Introduction
Autoimmune diseases are caused by immune
complex-induced activation of the complement system and subsequent
inflammation, both of which injure tissues (1). Recent studies have revealed an
association between autoimmune diseases, including rheumatoid
arthritis and thyroiditis, and worse survival in patients with
lung, breast, or thyroid cancers (2–4); however,
the underlying mechanism is still unclear.
Anaphylatoxin C5a, an N-terminal 74-amino acid
fragment of the α-chain of the complement fifth component (C5)
(5), is a byproduct of complement
activation and functions as a leukocyte chemoattractant and
inflammatory mediator (6,7). There is emerging evidence supporting a
role for C5a in cancer. C5a recruits myeloid-derived suppressor
cells (MDSCs) that inhibit the CD8+ cytotoxic T
cell-mediated anti-tumor response (8), facilitating increased survival of cancer
cells. C5a induces endothelial cell chemotaxis and blood vessel
formation (9), thereby promoting
neovascularization (10). Thus, C5a
indirectly aids cancer development and progression by creating a
microenvironment favorable for cancer cells. C5a acts by binding to
the C5a receptor (C5aR; CD88) on the cell membrane (11). We previously showed that a variety of
cancer cells aberrantly express C5aR at varying rates in organs,
and that C5a enhances cancer cell mobility, matrix metalloprotease
(MMP) secretion, and invasiveness in vitro and in nude mouse
skin via C5aR (12). Thus, the
C5a-C5aR system was suggested to be directly involved in cancer
progression. Activation of the complement system has been shown to
occur in cancer tissues in human specimens (13,14) and
animal models (8,9), indicating generation of C5a in the
cancer microenvironment. Moreover, human cancer cells release C5a
from human C5 and plasma via a serine protease on the cell membrane
(15). The survival rates of patients
with C5aR-positive or highly expressing non-small cell lung
(16), breast (17), urothelial (18), clear cell renal (19), and gastric cancers (20,21) are
lower than those of patients with the corresponding C5aR-negative
cancers. It is likely that the C5a-C5aR system promotes human
cancer. C5a enhances cancer cell activities in a
concentration-dependent manner (12)
and the plasma C5a level was elevated in patients with autoimmune
diseases, such as systemic lupus erythematosus (22) or rheumatoid arthritis (23). Accordingly, cancer promotion by the
C5a-C5aR system may be exaggerated in autoimmune diseases.
The Arthus reaction is a model of autoimmune
diseases and caused by immune complex-triggered complement
activation (24,25). To explore the mechanism underlying the
poor prognosis of cancer patients with autoimmune diseases
(2–4),
the effect of the Arthus reaction on cancer invasion and growth,
and MDSC recruitment was investigated using wild-type mice and
syngeneic cancer cells with or without C5aR expression. The
C5a-C5aR system was further examined in lung nodules formed by
cancer cells intravenously injected into mice and in uterine
cervical cancer invasion using clinically obtained tissue samples
of the cancer.
Materials and methods
Materials and animals
Recombinant human C5a and anti-human C5aR mouse
monoclonal IgG were purchased from EMD Millipore (Billerica, MA,
USA) and Hycult Biotech (Uden, The Netherlands), respectively. A
set of anti-Ki-67 antibody and EnVision+ solution was
purchased from Dako; Agilent Technologies, Inc., (Santa Clara, CA,
USA). Polyclonal anti-ovalbumin mouse IgG and anti-BSA mouse IgG
were purchased from Condrex (Redmond, WA, USA) and Rockland
(Limerick, PA, USA), respectively. Ovalbumin and bovine serum
albumin (BSA) were obtained from Sigma-Aldrich; Merck KGaA,
(Darmstadt, Germany). Anti-mouse Ly6g rat IgG labeled with
Cy-5® and anti-mouse CD11b rat IgG labeled with
fluorescein isothiocyanate (FITC) were from Abcam (Cambridge, UK).
The near-infrared ray cell labeling probes Qtracker 655 and
Qtracker 800 were from Thermo Fisher Scientific, Inc., (Waltham,
MA, USA). Other chemicals were purchased from Wako Pure Chemical
Industries (Osaka, Japan). Nude mice and Balb/c mice were supplied
by Kyudo Experimental Animal Corp., (Kumamoto, Japan). The animal
experiments were approved by the Kumamoto University Animal
Experiment Committee (A 29–29) and performed according to the
criteria of the Committee.
Cells
The human bile duct cancer cell line HuCCT1 was
provided by the Cell Resource Center for Biomedical Research
Institute of Development, Aging, and Cancer, Tohoku University
(Sendai, Japan). The mouse kidney cancer cell line Renca (CRL-2947)
was obtained from the American Type Culture Collection. The cells
were cultured in RPMI 1640 medium supplemented with 10% fetal
bovine serum (FBS), penicillin (40 U/ml), and streptomycin (40
µg/ml) and maintained at 37°C in 5% CO2. HuCCT1 and
Renca cells do not express C5aR, but we established HuCCT1 cells
stably expressing C5aR (HuCCT1/C5aR) by transfection with a plasmid
carrying human C5aR cDNA (12)
and Renca cells stably expressing C5aR (Renca/C5aR) by transfection
with a plasmid carrying mouse C5aR cDNA (26).
Invasion assay
Mouse cancer cells expressing C5aR and the control
cells from the same mother cells were necessary in the invasion
assay. Thus, previously established Renca/C5aR cells and Renca/mock
cells (26) were used. Renca/C5aR
cells and Renca/mock cells were incubated in 10 nM Qtracker 800 and
Qtracker 655, respectively, at a density of 1×107
cells/ml in PBS at 37°C for 1 h. The cells were washed with PBS and
suspended in PBS at 2×107 cells/ml. Equal volumes of the
Renca/C5aR and Renca/mock cell suspensions were mixed. To induce
the passive Arthus reaction, 10 µl of anti-ovalbumin or control
mouse IgG (10 mg/ml PBS) was added to 40 µl of the cell mixture,
and the mixture was injected intradermally into depilated Balb/c
mice sedated by an intraperitoneal (i.p.) injection of ketamine
(140 mg/kg body weight), followed by injection of 200 µl of
ovalbumin (10 mg/ml) via the tail vein. After 24 or 48 h, the mice
were sacrificed by cervical dislocation and cancer cell-injected
skin tissues were harvested, fixed in formalin and embedded in
paraffin. Fluorescence from the cells labeled with near-infrared
ray probes in 4-µm-thick tissue sections was measured using a
BZ-X710 fluorescence microscope (Keyence Corporation, Osaka,
Japan). Qtracker 800 and Qtracker 655 were observed at 810 nm
emission with 710 nm excitation and 630 nm emission with 560 nm
excitation and colored in green and red, respectively. To quantify
the distribution of cancer cells, the areas with fluorescent dots
representing labeled cells were encircled, and the area size was
measured using imaging analysis software (VH-Analyzer; Keyence
Corporation). The ratio of the distribution areas of Renca/C5aR
cells to those of Renca/mock cells was calculated.
Assessment of tumor growth and
myeloid-derived suppressor cell (MDSC) accumulation
Cell suspension (50 µl, 2×106 cells)
supplemented with anti-BSA or control mouse IgG (25 µg) was
injected intradermally into depilated Balb/c mice sedated by an
i.p. injection of ketamine (140 mg/kg body weight), followed by
injection of 200 µl of BSA (10 mg/ml) via the tail vein. The tumor
size was calculated by multiplying the lengths of the major and
minor axes. After 14 days, the mice were sacrificed by cervical
dislocation, tumors were harvested, and the 4-µm-thick frozen
sections were prepared and immunostained with anti-mouse Ly6g rat
IgG labeled with PE/Cy-5® (1:100 dilution) and
anti-mouse CD11b rat IgG labeled with FITC (1:100 dilution).
Fluorescence was observed with a fluorescence microscope (BZ-X710)
at 590–650 nm excitation and 662.5–737.5 nm emission for
PE/Cy-5® and at 450–490 nm excitation and 500–550 nm
emission for FITC. Double-positive cells, recognized as MDSCs
(27), were counted in five randomly
selected high-power fields (×400), and the average cell number per
high-power field was determined.
Assessment of nodule formation in the
lungs
Cancer cells expressing C5aR and control cells from
the same mother cells were used to assess lung nodule formation. As
bile duct cancer has the highest in C5aR-positive rate among human
cancers (12), it was suggested to be
most affected by the C5a-C5aR system. In a previous study, we
established HuCCT1/C5aR cells and HuCCT1/mock cells for the
previous study and demonstrated enhancement of HuCCT1/C5aR cell
invasion by C5a in the nude mouse skin (12). In connection with this study, we used
the same two HuCCT1 bile duct cancer cell lines. HuCCT1/C5aR and
HuCCT1/mock cells were incubated in RPMI 1640 medium in the
presence or absence of 100 nM C5a for 6 h. After washing with PBS,
cells were suspended in PBS (1×107 cells/ml) and 0.1 ml
of the suspension was injected into nude mice via the tail vein.
Six weeks later, the mice were sacrificed by cervical dislocation
and the lungs were harvested, fixed in formalin and embedded in
paraffin. Sections of 3-µm thickness were prepared from the
paraffin-embedded lungs for hematoxylin-eosin staining. For Ki-67
immunohistochemical staining, the deparaffinized lung sections were
autoclaved for 15 min in 10 mM citrate buffer, pH 6.0. The sections
were washed with PBS, incubated with anti-Ki-67 antibody (1:50
dilution) at room temperature for 1 h, and stained using
EnVision+ solution and 3,30-diaminobenzidine
tetrahydrochloride solution containing 0.006%
H2O2, according to the manufacturer's
instructions. Nuclei were counterstained with hematoxylin. To
evaluate nodule formation, nodules containing Ki-67-positive cells
were counted in five random microscopic fields (×100) in a section,
and the total number of nodules was determined.
C5aR immunohistochemistry
Uterine cervical tissue biopsy samples obtained from
the Kumamoto University Hospital from January to December 2015 and
diagnosed as cervical intraepithelial neoplasia (CIN3) or squamous
cell carcinoma stage I according to the FIGO staging system 2008
(28) were examined for C5aR
expression. Written informed consent for the tissue usage was
obtained from the patients, and the use of these tissues was
approved by the internal ethics committee (Rinri No. 706).
Cervical squamous cell carcinoma stage I differs
from CIN 3 in terms of tumor cells invasion from the epithelium;
thus, C5aR expression between the two stages may be compared to
explore possible involvement of the C5a-C5aR system in human cancer
invasion. Deparaffinized 3-µm-thick sections were pretreated with
0.3% H2O2 in methanol for 20 min, followed by
Protein Block, Serum-Free (Dako Cytomation, Glostrup, Denmark)
treatment for 20 min. The sections were incubated with anti-human
C5aR mouse monoclonal IgG (2 µg/ml) at room temperature for 1 h and
subsequently stained using EnVision+ solution and
3,30-diaminobenzidine tetrahydrochloride solution containing 0.006%
H2O2, according to the manufacturer's
instructions. Nuclei were counterstained with hematoxylin. Normal
mouse IgG was used rather than the primary antibody as a negative
control, and it did not react with the tissue sections. For each
section, high or low C5aR expression was defined as C5aR-positive
cancer cell area >30% or 0–30% of the total cancer cell area,
respectively, according to previous methods (29,30).
Statistical analyses
Experimental data were expressed as average ± SD.
Groups were compared using the Stata statistical software, release
15.1 (Stata Corp LP, College Station, TX, USA) by analysis of
variance (ANOVA) Wilcoxon rank-sum (Mann-Whitney) test for
nonparameric distribution followed by Bonferroni
multiple-comparison adjustment or Student's t-test for
normal distribution. The association of C5aR expression with
invasion in uterine cervical cancer was analyzed using Fisher's
exact test. P<0.05 was considered to indicate a statistically
significant difference.
Results
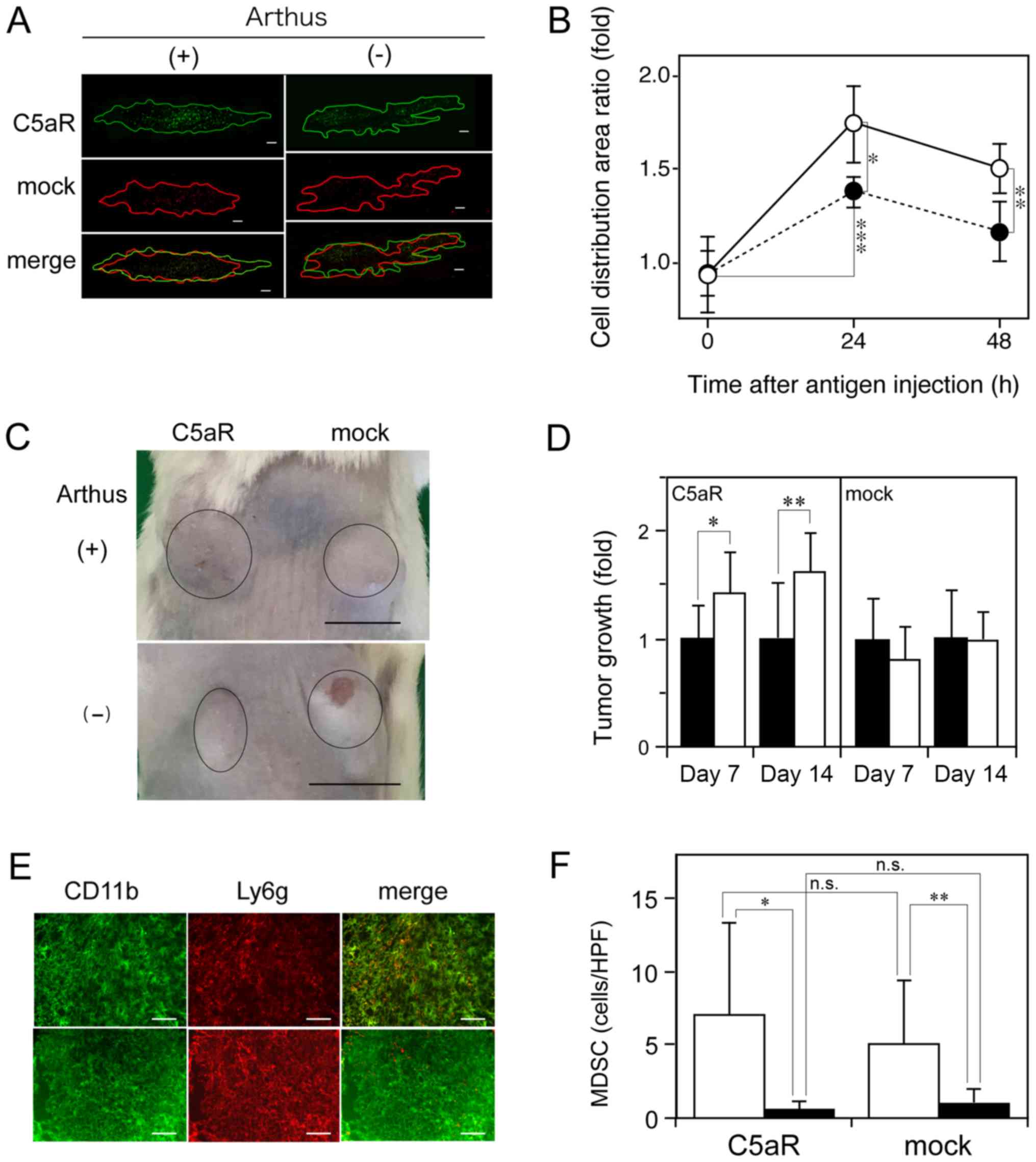
Arthus reaction enhances the invasion
and growth of C5aR-positive cancer cells and induces MDSC
recruitment
To determine whether autoimmune reactions affect
cancer progression, the Arthus reaction was induced in the Renca
cell-injected wild-type mouse skin site using the mouse
immune-complex, and the effect of the reaction on the spread of the
cells was studied. To avoid the immune response against Renca
cells, which were derived from a Balb/c mouse (31), Balb/c mice were used. To exclude
differences in experimental conditions (injection volume and site
and Arthus reaction intensity) between Renca/C5aR and Renca/mock
cells, the Renca-derived cells were mixed and injected into the
mouse skin with the mouse antibody, followed by intravenous
injection of the antigen. In the presence of the Arthus reaction,
Renca/C5aR cells spread to a larger area than Renca/mock cells did;
however, in the absence of the reaction, the distribution areas of
the two types of cells were not different (Fig. 1A). At 24 h after the initiation of the
reaction, the distribution area of Renca/C5aR cells was ~1.3-fold
larger than that of Renca/mock cells (Fig. 1B). The C5aR-dependent enhancement of
Renca cell invasion indicated that endogenous C5a contributed to
the enhanced cancer invasion induced by the Arthus reaction. Next,
we examined whether the Arthus reaction enhanced the tumor growth
of Renca cells inoculated in the wild-type mouse skin. In the
presence of the Arthus reaction, the tumor size of Renca/C5aR cells
increased by approximately 1.4-fold at day 7 and 1.6-fold at day
14, but the reaction did not affect the growth of tumors formed by
Renca/mock cells (Fig. 1C and D).
MDSCs suppress the CD8+ T cell-mediated anti-tumor
response (8), thus facilitating tumor
growth. Hence, the effect of the Arthus reaction on the
accumulation of MDSCs in Renca cell-injected sites was analyzed. A
considerable number of MDSCs (cells with yellow fluorescence in
merged images) was present in the skin sites after the Arthus
reaction, but few MDSCs were seen in the cancer tissue without the
reaction (Fig. 1E). The number of
recruited MDSCs was significantly increased by the Arthus reaction
in the cancer cell injection sites (Fig.
1F); however, no significant difference in MDSC number between
the sites injected with Renca/C5aR or Renca/mock cells was observed
(Fig. 1F). Thus, it is likely that
the enhanced tumor growth of Renca/C5aR cells by the Arthus
reaction (Fig. 1D) was caused by the
C5a-C5aR system rather than antitumor immune response suppression
by MDSCs.
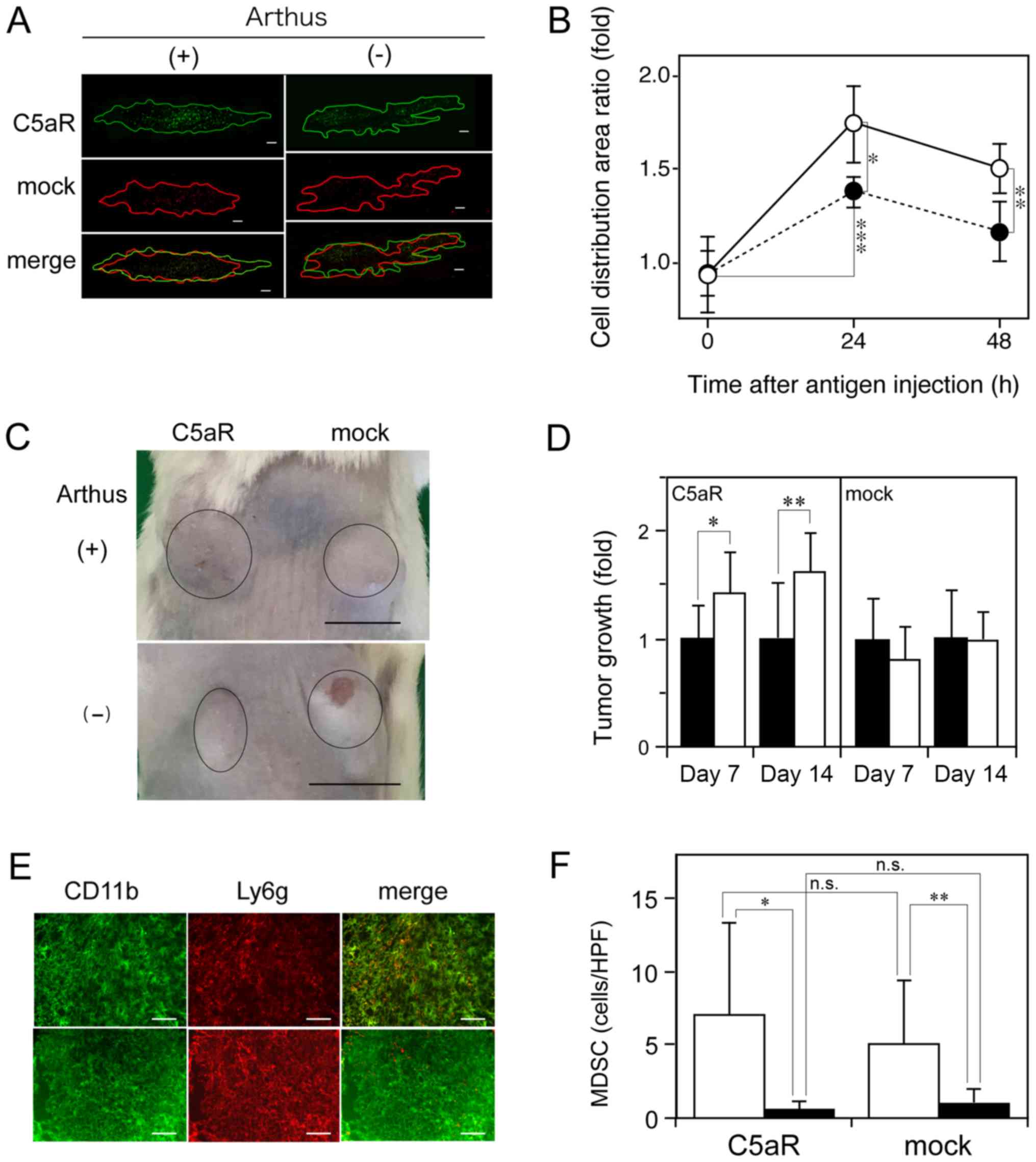 | Figure 1.Promotion of C5aR-positive cancer
cell invasion, tumor growth, and induction of MDSC recruitment by
the Arthus reaction. Renca/C5aR cells (green) and Renca/mock cells
(red) were labeled with different fluorescence probes, mixed, and
injected subcutaneously into a wild-type mouse in combination with
anti-ovalbumin mouse IgG or control IgG, followed by intravenous
injection of ovalbumin (A, B) or with anti-BSA mouse IgG or control
IgG, followed by intravenous injection of BSA (C-F). (A) Skin areas
showing fluorescence from Renca/C5aR cells and Renca/mock cells
(encircled in green and red lines, respectively), 24 h after
ovalbumin injection. Scale bar: 200 µm. (B) Ratio of fluorescence
distribution area of Renca/C5aR cells vs. that of Renca/mock cells
was calculated. The values indicate the mean ± SD (n=4). Open
circles: Anti-ovalbumin IgG; closed circles: Control IgG. Values
were compared by analysis of variance (ANOVA) followed by
Bonferroni multiple-comparison adjustment. *P=0.03, **P=0.067,
***P=0.008. (C) Images showing tumors at Renca cell-injected sites
in the presence or absence of the Arthus reaction at day 14. Tumors
are encircled in black lines. Scale bar: 1 cm. (D) Tumor growth at
7 and 14 days in sites subcutaneously injected with anti-BSA IgG
(open column) or control IgG (closed column) after an intravenous
BSA injection. Tumor size was measured and expressed as a ratio
relative to the average tumor size in the absence of the Arthus
reaction and vertical bars indicate the SD (n=6). *P=0.036,
**P=0.021. (E) Fluorescence immunohistochemistry of Renca/C5aR
cell-injected sites at day 14 using FITC-labeled anti-mouse CD11b
rat IgG and Cy-5®-labeled anti-mouse Ly6g rat IgG. Upper
and lower panels are from the sites where the Arthus reaction was
induced or not, respectively. Scale bar: 50 µm. (F) MDSCs
(CD11b+Ly6g+) were counted in the cancer
tissues where the Arthus reaction was induced (open column) or not
(closed column) and the average MDSCs/high-power field (HPF) ± SD
(n=6) were recorded. Values were compared by Wilcoxon rank-sum
(Mann-Whitney) test for nonparameric distribution followed by
Bonferroni multiple-comparison adjustment. *P=0.031, **P=0.031,
n.s, not significant. |
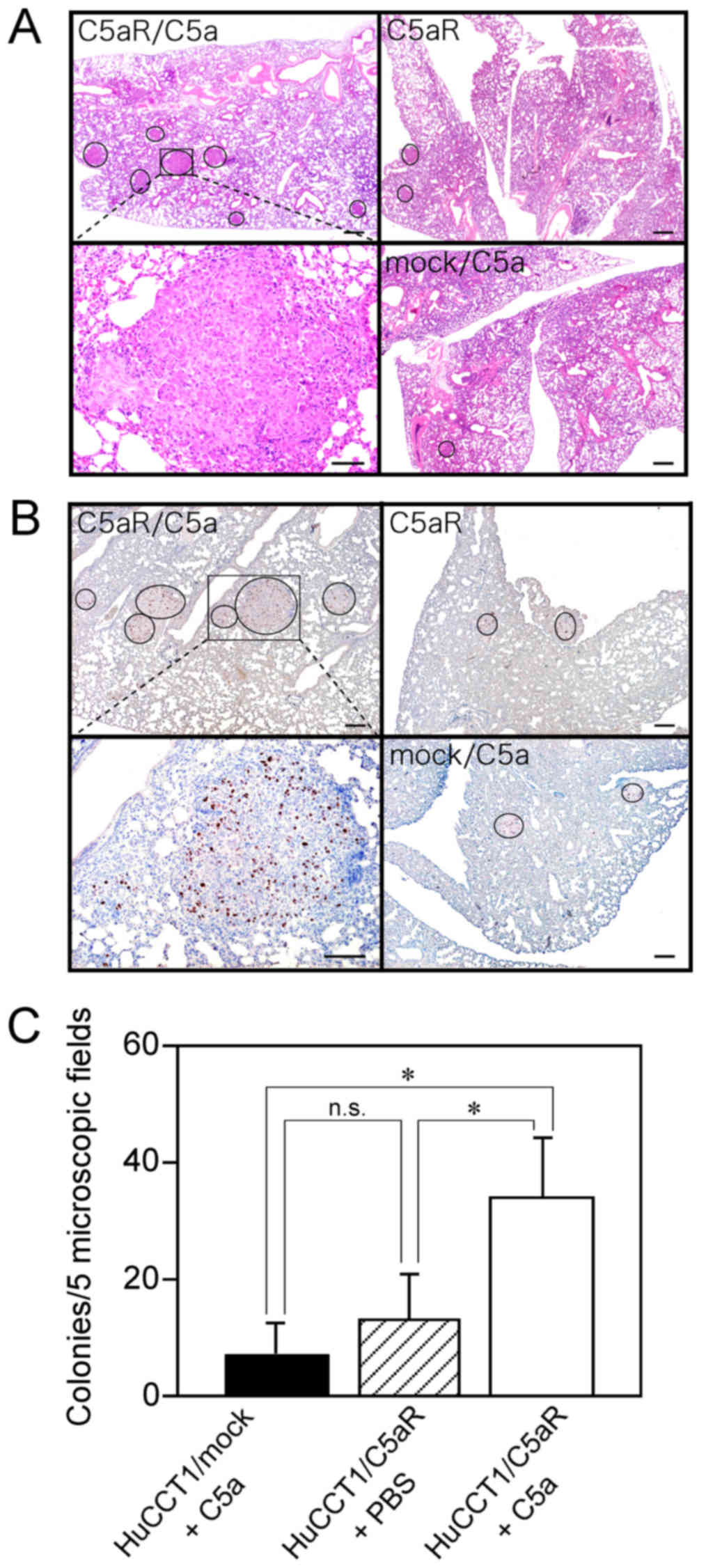
C5a promotes nodule formation of
C5aR-positive cancer cells in the lungs
C5a does not affect the anoikis of cancer cells
(26), but the positive correlation
of patients' cancer cell C5aR expression with vascular invasion in
the primary sites (20,21,26) and
with metastasis (16,17,26)
suggested the involvement of C5a in the entry of cancer cells into
the circulation through the endothelial layer and subsequent cancer
growth in metastasized organs. To further investigate the effect of
the C5a-C5aR system on cancer tumor growth, cancer cells were
injected intravenously into nude mice, and to evaluate tumor growth
cancer cell nodule formation in the lungs was examined. The lungs
appeared to be unchanged and no cancer cell nodules were visible
macroscopically. However, micro-nodules were observed in the lungs
microscopically (Fig. 2A). As these
nodules contained Ki-67-positive cells, they were recognized as
cancer cell nodules (Fig. 2B).
Nodules formed by C5a-stimulated C5aR-positive cancer cells
appeared larger, and the number of nodules was approximately
three-fold higher than that formed by non-stimulated C5aR-positive
cancer cells, which showed a nodule number almost equal to that of
C5a-stimulated C5aR-negative cancer cells (Fig. 2C). The enhanced lung nodule formation
by cancer cells inoculated intravenously supported the tumor growth
enhancement via the C5a-C5aR system (Fig.
1D) and suggested the possible participation of the system in
the promotion of cancer metastasis.
High C5aR expression is associated
with cervical cancer invasion in the uterus
In clinically obtained tissue samples, C5aR was
expressed in urothelial carcinoma cells at the invasive front
rather than the surface layer in the epithelium and in almost all
the cells in the deeper invasion site (18), which, together with high C5aR
expression in gastric cancer cells invading the adjacent blood
vessels (20,21), implies the involvement of the C5a-C5aR
system in human cancer invasion. However, C5a-C5aR-mediated cancer
invasion has not been fully elucidated in cancer patients. Cervical
carcinoma cells at stage I invade into the deeper tissues of the
uterus, whereas cells at CIN3 remain in the epithelium (19). To investigate the relationship between
cancer cell C5aR expression and invasion in cancer patients,
cervical tissue samples diagnosed as CIN3 or squamous cell
carcinoma stage I were examined for C5aR expression of tumor cells
(Fig. 3). Twenty-one of 49 samples
tested were positive for C5aR (42.9%) (95% confidence interval:
29.0–56.8%). C5aR was expressed on the cell membrane of the cancer
cells (Fig. 3B). Noncancerous
epithelial cells did not express C5aR (Fig. 3D). To evaluate the C5aR expression of
cells at CIN3 or stage I, the tissue samples were further assessed
for high C5aR and low C5aR expression (representative images in
Fig. 3A and C, respectively). The
proportion of cells with high C5aR expression was 38% (10/23) in
stage I cells and 12% (3/26) in CIN3 cells, and it was
significantly higher (P=0.021) at stage I than at CIN3 (Table I). The cells of the three CIN3 samples
belonging to the high C5aR expression group were all carcinoma
in situ (CIS). The association of high C5aR expression with
human cervical cancer invasion suggests that the C5a-C5aR system
has an invasion-enhancing effect on cervical cancer.
 | Table I.Association between C5a receptor
expression and invasion in uterus cervical cancer. |
Table I.
Association between C5a receptor
expression and invasion in uterus cervical cancer.
|
| C5aR
expression |
|
|---|
|
|
|
|
|---|
| Lesion | Low | High | P-value |
|---|
| CIN3 | 23 | 3 | 0.021 |
| Stage I | 13 | 10 |
|
Discussion
The Arthus reaction is caused by the immune
complex-triggered complement activation (24,25) and
serves as a model of autoimmune diseases, in which excessive
activation of the complement has been implicated (1,32).
Autoimmune-diseased organs and tissues have a high risk of cancer
development (33,34); hence, it is possible that the Arthus
reaction occurs in cancer tissues. We showed that the Arthus
reaction enhanced cancer invasion and growth in a C5aR-dependent
manner and induced recruitment of MDSCs at the site (Fig. 1). Thus, the endogenous C5a in the
reaction site acted on both cancer cells and the cancer
microenvironment, synergistically promoting cancer. The cancer
promotion by the Arthus reaction suggests that C5a generation may
be an underlying mechanism for the poor prognosis of the cancer
patients with autoimmune diseases (2–4),
particularly patients with C5aR-positive cancers. The promotion of
lung nodule formation of intravenously injected C5aR-positive
cancer cells (Fig. 2) provides
additional evidence of the tumor growth enhancement via the
C5a-C5aR system. The significantly high proportion of cells with
high C5aR expression at the early cervical cancer invasion stage in
comparison with the non-invasive stage (Table I) clinically supports the association
of the C5a-C5aR system with cancer invasion.
The C5aR-dependent enhancement of Renca cell
invasion in the wild-type mouse skin (Fig. 1A and B) corresponded with the
invasion-enhancing effect of recombinant mouse C5a on Renca/C5aR
cells (26) and HuCCT1/C5aR cells
in vitro and in nude mouse skin (12). However, contradictory results have
been reported regarding the effect of C5a on in vitro
proliferation of cancer cells. C5a enhanced the proliferation of
human breast (17,35) and nasopharyngeal (36) cancer cells, but not that of mouse lung
cancer cells (9), in a C5aR-dependent
manner. In the current study, we found that the Arthus reaction
augmented cancer cell growth in a C5aR-dependent fashion (Fig. 1D). The enhanced nodule formation of
cancer cells in the mouse lung (Fig.
2C) indicated the growth-enhancing activity of C5a in
C5aR-positive cancer cells. The C5aR-positive human cancer cells,
once stimulated with C5a and washed, maintained their enhanced
invasiveness (12); accordingly, C5a
stimulation was presumably able to enhance the growth of
C5aR-positive cancer cells in the lungs. The growth-enhancing
activity of the C5a-C5aR system in Renca/C5aR cells in the Arthus
reaction site (Fig. 1C and D) may
have been increased by accumulated MDSCs (Fig. 1E and F), which suppress the anticancer
immune response of CD8+ cytotoxic T cells and create a
microenvironment favorable for cancer cells (8).
Examination of clinically obtained cancer tissue
samples for cancer cell C5aR expression implicated the C5a-C5aR
system in human cancer progression. Cancer cell C5aR expression
correlated with advanced clinical stage (17,20,21),
presence of lymph node metastasis (16,17), and
low survival rate (16,21). However, no clinical evidence has
indicated a relationship between the C5a-C5aR system and cancer
invasion. Cervical cancer cells at stage I invade to the deeper
uterine tissues, whereas cells at CIN3 remain in the epithelial
layer (28). Thus, cervical cancer
cell invasion from the epithelial layer advances from CIN3 to stage
I. A significantly higher proportion of cells with high C5aR
expression at stage I compared to cells at CIN3 (Table I) might be the first evidence of an
association between the C5a-C5aR system and human cancer
invasion.
Plasma C5a levels are elevated in patients with
systemic lupus erythematosus (22)
and rheumatoid arthritis (23). The
cancer promotion by the Arthus reaction observed in this study
suggests that acceleration of cancer progression may occur via
elevated C5a level in patients with an autoimmune disease. Recent
studies have revealed an association between autoimmunity,
including rheumatoid arthritis and thyroiditis, and worse survival
in patients with lung, breast, or thyroid cancers (2–4); this
likely substantiates a close link of the C5a-C5aR system to cancer
aggravation in patients with autoimmune diseases. The cancer cell
C5aR-positive rates were different in the primary organs (12); accordingly, in C5aR-positive cancers,
the contribution of the C5a-C5aR system to poor prognosis of cancer
patients with autoimmune diseases presumably increases. Therefore,
blocking this system might be a useful therapeutic approach for
cancers, particularly in patients with autoimmune diseases.
Improved survival of metastatic renal cell carcinoma patients with
genetic deficiency of complement C4 (37), which blocks complement activation by
immune complexes and results in absence of C5a generation, further
supports the effectiveness of this treatment approach and is
consistent with the present results that showed cancer promotion
via the C5a-C5aR system. It has been reported that C5a signaling
inhibition by an L-aptamer reduced cancer growth and metastasis and
prolonged the survival of cancer-burdened mice, with a synergistic
effect by a combination with the blockade of programmed cell death
1 (PD-1) (38). Collectively, the
C5a-C5aR system may be a promising target for cancer therapy.
Furthermore, the association of C5aR expression with poor outcomes
in patients with diverse types of cancer (16–21)
suggests availability of such a therapy for a broad range of
cancers.
Acknowledgements
The authors would like to thank Ms. Tatsuko Kubo
(Department of Molecular Pathology, Kumamoto University, Kumamoto,
Japan), and Ms. Honami Miyahara, Ms. Yuri Nakamura, Ms. Mayuko
Ueda, Ms. Miharu Ohtsuki, and Ms. Eimi Onizuka (Shokei University,
Kumamoto, Japan) for technical assistance.
Funding
The present study was supported in part by Japan
Society for the Promotion of Science KAKENHI (grant nos. 25460498
and 16K08741) to Takahisa Imamura, (grant no. 17K11879) to Hidenao
Ogi and (grant no. 17K11912) to Takuya Tanaka.
Availability of data and materials
The data of the present study are available from the
corresponding author on reasonable request.
Authors' contributions
MY wrote the initial manuscript. MY, RI, HNi and KT
performed animal experiments, and KK performed statistical analysis
of data. FS and HK contributed to tissue sample collection. TT and
HO contributed to acquisition and interpretation of animal
experiment data and obtained financial support. TI and HNa made
substantial contributions to the conception, design and
intellectual content of this study. TI performed
immunohistochemistry and revised the manuscript. All the authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The animal experiments were approved by the Kumamoto
University Animal Experiment Committee (A 29–29) and performed
according to the criteria of the Committee. Written informed
consent for the tissue usage was obtained from the patients, and
the use of these tissues was approved by the internal ethics
committee (Rinri No. 706).
Patient consent for publication
Informed consent for publication was obtained from
the patients.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
C5aR
|
C5a receptor
|
|
CIN
|
cervical intraepithelial neoplasia
|
|
MDSC
|
myeloid-derived suppressor cell
|
References
|
1
|
Hellewell PG and Rossi AG: Arthus
reaction. In: Encyclopedia of immunology. 2nd. Delves PJ and Roitt
IM: Elsevier Academic Press; Amsterdam (Netherlands): pp. 237–240.
1998
|
|
2
|
Pak JK, Yang JA, Ahn EY, Chang SH, Song
YW, Curtis JR and Lee EB: Survival rate of cancer patients with and
without rheumatic disease: A retrospective cohort analysis. BMC
Cancer. 16:3812016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Criscitiello C, Bangnardi V, Esposito A,
Gelao L, Santillo B, Viale G, Rotmensz N, Goldhirsch A and
Curigliano G: Impact of autoimmune diseases on outcome of patients
with early breast cancer. Oncotarget. 7:51184–51192. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Souza SL, Montalli Da Assumpção LV and
Ward LS: Impact of previous thyroid autoimmune diseases on
prognosis of patients with well-differentiated thyroid cancer.
Thyroid. 13:491–495. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fernandez HN and Hugli TE: Primary
structural analysis of the polypeptide portion of human C5a
anaphylatoxin. Polypeptide sequence determination and assignment of
the oligosaccharide attachment site in C5a. J Biol Chem.
253:6955–6964. 1978.PubMed/NCBI
|
|
6
|
Guo RF and Ward PA: Role of C5a in
inflammatory responses. Annu Rev Immunol. 23:821–852. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Markiewski MM and Lambris JD: The role of
complement in inflammatory diseases from behind the scenes into the
spotlight. Am J Pathol. 171:715–727. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Markiewski MM, DeAngelis RA, Benencia F,
Ricklin-Lichtsteiner SK, Koutoulaki A, Gerard C, Coukos G and
Lambris JD: Modulation of the antitumor immune response by
complement. Nat Immunol. 9:1225–1235. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Corrales L, Ajona D, Rafail S, Lasarte JJ,
Riezu-Boj JI, Lambris JD, Rouzaut A, Pajares MJ, Montuenga LM and
Pio R: Anaphylatoxin C5a creates a favorable microenvironment for
lung cancer progression. J Immunol. 189:4674–4683. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nozaki M, Raisler BJ, Sakurai E, Sarma JV,
Barnum SR, Lambris JD, Chen Y, Zhang K, Ambati BK, Baffi JZ and
Ambati J: Drusen complement components C3a and C5a promote
choroidal neovascularization. Proc Natl Acad Sci USA.
103:2328–2333. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gerard NP and Gerard C: The chemotactic
receptor for human C5a anaphylatoxin. Nature. 349:614–617. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nitta H, Wada Y, Kawano Y, Murakami Y,
Irie A, Taniguchi K, Kikuchi K, Yamada G, Suzuki K, Honda J, et al:
Enhancement of human cancer cell motility and invasiveness by
anaphylatoxin C5a via aberrantly expressed C5a receptor (CD88).
Clin Cancer Res. 19:2004–2013. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Niculescu F, Rus HG, Retegan M and Vlaicu
R: Persistent complement activation on tumor cells in breast
cancer. Am J Pathol. 140:1039–1043. 1992.PubMed/NCBI
|
|
14
|
Bjørge L, Hakulinen J, Vintermyr OK, Jarva
H, Jensen TS, Iversen OE and Meri S: Ascitic complement system in
ovarian cancer. Br J Cancer. 92:895–905. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nitta H, Murakami Y, Wada Y, Eto M, Baba H
and Imamura T: Cancer cells release anaphylatoxin C5a from C5 by
serine protease to enhance invasiveness. Oncol Rep. 32:1715–1719.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gu J, Ding JY, Lu CL, Lin ZW, Chu YW, Zhao
GY, Guo J and Ge D: Overexpression of CD88 predicts poor prognosis
in non-small cell lung cancer. Lung Cancer. 81:259–265. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Imamura T, Yamamoto-Ibusuki M, Sueta A,
Kubo T, Irie A, Kikuchi K, Kariu T and Iwase H: Influence of the
C5a-C5a receptor system on breast cancer progression and patient
prognosis. Breast Cancer. 23:876–885. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wada Y, Maeda Y, Kubo T, Kikuchi K, Eto M
and Imamura T: C5a receptor expression is associated with poor
prognosis in urothelial cell carcinoma patients treated with
radical cystectomy or nephroureterectomy. Oncol Lett. 12:3995–4000.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xi W, Liu L, Wang J, Xia Y, Bai Q, Xiong
Y, Qu Y, Long Q, Xu J and Guo J: Enrichment of C5a-C5aR axis
predicts poor postoperative prognosis of patients with clear cell
renal cell carcinoma. Oncotarget. 7:80925–80934. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kaida T, Nitta H, Kitano Y, Yamamura K,
Arima K, Izumi D, Higashi T, Kurashige J, Imai K, Hayashi H, et al:
C5a receptor (CD88) promotes motility and invasiveness of gastric
cancer by activating RhoA. Oncotarget. 7:84798–84809. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nitta H, Shimose T, Emi Y, Imamura T,
Ohnishi K, Kusumoto T, Yamamoto M, Fukuzawa K, Takahashi I, Higashi
H, et al: Expression of the anaphylatoxin C5a receptor in gastric
cancer: Implications for vascular invasion and patient outcomes.
Med Oncol. 33:1182016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sakuma Y, Nagai T, Yoshio T and Hirohata
S: Differential activation mechanisms of serum C5a in lupus
nephritis and neuropsychiatric systemic lupus erythematosus. Mod
Rheumatol. 27:292–297. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hornum L, Hansen AJ, Tornehave D, Fjording
MS, Colmenero P, Wätjen IF, Søe Nielsen NH, Bliddal H and Bartels
EM: C5a and C5aR are elevated in joints of rheumatoid and psoriatic
arthritis patients, and C5aR blockade attenuates leukocyte
migration to synovial fluid. PLoS One. 12:e01890172017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cream JJ, Bryceson AD and Ryder G:
Disappearance of immunoglobulin and complement from the Arthus
reaction and its relevance to studies of vasculitis in man. Br J
Dermatol. 84:106–109. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ramos BF, Zhan Y and Jakschik BA:
Neutrophil elicitation in the reverse passive Arthus reaction.
Complement-dependent and -independent mast cell involvement. J
Immunol. 152:1380–1384. 1994.PubMed/NCBI
|
|
26
|
Maeda Y, Kawano Y, Wada Y, Yatsuda J,
Motoshima T, Murakami Y, Kikuchi K, Imamura T and Eto M: C5aR is
frequently expressed in metastatic renal cell carcinoma and plays a
crucial role in cell invasion via the ERK and PI3 kinase pathways.
Oncol Rep. 33:1844–1850. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shojaei F, Wu X, Malik AK, Zhong C,
Baldwin ME, Schanz S, Fuh G, Gerber HP and Ferrara N: Tumor
refractoriness to anti-VEGF treatment is mediated by
CD11b+Gr1+ myeloid cells. Nat Biotechnol.
25:911–920. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
FIGO Committee on Gynecologic Oncology:
FIGO staging for carcinoma of the vulva, cervix, and corpus uteri.
Int J Gynecol Obstet. 125:97–98. 2014. View Article : Google Scholar
|
|
29
|
Koomägi R and Volm M: Expression of Fas
(CD95/APO-1) and Fas ligand in lung cancer, its prognostic and
predictive relevance. Int J Cancer. 84:239–243. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Rahman MA, Dhar DK, Yamaguchi E, Maruyama
S, Sato T, Hayashi H, Ono T, Yamanoi A, Kohno H and Nagasue N:
Coexpression of inducible nitric oxide synthase and COX-2 in
hepatocellular carcinoma and surrounding liver: Possible
involvement of COX-2 in the angiogenesis of hepatitis C
virus-positive case. Clin Cancer Res. 7:1325–1332. 2001.PubMed/NCBI
|
|
31
|
Shvarts O, Janzen N, Lam JS, Leppert JT,
Caliliw R, Figlin RA, Belldegrum AS and Zeng G: RENCA/carbonic
anhydrase-IX: A murine model of a carbonic anhydrase-IX-expressing
renal cell carcinoma. Urology. 68:1132–1138. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Vignesh P, Rawat A, Sharma M and Singh S:
Complement in autoimmune diseases. Clin Chim Acta. 465:123–130.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Landgren AM, Landgren O, Gridley G, Dores
GM, Linet MS and Morton LM: Autoimmune disease and subsequent risk
of developing alimentary tract cancers among 4.5 million US male
veterans. Cancer. 117:1163–1171. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yu KH, Kuo CF, Huang LH, Huang WK and See
LC: Cancer risk in patients with inflammatory systemic autoimmune
Rheumatic diseases. A nationwide population-based dynamic cohort
study in Taiwan. Medicine (Baltimore). 95:e35402016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lu Y and Hu XB: C5a stimulates the
proliferation of breast cancer cells via Akt-dependent RGC-32 gene
activation. Oncol Rep. 32:2817–2823. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Cai K, Wang Y, Wang Z, Wang Y, Zhao X and
Bao X: C5a promotes the proliferation of human nasopharyngeal
carcinoma cells through PCAF-mediated STAT3 acetylation. Oncol Rep.
32:2260–2266. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zafar GI, Grimm EA, Wei W, Johnson MM and
Ellerhorst JA: Genetic deficiency of complement isoforms C4A or C4B
predicts improved survival of metastatic renal cell carcinoma. J
Urol. 181:1028–1034. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ajona D, Ortiz-Espinosa S, Moreno H,
Lozano T, Pajares MJ, Agorreta J, Bértolo C, Lasarte JJ, Vicent S,
Hoehlig K, et al: A combined PD-1/C5a blockade synergistically
protects against cancer growth and metastasis. Cancer Discov.
7:694–703. 2017. View Article : Google Scholar : PubMed/NCBI
|