|
1
|
Villa E, Baldini GM, Pasquinelli C,
Melegari M, Cariani E, Di Chirico G and Manenti F: Risk factors for
hepatocellular carcinoma in Italy. Male sex, hepatitis B virus,
non-A non-B infection, and alcohol. Cancer. 62:611–615. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhang X, El-Serag HB and Thrift AP: Sex
and race disparities in the incidence of hepatocellular carcinoma
in the United States examined through age-period-cohort analysis.
Cancer Epidemiol Biomarkers Prev. 29:88–94. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
McGlynn KA, Petrick JL and El-Serag HB:
Epidemiology of hepatocellular carcinoma. Hepatology. 73 (Suppl
1):S4–S13. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ma WL, Lai HC, Yeh S, Cai X and Chang C:
Androgen receptor roles in hepatocellular carcinoma, cirrhosis, and
hepatitis. Endocr Relat Cancer. 21:R165–R182. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li Y, Xu A, Jia S and Huang J: Recent
advances in the molecular mechanism of sex disparity in
hepatocellular carcinoma. Oncol Lett. 17:4222–4228. 2019.PubMed/NCBI
|
|
6
|
Villa E: Role of estrogen in liver cancer.
Womens Health (Lond). 4:41–50. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shi L, Feng Y, Lin H, Ma R and Cai X: Role
of estrogen in hepatocellular carcinoma: Is inflammation the key? J
Transl Med. 12:932014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Naugler WE, Sakurai T, Kim S, Maeda S, Kim
K, Elsharkawy AM and Karin M: Gender disparity in liver cancer due
to sex differences in MyD88-dependent IL-6 production. Science.
317:121–124. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
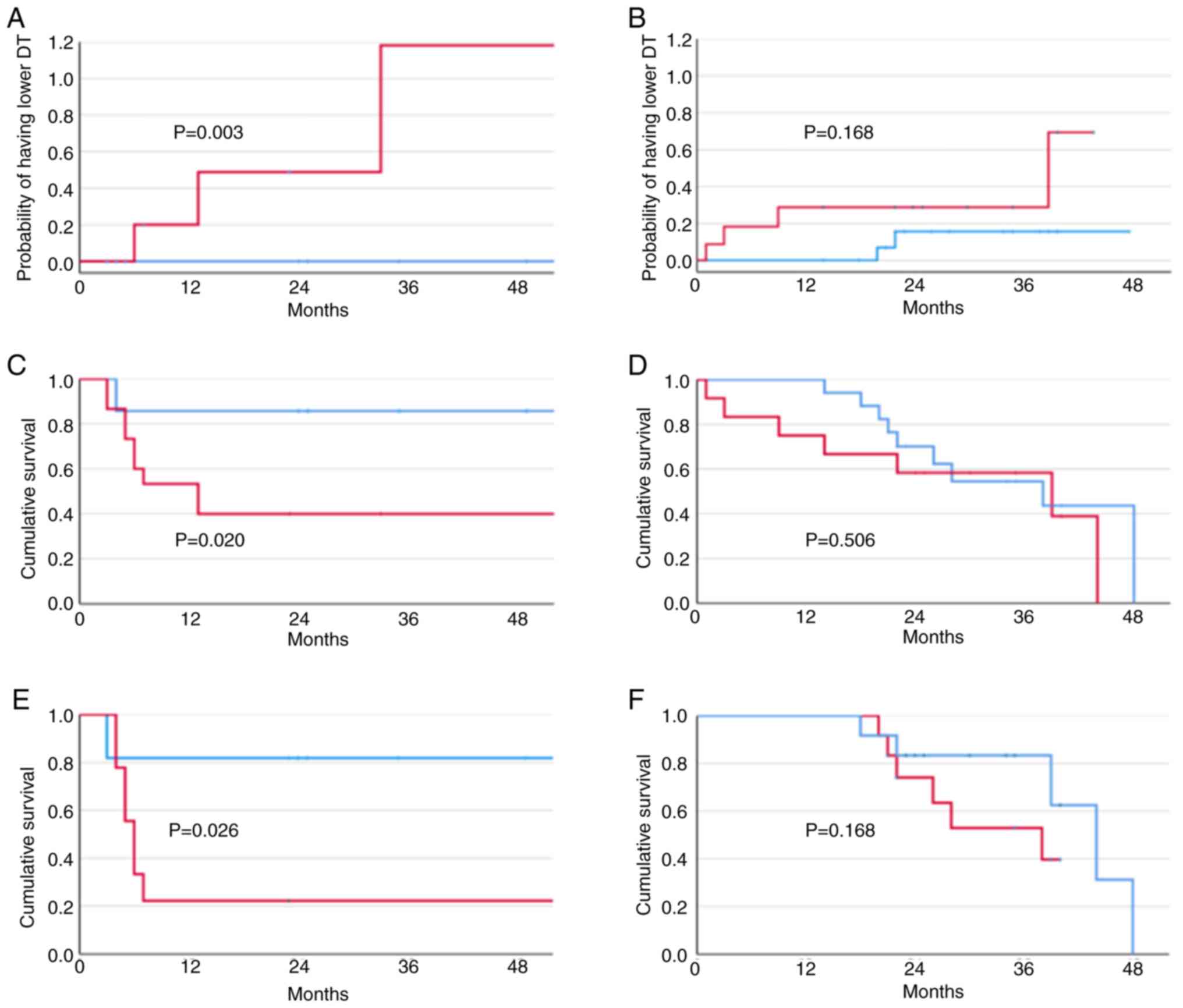
Villa E, Critelli R, Lei B, Marzocchi G,
Cammà C, Giannelli G, Pontisso P, Cabibbo G, Enea M, Colopi S, et
al: Neoangiogenesis-related genes are hallmarks of fast-growing
hepatocellular carcinomas and worst survival. Results from a
prospective study. Gut. 65:861–869. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Berglund JA, Voelker R, Barber P, Diegel
J, Mahady A and Bodner M: RNA regulation by estrogen. Oregon Univ
Eugene; 2011, View Article : Google Scholar
|
|
11
|
Li H, Han D, Hou Y, Chen H and Chen Z:
Statistical inference methods for two crossing survival curves: A
comparison of methods. PLoS One. 10:e01167742015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Martik ML and McClay DR: Deployment of a
retinal determination gene network drives directed cell migration
in the sea urchin embryo. Elife. 4:e088272015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu Y, Han N, Zhou S, Zhou R, Yuan X, Xu
H, Zhang C, Yin T and Wu K: The DACH/EYA/SIX gene network and its
role in tumor initiation and progression. Int J Cancer.
138:1067–1075. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Micalizzi DS, Christensen KL, Jedlicka P,
Coletta CD, Barón AE, Harrel JC, Horwitz KB, Billheimer D, Heichman
KA, Welm AL, et al: The Six1 homeoprotein induces human mammary
carcinoma cells to undergo epithelial-mesenchymal transition and
metastasis in mice through increasing TGF-beta signaling. J Clin
Invest. 119:2678–2690. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Micalizzi DS, Wang CA, Farabaugh SM,
Schiemann WP and Ford HL: Homeoprotein Six1 increases TGF-beta type
I receptor and converts TGF-beta signaling from suppressive to
supportive for tumor growth. Cancer Res. 70:10371–10380. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Min WP and Wei XF: Silencing SIX1 inhibits
epithelial mesenchymal transition through regulating TGF-β/Smad2/3
signaling pathway in papillary thyroid carcinoma. Auris Nasus
Larynx. 48:487–495. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu W, Gao M, Li L, Chen Y, Fan H, Cai Q,
Shi Y, Pan C, Liu J, Cheng L, et al: Homeoprotein SIX1 compromises
antitumor immunity through TGF-β-mediated regulation of collagens.
Cell Mol Immunol. 18:2660–2672. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Critelli R, Milosa F, Faillaci F, Condello
R, Turola E, Marzi L, Lei B, Dituri F, Andreani S, Sighinolfi P, et
al: Microenvironment inflammatory infiltrate drives growth speed
and outcome of hepatocellular carcinoma: A prospective clinical
study. Cell Death Dis. 8:e30172017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Christensen KL, Patrick AN, McCoy EL and
Ford HL: The six family of homeobox genes in development and
cancer. Adv Cancer Res. 101:93–126. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Behbakht K, Qamar L, Aldridge CS, Coletta
RD, Davidson SA, Thorburn A and Ford HL: Six1 overexpression in
ovarian carcinoma causes resistance to TRAIL-mediated apoptosis and
is associated with poor survival. Cancer Res. 67:3036–3042. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cheng Q, Ning D, Chen J, Li X, Chen XP and
Jiang L: SIX1 and DACH1 influence the proliferation and apoptosis
of hepatocellular carcinoma through regulating p53. Cancer Biol
Ther. 19:381–390. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ford HL, Kabingu EN, Bump EA, Mutter GL
and Pardee AB: Abrogation of the G2 cell cycle checkpoint
associated with overexpression of HSIX1: A possible mechanism of
breast carcinogenesis. Proc Natl Acad Sci USA. 95:12608–12613.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jin J, Jin T, Quan M, Piao Y and Lin Z:
Ezrin overexpression predicts the poor prognosis of gastric
adenocarcinoma. Diagn Pathol. 7:1352012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kahlert C, Lerbs T, Pecqueux M, Herpel E,
Hoffmeister M, Jansen L, Brenner H, Chang-Claude J, Bläker H, Kloor
M, et al: Overexpression of SIX1 is an independent prognostic
marker in stage I–III colorectal cancer. Int J Cancer.
137:2104–2113. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kong J, Zhou X, Liu S, Jin T, Piao Y, Liu
C and Lin Z: Overexpression of sineoculis homeobox homolog 1
predicts poor prognosis of hepatocellular carcinoma. Int J Clin Exp
Pathol. 7:3018–3027. 2014.PubMed/NCBI
|
|
27
|
Chen K, Wei H, Pan J, Chen Z, Pan D, Gao
T, Huang J, Huang M, Ou M and Zhong W: Six1 is negatively
correlated with poor prognosis and reduces 5-fluorouracil
sensitivity via attenuating the stemness of hepatocellular
carcinoma cells. Eur J Pharmacol. 861:1725992019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cui Q, Kong D, Li Z, Ahiable P, Wang K, Wu
K and Wu G: Dachshund 1 is differentially expressed between male
and female breast cancer: A matched case-control study of clinical
characteristics and prognosis. Clinical Breast Cancer.
18:e875–e882. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Suen AA, Jefferson WN, Wood CE,
Padilla-Banks E, Bae-Jump VL and Williams CJ: SIX1 oncoprotein as a
biomarker in a model of hormonal carcinogenesis and in human
endometrial cancer. Mol Cancer Res. 14:849–858. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jefferson WN, Padilla-Banks E, Phelps JY,
Gerrish KE and Williams CJ: Permanent oviduct posteriorization
after neonatal exposure to the phytoestrogen genistein. Environ
Health Perspect. 119:1575–1582. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jefferson WN, Chevalier DM, Phelps JY,
Cantor AM, Padilla-Banks E, Newbold RR, Archer TK, Kinyamu HK and
Williams CJ: Persistently altered epigenetic marks in the mouse
uterus after neonatal estrogen exposure. Mol Endocrinol.
27:1666–1677. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Rossini GP, Baldini GM, Villa E and
Manenti F: Characterization of estrogen receptor from human liver.
Gastroenterology. 96:1102–1109. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Villa E, Vukotic R, Cammà C, Petta S, Di
Leo A, Gitto S, Turola E, Karampatou A, Losi L, Bernabucci V, et
al: Reproductive status is associated with the severity of fibrosis
in women with hepatitis C. PLoS One. 7:e446242012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Meng F, Glaser SS, Francis H, DeMorrow S,
Han Y, Passarini JD, Stokes A, Cleary JP, Liu X, Venter J, et al:
Functional analysis of microRNAs in human hepatocellular cancer
stem cells. J Cell Mol Med. 16:160–173. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wang B, Hsu SH, Majumder S, Kutay H, Huang
W, Jacob ST and Ghoshal K: TGFbeta-mediated upregulation of hepatic
miR-181b promotes hepatocarcinogenesis by targeting TIMP3.
Oncogene. 29:1787–1797. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhou Q, Zheng X, Chen L, Xu B, Yang X,
Jiang J and Wu C: Smad2/3/4 pathway contributes to TGF-β-induced
MiRNA-181b expression to promote gastric cancer metastasis by
targeting Timp3. Cell Physiol Biochem. 39:453–466. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li B, Liu L, Li X and Wu L: miR-503
suppresses metastasis of hepatocellular carcinoma cell by targeting
PRMT1. Biochem Biophys Res Commun. 464:982–987. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Xiao Z, Shen J, Zhang L, Li M, Hu W and
Cho C: Therapeutic targeting of noncoding RNAs in hepatocellular
carcinoma: Recent progress and future prospects. Oncol Lett.
15:3395–3402. 2018.PubMed/NCBI
|
|
39
|
Xiao Y, Tian Q, He J, Huang M, Yang C and
Gong L: MiR-503 inhibits hepatocellular carcinoma cell growth via
inhibition of insulin-like growth factor 1 receptor. Onco Targets
Ther. 9:3535–3544. 2016.PubMed/NCBI
|
|
40
|
Yang X, Zang J, Pan X, Yin J, Xiang Q, Yu
J, Gan R and Lei X: miR-503 inhibits proliferation making human
hepatocellular carcinoma cells susceptible to 5-fluorouracil by
targeting EIF4E. Oncol Rep. 37:563–570. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Qiu G, Lin Y, Zhang H and Wu D: miR-139-5p
inhibits epithelial-mesenchymal transition, migration and invasion
of hepatocellular carcinoma cells by targeting ZEB1 and ZEB2.
Biochem Biophys Res Commun. 463:315–321. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Li J, Fang L, Yu W and Wang Y:
MicroRNA-125b suppresses the migration and invasion of
hepatocellular carcinoma cells by targeting transcriptional
coactivator with PDZ-binding motif. Oncol Lett. 9:1971–1975. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yang J, Li Z, Pang Y, Zhou T, Sun J, Cheng
XY and Zheng WV: MicroRNA-139-5p negatively regulates NME1
expression in hepatocellular carcinoma cells. Adv Clin Exp Med.
31:655–670. 2022. View Article : Google Scholar : PubMed/NCBI
|