|
1
|
Libby P, Bornfeldt KE and Tall AR:
Atherosclerosis: Successes, surprises, and future challenges. Circ
Res. 118:531–534. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chistiakov DA, Kashirskikh DA, Khotina VA,
Grechko AV and Orekhov AN: Immune-inflammatory responses in
atherosclerosis: The role of myeloid cells. J Clin Med. 8:17982019.
View Article : Google Scholar
|
|
3
|
Hanna A and Frangogiannis NG: Inflammatory
cytokines and chemokines as therapeutic targets in heart failure.
Cardiovasc Drugs Ther. 34:849–863. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Taleb S: Inflammation in atherosclerosis.
Arch Cardiovasc Dis. 109:708–715. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Veluswamy P, Wacker M, Scherner M and
Wippermann J: Delicate role of PD-L1/PD-1 axis in blood vessel
inflammatory diseases: Current insight and future significance. Int
J Mol Sci. 21:81592020. View Article : Google Scholar
|
|
6
|
Sethwala AM, Goh I and Amerena JV:
Combatting inflammation in cardiovascular disease. Heart Lung Circ.
30:197–206. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Koushki K, Shahbaz SK, Mashayekhi K,
Sadeghi M, Zayeri ZD, Taba MY, Banach M, Al-Rasadi K, Johnston TP
and Sahebkar A: Anti-inflammatory action of statins in
cardiovascular disease: The role of inflammasome and toll-like
receptor pathways. Clin Rev Allergy Immunol. May 6–2020.(Epub ahead
of print). doi: 10.1007/s12016-020-08791-9. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Luque-Martin R, Van den Bossche J, Furze
RC, Neele AE, van der Velden S, Gijbels MJJ, van Roomen CPPA,
Bernard SG, de Jonge WJ, Rioja I, et al: Targeting histone
deacetylases in myeloid cells inhibits their maturation and
inflammatory function with limited effects on atherosclerosis.
Front Pharmacol. 10:12422019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mog B, Asase C, Chaplin A, Gao H,
Rajagopalan S and Maiseyeu A: Nano-antagonist alleviates
inflammation and allows for MRI of atherosclerosis.
Nanotheranostics. 3:342–355. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang G, Zhuo J, Lin Y, Zhang M, Liu L,
Chen X and Gao R: Ginsenoside Rb1 prevents dysfunction of
endothelial cells by suppressing inflammatory response and
apoptosis in the high-fat diet plus balloon catheter-injured rabbit
model via the G protein-coupled estrogen receptor-mediated
phosphatidylinositol 3-kinases (PI3K)/akt pathway. Med Sci Monit.
25:7407–7417. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
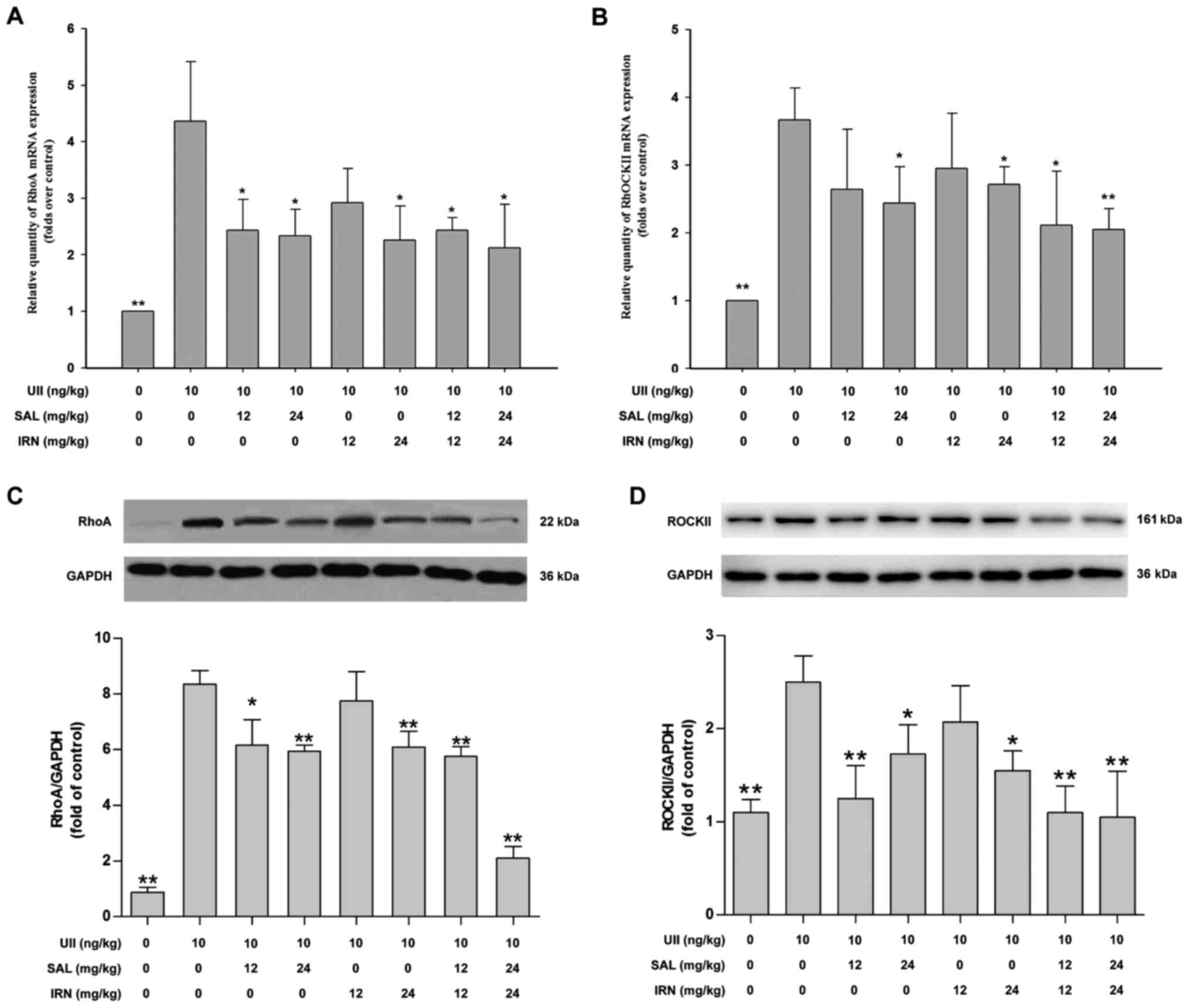
11
|
Cai A, Li L and Zhou Y: Pathophysiological
effects of RhoA and Rho-associated kinase on cardiovascular system.
J Hypertens. 34:3–10. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Deng Z, Jia Y, Liu H, He M, Yang Y, Xiao W
and Li Y: RhoA/ROCK pathway: Implication in osteoarthritis and
therapeutic targets. Am J Transl Res. 11:5324–5331. 2019.PubMed/NCBI
|
|
13
|
Strzelecka-Kiliszek A, Mebarek S,
Roszkowska M, Buchet R, Magne D and Pikula S: Functions of Rho
family of small GTPases and Rho-associated coiled-coil kinases in
bone cells during differentiation and mineralization. Biochim
Biophys Acta Gen Subj. 1861:1009–1023. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li N, Chen J, Zhao J and Wang T:
MicroRNA-3188 targets ETS-domain protein 4 and participates in
RhoA/ROCK pathway to regulate the development of atherosclerosis.
Pharmazie. 72:687–693. 2017.PubMed/NCBI
|
|
15
|
Surma M, Wei L and Shi J: Rho kinase as a
therapeutic target in cardiovascular disease. Future Cardiol.
7:657–671. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhou Q, Gensch C and Liao JK:
Rho-associated coiled-coil-forming kinases (ROCKs): Potential
targets for the treatment of atherosclerosis and vascular disease.
Trends Pharmacol Sci. 32:167–173. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cheng CI, Chen PH, Lin YC and Kao YH: High
glucose activates Raw264.7 macrophages through RhoA kinase-mediated
signaling pathway. Cell Signal. 27:283–292. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Loirand G, Guerin P and Pacaud P: Rho
kinases in cardiovascular physiology and pathophysiology. Circ Res.
98:322–334. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shimada H and Rajagopalan LE: Rho-kinase
mediates lysophosphatidic acid-induced IL-8 and MCP-1 production
via p38 and JNK pathways in human endothelial cells. FEBS Lett.
584:2827–2832. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Desche P, Couderc LJ and Epardeau B:
Sjogren's syndrome and pulmonary lymphangiomyomatosis. Chest.
94:8981988. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
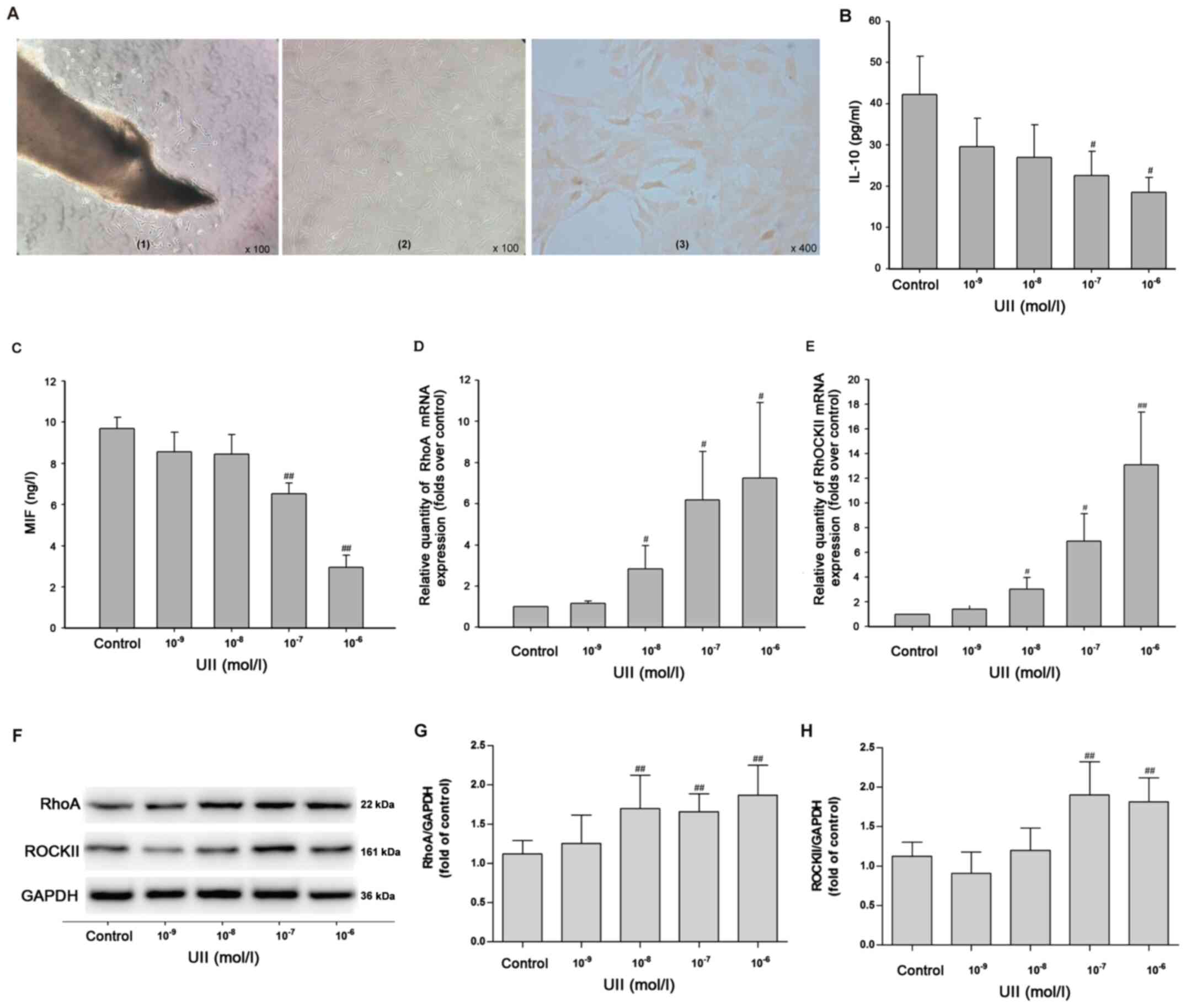
Douglas SA and Ohlstein EH: Human
urotensin-II, the most potent mammalian vasoconstrictor identified
to date, as a therapeutic target for the management of
cardiovascular disease. Trends Cardiovasc Med. 10:229–237. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Albanese I, Daskalopoulou SS, Yu B, You Z,
Genest J, Alsheikh-Ali A and Schwertani AG: The urotensin II system
and carotid atherosclerosis: A role in vascular calcification.
Front Pharmacol. 7:1492016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Demirpence M, Guler A, Yilmaz H, Sayin A,
Pekcevik Y, Turkon H, Colak A, Ari EM, Aslanipour B, Kocabas GU and
Calan M: Is elevated urotensin II level a predictor for increased
cardiovascular risk in subjects with acromegaly? J Endocrinol
Invest. 42:207–215. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Şatıroğlu Ö, Durakoğlugil ME, Çetin M,
Çiçek Y, Erdoğan T and Duman H: The role of urotensin II and
atherosclerotic risk factors in patients with slow coronary flow.
Interv Med Appl Sci. 8:158–163. 2016.PubMed/NCBI
|
|
25
|
Li Y, Zhao S, Wang Y, Chen Y, Lin Y, Zhu
N, Zheng H, Wu M, Cheng D, Li Y, et al: Urotensin II promotes
atherosclerosis in cholesterol-fed rabbits. PLoS One. 9:e950892014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lu D, Peng F, Li J, Zhao J, Ye X, Li B and
Ding W: Urotensin II promotes secretion of LTB4 through
5-lipoxygenase via the UT-ROS-Akt pathway in RAW264.7 macrophages.
Arch Med Sci. 15:1065–1072. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Xu S, Jiang H, Wu B, Yang J and Chen S:
Urotensin II induces migration of endothelial progenitor cells via
activation of the RhoA/Rho kinase pathway. Tohoku J Exp Med.
219:283–288. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Saito K, Yonekura-Sakakibara K,
Nakabayashi R, Higashi Y, Yamazaki M, Tohge T and Fernie AR: The
flavonoid biosynthetic pathway in arabidopsis: Structural and
genetic diversity. Plant Physiol Biochem. 72:21–34. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhong Z, Han J, Zhang J, Xiao Q, Hu J and
Chen L: Pharmacological activities, mechanisms of action, and
safety of salidroside in the central nervous system. Drug Des Devel
Ther. 12:1479–1489. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Boesch-Saadatmandi C, Loboda A, Wagner AE,
Stachurska A, Jozkowicz A, Dulak J, Döring F, Wolffram S and
Rimbach G: Effect of quercetin and its metabolites isorhamnetin and
quercetin-3-glucuronide on inflammatory gene expression: Role of
miR-155. J Nutr Biochem. 22:293–299. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lodi F, Jimenez R, Moreno L, Kroon PA,
Needs PW, Hughes DA, Santos-Buelga C, Gonzalez-Paramas A, Cogolludo
A, Lopez-Sepulveda R, et al: Glucuronidated and sulfated
metabolites of the flavonoid quercetin prevent endothelial
dysfunction but lack direct vasorelaxant effects in rat aorta.
Atherosclerosis. 204:34–39. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
National Research Council (US): Committee
for the Update of the Guide for the Care and Use of Laboratory
Animals: Guide for the Care and Use of Laboratory Animals. 8th
edition. National Academies Press; Washington, DC: 2011
|
|
33
|
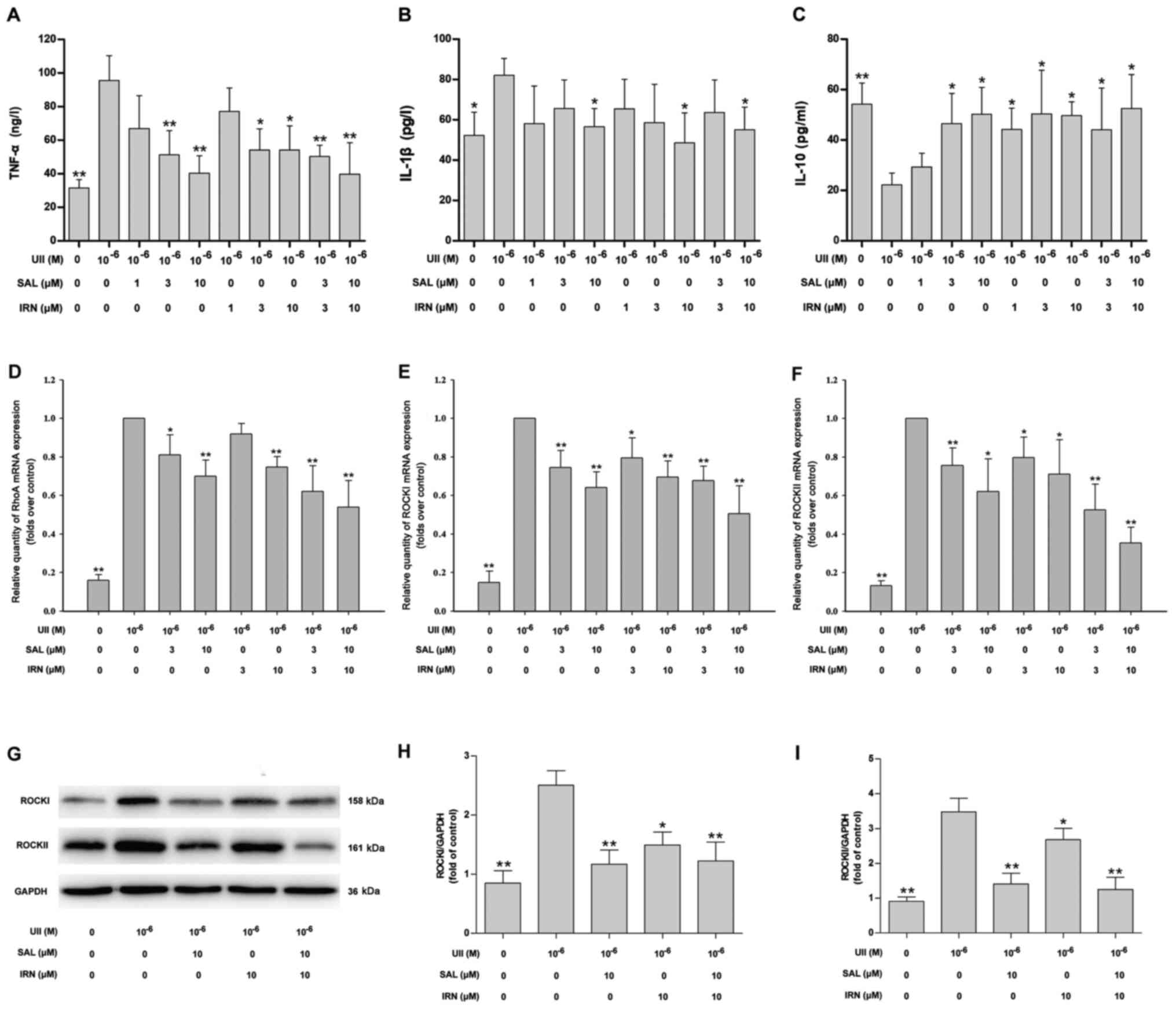
Chen L, Liu P, Feng X and Ma C:
Salidroside suppressing LPS-induced myocardial injury by inhibiting
ROS-mediated PI3K/Akt/mTOR pathway in vitro and in vivo. J Cell Mol
Med. 21:3178–3189. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jamali-Raeufy N, Baluchnejadmojarad T,
Roghani M, Keimasi S and Goudarzi M: Isorhamnetin exerts
neuroprotective effects in STZ-induced diabetic rats via
attenuation of oxidative stress, inflammation and apoptosis. J Chem
Neuroanat. 102:1017092019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhang N, Pei F, Wei H, Zhang T and Yang C,
Ma G and Yang C: Isorhamnetin protects rat ventricular myocytes
from ischemia and reperfusion injury. Exp Toxicol Pathol. 63:33–38.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hwang SM, Lee YJ, Lee YP, Yoon JJ, Lee SM,
Cha JD, Choi KM, Kang DG and Lee HS: Anti-proliferative effect of
an aqueous extract of prunella vulgaris in vascular smooth muscle
cells. Evid Based Complement Alternat Med. 2013:9364632013.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhou J, Yin G, Yu T, Zhang Y, Tian X, Xia
D and Shi L: Rosuvastatin reduces expression of tissue factor
through inhibiting RhoA/ROCK pathway to ameliorate atherosclerosis.
Panminerva Med. Sep 24–2019.(Epub ahead of print). doi:
10.23736/S0031-0808.19.03761-3.
|
|
39
|
Pereira-Castro J, Bras-Silva C and
Fontes-Sousa AP: Novel insights into the role of urotensin II in
cardiovascular disease. Drug Discov Today. 24:2170–2180. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yu QQ, Cheng DX, Xu LR, Li YK, Zheng XY,
Liu Y, Li YF, Liu HL, Bai L, Wang R, et al: Urotensin II and
urantide exert opposite effects on the cellular components of
atherosclerotic plaque in hypercholesterolemic rabbits. Acta
Pharmacol Sin. 41:546–553. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Tsai CS, Loh SH, Liu JC, Lin JW, Chen YL,
Chen CH and Cheng TH: Urotensin II-induced endothelin-1 expression
and cell proliferation via epidermal growth factor receptor
transactivation in rat aortic smooth muscle cells. Atherosclerosis.
206:86–94. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Diebold I, Petry A, Burger M, Hess J and
Görlach A: NOX4 mediates activation of FoxO3a and matrix
metalloproteinase-2 expression by urotensin-II. Mol Biol Cell.
22:4424–4434. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yang Y, Zhang J, Chen X, Wu T, Xu X, Cao
G, Li H and Li Y: UII/GPR14 is involved in NF-κB-mediated colonic
inflammation in vivo and in vitro. Oncol Rep. 36:2800–2806. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fiordelisi A, Iaccarino G, Morisco C,
Coscioni E and Sorriento D: NFkappaB is a key player in the
crosstalk between inflammation and cardiovascular diseases. Int J
Mol Sci. 20:15992019. View Article : Google Scholar
|
|
45
|
Li Q, Zhao W, Zeng X and Hao Z: Ursolic
acid attenuates atherosclerosis in apoE(−/-) mice: Role of LOX-1
mediated by ROS/NF-κB pathway. Molecules. 23:1101–1108. 2018.
View Article : Google Scholar
|
|
46
|
Zhang J, Wang X, Vikash V, Ye Q, Wu D, Liu
Y and Dong W: ROS and ROS-mediated cellular signaling. Oxid Med
Cell Longev. 2016:43509652016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bustelo XR, Sauzeau V and Berenjeno IM:
GTP-binding proteins of the Rho/Racfamily: Regulation, effectors
and functions in vivo. Bioessays. 29:356–370. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Tang ST, Zhang Q, Tang HQ, Wang CJ, Su H,
Zhou Q, Wei W, Zhu HQ and Wang Y: Effects of glucagon-like
peptide-1 on advanced glycation endproduct-induced aortic
endothelial dysfunction in streptozotocin-induced diabetic rats:
Possible roles of Rho kinase- and AMP kinase-mediated nuclear
factor κB signaling pathways. Endocrine. 53:107–116. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wang HW, Liu PY, Oyama N, Rikitake Y,
Kitamoto S, Gitlin J, Liao JK and Boisvert WA: Deficiency of ROCK1
in bone marrow-derived cells protects against atherosclerosis in
LDLR-/-mice. FASEB J. 22:3561–3570. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Li R, Dong Z, Zhuang X, Liu R, Yan F, Chen
Y, Gao X and Shi H: Salidroside prevents tumor necrosis
factor-α-induced vascular inflammation by blocking
mitogen-activated protein kinase and NF-κB signaling activation.
Exp Ther Med. 18:4137–4143. 2019.PubMed/NCBI
|
|
51
|
Xing SS, Li J, Chen L, Yang YF, He PL, Li
J and Yang J: Salidroside attenuates endothelial cellular
senescence via decreasing the expression of inflammatory cytokines
and increasing the expression of SIRT3. Mech Ageing Dev. 175:1–6.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Luo Y, Sun G, Dong X, Wang M, Qin M, Yu Y
and Sun X: Isorhamnetin attenuates atherosclerosis by inhibiting
macrophage apoptosis via PI3K/AKT activation and HO-1 induction.
PLoS One. 10:e1202592015.
|
|
53
|
Park C, Cha HJ, Choi EO, Lee H, Hwang-Bo
H, Ji SY, Kim MY, Kim SY, Hong SH, Cheong JH, et al: Isorhamnetin
induces cell cycle arrest and apoptosis via reactive oxygen
species-mediated AMP-activated protein kinase signaling pathway
activation in human bladder cancer cells. Cancers (Basel).
11:14942019. View Article : Google Scholar
|