Introduction
Primary vaginal cancer, including squamous cell
carcinoma, adenocarcinoma, melanoma and sarcoma, is an uncommon
type of malignancy. By convention, if both the cervix and vagina
are involved, the primary diagnosis is cervical cancer. Surgery
serves an important role in the treatment of primary vaginal and
cervical cancer in patients with early stage disease (1,2). The
5-year survival rate for stage I carcinomas is 73% after surgical
therapy (1).
Non-Hodgkin's lymphoma (NHL) with the female genital
tract as the primary site is rare; the National Cancer Database
reported that only 1.5% of extra-nodal NHL originates in the female
genital tract (3). Surgery does not
serve a role in the treatment of this disease, as chemotherapy is
relatively effective (4). As a
result, it is important for gynecologists to be aware of this
disease in the differential diagnosis of gynecological cancer. The
present case report illustrates the presentation, diagnosis and
appropriate treatment of primary extra-nodal non-Hodgkin's lymphoma
of the vagina (PNHLV).
Case report
A 54-year-old woman was referred to the gynecology
outpatient clinic of Shandong Cancer Hospital Affiliated to
Shandong University with a 2-month history of vaginal bleeding. The
patient provided written informed consent to participate in the
present case report. The patient did not report any other symptoms,
including fever, night sweats, weight loss or fatigue (‘B’
symptoms), and they had no notable past medical history. Upon
digital rectal examination, a palpable mass was discovered between
the rectum and vagina, apparently invading the rectal mucosa. The
colposcopy revealed a thickening of the posterior vaginal wall.
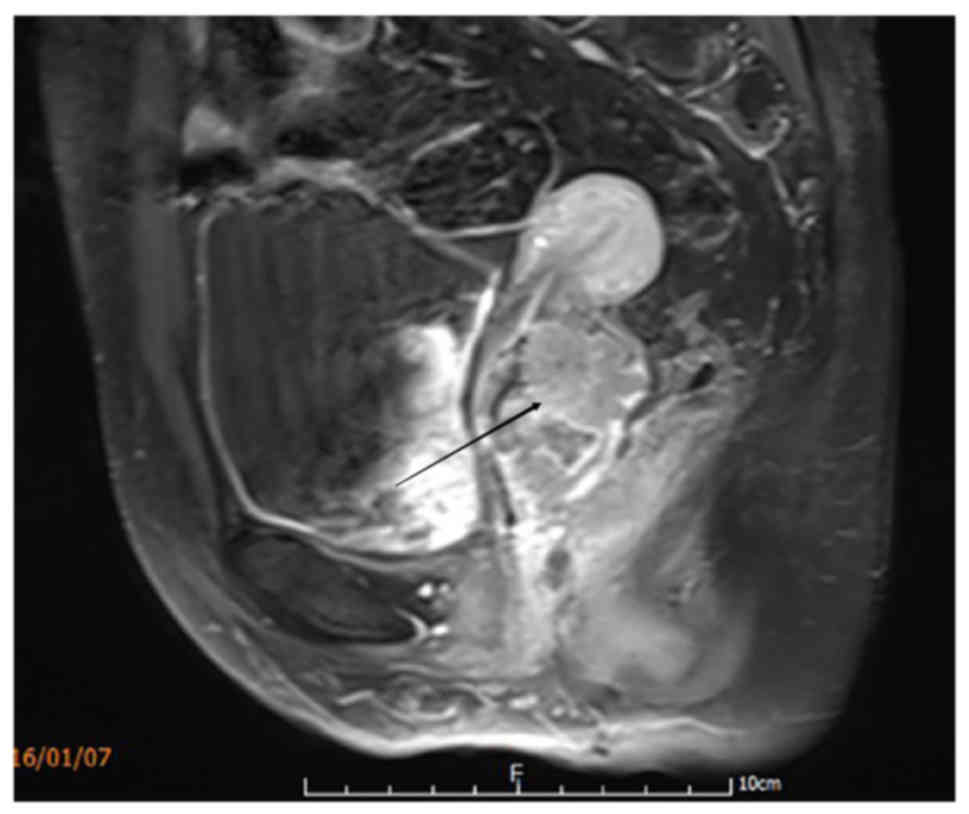
Magnetic resonance imaging (MRI) (Fig.
1) of the pelvis and ultrasonography revealed a diffuse mass
with a diameter of ~6 cm in the external cervical orifice and
invading the vagina. The uterus and bladder were not involved.
On admission, the following laboratory parameters
were noted: Blood cell count 4.1×1012/l (normal range,
4.0–5.0×1012/l); dehydrogenase 181 U/l (normal range,
109–245 U/l); and cancer antigen-125; 29 kU/ml (normal range,
0–35.0 kU/ml). Baseline renal and liver function test results were
also normal. Hepatitis B virus markers, hepatitis C virus antibody
(Ab) and human immunodeficiency virus Ab tests were negative. Based
on physical examination and laboratory findings, a surgical
exploration was performed following a suspected diagnosis of
cervical carcinoma or primary vaginal carcinoma. The mass was
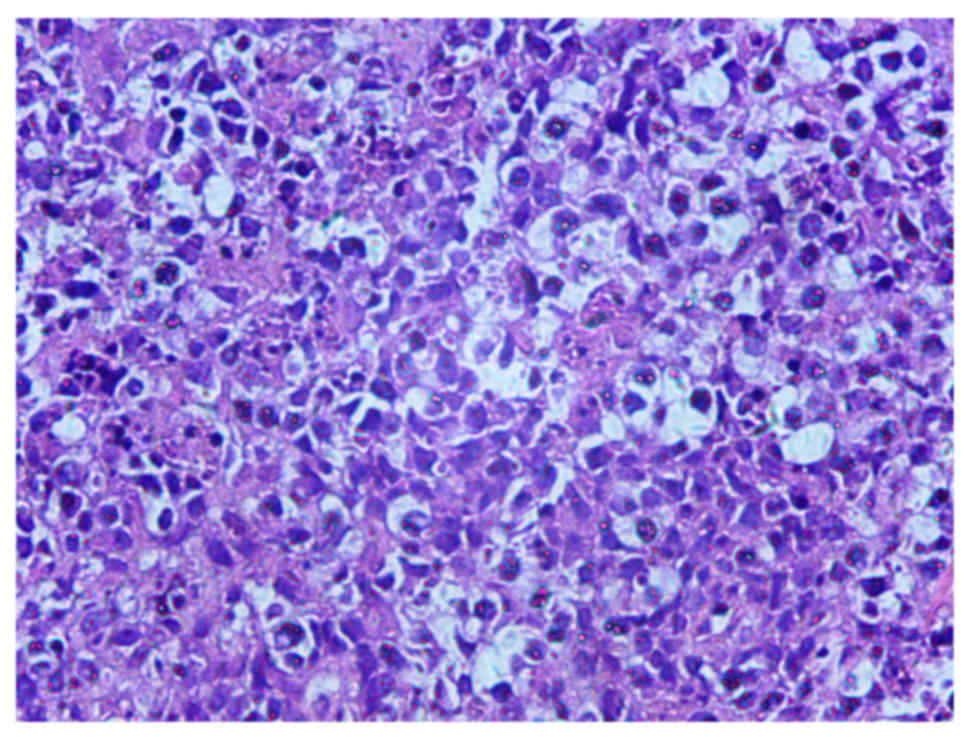
resected from the patient under anesthesia (Fig. 2). Immunohistochemistry and biopsy
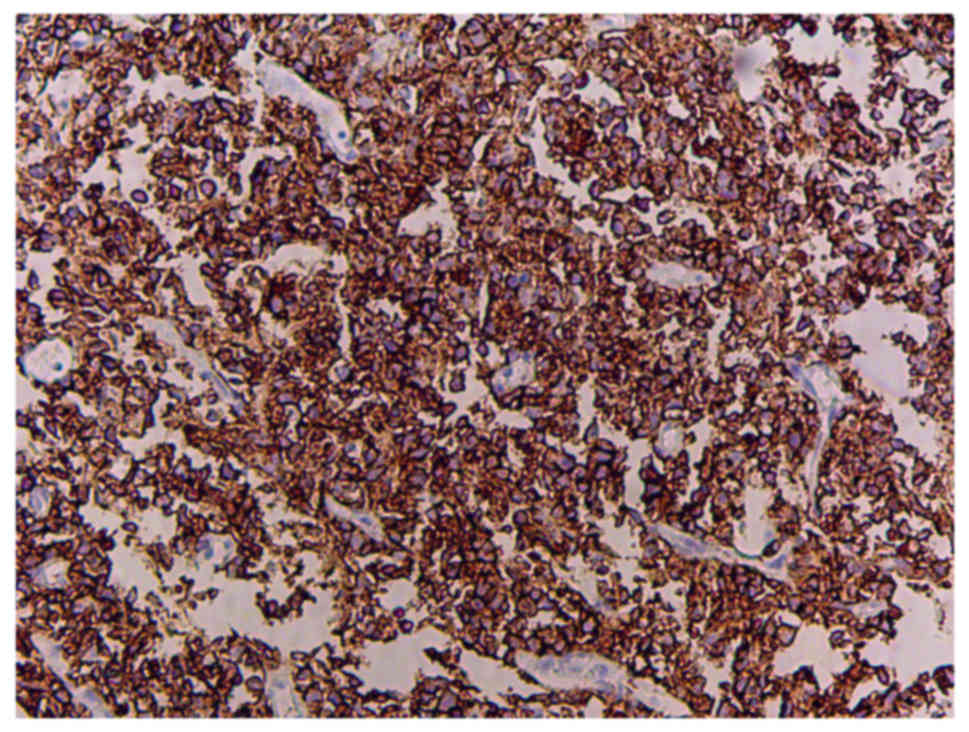
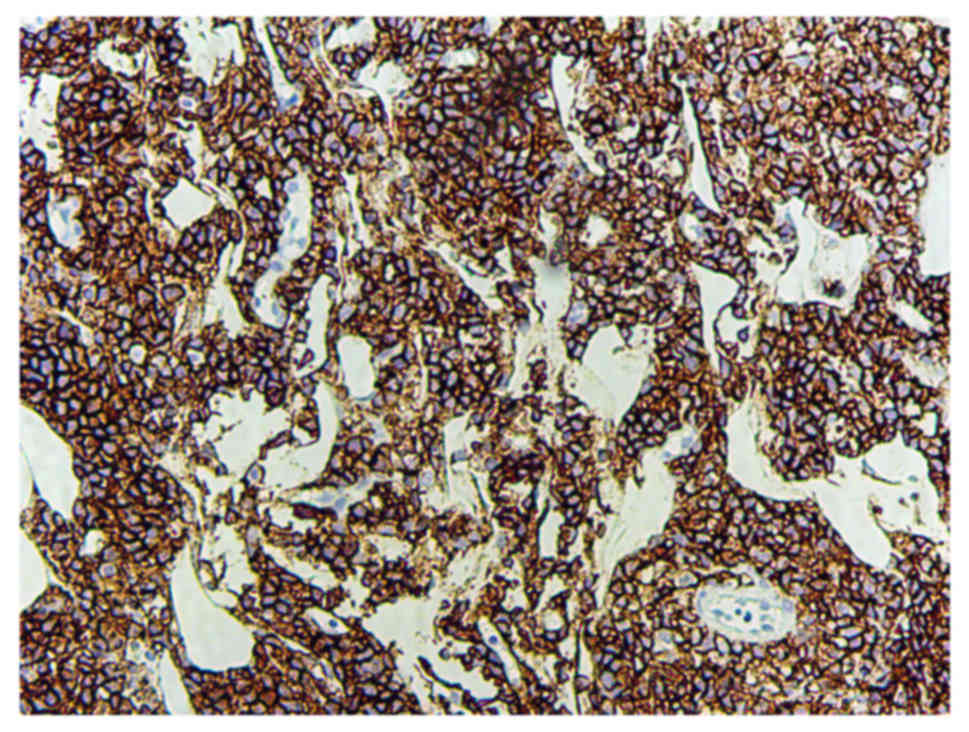
confirmed the lymphoid origin of the neoplasm (Fig. 3), and tumor cells were positive for
cluster of differentiation 20 (CD20) (Fig. 4) and CD79a (Fig. 5). The bone marrow aspirate and biopsy
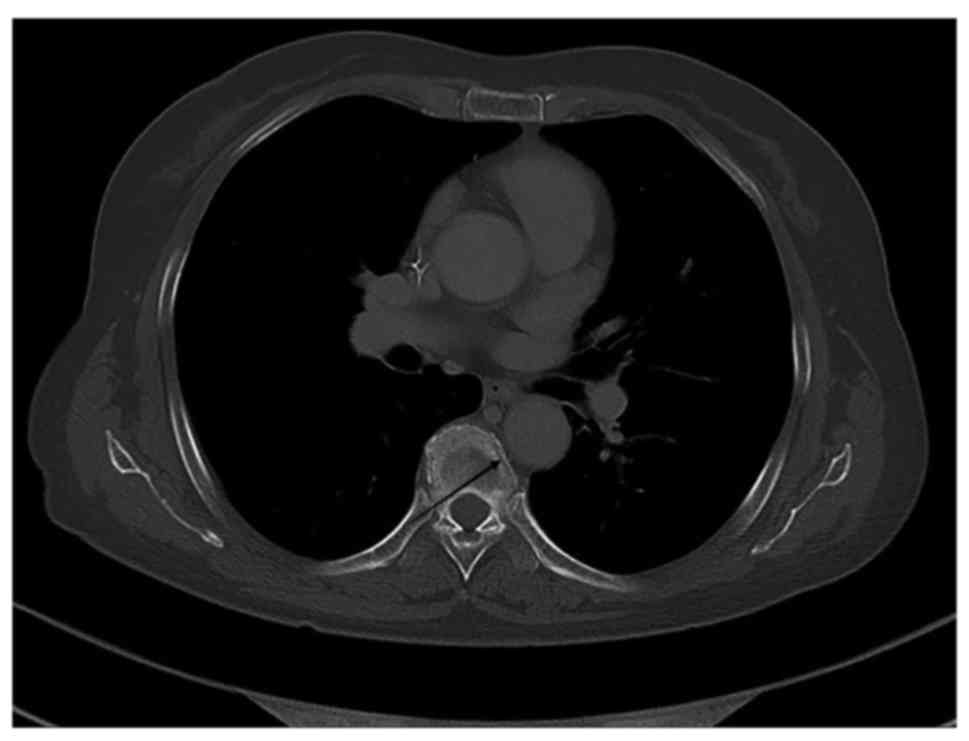
did not reveal lymphomatous infiltration. A computed tomography
(CT) scan of the chest and abdomen did not detect metastasis to
other locations. The patient was diagnosed with stage IE primary
vaginal large B-cell NHL disease based on the Ann Arbor system
(5) for staging NHL. One month after
the surgery, oncologists reviewed the patient and recommended 6
cycles of the CHOP regime (1,000 mg cyclophosphamide on days 1 and
8, 50 mg doxorubicin on day 1, vincristine 2 mg on day 1 and 100 mg
prednisone on days 1–5 for 21 days/cycle). Rituximab was not used
in the chemotherapy regimen for financial reasons.
Following 2 cycles of chemotherapy, CT scans of the
pelvis, abdomen and thorax were negative. Following the 6 cycles of
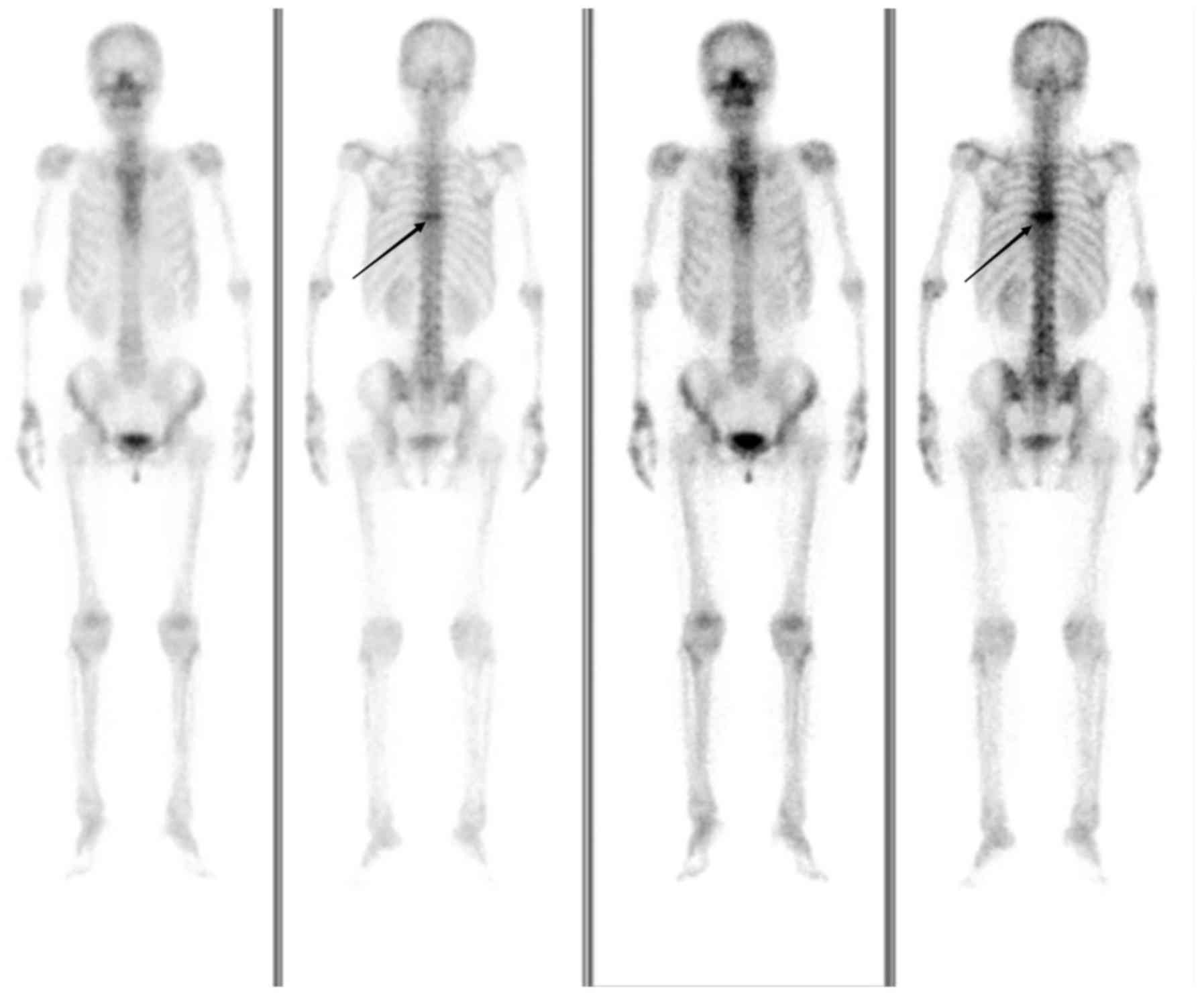
chemotherapy, a CT scan (Fig. 6) and
whole-body bone imaging (Fig. 7)
revealed evidence of thoracic vertebral body metastasis. However,
the abdomen and pelvis were negative for NHL. The patient received
palliative radiation (36 Gy in 20 fractions) for the vertebral body
metastasis. At time of publication, the patient was reviewed every
three months and no recurrence or other metastasis had been
observed.
Discussion
Fewer than 0.5% of all cases of extra-nodal NHL
involve the female genital tract (5).
Chorlton et al (6) reviewed
~9,500 cases of lymphomas in women and observed only 4 cases of
primary vaginal lymphoma. Primary vaginal lymphomas are reported in
patients from a wide range of ages, with a mean age at presentation
of 42 years (range, 26–66 years) (7).
Guastafierro et al (8) identified that 63 patients with primary
extra-nodal NHL of the vagina were reported between 1954 and 2012.
The most common histological feature was diffuse large B-cell NHL
(DLBCL; 40/58 evaluable cases, 69%). At diagnosis, the most common
clinical presentations were vaginal bleeding (34.8%), vaginal
masses (23.9%), vaginal discharge (17.4%) and abdominal and/or
pelvic pain (15.2%), with 13% being fully asymptomatic (8). As indicated in the present case report,
‘B’ symptoms at diagnosis of NHL of the vagina are exceedingly rare
compared with other lymphomas. Therefore, non-specific clinical
findings usually delay the diagnosis of this disease.
In general, the prognosis for extra-nodal lymphoma
is worse than nodal lymphoma, primarily due to the inaccurate or
delayed diagnosis and inadequate treatment (3). It is important for gynecologists to be
aware of this disease in the differential diagnosis of
gynecological cancer. In practice, irregular vaginal bleeding is
often indicative of gynecological pathology, with the initial
diagnostic step a Pap smear test and/or colposcopy. In DLBCL,
sheets of neoplastic cells infiltrate deeply into the stroma,
producing a dense sclerosis. The lymphoma cells lack tropism for
the overlying epithelium, and lymphoepithelial lesions are not
observed (9). The sensitivity of a
conventional Pap smear for the detection of malignant lymphoma is
low, ranging between 20 and 30% (10). Colposcopy results are unremarkable
(11), and may mislead clinicians, as
in the case of the subject of the present case report.
Zeppa et al (12) demonstrated that fine-needle aspiration
cytology (FNAC) coupled with flow cytometry is effective in the
cytological diagnosis and classification of NHL with reproducible
results. However, the lack of diagnostic material and other
clinicopathological limitations may represent an obstacle to
achieving accurate diagnosis. As a result, a biopsy is the
preferable option, while FNAC may be performed in patients for whom
excisional biopsy is contraindicated, or in the case of ancillary
studies (8). In the present case
report, NHL was not suspected clinically and may have been missed
without biopsy and tissue diagnosis.
The differential diagnosis of vaginal NHL includes
other hematopoietic lesions (including granulocytic sarcoma and
Langerhan's cell histiocytosis), carcinoma, malignant mixed
Mullerian tumor, epithelioid leiomyosarcoma and endometrial stromal
tumors, including endometrial stromal sarcoma, melanoma and
extraosseous Ewing's sarcoma/primitive neuroectodermal tumor
(13). The pathological diagnosis of
DLBCL is based on morphology and immunophenotyping. DLBCL is a
heterogeneous group of tumors consisting of large, transformed B
cells with prominent nucleoli, a basophilic cytoplasm, a diffuse
growth pattern and a high proliferation fraction. Tumor cells
generally express pan-B cell antigens, including CD19, CD20, CD22
and CD79a (14). A screening panel
consisting of CD45, CD3, CD20 and cytokeratin is useful in
determining whether the tumor is a B-cell lymphoma (CD20+), T-cell
lymphoma (CD3+), granulocytic sarcoma (only CD45+) or carcinoma
(cytokeratin+) (9).
CT and/or positron emission tomography (PET) imaging
of the pelvis may provide valuable information regarding the sites
involved in NHL, particularly with respect to nodular involvement.
In addition, these techniques, in conjunction with bone marrow
biopsy, aid in the staging of disease (4,15). Initial
imaging serves both to determine disease stage at diagnosis and to
provide baseline measurements for comparison to determine the
response to treatment (14).
It is important to recognize the prognostic factors
of NHL in order to identify the patients who may be refractory to
standard therapy as early as possible and to enable them to benefit
from more intensive treatments. PET scanning has been used for the
surveillance and assessment of the response to treatment (16). The end-of-treatment PET scan is highly
predictive of progression-free survival (PFS). Among 88 DLBCL
patients treated with 6–8 courses of R-CHOP, patients with a
negative final PET scan achieved a 2-year PFS of 83%, compared with
64% for patients with a positive final PET scan (P<0.001)
(17). Elevated serum levels of
cancer antigen-125 at the time of diagnosis have been associated
with a decreased 5-year survival rate (18). Vang et al (7) demonstrated that patients with low-stage
vaginal NHL usually have an excellent prognosis.
On the other hand, the observation that the
prognosis of extra-nodal NHL is worse than that for nodal lymphoma
may be associated with substandard treatment (19). According to the National Cancer
Database, only 46% of patients with extra-nodal lymphoma were
treated with any chemotherapy, compared with 70% of patients with
nodal lymphoma (3).
There is no established treatment for primary NHL of
the vagina, most likely due to its rarity. According to recent
international guidelines (20), the
treatment for early stage DLBCL is chemotherapy with R-CHOP with or
without subsequent local radiation therapy. In a review by
Signorelli et al (21), which
evaluated 10 cases of extra-nodal genital lymphoma treated with the
CHOP or R-CHOP regimen, 9 complete responses were observed. In a
case reported by Guastafierro et al (8), the patient remained in complete
remission for 72 months following chemotherapy with 8 cycles of the
R-CHOP regime. Signorelli et al (21) reported on a patient with stage IEA NHL
of the vagina who underwent complete remission following treatment
with the MACOP-B regimen (methotrexate with leucovorin rescue,
doxorubicin, cyclophosphamide, vincristine, prednisone and
bleomycin), and the patient gave birth four years after the
treatment. As these tumors are highly responsive to chemotherapy,
surgery is not the primary mode of therapy for NHL (15).
In modern clinical practice, the R-CHOP treatment
regimen has proven to be highly effective and radiation therapy
(RT) is slowly being phased out as a treatment option for DLBCL.
Modern advanced imaging and conformal RT techniques now enable the
treatment of larger and anatomically more challenging target
volumes with much less radiation exposure than normal tissues and,
consequently, much lower risks of long-term complications (22). Different forms of RT, including
involved-field RT, involved-node RT and involved-site RT, may be
used alongside these ‘new-age’ treatment strategies to further
improve prognostic outcomes and overall survival rates.
Nevertheless, RT remains an important treatment method and may be
used instead of certain treatments, including the treatment of
patients who are unresponsive to or develop complications from the
use of chemotherapy (23). A study by
Held et al (24) provided
strong support for adding RT in the treatment of large (≥7.5 cm in
diameter) tumors in elderly patients (>60 years of age) with
aggressive B-cell lymphoma. However, it is unclear whether or not a
positive post-chemotherapy PET scan can identify patients who are
likely to benefit from RT (22).
Therefore, RT may be reserved for chemo-resistant disease, disease
failing to achieve remission following chemotherapy, or sites of
large tumors.
In conclusion, primary NHL of the vagina occurs
rarely. Early diagnosis and standard treatment lead to improved
survival rates for the affected patients. The present case report
aims to raise awareness of this rare disease, which must be
considered in the differential diagnosis of genital tract diseases.
Radical surgery does not serve a role in the treatment of vaginal
NHL, as chemotherapy is relatively effective.
References
|
1
|
Creasman WT, Phillips JL and Menck HR: The
national cancer data base report on cancer of the vagina. Cancer.
83:1033–1040. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Otton GR, Nicklin JL, Dickie GJ, Niedetzky
P, Tripcony L, Perrin LC and Crandon AJ: Early-stage vaginal
carcinoma-an analysis of 70 patients. Int J Gynecol Cancer.
14:304–310. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Trenhaile TR and Killackey MA: Primary
pelvic non-Hodgkin's lymphoma. Obstet Gynecol. 97:717–720. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ragupathy K and Bappa L: Primary vaginal
non-Hodgkin lymphoma: Gynecologic diagnosis of a hematologic
malignancy. J Low Genit Tract Dis. 17:326–329. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lister TA, Crowther D, Sutcliffe SB,
Glatstein E, Canellos GP, Young RC, Rosenberg SA, Coltman CA and
Tubiana M: Report of a committee convened to discuss the evaluation
and staging of patients with Hodgkin's disease: Cotswolds meeting.
J Clin Oncol. 7:1630–1636. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chorlton I, Karnei RF Jr, King FM and
Norris HJ: Primary malignant reticuloendothelial disease involving
the vagina, cervix, and corpus uteri. Obstet Gynecol. 44:735–748.
1974.PubMed/NCBI
|
|
7
|
Vang R, Medeiros LJ, Silva EG, Gershenson
DM and Deavers M: Non-Hodgkin's lymphoma involving the vagina: A
clinicopathologic analysis of 14 patients. Am J Surg Pathol.
24:719–725. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guastafierro S, Tedeschi A, Criscuolo C,
Celentano M, Cobellis L, Rossiello R and Falcone U: Primary
extranodal non-Hodgkin's lymphoma of the vagina: A case report and
a review of the literature. Acta Haematol. 128:33–38. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lagoo AS and Robboy SJ: Lymphoma of the
female genital tract: Current status. Int J Gynecol Pathol.
25:1–21. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Harris NL and Scully RE: Malignant
lymphoma and granulocytic sarcoma of the uterus and vagina. A
clinicopathologic analysis of 27 cases. Cancer. 53:2530–2545. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hanley KZ, Tadros TS, Briones AJ, Birdsong
GG and Mosunjac MB: Hematologic malignancies of the female genital
tract diagnosed on liquid-based Pap test: Cytomorphologic features
and review of differential diagnoses. Diagn Cytopathol. 37:61–67.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zeppa P, Vigliar E, Cozzolino I, Troncone
G, Picardi M, De Renzo A, Grimaldi F, Pane F, Vetrani A and
Palombini L: Fine needle aspiration cytology and flow ytometry
immunophenotyping of non-Hodgkin lymphoma: Can we do better.
Cytopathology. 21:300–310. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vang R, Medeiros LJ, Ha CS and Deavers M:
Non-Hodgkin's lymphomas involving the uterus: A clinicopathologic
analysis of 26 cases. Mod Pathol. 13:19–28. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Silva V, Correia P, Oliveira N and Sá L:
Primary vaginal non-Hodgkin's lymphoma: Report of a rare clinical
entity. Clin Pract. 5:8212015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kendrick JE IV and Straughn JM Jr: Two
cases of non-Hodgkin's lymphoma presenting as primary gynecologic
malignancies. Gynecol Oncol. 98:490–492. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lavely WC, Delbeke D, Greer JP, Morgan DS,
Byrne DW, Price RR and Hallahan DE: FDG PET in the follow-up
management of patients with newly diagnosed Hodgkin and non-Hodgkin
lymphoma after first-line chemotherapy. Int J Radiat Oncol Biol
Phys. 57:307–315. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pregno P, Chiappella A, Bellò M, Botto B,
Ferrero S, Franceschetti S, Giunta F, Ladetto M, Limerutti G, Menga
M, et al: Interim 18-FDG-PET/CT failed to predict the outcome in
diffuse large B-cell lymphoma patients treated at the diagnosis
with rituximab-CHOP. Blood. 119:2066–2073. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zacharos ID, Efstathiou SP, Petreli E,
Georgiou G, Tsioulos DI, Mastorantonakis SE, Christakopoulou I and
Roussou PP: The prognostic significance of CA 125 in patients with
non-Hodgkin's lymphoma. Eur J Haematol. 69:221–226. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cohn DE, Resnick KE, Eaton LA, deHart J
and Zanagnolo V: Non-Hodgkin's lymphoma mimicking gynecological
malignancies of the vagina and cervix: A report of four cases. Int
J Gynecol Cancer. 17:274–279. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tilly H, Gomes da Silva M, Vitolo U, Jack
A, Meignan M, Lopez-Guillermo A, Walewski J, André M, Johnson PW,
Pfreundschuh M, et al: Diffuse large B-cell lymphoma (DLBCL): ESMO
Clinical Practice Guidelines for diagnosis, treatment and
follow-up. Ann Oncol. 26 Suppl 5:v116–v125. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Signorelli M, Maneo A, Cammarota S,
Isimbaldi G, Garcia Parra R, Perego P, Maria Pogliani E and
Mangioni C: Conservative management in primary genital lymphomas:
The role of chemotherapy. Gynecol Oncol. 104:416–421. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Specht L: Does radiation have a role in
advanced stage Hodgkin's or non-Hodgkin lymphoma? Curr Treat
Options Oncol. 17:42016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mendes F, Domingues C, Teixo R, Abrantes
AM, Gonçalves AC, Nobre-Gois I, Jacobetty M, Sarmento AB, Botelho
MF and Rosa MS: The importance of radiotherapy on diffuse large B
cell lymphoma treatment: A current review. Cancer Metastasis Rev.
34:511–525. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Held G, Murawski N, Ziepert M,
Fleckenstein J, Pöschel V, Zwick C, Bittenbring J, Hänel M, Wilhelm
S, Schubert J, et al: Role of radiotherapy to bulky disease in
elderly patients with aggressive B-cell lymphoma. J Clin Oncol.
32:1112–1118. 2014. View Article : Google Scholar : PubMed/NCBI
|