hospital of
Changzhou affiliated to Nanjing Medical University from January
2010 to October 2015, achieving good clinical outcomes.
Patients and methods
Patients
There were 27 patients in the group, including 15
males and 12 females aged 30–81 years with an average age of 53.7
years; there were 4 cases of cervical segment, 6 cases of thoracic
segments and 17 cases of lumbar and sacral segments; there were 25
cases of intradural-extramedullary tumor and 2 cases of epidural
tumor. The course of disease was 4–36 months with an average
duration of 13.5 months. Seventeen cases suffered from limb
radiating pain accompanied with hypoesthesia or hyperalgesia in
different degrees in physical examination; 10 cases suffered from
weakness in walking accompanied with decreased muscle strength,
positive pathological signs, tendon hyperreflexia or active in
physical examination; 2 cases suffered from numbness in saddle
area, fecal and urinary dysfunction. This study was approved by the
Ethics Committee of the Second People's Hospital of Changzhou.
Signed written informed consents were obtained from all
participants before the study.
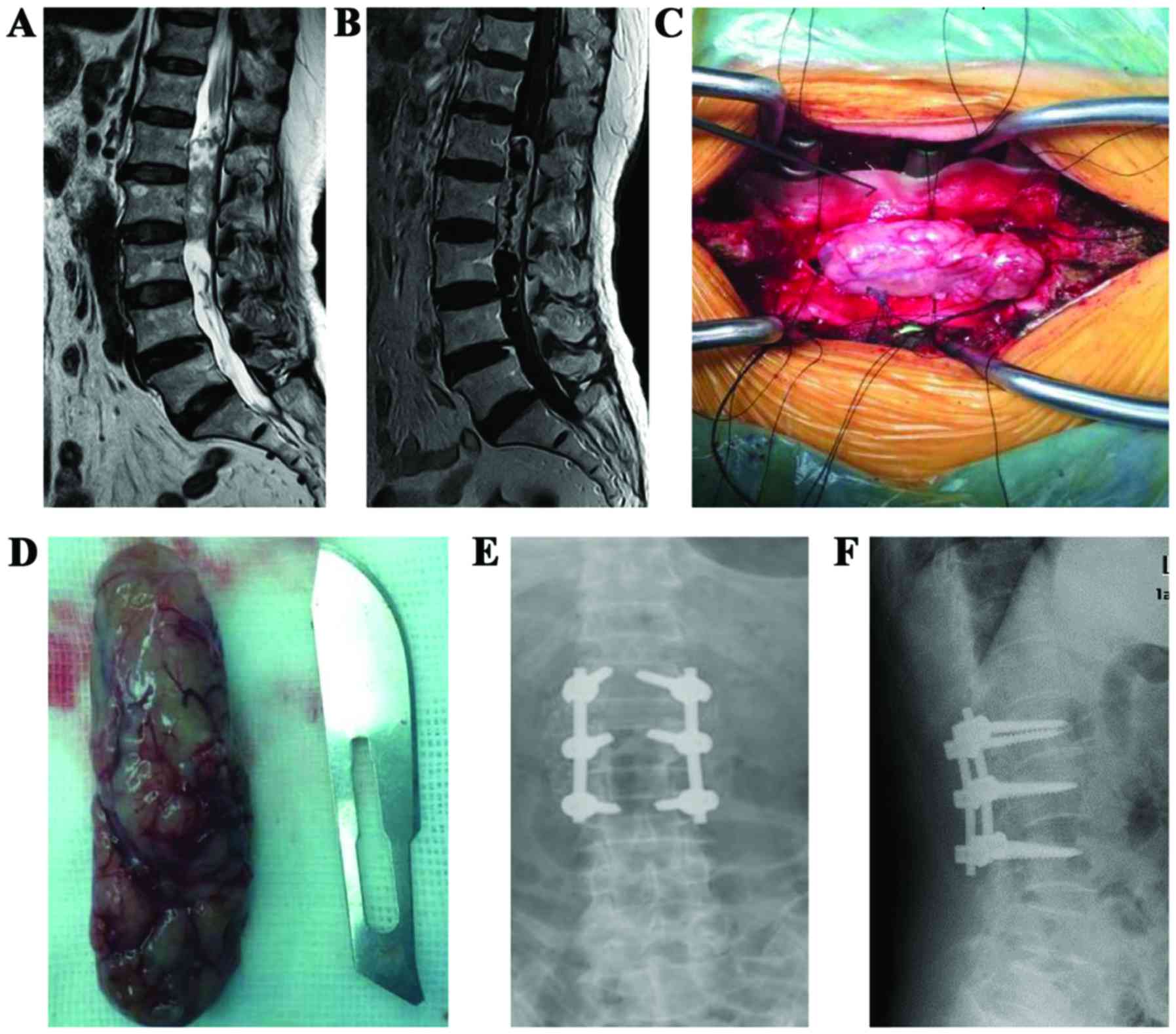
Radiological examination
All patients underwent X-ray, CT and MRI
examinations before operation. X-ray film showed that there were 8
cases of spinal canal enlargement and vertebral posterior
compression, and 5 cases of intervertebral foramen expansion and
vertebral pedicle narrowing. CT examination showed that the tumors
were mostly oval or circular solid lesions, and some were
dumbbell-shaped tumors. MRI examination showed 20 cases of
intradural extramedullary oval mass with clear border, 6 cases of
dumbbell-shaped tumors and 1 case of larger sacral tumor with
irregular shape growing to the anterior pelvic cavity. T1-weighted
image (T1WI) showed slightly lower signal, equal signal or
equally-low mixed signal, and T2-weighted image (T2WI) mostly
showed high signal or mixed signal. Sixteen patients underwent MRI
enhanced scan, among which 6 cases showed significant enhancement
and 10 cases showed irregular edge enhancement. Before operation,
19 patients were clinically diagnosed as neurilemmoma, and another
8 patients had difficulty in diagnosis and diagnosed pathologically
after operation (Table I).
 | Table I.Demographic data for the 27 enrolled
patients. |
Table I.
Demographic data for the 27 enrolled
patients.
| Items | Number of cases |
|---|
| Sex |
|
|
Male/Female | 15/12 |
| Segment |
|
| Cervical
segment | 4 |
| Thoracic
segment | 6 |
|
Lumbosacral segment | 17 |
| Location |
|
|
Subdural | 25 |
|
Epidural | 2 |
Surgical procedures
Under general anesthesia with tracheal intubation,
all patients received posterior midline approach in prone position,
except 1 case of large sacral tumor receiving combined anterior and
posterior approach. Thoracic tumors were positioned using clip
before operation. Longitudinal incision was made on skin and
subcutaneous tissue with the affected vertebra as the center, and
the paravertebral muscles were peeled off to the articular process.
Sixteen cases of tumors were significantly biased to one side, so
they received semi-laminectomy, and 6 cases of tumors could be
exposed using facetectomy on the affected side; 11 cases of tumor
involved a large area, so they received total laminectomy, and
zygapophyseal joints on both sides were retained as far as
possible. Dura mater was cut along the posterior midline to
completely expose tumor tissue, followed by blunt dissection using
nerve detacher. One to two nerve roots crossed 5 cases of tumors
with unclear boundary, so they were totally resected. Sixteen cases
of tumors were totally resected due to complete capsule and clear
boundary. Five cases of tumors were partially resected due to
difficult in total resection. One case of large sacral tumor
received combined anterior and posterior approach. Dural sac was
closely and continuously sutured using 6–0 non-invasive stitches,
and 6 cases of dural tear were sealed using adjacent fascia.
Seventeen patients were treated with spinal dynamic pedicle screw
fixation or replantation of lamina or bone graft fusion and
internal fixation, including 4 cases of cervical vertebra receiving
lateral mass fixation, 1 case of thoracic vertebra receiving
replantation of lamina, 6 cases of thoracolumbar vertebrae
receiving dynamic pedicle screw fixation and 6 cases of lumbosacral
vertebrae receiving pedicle screw fixation + posterior-lateral bone
graft fusion.
Post-operative treatment
After operation, patients received conventional
antibiotics to prevent infection, dehydration and swelling, and
anti-inflammatory treatment using hormone. Cervical gear or waist
gear was used for protection for 3 months. Patients were followed
up regularly after operation, and spinal stability and bone graft
fusion were observed via X-ray in the review; whether there was
tumor recurrence was observed via MRI in the review according to
individual conditions.
Results
The operation time was 2.5–8 h (4.2 h on average).
The intraoperative blood loss was 420–1,500 ml (760 ml on average).
Tumors in 26 patients were totally resected, and tumor in 1 patient
was partially resected due to tumor tissue invasion against the
anterior sacral vascular plexus. All patients were pathologically
confirmed as neurilemmoma after operation. Ten patients suffered
from cerebrospinal fluid leakage after operation, so the position
was adjusted, followed by pressure dressing and wound dressing; and
the drainage time was prolonged appropriately, and non-vacuum
drainage was adopted. There were 3 cases of refractory
cerebrospinal fluid leakage, and the wound was sutured in
debridement and healed. During the follow-up for 6–75 months after
operation, clinical symptoms and neurological functions of all
patients were significantly improved. The mean pain VAS score of 17
patients with limb radiating pain was reduced from 8 points on
admission to 4 points at discharge. The average muscle strength of
10 patients with limb weakness and walking instability recovered
from Level 3 before operation to level 5 in the review at 1 month
after operation. Symptoms of 2 patients with numbness in saddle
area and fecal and urinary dysfunction disappeared and the function
was recovered in the review at 5 months after operation. Partial
tumor tissue was left in 1 patient due to the invasion of larger
tumor against anterior sacral vascular plexus, and MRI showed that
the tumor tissue did not grow in the review at 6 months after
operation. There was no recurrence. The internal fixation in
patients receiving spinal internal fixation was in place and the
fusion in patients receiving fusion surgery was fine. No pedicle
prolapse, broken nail or broken rod was found. No spondylolisthesis
and instability were found during follow-up (Fig. 1).
Discussion
Most patients with neurilemmoma are characterized by
hidden onset and a longer course of disease. The main symptoms and
signs are pain, paresthesia, dyskinesia and sphincter dysfunction.
The initial symptom is mostly nerve root pain, followed by
paresthesia and motor dysfunction (5). The course of disease in this group was
4–36 months (13.5 months on average), but that of 6 cases with
thoracic tumor was shorter for 4–9 months (5.4 months on average);
it was easy to be misdiagnosed as cervical spondylosis due to the
radiating pain in chest and back and weakness in walking in lower
limb. Seventeen patients suffered from obvious limb radiating pain,
night pain and supine pain. Paresthesia in different degrees was
found in physical examination. Tumor tissues of 10 patients
associated with the symptoms of weakness in walking were located in
the cervical and thoracic segments, and physical examination showed
the decreased muscle strength, tendon reflex active or
hyperreflexia, and positive pathological signs; 2 patients with
lumbosacral tumor suffered from numbness in saddle area and fecal
and urinary dysfunction.
Early diagnosis is critical because the long-term
spinal cord compression may lead to permanent loss of function.
Detailed physical examination combined with MRI has a higher
diagnostic value (6). MRI often
showed intradural extramedullary circular, or dumbbell-shaped mass,
T1WI showed the slightly lower signal, equal signal or equally-low
mixed signal, and T2WI mostly showed high signal or mixed signal,
and cystic change and necrosis might occur (7). In this group, 20 cases had intradural
extramedullary oval mass with clear border, 6 cases had
dumbbell-shaped tumors and 1 case had larger sacral tumor with
irregular shape growing to the anterior pelvic cavity. Enhanced MRI
scan mostly showed the uniform enhancement or ring and lace-like
enhancement, and few showed the non-uniform enhancement; cystic
necrosis area and spinal dura mater had no significant enhancement
(8–10). In this group, 16 cases underwent MRI
enhanced scan, among which 6 cases showed the significant
enhancement and 10 cases showed the irregular edge enhancement. It
is not difficult to be diagnosed as intraspinal tumor, but its
nature is hard to be defined before operation, and intraspinal
neurilemmoma should be distinguished from meningioma, neurofibroma,
teratoma and metastatic tumor (4,6).
Pre-operative prediction of tumor nature is essential for
intraoperative operation and post-operative recovery. In this
group, the nature of 19 cases of tumors was correct before
operation, and another 8 cases were difficult to diagnose, but
confirmed pathologically after operation.
Intraspinal neurilemmoma should receive operation as
soon as possible once diagnosed (11). Intraspinal neurilemmoma is a mostly
benign tumor and surgical resection has a good effect with little
recurrence after total resection (12). Surgical approach should be determined
based on the tumor site and invasion range, and the
semi-laminectomy on the affected side or total laminectomy
retaining both sides of zygapophyseal joints or semi-laminectomy
combined with facetectomy on the affected side should be performed.
One case in this group received combined anterior and posterior
approach due to the invasion of large tumor against anterior pelvic
cavity. The intraoperative fluoroscopy is difficult for the
upper-middle thoracic tumor, due to the blocking of scapula, so we
think it is necessary to accurately position before surgery, and
the corresponding parts should be often fixed with one to two clips
for intraoperative positioning. The operation should be gentle to
avoid excessive pulling of spinal cord nerve. High-speed abrasive
drilling should be used for patients with cervical and thoracic
tumors, and if the tumor is located in the spinal cord ventrally or
ventral lateral region, the bone window should be made to fully
expose tumor tissue (9). If the tumor
is larger and the total resection is difficult, tumors can be
resected in batches. For dumbbell-shaped tumors, it is necessary to
fully remove the lamina and zygapophyseal joint on the affected
side to fully expose the tumor and realize one-time resection
(13,14).
According to the current viewpoint, the tumor tissue
should be totally resected as far as possible when tumor-bearing
nerves are treated. For thoracolumbar tumors, the pure
disconnection of nerve roots generally does not cause new
neurological deficits, but the cervical segment should be retained
as far as possible (15). Schultheiss
and Gullotta (16) found that
patients did not suffer from serious functional loss after the
tumor-bearing nerves were cut off. Celli (17) reported that a small number of patients
suffered from permanent motor dysfunction after nerve roots in
C5-C8 or L3-S1 were cut off. In this group with 5 cases of tumors,
there was 1 case in cervical segment, 3 cases in thoracic segment
and 1 case in lumbar segment; 1–2 nerve roots crossed with unclear
boundary, and the tumor was totally resected; no obvious
neurological dysfunction was found after operation.
In total laminectomy, the bony structures of
posterior ligament complex and posterior column are resected,
easily leading to iatrogenic spinal instability, so the internal
fixation and bone graft fusion are needed to reduce the risk of
post-operative spinal deformity (18,19).
According to the age and activity requirement, 11 patients
receiving total laminectomy in this group adopted spinal dynamic
pedicle screw fixation or replantation of lamina or bone graft
fusion and internal fixation. Semi-laminectomy has less affect on
spinal stability, so 10 patients receiving semi-laminectomy in this
group did not adopt the internal fixation, and no significant
spinal instability was found during the follow-up for 48 months
after operation. Moreover, 6 patients receiving semi-laminectomy
combined with facetectomy on the affected side adopted the internal
fixation.
Dural sac often needs to be opened in such surgery,
so the cerebrospinal fluid leakage is more common after operation.
Yang et al (20) reported
their experience that the drainage and infection prevention time
should be appropriately prolonged and drainage port should be
locally sutured after drainage tube is removed. Ten patients
suffered from cerebrospinal fluid leakage after operation, so the
position was adjusted (Trendelenburg positionor dorsal elevated
position), followed by wound dressing and pressure dressing (thick
cotton cushion and elastic bandage could be used locally); the
drainage time was prolonged appropriately, fluid infusion was
enhanced and non-vacuum drainage was adopted. There were 3 cases of
refractory cerebrospinal fluid leakage, and the wound was sutured
in debridement and healed. We think that the prevention of
cerebrospinal fluid leakage is very important, and the dural sac
opened during operation should be closely and continuously sutured
using 6–0 non-invasive stitches with the stitch controlled within 1
mm. Multiple suture is not appropriate for patients with dural tear
during operation, due to dural thinning and increased brittleness,
because the tear will be larger; so the adjacent fascial flap can
be used to cover the tear. When the incision is sutured, the muscle
layer should be aligned closely without dead space, and the fascia,
subcutaneous tissue and skin should be sutured layer by layer.
Acknowledgements
This study was supported by the Project of
Invigorating Health Care through Science, Technology and Education
(Jiangsu Provincial Medical Youth Talent) and Changzhou High-level
Medical Talents Training Project (2016CZBJ029).
References
|
1
|
Weber C, Gulati S, Jakola AS, Habiba S,
Nygaard ØP, Johannesen TB and Solheim O: Incidence rates and
surgery of primary intraspinal tumors in the era of modern
neuroimaging: A national population-based study. Spine.
39:E967–E973. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pan Z, Yang G, He H, Zhao G, Yuan T and Li
Y, Shi W, Gao P, Dong L and Li Y: Concurrent radiotherapy and
intrathecal methotrexate for treating leptomeningeal metastasis
from solid tumors with adverse prognostic factors: A prospective
and single-arm study. Int J Cancer. 139:1864–1872. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sowash M, Barzilai O, Kahn S, McLaughlin
L, Boland P, Bilsky MH and Laufer I: Clinical outcomes following
resection of giant spinal schwannomas: A case series of 32
patients. J Neurosurg Spine. 26:494–500. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Merhemic Z, Stosic-Opincal T and Thurnher
MM: Neuroimaging of Spinal Tumors. Magn Reson Imaging Clin N Am.
24:563–579. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Safaee MM, Lyon R, Barbaro NM, Chou D,
Mummaneni PV, Weinstein PR, Chin CT, Tihan T and Ames CP:
Neurological outcomes and surgical complications in 221 spinal
nerve sheath tumors. J Neurosurg Spine. 26:103–111. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
dos Santos MP, Zhang J, Ghinda D,
Glikstein R, Agid R, Rodesch G, Tampieri D and terBrugge KG:
Imaging diagnosis and the role of endovascular embolization
treatment for vascular intraspinal tumors. Neurosurg Focus.
39:E162015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Masaryk TJ: Neoplastic disease of the
spine. Radiol Clin North Am. 29:829–845. 1991.PubMed/NCBI
|
|
8
|
Bendszus M, Urbach H, Wolf HK, Schramm J
and Solymosi L: Magnetic resonance imaging of intraspinal melanotic
schwannoma. Eur Radiol. 8:11971998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee RR: MR imaging of intradural tumors of
the cervical spine. Magn Reson Imaging Clin N Am. 8:529–540.
2000.PubMed/NCBI
|
|
10
|
Ahn DK, Park HS, Choi DJ, Kim KS, Kim TW
and Park SY: The surgical treatment for spinal intradural
extramedullary tumors. Clin Orthop Surg. 1:165–172. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zong S, Wu Y, Tao Y, Chen X, Fang Y, Du L,
Zhao J and Zeng G: Treatment results in different surgical
approaches for intraspinal tumor in 51 patients. Int J Clin Exp
Med. 8:16627–16633. 2015.PubMed/NCBI
|
|
12
|
Viereck MJ, Ghobrial GM, Beygi S and
Harrop JS: Improved patient quality of life following intradural
extramedullary spinal tumor resection. J Neurosurg Spine.
25:640–645. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang Q, Ni M, Liu WM, Jia W, Jia GJ and
Zhang JT: Intra- and extramedullary dumbbell-shaped schwannoma of
the medulla oblongata: A case report and review of the literature.
World Neurosurg. 98:873.e1–873.e7. 2017. View Article : Google Scholar
|
|
14
|
Iacopino DG, Giugno A, Gulì C, Basile L,
Graziano F and Maugeri R: Surgical nuances on the treatment of
giant dumbbell cervical spine schwannomas: Description of a
challenging case and review of the literature. Spinal Cord Ser
Cases. 2:150422016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Das JM and Peethambaran A: Total excision
of a giant ventral midline cervical spinal intradural schwannoma
via posterior approach. Asian Spine J. 10:153–157. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schultheiss R and Gullotta G: Resection of
relevant nerve roots in surgery of spinal neurinomas without
persisting neurological deficit. Acta Neurochir (Wien). 122:91–96.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Celli P: Treatment of relevant nerve roots
involved in nerve sheath tumors: Removal or preservation?
Neurosurgery. 51:684–692. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang P, He X, Li H, Zang Q and Wang G:
Therapy for thoracic lumbar and sacral vertebrae tumors using total
spondylectomy and spine reconstruction through posterior or
combined anterior-posterior approaches. Oncol Lett. 11:1778–1782.
2016.PubMed/NCBI
|
|
19
|
Hussein HA and Goda HA: Paravertebral
neurogenic tumors with intraspinal extension: Preoperative
evaluation and surgical approach. J Egypt Natl Canc Inst. 21:12–22.
2009.PubMed/NCBI
|
|
20
|
Yang B, Wang Y, He X and Li H: Treatment
for thoracic ossification of posterior longitudinal ligament with
posterior circumferential decompression: Complications and
managements. J Orthop Surg. 11:1532016. View Article : Google Scholar
|