Introduction
Lung cancer, characterized by increased morbidity
and mortality among malignant tumors, is predominantly represented
by non-small cell lung cancer (NSCLC), accounting for 85% of all
lung cancer cases. Among NSCLC subtypes, lung adenocarcinoma (LUAD)
has the highest incidence (1). The
tumor microenvironment (TME) plays an important role in
tumorigenesis, development and prognosis of lung cancer.
Neutrophils are an important component of the TME and affect the
growth, progression and prognosis of almost all solid tumors
(2).
Neutrophils account for 50–70% of the total
circulating leukocytes. Increasing evidence suggests that
tumor-associated neutrophils (TANs) are involved in the malignant
behavior of tumors, including recurrence and metastasis (3). TANs exhibit high functional
plasticity. A previous study revealed that TANs resemble the
two-sided phenotype of tumor-associated macrophages: the ‘N1’ type,
which inhibits tumor growth, and the ‘N2’ type, which promotes
tumor growth and malignant metastasis (4). Most studies have revealed a
significant association between TANs and poor prognosis in various
tumors, such as liver, head and neck, and kidney cancers; however,
higher TAN infiltration is significantly associated with longer
survival in gastric and colon cancer (5–9). CD177
is a surface protein unique to neutrophils with stable expression
and an adhesion molecule involved in the adhesion between
neutrophils and endothelial cells and the migration of neutrophils,
can represent neutrophils that exert activity in TME (10).
As the role of CD177+ neutrophils in LUAD
has not been previously elucidated, in the present study,
CD177+ neutrophils were detected in LUAD using
immunohistochemistry and their association with clinical
characteristics was analyzed. Additionally, the prognostic value in
the survival of patients with LUAD was evaluated.
Materials and methods
Reagent
The CD177+ polyclonal antibody was
purchased from Wuhan Boster Biological Technology, Ltd (cat. no.
PA5-83575).
Patients and clinical tissue
specimens
Between January 2021 and August 2021, at the
Department of Thoracic Surgery, tumor (T) and adjacent normal (DN)
tissues were collected from 16 patients with LUAD who underwent
curative surgery at Jining First People's Hospital (Jining, China).
These tissue samples were used for immunohistochemical analyses.
Moreover, 120 qualified formalin-fixed paraffin-embedded tissue
samples were obtained from patients with LUAD at the Department of
Pathology in Jining First People's Hospital (Jining, China) from
January 2013 to June 2017 and subjected to immunohistochemical
analysis. Tumor tissues were collected from LUADs pathologically
confirmed after thoracic surgery. The samples were obtained from
respiratory or oncology biopsies conducted via bronchoscopy or
percutaneous lung puncture. Notably, all patients included in the
present study had not undergone any prior antitumor therapy and had
no comorbidities related to other tumors, autoimmune diseases, or
infectious diseases. Therapeutic choices were made in accordance
with the prevailing yearly Chinese Society of Clinical Oncology
guidelines on the diagnosis and treatment of NSCLCs based on stage,
condition and family selection. All patients were followed-up over
telephone, outpatient follow-up, and case data review; the date of
diagnosis was marked as the starting time of follow-up.
Progression-free survival (PFS) was calculated from the date of
diagnosis to the date of tumor progression (in any aspect). Overall
survival (OS) was estimated from the date of diagnosis to the date
of death or last follow-up. The follow-up period was up to June
2022. The present study followed the principles of the Declaration
of Helsinki (2013) and was approved by the Ethics Committee of
Jining First People's Hospital (approval no. 2020-035). Written
informed consent was provided from all prospective patients for
participation in the study. The retrospective study was approved a
request to waive the documentation of informed consent.
Hematoxylin and eosin (H&E)
staining
Tissue sections (4-µm thick) were heated at 65°C for
30 min and were deparaffinized by conventional xylene, and
dehydrated with gradient alcohol. Further, the sections were
stained with hematoxylin for 3–5 min at room temperature and
washed. The sections were then reblued with rebluing solution for
45–60 sec at room temperature and washed, followed by which they
were immersed in 95% alcohol for 30–45 sec and stained with drops
of eosin staining solution for ~30 sec. The sections were then
dehydrated with gradient alcohol, made transparent with xylene and
sealed with neutral gum.
Immunohistochemistry
Tissue sections (4-µm thick) were heated at 65°C for
1 h and were deparaffinized by conventional xylene and dehydrated
with gradient alcohol. To facilitate antigen retrieval, the
sections were heated in sodium chloride/sodium citrate cleaning
solution at 95°C for 30 min. After achieving antigen retrieval, the
sections were treated with 3% H2O2 at 37°C
for 15 min to inactivate endogenous peroxidase. The sections were
rinsed with phosphate-buffered saline and incubated with
CD177+ polyclonal antibody diluted at 1:200 overnight at
4°C. After which the IHC-specific secondary antibody was added to
the tissue and incubated for 30 min. The sections were washed,
subjected to DAB color development, re-stained with hematoxylin,
re-blued with reblueing solution, and separated with a color
separation solution. The sections were then dehydrated with
gradient alcohol, made transparent with xylene and sealed with
neutral gum. Finally, the sections were viewed under light
microscope by two independent pathologists blinded to the patients'
clinical data. When each tissue section was reviewed, stromal and
epithelial cells were randomly selected from six representative
regions at ×400 magnification. Moreover, the number of
CD177+ neutrophils was analyzed, and the mean of the six
counts was calculated. The number of CD177+ neutrophils
in the tumor and paracancerous tissues was determined as the mean
number of positively stained cells per high-power microscopic field
[high-power field (HPF), ×400). The patients were divided into
high- and low-density groups according to the median number of
CD177+ neutrophils (11).
Statistical analysis
All data are expressed as the mean ± SEM and were
analyzed using SPSS V.22.0 (IBM Corp.). An unpaired two-tailed
Student's t test was performed for statistical comparisons, and a
chi-square test was used to evaluate the association between
CD177+ neutrophil density and the clinicopathological
characteristics of patients with LUAD. Based on the median density
(6 cells/HPF) of CD177+ neutrophils, patients with LUAD
were divided into the high-density group and low-density group, and
PFS and OS curves were plotted using the Kaplan-Meier method and
compared utilizing the log-rank test. Univariate and multivariate
COX risk regression analysis were employed to detect prognostic
factors. P<0.05 was considered to indicate a statistically
significant difference.
Results
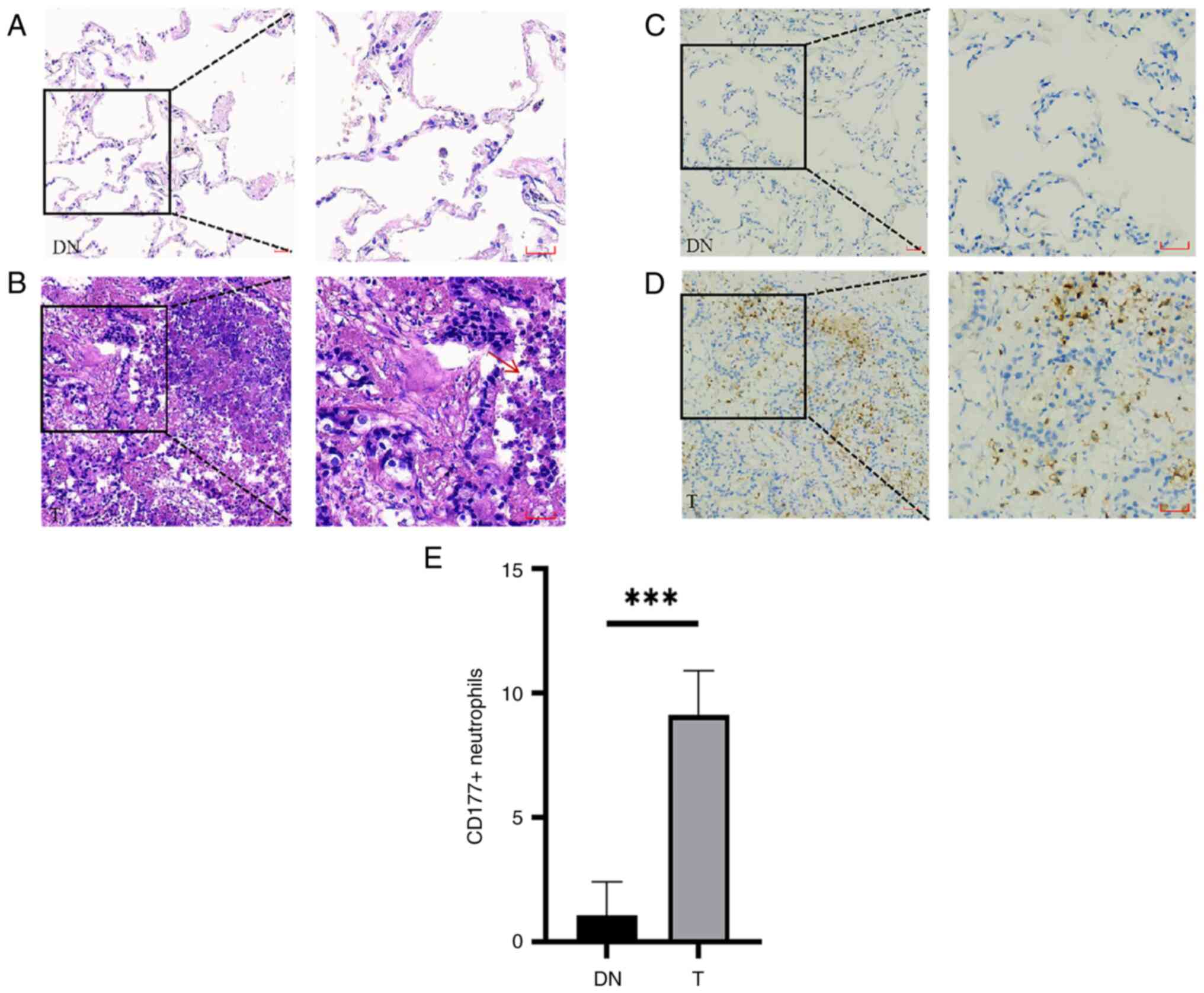
Increased infiltration of
CD177+ neutrophils in tumor tissues of LUAD
CD177+ neutrophils may signify active
neutrophils within the TME. The potential increase of the
infiltration of CD177+ neutrophil in the tumor tissues
of patients with LUAD was investigated. Neutrophils were detected
in tumor (T) tissues and adjacent normal (DN) tissues. It was
observed through H&E staining that neutrophils infiltrated
higher in ‘T’ compared with ‘DN’ of LUAD (Fig. 1A and B); then it was also observed
through immunohistochemistry that the CD177+ neutrophils
infiltrated higher in ‘T’ compared with ‘DN’ of LUAD (Fig. 1C-E).
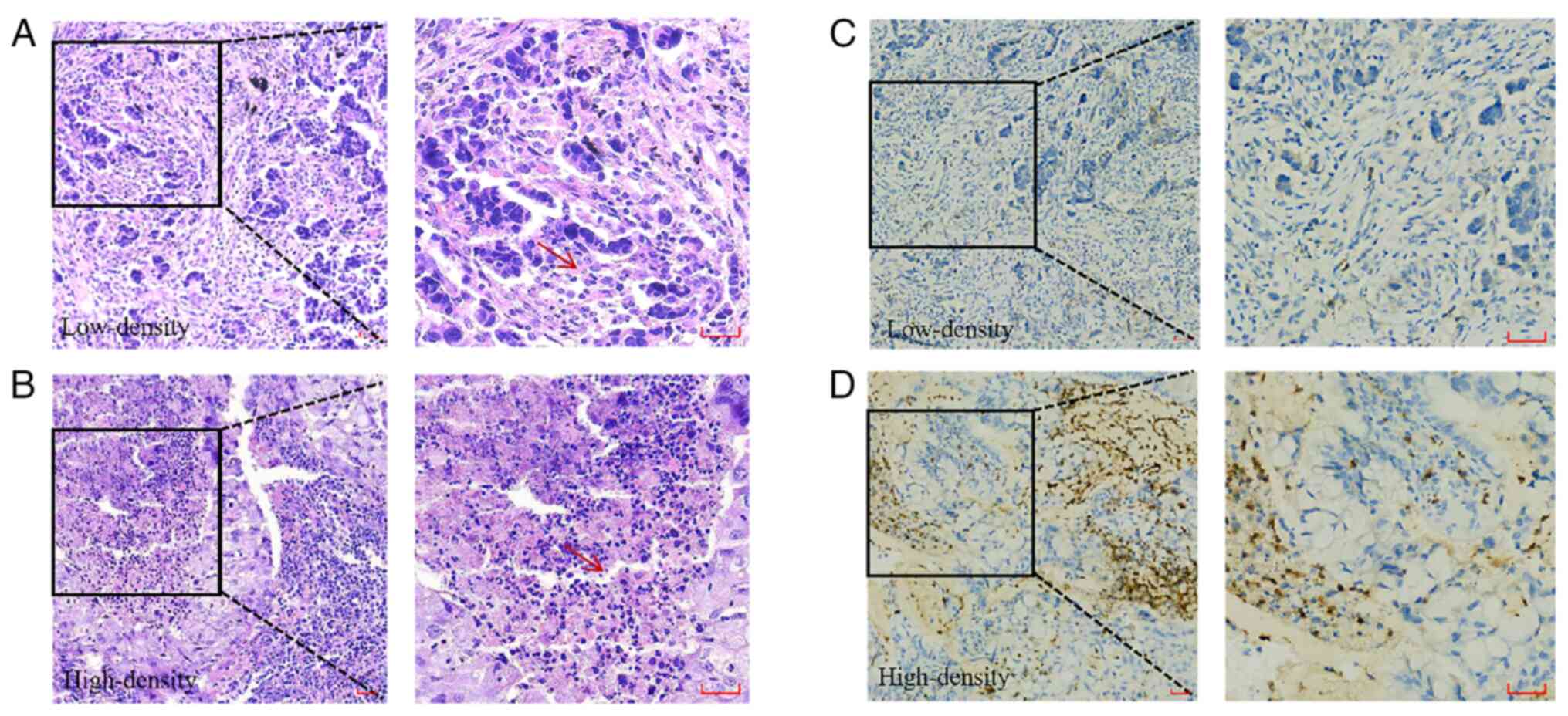
Association of CD177+
neutrophils with clinical characteristics of LUAD
To further examine whether CD177+
neutrophil infiltration is associated with the clinical
characteristics of LUAD, 120 paraffin-embedded LUAD tissue
specimens were collected and used for immunohistochemical analysis.
The clinical characteristics of the 120 LUAD patients (including
sex and age distribution) enrolled in the present study are
summarized in Table I. There was no
statistical difference in treatment regimen selection between the
two populations. Through H&E staining, the variations in
neutrophils infiltration among different patients with LUAD were
observed (Fig. 2A and B).
Additionally, immunohistochemistry revealed distinct patterns of
CD177+ neutrophil infiltration in different patients
with LUAD (Fig. 2C and D). Based on
the median density (6 cells/HPF) of CD177+ neutrophils,
120 patients with LUAD were divided into the high-density group (≥6
cells/HPF) and low-density group (<6 cells/HPF) (7). A significant association between the
density of CD177+ neutrophil infiltration, TNM stage and
tumor differentiation (P<0.05) was observed; however, no
significant association was observed between age, sex, tumor size,
smoking index, and lymph node metastasis (P>0.05) (Table II). These differences indicated
that increased CD177+ neutrophil infiltration in tumor
tissues was associated with the malignant progression of LUAD.
 | Table I.Clinical characteristics of patients
with lung adenocarcinoma. |
Table I.
Clinical characteristics of patients
with lung adenocarcinoma.
| Clinicopathological
characteristics (n=120) | N (%) |
|---|
| Age, years |
|
|
<60 | 58 (48.3) |
|
≥60 | 62 (51.7) |
| Sex |
|
|
Male | 59 (49.2) |
|
Female | 61 (50.8) |
| Smoking index |
|
| 0 | 72 (60.0) |
|
>0 | 48 (40.0) |
| TNM stage |
|
| I | 41 (34.2) |
| II | 27 (22.5) |
|
III | 27 (22.5) |
| IV | 25 (20.8) |
| T stage |
|
| T1 | 48 (40.0) |
| T2 | 45 (37.5) |
| T3 | 22 (18.3) |
| T4 | 5 (4.2) |
| Lymph node
metastasis |
|
|
Positive | 59 (50.0) |
|
Negative | 61 (50.0) |
|
Differentiation |
|
|
Poor | 36 (25.0) |
|
Moderate | 76 (37.5) |
|
Well | 8 (37.5) |
 | Table II.Association between CD177+
neutrophils and clinical characteristics of lung
adenocarcinoma. |
Table II.
Association between CD177+
neutrophils and clinical characteristics of lung
adenocarcinoma.
|
| Density of
CD177+ neutrophils |
|
|---|
|
|
|
|
|---|
| Clinicopathological
characteristics | High-density, n
(%) | Low-density, n
(%) | P-value |
|---|
| Age, years |
|
| 0.29 |
|
<60 | 29 (43.9) | 29 (53.7) |
|
|
≥60 | 37 (56.1) | 25 (46.3) |
|
| Sex |
|
| 0.1 |
|
Male | 37 (56.1) | 22 (40.7) |
|
|
Female | 29 (43.9) | 32 (59.3) |
|
| Smoking index |
|
| 0.55 |
| No | 38 (57.6) | 34 (63.0) |
|
|
Yes | 28 (42.4) | 20 (37.0) |
|
| TNM stage |
|
| 0.002 |
| I | 19 (28.8) | 22 (40.7) |
|
| II | 17 (25.8) | 10 (18.5) |
|
|
III | 22 (33.3) | 5 (9.3) |
|
| IV | 8 (12.1) | 17 (31.5) |
|
| T stage |
|
| 0.56 |
| T1 | 25 (37.9) | 23 (42.6) |
|
| T2 | 23 (34.8) | 22 (40.7) |
|
| T3 | 15 (22.7) | 7 (13.0) |
|
| T4 | 3 (4.5) | 2 (3.7) |
|
| Lymph node
metastasis |
|
| 0.57 |
|
Positive | 34 (51.5) | 25 (46.3) |
|
|
Negative | 32 (48.5) | 29 (53.7) |
|
|
Differentiation |
|
| 0.023 |
|
Poor | 23 (34.8) | 13 (24.1) |
|
|
Moderate | 42 (63.6) | 34 (63.0) |
|
|
Well | 1 (1.5) | 7 (13.0) |
|
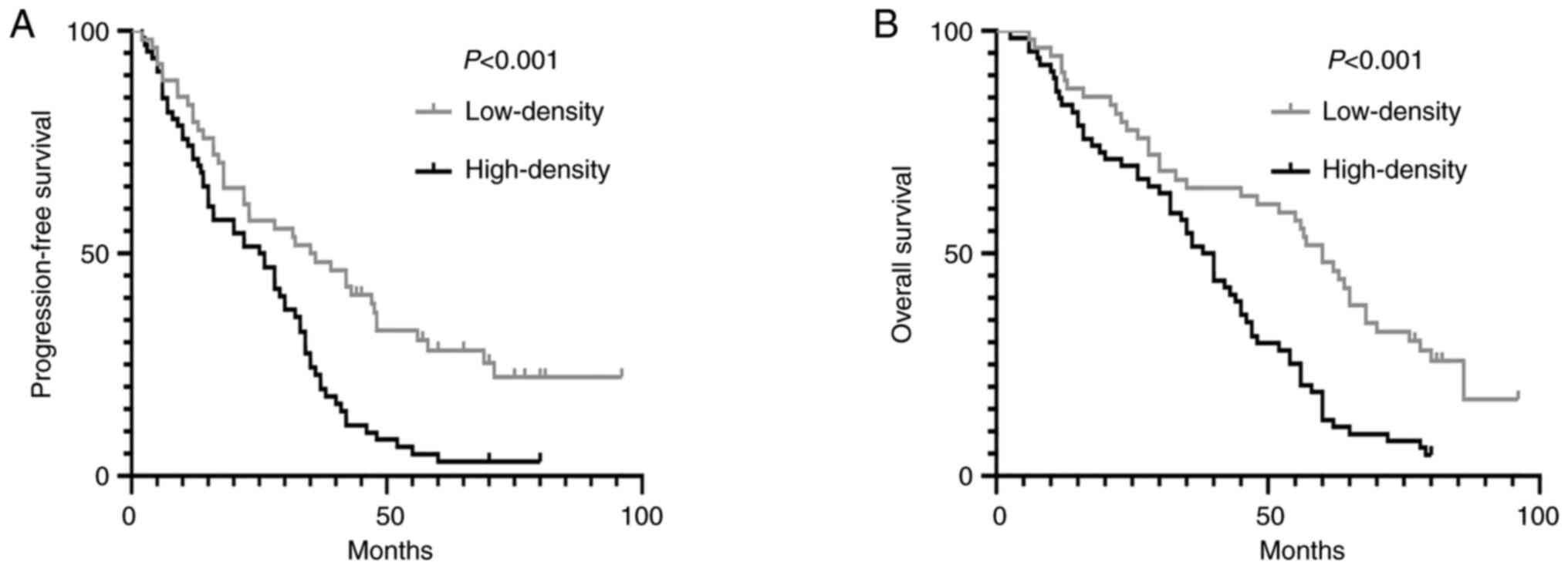
Association of CD177+
neutrophils with prognosis of LUAD
During a 96 months follow-up period (ranging from
2.5 to 96 months), the association between CD177+
neutrophil infiltration and PFS and OS of LUAD patients was further
examined using Kaplan-Meier survival curve analysis. It was
revealed that patients with high-density of CD177+
neutrophils had shorter PFS (25.48±2.18 months vs. 43.56±4.56
months) and OS (38.16±2.63 months vs. 55.65±4.09 months) than those
with low-density in LUAD (Fig. 3A and
B, respectively). These data indicated that a higher density of
CD177+ neutrophils was associated with poor PFS and OS
in patients with LUAD.
Univariate and multivariate analyses were performed
to assess whether CD177+ neutrophils served as
independent indicators of PFS and OS. Univariate analysis revealed
that the CD177+ neutrophils [PFS: Hazard Ratio (HR),
2.063; 95% CI, 1.367–3.113; P=0.001. OS: HR, 2.184; 95% CI,
1.446–3.298; P<0.001], TNM stage (PFS: HR, 3.269; 95% CI,
2.098–5.095; P<0.001. OS: HR, 3.290; 95% CI: 2.122–5.101;
P<0.001), lymph node metastasis (PFS: HR, 2.592; 95% CI:
1.723–3.901; P<0.001. OS: HR, 2.813; 95% CI, 1.878–4.212;
P=0.001) and poor tumor differentiation (PFS: HR, 6.779; 95% CI,
2.378–19.321; P<0.001. OS: HR, 6.732; 95% CI, 2.364–19.174;
P<0.001) were the major factors affecting the OS and PFS of LUAD
patients (Tables III and IV). Moreover, following adjustment for
all potential clinical factors that may influence PFS and OS
through multivariate Cox regression analyses, the density of
CD177+ neutrophils (PFS: HR, 1.759; 95% CI, 1.162–2.661;
P=0.008. OS: HR, 1.987; 95% CI, 1.304–3.026; P=0.001), TNM stage
(PFS: HR, 2.519; 95% CI, 1.525–4.162; P<0.001. OS: HR, 2.384;
95% CI, 1.461–3.891; P=0.001) and lymph node metastasis (PFS: HR,
1.691; 95% CI, 1.065–2.685; P=0.026. OS: HR, 2.054; 95% CI,
1.326–3.181; P=0.001) along with poor tumor differentiation (PFS:
HR, 3.620; 95% CI, 1.182–11.090; P=0.024. OS: HR, 3.602; 95% CI,
1.208–10.743; P=0.022) were independent indicators for predicting
the PFS and OS in LUAD patients (Tables III and IV).
 | Table III.Univariate and multivariate analyses
of progression-free survival in patients with lung
adenocarcinoma. |
Table III.
Univariate and multivariate analyses
of progression-free survival in patients with lung
adenocarcinoma.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factors | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Density of CD177+
neutrophils (high vs. low) | 2.063 | 1.367–3.113 | 0.001 | 1.759 | 1.162–2.661 | 0.008 |
| TNM stage (IIIB +
IV vs. I–IIIA) | 3.269 | 2.098–5.095 | <0.001 | 2.519 | 1.525–4.162 | <0.001 |
|
Differentiation |
|
|
|
|
|
|
|
Poor | 6.779 | 2.378–19.321 | <0.001 | 3.620 | 1.182–11.090 | 0.024 |
|
Moderate | 2.861 | 1.035–7.908 | 0.043 | 2.331 | 0.810–6.714 | 0.117 |
|
High | Ref. |
|
|
|
|
|
| Lymph node
metastasis (Positive vs. Negative) | 2.592 | 1.723–3.901 | <0.001 | 1.691 | 1.065–2.685 | 0.026 |
| Smoking index (Yes
vs. No) | 1.654 | 1.114–2.458 | 0.013 | 1.212 | 0.787–1.864 | 0.383 |
 | Table IV.Univariate and multivariate analyses
of overall survival in patients with lung adenocarcinoma. |
Table IV.
Univariate and multivariate analyses
of overall survival in patients with lung adenocarcinoma.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factors | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Density of
CD177+ neutrophils (high vs. low) | 2.184 | 1.446–3.298 | <0.001 | 1.987 | 1.304–3.026 | 0.001 |
| TNM stage (IIIB +
IV vs. I–IIIA) | 3.290 | 2.122–5.101 | <0.001 | 2.384 | 1.461–3.891 | 0.001 |
|
Differentiation |
|
|
|
|
|
|
|
Poor | 6.732 | 2.364–19.174 | <0.001 | 3.602 | 1.208–10.743 | 0.022 |
|
Moderate | 2.630 | 0.954–7.254 | 0.062 | 2.055 | 0.724–5.833 | 0.176 |
|
High | Ref. |
|
|
|
|
|
| Lymph node
metastasis (Positive vs. Negative) | 2.813 | 1.878–4.212 | <0.001 | 2.054 | 1.326–3.181 | 0.001 |
| Smoking index (Yes
vs. No) | 1.487 | 1.003–2.204 | 0.048 | 1.025 | 0.668–1.573 | 0.911 |
In summary, these data indicated that tumor
associated CD177+ neutrophils may be independent and
unfavorable prognostic biomarkers for LUAD.
Discussion
Lung cancer is a global health concern with the
highest rates of morbidity and mortality. Among its subtypes, LUAD
holds the highest proportion, significantly impacting human health
(12). Chronic inflammation is
closely related to lung cancer (13). Neutrophils are the most abundant
immune cells, serving as the organism's first line of defense
against infection and responding to various inflammatory signals,
even in cancer (14). In previous
years, the correlations between the neutrophil-to-lymphocyte ratio
(NLR) in the peripheral blood and the treatment effectiveness and
prognosis of malignant tumors have been extensively studied. Most
of the studies have found that a higher NLR is associated with
poorer survival and tumor recurrence (15–17);
therefore, concern is growing regarding neutrophil infiltration in
tumors.
In malignant tumors, an increase in neutrophils or
NLR usually leads to a systemic inflammatory reaction. This can
lead to a poor prognosis by inhibiting tumor cell apoptosis,
promoting angiogenesis, inducing DNA damage, and promoting tumor
cell proliferation and metastasis (18–20).
Studies identified NLR as a potential prognostic marker strongly
associated with outcomes and responsiveness to various treatments,
including anti-angiogenic therapy such as bevacizumab,
chemotherapy, radiotherapy and immunotherapy in patients with lung
cancer (21–25). However, limited studies have
investigated the relationship between TAN and the therapeutic
efficacy and prognosis of different lung cancer treatment
regimens.
TANs can be detected in most intratumoral stroma;
they play important roles in tumor progression, angiogenesis, cell
migration, extracellular matrix modification and immunosuppression,
and can also affect the growth and progression of almost all solid
tumors (26,27). In the present study, a higher
infiltration of CD177+ neutrophils in LUAD tumor tissues
was discovered. An association between the density of
CD177+ neutrophils and clinical characteristics of LUAD
was also revealed. CD177+ neutrophils were significantly
associated with the TNM stage and tumor differentiation, indicating
that CD177+ neutrophil infiltration in LUAD was
associated with malignant progression. During the collection of
cases from January 2013 to June 2017, immunotherapy had not been
implemented in China. Nevertheless, additional fresh lung tissues
for the detection of TAN using flow cytometry, western blotting, or
multiple immunofluorescence techniques can be acquired. Future
studies will delve into the association of tumor-associated
CD177+ neutrophil infiltration status with tumor immune
status, pathological phenotype, microvessel density, and LUAD locus
size to provide further insights into how TANs regulate the
TME.
The association between TANs and the prognosis of
lung cancer patients is debatable. Eruslanov et al (28) reported that TANs inhibit the
malignant progression of lung cancer. A previous study has reported
that CD66b+ neutrophils are an adverse prognostic factor
in NSCLC (29). Another study found
that high CD66b neutrophil density had a small effect on OS but was
correlated with the incidence of recurrence after surgical
resection in early stage (stage I–III) in patients with NSCLC
(30). Previous studies showed that
the expression of CD177+ can be used to represent the
infiltration of neutrophils. It was demonstrated that high
expression of CD177+ was associated with poor prognosis
in pancreatic ductal adenocarcinoma (28) and that CD177+ tumor
neutrophil infiltration was an adverse prognostic factor for
bevacizumab treatment in colorectal cancer (31). However, CD177+
neutrophils were highly expressed in gastric and colorectal
cancers. Furthermore, a high density of CD177+
neutrophils predicts a favorable prognosis in these patients and is
an independent prognostic factor for OS in gastric and colorectal
cancers, as indicated by multivariate analysis (8,11).
Therefore, the association between CD177+ neutrophils
and the overall prognosis of LUAD was further explored. The
analysis of the present study confirmed that patients with
high-density of CD177+ neutrophils had shorter PFS
(25.48±2.18 months vs. 43.56±4.56 months) and OS (38.16±2.63 months
vs. 55.65±4.09 months) than those with low-density in LUAD. The
preliminary experiment of the present study also identified that
the density of CD177+ neutrophils in lung squamous
carcinoma (LUSC) tumor tissues was significantly higher than that
in paracancerous tissues, and a large amount of neutrophil
infiltration was observed when focal necrosis was detected in LUSC.
However, Rakaee et al (32)
revealed an association between TAN infiltration in lung cancer and
patient survival; high intratumoral CD66b+ TANs density
in the LUSC subgroup was an independent positive prognostic factor
for disease-specific survival, whereas high intratumoral TANs
density was an independent negative prognostic factor in the LUAD
subgroup. Therefore, CD177+ neutrophils in LUSC can be
considered as a potential target for future studies.
The treatment plans collected included postoperative
sequential chemoradiotherapy, chemotherapy combined with or without
radiotherapy, and targeted therapy. It is not yet possible to
analyze the predictive effect of tumor-associated CD177+
neutrophil infiltration on the treatment course of a single
regimen. Additionally, immunotherapy had not yet been performed in
China during the period in which the cases were collected. In the
future, relevant research to determine whether tumor-associated
CD177+ neutrophil infiltration can predict the clinical
outcomes of surgery, chemotherapy, radiotherapy, or immunotherapy
will be conducted. Univariate and multivariate analyses revealed
that PFS and OS were significantly associated with
CD177+ neutrophils, TNM stage, lymph node metastasis and
tumor differentiation. These findings suggested that
tumor-associated CD177+ neutrophils may be independent
and unfavorable prognostic biomarkers for LUAD. Smoking can cause
chronic inflammation in the lungs and induce lung cancer, which is
a risk factor for poor prognosis of lung cancer (33,34).
To the best of the authors' knowledge, this is the first study
demonstrating the prognostic value of CD177+ neutrophil
infiltration in LUAD.
In conclusion, the present study revealed that
CD177+ neutrophils are functionally activated neutrophil
populations that infiltrate LUAD. Tumor-associated
CD177+ neutrophils are highly associated with malignant
progression and poor survival and may be used as an independent and
unfavorable prognostic biomarker of LUAD. Therefore,
tumor-associated CD177+ neutrophils may serve as novel
therapeutic targets for the treatment and prognosis of LUAD.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Shandong Medicine and
Health Project (grant no. 202003020509) and the Key R&D Program
of Jining (grant no. 2023YXNS243).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are not publicly available due to privacy or ethical
restrictions but are available from the corresponding author on
reasonable request.
Authors' contributions
JZ, SJ and WW contributed to conception and design
of the study. JM, CB and YW acquired and interpreted the data. QX
performed the experiments. JZ and HL performed the statistical
analysis. JZ wrote the first draft of the manuscript. SJ supervised
the project and provided funds for the whole project. JZ and SJ
confirm the authenticity of all the raw data. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study followed the principles of the
Declaration of Helsinki and was approved by the ethics committees
of Jining First People's Hospital (approval no. 2020-035; Jining,
China). Written informed consent was provided from all prospective
patients for participation in the study. The retrospective study
was approved a request to waive the documentation of informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
LUAD
|
lung adenocarcinoma
|
|
NSCLC
|
non-small cell lung cancer
|
|
TANs
|
tumor-associated neutrophils
|
|
TME
|
tumor microenvironment
|
|
OS
|
overall survival
|
|
PFS
|
progression-free survival
|
|
NLR
|
neutrophil-to-lymphocyte ratio
|
|
LUSC
|
lung squamous carcinoma
|
References
|
1
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Orozco-Morales M, Soca-Chafre G,
Bios-Bernal P, Hernández-Pedro N and Arrieta O: Interplay between
cellular and molecular inflammatory mediators in lung cancer.
Mediators Inflamm. 2016:34946082016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Masucci MT, Minopoli M and Carriero MV:
Tumor associated neutrophils. Their role in tumorigenesis,
metastasis, prognosis and therapy. Front Oncol. 9:11462019.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dumitru CA, Lang S and Brandau S:
Modulation of neutrophil granulocytes in the tumor
microenvironment: Mechanisms and consequences for tumor
progression. Semin Cancer Biol. 23:141–148. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim J and Bae JS: Tumor-Associated
macrophages and neutrophils in tumor microenvironment. Mediators
Inflamm. 2016:60581472016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kuang DM, Zhao Q, Wu Y, Peng C, Wang J, Xu
Z, Yin XY and Zheng L: Peritumoral neutrophils link inflammatory
response to disease progression by fostering angiogenesis in
hepatocellular carcinoma. J Hepatol. 54:948–955. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Galdiero MR, Bianchi P, Grizzi F, Di Caro
G, Basso G, Ponzetta A, Bonavita E, Barbagallo M, Tartari S,
Polentarutti N, et al: Occurrence and significance of
tumor-associated neutrophils in patients with colorectal cancer.
Int J Cancer. 139:446–456. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhou G, Peng K, Song Y, Yang W, Shu W, Yu
T, Yu L, Lin M, Wei Q, Chen C, et al: CD177+ neutrophils suppress
epithelial cell tumourigenesis in colitis-associated cancer and
predict good prognosis in colorectal cancer. Carcinogenesis.
39:272–282. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Toyoda T, Tsukamoto T, Yamamoto M, Ban H,
Saito N, Takasu S, Shi L, Saito A, Ito S, Yamamura Y, et al: Gene
expression analysis of a Helicobacter pylori-infected and high-salt
diet-treated mouse gastric tumor model: Identification of CD177 as
a novel prognostic factor in patients with gastric cancer. BMC
Gastroenterol. 13:1222013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jerke U, Rolle S, Dittmar G, Bayat B,
Santoso S, Sporbert A, Luft F and Kettritz R: Complement receptor
Mac-1 is an adaptor for NB1 (CD177)-mediated PR3-ANCA neutrophil
activation. J Biol Chem. 286:7070–7081. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao JJ, Pan K, Wang W, Chen JG, Wu YH, Lv
L, Li JJ, Chen YB, Wang DD, Pan QZ, et al: The prognostic value of
tumor-infiltrating neutrophils in gastric adenocarcinoma after
resection. PLoS One. 7:e336552012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zheng RS, Zhang SW, Sun KX, Chen R, Wang
SM, Li L, Zeng HM, Wei WW and He J: Cancer statistics in China,
2016. Zhonghua Zhong Liu Za Zhi. 45:212–220. 2023.(In Chinese).
PubMed/NCBI
|
|
13
|
de Torres JP, Marín JM, Casanova C, Cote
C, Carrizo S, Cordoba-Lanus E, Baz-Dávila R, Zulueta JJ,
Aguirre-Jaime A, Saetta M, et al: Lung cancer in patients with
chronic obstructive pulmonary disease-incidence and predicting
factors. Am J Respir Crit Care Med. 184:913–919. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shaul ME and Fridlender ZG:
Tumour-associated neutrophils in patients with cancer. Nat Rev Clin
Oncol. 16:601–620. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Capone M, Giannarelli D, Mallardo D,
Madonna G, Festino L, Grimaldi AM, Vanella V, Simeone E, Paone M,
Palmieri G, et al: Baseline neutrophilto-lymphocyte ratio (NLR) and
derived NLR could predict overall survival in patients with
advanced melanoma treated with nivolumab. J Immunother Cancer.
6:742018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang Y, Lu JJ, Du YP, Feng CX, Wang LQ
and Chen MB: Prognostic value of neutrophil-to-lymphocyte ratio and
platelet-to-lymphocyte ratio in gastric cancer. Medicine
(Baltimore). 97:e1442018.
|
|
17
|
Sebastian NT, Raj R, Prasad R, Barney C,
Brownstein J, Grecula J, Haglund K, Xu-Welliver M, Williams TM and
Bazan JG: Association of pre-and posttreatment
neutrophil-lymphocyte ratio with recurrence and mortality in
locally advanced non-small cell lung cancer. Front Oncol.
10:5988732020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang J, Yibin J, Nana W, Zhang X, Tan B,
Zhang G and Cheng Y: The clinical significance of tumorinfiltrating
neutrophils and neutrophil-to-CD8+ lymphocyte ratio in patients
with resectable esophageal squamous cell carcinoma. J Transl Med.
12:72014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fang LY, Izumi K, Lai KP, Liang L, Li L,
Miyamoto H, Lin WJ and Chang C: Infiltrating macrophages promote
prostate tumorigenesis via modulating androgen receptor-mediated
CCL4-STAT3 signaling. Cancer Res. 73:5633–5646. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang Y, Fang T, Huang L, Wang H, Zhang L,
Wang Z and Cui Y: Neutrophils infiltrating pancreatic ductal
adenocarcinoma indicate higher malignancy and worse prognosis.
Biochem Biophys Res. 501:313–319. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yang J, Deng M, Bi M, Wang Y, Qiao X and
Zhang S: Prognostic values of inflammatory indexes in
bevacizumab-treated patients with advanced non-small-cell lung
cancer. Future Sci OA. 8:FSO7982022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Svaton M, Blazek J, Krakorova G, Buresova
M, Teufelova Z, Vodicka J, Hurdalkova K, Barinova M and Pesek M:
Laboratory parameters are possible prognostic markers in patients
with advanced-stage NSCLC treated with bevacizumab plus
chemotherapy. J Cancer. 12:5753–5759. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liu D, Jin J, Zhang L, Li L, Song J and Li
W: The neutrophil to lymphocyte ratio may predict benefit from
chemotherapy in lung cancer. Cell Physiol Biochem. 46:1595–1605.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Punjabi A, Barrett E, Cheng A, Mulla A,
Walls G, Johnston D, McAleese J, Moore K, Hicks J, Blyth K, et al:
Neutrophil-Lymphocyte ratio and absolute lymphocyte count as
prognostic markers in patients treated with curative-intent
radiotherapy for non-small cell lung cancer. Clin Oncol (R Coll
Radiol). 33:e331–e338. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Platini H, Ferdinand E, Kohar K, Prayogo
SA, Amirah S, Komariah M and Maulana S: Neutrophil-to-Lymphocyte
ratio and platelet-to-lymphocyte ratio as prognostic markers for
advanced non-small-cell lung cancer treated with immunotherapy: A
systematic review and meta-analysis. Medicina (Kaunas).
58:10692022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Coffelt SB, Wellenstein MD and de Visser
KE: Neutrophils in cancer:neutral no more. Nat Rev Cancer.
16:443–446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sionov RV, Fridlender ZG and Granot Z: The
multifaceted roles neutrophils play in the tumor microenvironment.
Cancer Microenviron. 8:125–158. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Eruslanov EB, Bhojnagarwala PS, Quatromoni
JG, Stephen TL, Ranganathan A, Deshpande C, Akimova T, Vachani A,
Litzky L, Hancock WW, et al: Tumor-associated neutrophils stimulate
T cell responses in earlystage human lung cancer. J Clin Invest.
124:5466–5480. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Carus A, Ladekarl M, Hager H, Pilegaard H,
Nielsen PS and Donskov F: Tumor-associated neutrophils and
macrophages in non-small cell lung cancer: No immediate impact on
patient outcome. Lung Cancer. 81:130–137. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ilie M, Hofman V, Ortholan C, Bonnetaud C,
Coëlle C, Mouroux J and Hofman P: Predictive clinical outcome of
the intratumoral CD66b-positive neutrophil-to-CD8-positive T-cell
ratio in patients with resectable nonsmall cell lung cancer.
Cancer. 118:1726–1737. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Schiffmann LM, Fritsch M, Gebauer F,
Günther SD, Stair NR, Seeger JM, Thangarajah F, Dieplinger G,
Bludau M, Alakus H, et al: Tumour-infiltrating neutrophils
counteract anti-VEGF therapy in metastatic colorectal cancer. Br J
Cancer. 120:69–78. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Rakaee M, Busund LT, Paulsen EE,
Richardsen E, Al-Saad S, Andersen S, Donnem T, Bremnes RM and
Kilvaer TK: Prognostic effect of intratumoral neutrophils across
histological subtypes of non-small cell lung cancer. Oncotarget.
7:72184–72196. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Albrengues J, Shields MA, Ng D, Park CG,
Ambrico A, Poindexter ME, Upadhyay P, Uyeminami DL, Pommier A,
Küttner V, et al: Neutrophil extracellular traps produced during
inflammation awaken dormant cancer cells in mice. Science.
361:eaao42272018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Taucher E, Mykoliuk I, Lindenmann J and
Smolle-Juettner FM: Implications of the immune landscape in COPD
and lung cancer: Smoking versus other causes. Front Immunol.
13:8466052022. View Article : Google Scholar : PubMed/NCBI
|