Introduction
Colorectal cancer (CRC) is highly prevalent in many countries, and surgery is an important curative treatment. Postoperative complications related to anastomosis, including postoperative anastomotic bleeding and leakage, remain serious, and surgeons are always concerned about them. Anastomotic complications are related to short-term outcomes, including the length of hospital stay and reoperation rate, and to long-term outcomes, such as disease-free survival and overall survival, because they are related to postoperative chemotherapy administration (1,2). The reported anastomotic leakage incidence in left-sided colorectal surgery is approximately 10%, and various risk factors have been identified, including male sex and low rectal anastomosis (3,4). The significance of instrumented anastomosis compared to manual suturing in anastomotic leakage is still under debate (5). However, the use of instrumented anastomosis is globally widespread because of its advantage of being a simplified and stable anastomotic technique, and secure stapler manipulation is becoming increasingly important (6). Manual circular staplers (MCSs) have long been used for anastomosis. Applying considerable force is necessary to run the MCS stably. Stabilizing the anastomosis device and performing an anastomosis without applying stress to the site is difficult for some surgeons, depending on their body shape and arm strength. Automated anastomosis devices have been commercially available in Japan since 2019. Automatic anastomosis machines significantly reduce the force required by the operator for anastomosis. Therefore, it is expected that surgeons with small hands, including female surgeons, can stably use them. However, analyses of the association between manual/automatic anastomosis devices and postoperative anastomosis-related complications are limited. We aimed to clarify the usefulness of the automatic anastomosis device in sigmoid colon and rectal cancer surgeries, using cases from our institution and a meta-analysis based on a literature review.
Materials and methods
Patients and study design of the retrospective study
This retrospective observational cohort study was approved by the Ethical Review Board of the Osaka University Hospital (No. 15144-7). Written informed consent was obtained from the patients for data publication.
This was a single-center retrospective study. Patients undergoing radical resection and anastomosis for sigmoid colon or rectal cancer using a circular stapler between 2018 and 2022 were enrolled in this cohort study. Cases of emergency surgery, inflammatory bowel disease, and simultaneous surgery for other cancers were excluded, and 415 were included in this study (Table I). The median age was 66 years (age range: 27–98 years). Skilled gastrointestinal surgeons performed the surgeries. Bowel dissection was performed using a stapler, and an air leak test was intraoperatively performed after anastomosis in all cases. No air leak was confirmed in all cases. Preoperative chemotherapy, super-low anterior resection, and high-risk cases were treated by covering the stoma and/or performing transanal drainage at the discretion of the surgeon. Postoperative management followed a uniform flow according to the clinical pathway. The primary endpoint was the anastomotic complication rate. All data were collected from medical records up to 30 days after surgery.
 |
Table I.
Patient characteristics (n=414).
|
Table I.
Patient characteristics (n=414).
| Characteristics |
Value |
| Mean age, years (range) |
66.0 (27–98) |
| Sex, n (male/female) |
229/185 |
| BMI, n (<25/≥25 kg/m2) |
329/85 |
| Smoking history, n (yes/no) |
79/335 |
| History of DM, n (yes/no) |
56/358 |
| Preoperative Alb, n (<3.8/≥3.8 g/dl) |
78/336 |
| Tumor lesion, n (Ra, Rb/S, RS) |
197/217 |
| Surgical method, n (LAR, sLAR/SR, AR) |
189/225 |
| Surgical approach, n (Op/Lp/Rbs) |
7/212/195 |
| Mean operation time, min (range) |
289 (69–836) |
| Mean blood loss, ml (range) |
61 (0–4900) |
| CS, n (manual/automatic) |
231/183 |
| Transanal drain, n (yes/no) |
106/308 |
| Diverting stoma, n (yes/no) |
81/333 |
| Anastomosis complication, n (yes/no) |
11/403 |
Anastomosis
Manual anastomosis was performed using the ETHICON Circular Stapler CDH or the EEA Circular Stapler, and automatic anastomosis was performed using the ECHELON CIRCULAR Powered Stapler. Gastrointestinal surgeons with at least five years of experience operated the anastomotic devices.
Definition of anastomotic complications
Anastomotic leakage and bleeding were included as anastomotic complications. Postoperative fever, abdominal pain, elevated inflammatory levels, other clinical findings, peri-anastomotic fluid retention and free air observed on computed tomography, and digestive fluid drainage from the drain were considered to indicate anastomotic leakage. Additionally, postoperative hemorrhage with delayed initiation of postoperative feeding was considered an anastomotic hemorrhage.
Statistical analysis of the retrospective study
Statistical analyses were performed using JMP 17.0 statistical software (SAS Institute) and R. Enumeration data were compared using Mann-Whitney's U test, Pearson's Chi-square tests, Fisher's exact test and propensity score matching. Statistical significance was defined as a P-value <0.05.
Meta-analysis
We performed a meta-analysis, including the present outcomes to evaluate the advantages of the powered circular stapler (PCS) over the manual circular stapler for anastomoses in left-sided colorectal surgery. The included studies assessed anastomotic complications and validated circular staplers following CRC surgery. This review was performed in accordance with the PRISMA Reporting Items for Systematic Reviews and Meta-Analyses guidelines. To collect the trial data, we searched the Cochrane Central Register of Controlled Trials (Central) and PubMed, using the following search terms: ‘powered circular’ AND ‘anastomotic’ on October 20, 2023. The following studies were excluded: emergency surgery and non-colorectal surgery. Two independent reviewers at Osaka University assessed the titles and abstracts. We performed the meta-analysis with the Mantel-Haenszel random-effects model, using R software (CRAN, R3·6·2; https://cran.r-project.org/). Statistical significance was set at a P-value <0.05. This systematic assessment has not been registered in a public database. The statistical methods used in this study were reviewed by Miyoshi N. Because all included studies were observational, the Risk of Bias Assessment tool for Nonrandomized Studies was used to assess the risk of bias in the included studies. Funnel plots assessed publication bias.
Results
Retrospective study
Table II presents the background characteristics of the 414 patients in the two groups, 231 and 183 in the MCS and PCS groups. On the basis of ROC curves, the age and albumin level cutoff values were 70 years and 3.8 g/dl. There were 11 anastomotic complication cases, including postoperative anastomotic leakage and bleeding: eight (3.5%) and three (1.6%) in the MCS and PCS groups. There was only one reoperation case which occurred in the PCS group. The PCS group was older than the MCS group, had a body mass index ≥25 kg/m2, and smokers were more common in the MCS group. The risk analysis of each factor for anastomotic complications was performed. Univariate analysis revealed significant surgical site and methodological differences (Table III).
 |
Table II.
Characteristics of patients in the two groups.
|
Table II.
Characteristics of patients in the two groups.
| |
Circular stapler (n=414) |
|
| |
|
|
| Characteristics |
Manual (n=231) |
Automatic (n=183) |
P-value |
| Mean age, years (range) |
64.6 (27.0–93.0) |
67.9 (35.0–98.0) |
0.001a |
| Sex, n (male/female) |
129/102 |
100/83 |
0.807b |
| BMI, n (<25/≥25 kg/m2) |
175/56 |
154/29 |
0.035b |
| Smoking history, n (yes/no) |
54/177 |
25/158 |
0.012b |
| History of DM, n (yes/no) |
29/202 |
27/156 |
0.515b |
| Preoperative Alb, n (<3.8/≥3.8 g/dl) |
43/188 |
35/148 |
0.895b |
| Tumor lesion, n (Ra, Rb/S, RS) |
116/115 |
81/102 |
0.228b |
| Surgical method, n (LAR, sLAR/SR, AR) |
105/126 |
84/99 |
0.927b |
| Surgical approach, n (Op/Lp/Rbs) |
5/135/91 |
2/77/104 |
0.001c |
| Mean operation time, min (range) |
293.6 (69.0–836.0) |
284.3 (86.0–793.0) |
0.527a |
| Mean blood loss, ml (range) |
55.6 (0.0–3400.0) |
68.5 (0.0–4900.0) |
0.692a |
| Transanal drain, n (yes/no) |
67/164 |
39/144 |
0.074b |
| Diverting stoma, n (yes/no) |
38/193 |
43/140 |
0.072b |
| Anastomosis complication, n (yes/no) |
8/223 |
3/180 |
0.359c |
 |
Table III.
Results of univariate analysis of clinical factors for anastomotic complications.
|
Table III.
Results of univariate analysis of clinical factors for anastomotic complications.
| |
Anastomotic complication |
Univariate analysis |
|
| |
|
|
|
| Characteristics |
Yes, n |
No, n |
OR |
95% CI |
P-value |
| Age (<70/≥70 years) |
8/3 |
214/189 |
2.355 |
0.615–0.999 |
0.234 |
| Sex (male/female) |
7/4 |
222/181 |
1.426 |
0.411–4.950 |
0.761 |
| BMI (<25/≥25 kg/m2) |
9/2 |
320/83 |
1.167 |
0.247–5.505 |
1.000 |
| Smoking history (yes/no) |
2/9 |
77/326 |
0.940 |
0.199–4.442 |
1.000 |
| History of DM (yes/no) |
1/10 |
55/348 |
0.632 |
0.079–5.040 |
1.000 |
| Preoperative Alb level (<3.8/≥3.8 g/dl) |
3/8 |
75/328 |
1.640 |
0.424–6.328 |
0.441 |
| Tumor lesion (Ra, Rb/S, RS) |
9/2 |
188/215 |
5.146 |
1.098–24.116 |
0.027 |
| Surgical method (LAR, sLAR/SR, AR) |
9/2 |
180/223 |
5.575 |
1.189–26.127 |
0.029 |
| CS (manual/automatic) |
8/3 |
223/180 |
2.152 |
0.562–8.231 |
0.359 |
| Surgical approach (Op/Lp, Rbs) |
1/10 |
6/397 |
6.616 |
0.727–60.198 |
0.173 |
| Operation time (>274/≤274 min) |
9/2 |
160/243 |
6.834 |
1.457–32.042 |
0.009 |
| Blood loss (>15/≤15 ml) |
9/2 |
204/199 |
4.389 |
0.936–20.569 |
0.038 |
| Transanal drain (yes/no) |
5/6 |
101/302 |
2.491 |
0.744–8.339 |
0.158 |
| Diverting stoma (yes/no) |
3/8 |
78/325 |
1.562 |
0.405–6.025 |
0.456 |
Subsequently, we limited the analysis to patients older than 55 years of age and found an increased risk of anastomotic complications with MCS compared with PCS. However, this difference was not statistically significant in patients older than 55 years of age (Table IV). In the population older than 65 years of age, there were 0 and 4 anastomotic complications in the PCS and MCS groups, respectively. This finding indicates an increased risk of anastomotic complications with manual anastomotic devices in this cohort (Table V).
 |
Table IV.
Results of univariate analysis of clinical factors for anastomotic complications among patients older than 55 years.
|
Table IV.
Results of univariate analysis of clinical factors for anastomotic complications among patients older than 55 years.
| |
Anastomotic complication |
Univariate analysis |
|
| |
|
|
|
| Characteristics |
Yes, n |
No, n |
OR |
95% CI |
P-value |
| Sex (male/female) |
6/1 |
181/139 |
4.607 |
0.548–38.715 |
0.245 |
| BMI (<25/≥25 kg/m2) |
7/0 |
254/66 |
|
|
0.352 |
| Smoking history (yes/no) |
2/5 |
62/258 |
1.666 |
0.315–8.781 |
0.626 |
| History of DM (yes/no) |
1/6 |
53/267 |
0.839 |
0.099–7.117 |
1.000 |
| Preoperative Alb level (<3.8/≥3.8 g/dl) |
3/4 |
64/256 |
3.000 |
0.654–13.741 |
0.154 |
| Tumor lesion (Ra, Rb/S, RS) |
5/2 |
145/175 |
3.017 |
0.576–15.780 |
0.253 |
| Surgical method (LAR, sLAR/SR, AR) |
5/2 |
138/182 |
3.297 |
0.630–17.248 |
0.246 |
| CS (manual/automatic) |
6/1 |
172/148 |
5.162 |
0.614–43.373 |
0.131 |
| Surgical approach (Op/Lp, Rbs) |
1/6 |
5/315 |
10.500 |
1.059–104.096 |
0.122 |
| Operation time (>274/≤274 min) |
5/2 |
125/195 |
3.900 |
0.745–20.411 |
0.119 |
| Blood loss (>15/≤15 ml) |
6/1 |
162/158 |
5.851 |
0.696–49.159 |
0.122 |
| Transanal drain (yes/no) |
2/5 |
75/245 |
1.306 |
0.248–6.872 |
0.669 |
| Diverting stoma (yes/no) |
3/4 |
62/258 |
3.120 |
0.680–14.304 |
0.148 |
 |
Table V.
Results of univariate analysis of clinical factors for anastomotic complications among patients older than 65 years.
|
Table V.
Results of univariate analysis of clinical factors for anastomotic complications among patients older than 65 years.
| |
Anastomotic complication |
Univariate analysis |
|
| |
|
|
|
| Characteristics |
Yes, n |
No, n |
OR |
95% CI |
P-value |
| Sex (male/female) |
3/1 |
135/110 |
2.444 |
0.250–23.830 |
0.630 |
| BMI (<25/≥25 kg/m2) |
4/0 |
194/51 |
|
|
0.584 |
| Smoking history (yes/no) |
1/3 |
49/196 |
1.333 |
0.135–13.097 |
1.000 |
| History of DM (yes/no) |
1/3 |
45/200 |
1.481 |
0.150–14.573 |
0.560 |
| Preoperative Alb level (<3.8/≥3.8 g/dl) |
2/2 |
55/190 |
3.454 |
0.475–25.090 |
3.454 |
| Tumor lesion (Ra, Rb/S, RS) |
2/2 |
109/136 |
1.247 |
0.172–9.000 |
1.000 |
| Surgical method (LAR, sLAR/SR, AR) |
2/2 |
104/141 |
1.355 |
0.187–9.782 |
1.000 |
| CS (manual/automatic) |
4/0 |
122/123 |
|
|
0.122 |
| Surgical approach (Op/Lp, Rbs) |
1/3 |
3/242 |
26.888 |
1.153–302.993 |
0.063 |
| Operation time (>274/≤274/min) |
2/2 |
94/151 |
1.606 |
0.222–11.597 |
0.640 |
| Blood loss (>15/≤15 ml) |
3/1 |
119/126 |
3.176 |
0.325–30.962 |
0.362 |
| Transanal drain (yes/no) |
2/2 |
64/181 |
2.828 |
0.390–20.495 |
0.286 |
| Diverting stoma (no/yes) |
3/1 |
201/44 |
1.522 |
0.154–14.985 |
0.551 |
To balance the baseline characteristics between the MCS and PCS groups, we implemented 1:3 propensity score matching. After this matching, 285 patients were ultimately included in this study (Table SI). Although the risk associated with age did not increase as significantly as in the pre-matching analysis, the risk of anastomotic complications remained higher in the PCS group (Table SII, Table SIII, Table SIV). The systematic review did not reveal a clear significance; recognizing the limitation posed by the small sample size, we subsequently conducted a meta-analysis.
Meta-analysis
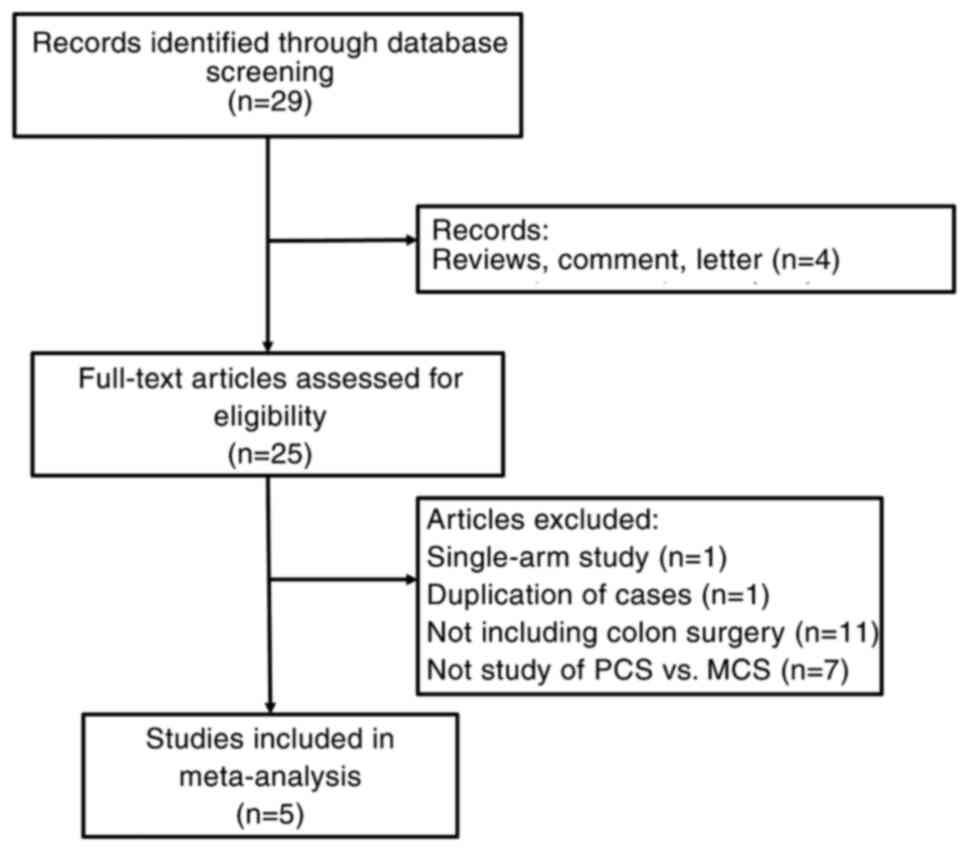
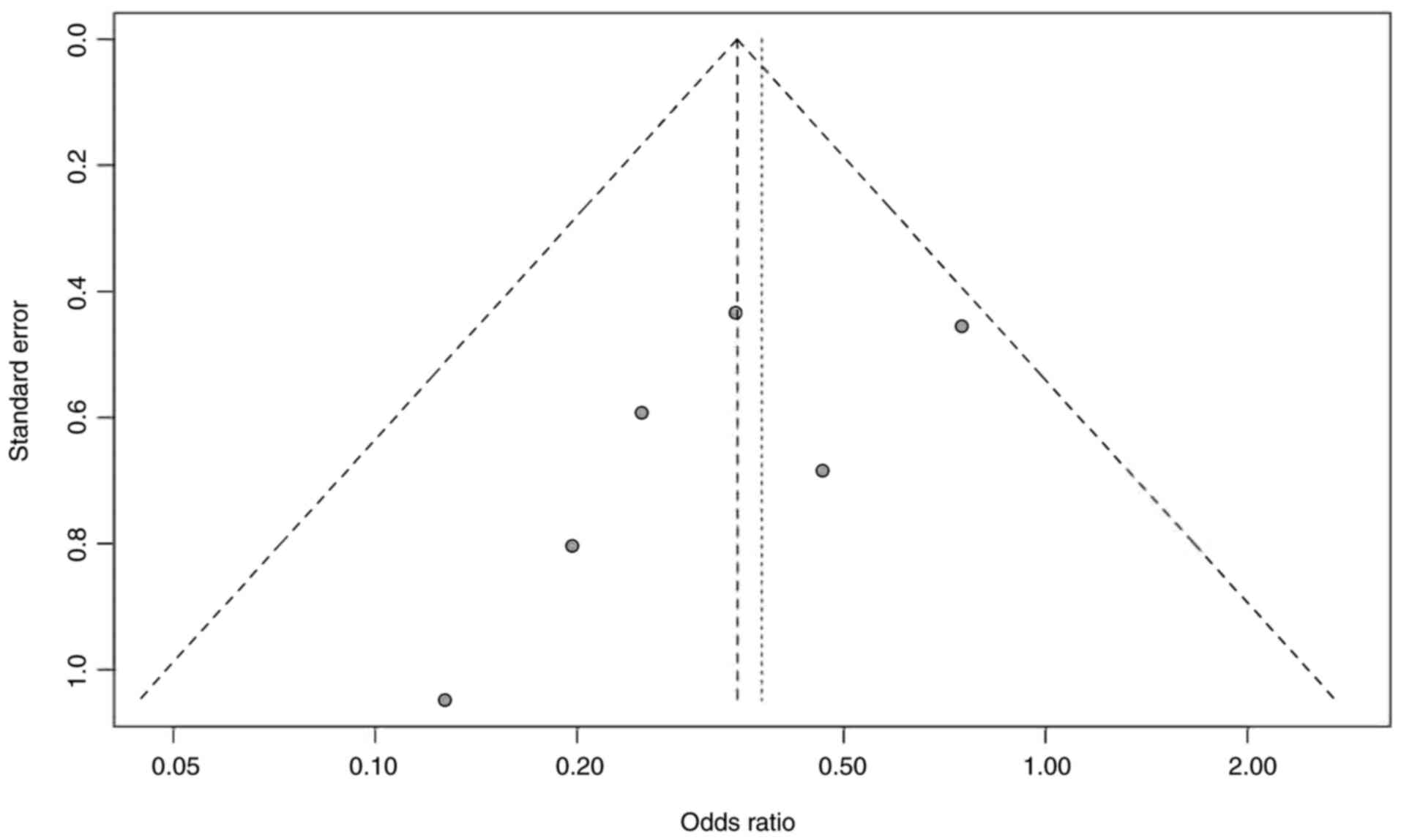
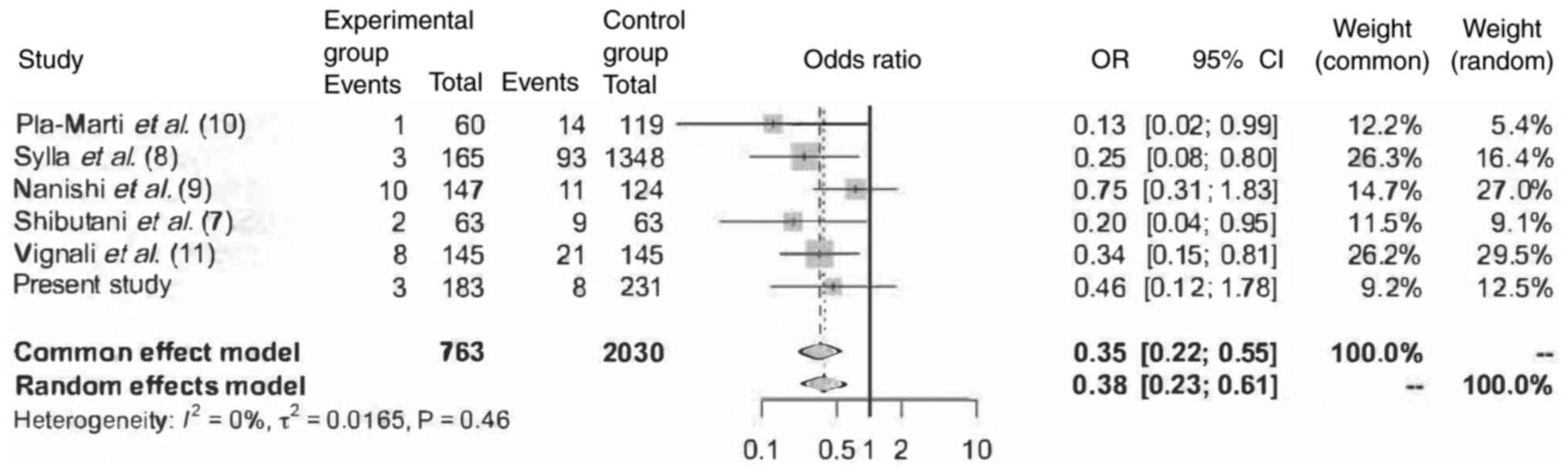
The search strategy retrieved 29 articles. Four articles were excluded on the basis of the article type. Of the remaining articles, 11 focused on vascular or upper gastrointestinal surgery, one was a duplication, and the other was a single-arm trial. Five articles and the present study were ultimately included in the meta-analysis (Fig. 1). Table VI summarizes the clinical characteristics of the five included studies (7–11), and Table SV summarizes the risk of bias for all the studies. The number of events reported by Nanishi et al (9) and Vignali et al (11) included anastomotic bleeding. Fig. 2 presents the funnel plot. Three studies demonstrated significant differences in the anastomotic complications between the powered and manual circular staplers. All articles were respective cohort studies, comprising 2793 patients: 763 and 2030 using PCS and MCS, respectively. Anastomotic leakage was observed in 27 and 156 patients in the PCS and MCS groups, retrospectively. One study focused on robot-assisted low anterior resection, whereas another focused exclusively on rectal surgery. Three studies focused on left-sided colorectal surgery, one of which focused on cancer surgery. The meta-analysis results are presented as a forest plot (Fig. 3). No heterogeneity was observed in these data. In the meta-analysis, the common-effect and random-effects models demonstrated similar results between PCS and MCS, with both methods demonstrating significant differences (common-effects model: odds ratio [OR]=0.346, 95% confidence interval [95% CI]: 0.219–0.547 P<0.0001; random-effects model: OR=0.376, 95% CI: 0.232–0.610 P<0.0001).
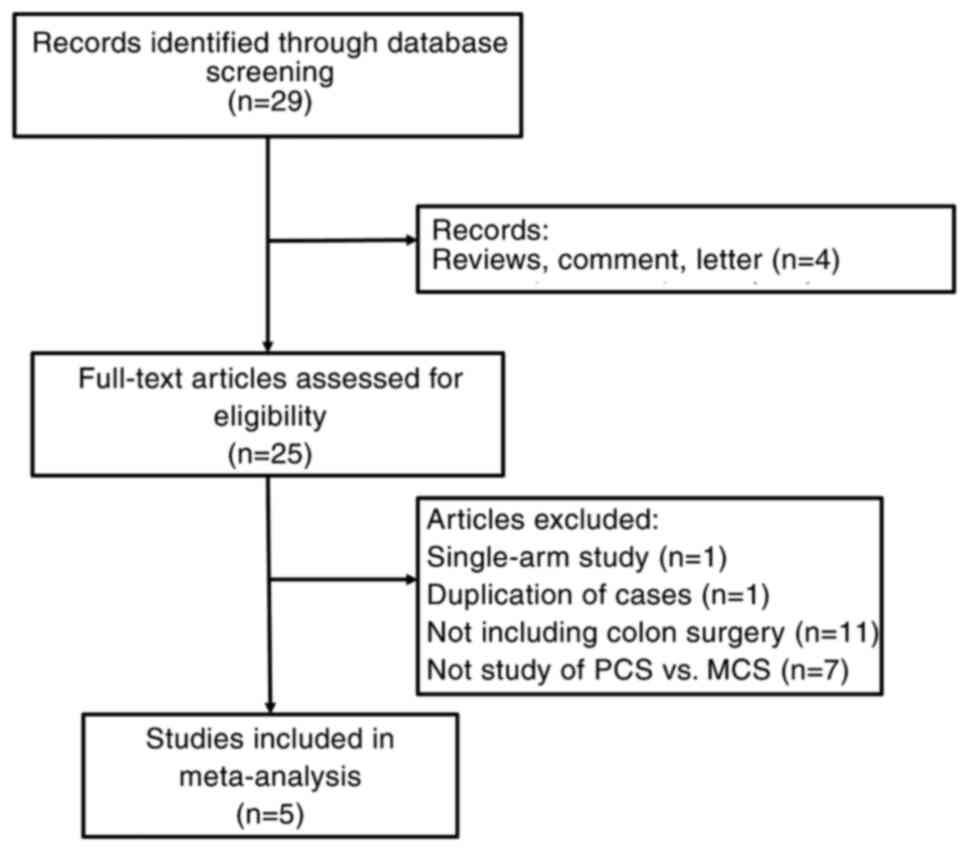 |
Figure 1.
Study flow diagram. MCS, manual circular stapler; PCS, powered circular stapler.
|
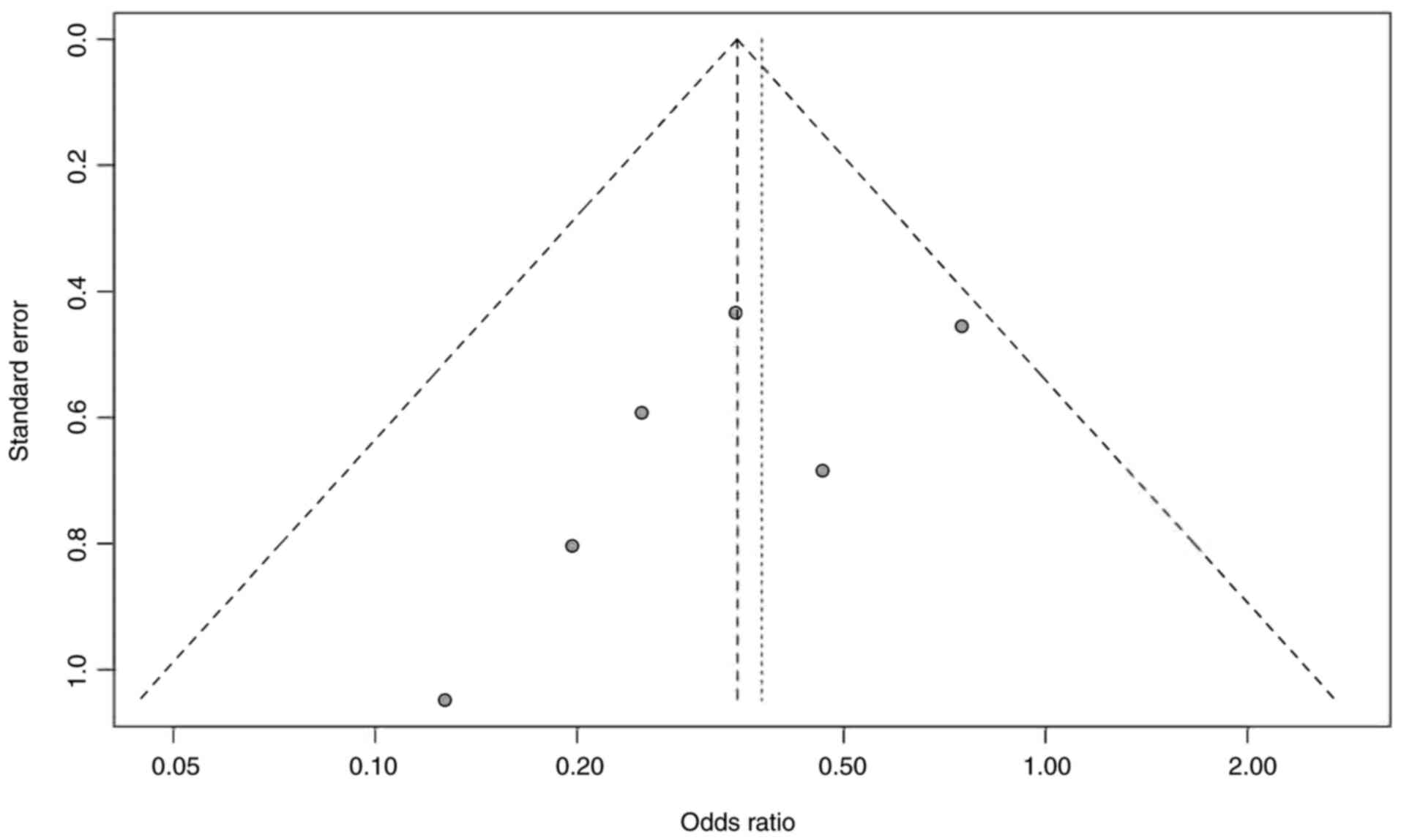 |
Figure 2.
Funnel plot of publication bias.
|
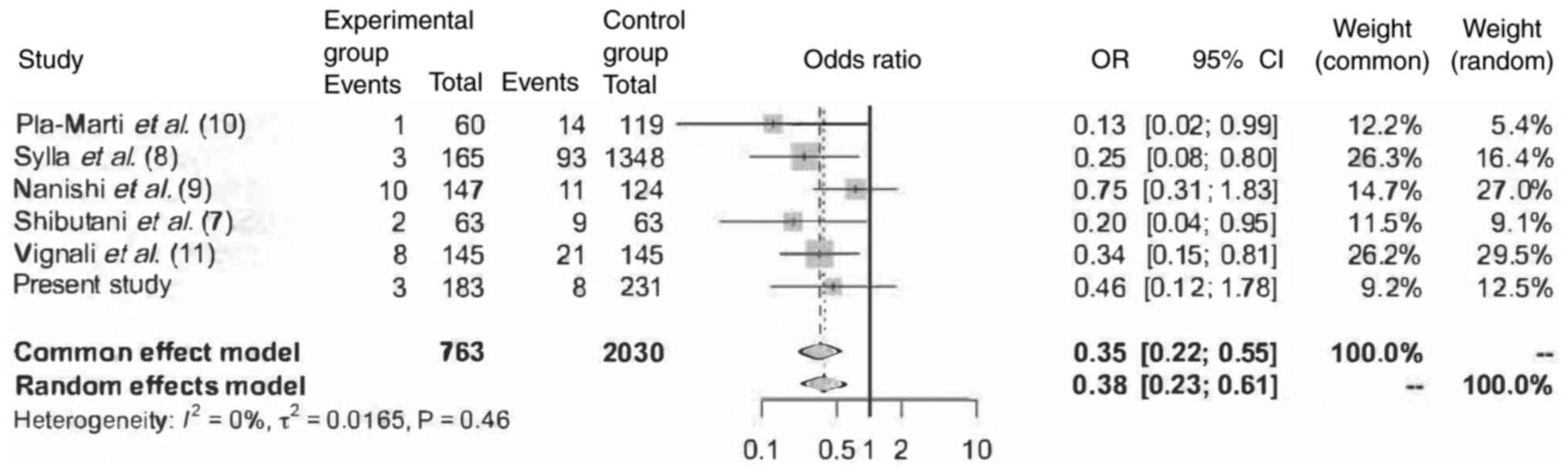 |
Figure 3.
Forest plot of the six studies. OR, odds ratio.
|
 |
Table VI.
Characteristics of the included studies.
|
Table VI.
Characteristics of the included studies.
| |
|
|
|
No. of patients |
|
|
Diverting stoma present/absent, n |
|
AL rate, % |
|
| First author/s, year |
Study design |
Setting (center)/country |
Study period |
|
Anastomosis type |
Included benign tumor |
|
Follow-up after surgery |
|
|
| MCS |
PCS |
MCS |
PCS |
MCS |
PCS |
(Refs.) |
| Shibutani et al, 2023 |
Retrospective cohort study |
Single/Japan |
2016-2022 |
63 |
63 |
Left-sided colorectal cancer with DST anastomosis |
No |
5/58 |
7/56 |
NR |
14.30 |
3.20 |
(7) |
| Sylla et al, 2022 |
Retrospective cohort study |
Multi/USA |
2016-2020 (single arm and historical cohort) |
1,348 |
165 |
Left-sided colorectal resection with anastomoses |
Yes |
NR |
NR |
28±14 days after discharge |
6.90 |
1.80 |
(8) |
| Nanishi et al, 2023 |
Retrospective cohort study |
Single/Japan |
2019-2022 |
124 |
147 |
Ro-LAR for primary rectal cancer |
No |
4/120 |
2/145 |
30 days |
8.90 |
6.80 |
(9) |
| Pla-Martí et al, 2021 |
Retrospective cohort study |
Single/Spain |
2017-2020 |
119 |
60 |
Left-sided circular stapled colorectal anastomosis 5 cm above the anal verge |
Yes |
0/119 |
0/60 |
30 days |
11.80 |
1.70 |
(10) |
| Vignali et al, 2023 |
Retrospective cohort study |
Single/Italy |
2017-2022 |
145 |
145 |
Laparoscopic colon resection and anastomosis to the rectum; age >18 years |
Yes |
33/112 |
37/108 |
30 days |
14.50 |
5.50 |
(11) |
Discussion
In this cohort study conducted at our institution, patients in the PCS group were significantly older than those in the MCS group. Automatic anastomosis machines have become popular only in recent years, possibly reflecting the older patients associated with the aging society of Japan. Attention has recently been focused on safe surgery in elderly patients at high surgical risk; however, age was not an independent risk factor in this cohort study. Conversely, the analysis limited to elderly patients demonstrated no significant difference; however, the risk ratio increased in the MCS group compared with the PCS group, suggesting that anastomotic device developments positively affected older patients. Older patients have more vulnerable tissues and less tissue regenerative capacity compared to younger patients, and the difference in stress on the anastomotic tissues was considered to have a major influence. Although the association between postoperative transanal drain placement, anastomotic leakage prevention, and increased anastomotic bleeding has been discussed, no association was found in the present cohort study (6,12). As is accepted, the complication risk increased as the anastomosis was lowered, and an increased risk was observed in patients with a covering stoma. However, this observation was made because the stoma was originally placed in patients with a high anastomotic leakage risk, including those with a low anastomosis.
Circular staplers and double-stapled techniques have been common anastomosis methods used for over 40 years (13). Circular staplers have improved over the years, with the automatic version becoming available in 2019 and introduced to our hospital in 2020 for colorectal surgery. The anastomosis has been modified regarding staple alignment and tissue compressibility, and automation is considered an alteration that can reduce inter-operator differences. Conventional manual anastomosis requires approximately 30 kg of force to fire, but the average grip force of women in Japan is approximately 30 kg, proving that it is not easy to fire (14–16). Inadequate manipulation causes complications by anastomotic tip instability, intestinal mucosa damage, and anastomotic site stress.
The meta-analysis revealed a significant difference between PCS and MCS. Furthermore, this analysis concluded that automatic anastomosis devices may be more useful than manual devices in reducing anastomotic complications.
This meta-analysis has several limitations. First, patients and their backgrounds differed slightly between studies. Notably, one study excluded all cases with diverting stomas, and another excluded cases in which a stoma was planned before surgery, possibly influencing the results. Second, publication bias could not be ruled out because of the few included studies. Third, all included studies were retrospective cohorts and may have had reporting bias.
In conclusion, a PCS may be useful for reducing the risk of anastomotic complications in patients undergoing CRC surgery.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be requested from the corresponding author.
Authors' contributions
RM, NM, YD and HE designed the study. RM, NM, RH, SK, SM, MTa, YS, TH, AH, TO, MTe, YK and MU performed the research and were responsible for collecting and analyzing clinical data. RM and NM confirm the authenticity of all the raw data. RM and NM analyzed the data. RM and NM wrote the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
The present retrospective, observational cohort study was approved by the Ethical Review Board of the Osaka University Hospital (approval no. 15144-7; Suita, Japan). Written informed consent was obtained from the patients for participation.
Patient consent for publication
Written informed consent was obtained from the patients for data publication.
Competing interests
The authors declare that they have no competing interests.
Glossary
Abbreviations
Abbreviations:
|
CRC
|
colorectal cancer
|
|
MCS
|
manual circular stapler
|
|
PCS
|
powered circular stapler
|
References
|
1
|
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P and Finan P: Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: Systematic review and meta-analysis. Ann Surg. 253:890–899. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Matsuda C, Kudo T, Morimoto Y, Kagawa Y, Tei M, Ide Y, Miyoshi N, Takahashi H, Uemura M, Takemasa I, et al: A phase II study of neoadjuvant capecitabine, oxaliplatin, and irinotecan (XELOXIRI) in patients with locally advanced rectal cancer. Ann Gastroenterol Surg. 7:81–90. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
2017 European Society of Coloproctology (ESCP) collaborating Group, : Association of mechanical bowel preparation with oral antibiotics and anastomotic leak following left sided colorectal resection: An international, multi-centre, prospective audit. Colorectal Dis. 20 (Suppl 6):S15–S32. 2018. View Article : Google Scholar
|
|
4
|
Lauricella S, Peyser D, Carrano FM and Sylla P: Intraluminal anastomotic assessment using indocyanine green near-infrared imaging for left-sided colonic and rectal resections: A systematic review. J Gastrointest Surg. 27:615–625. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tsalikidis C, Mitsala A, Mentonis VI, Romanidis K, Pappas-Gogos G, Tsaroucha AK and Pitiakoudis M: Predictive Factors for Anastomotic Leakage Following Colorectal Cancer Surgery: Where Are We and Where Are We Going? Curr Oncol. 30:3111–3137. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Guo C, Fu Z, Qing X and Deng M: Prophylactic transanal drainage tube placement for preventing anastomotic leakage after anterior resection for rectal cancer: A meta-analysis. Colorectal Dis. 24:1273–1284. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shibutani M, Fukuoka T, Iseki Y, Kasashima H, Kitayama K and Maeda K: Impact of a circular powered stapler on preventing anastomotic leakage in patients with left-sided colorectal cancer: A retrospective study. BMC Surg. 23:2052023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sylla P, Sagar P, Johnston SS, Dwarakanathan HR, Waggoner JR, Schwiers M and Roy S: Outcomes associated with the use of a new powered circular stapler for left-sided colorectal reconstructions: A propensity score matching-adjusted indirect comparison with manual circular staplers. Surg Endosc. 36:2541–2553. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nanishi K, Hino H, Shiomi A, Kagawa H, Manabe S, Yamaoka Y, Chen K and Maeda C: Use of a Powered Circular Stapler Can Prevent Anastomotic Air Leakage in Robotic Low Anterior Resection for Rectal Cancer. J Anus Rectum Colon. 7:82–90. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pla-Martí V, Martín-Arévalo J, Moro-Valdezate D, García-Botello S, Mora-Oliver I, Gadea-Mateo R, Cozar-Lozano C and Espí-Macías A: Impact of the novel powered circular stapler on risk of anastomotic leakage in colorectal anastomosis: A propensity score-matched study. Tech Coloproctol. 25:279–284. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vignali A, Gozzini L, Gasparini G, Calef R, Rosati R and Elmore U: Impact of powered circular stapler on anastomotic leak after anastomosis to the rectum: A propensity score matched study. Int J Colorectal Dis. 38:2112023. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fujino S, Yasui M, Ohue M and Miyoshi N: Efficacy of transanal drainage tube in preventing anastomotic leakage after surgery for rectal cancer: A meta-analysis. World J Gastrointest Surg. 15:1202–1210. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Griffen FD and Knight CD Sr, Whitaker JM and Knight CD Sr: The double stapling technique for low anterior resection. Results, modifications, and observations. Ann Surg. 211:745–751; discussion 751-2. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rojatkar P, Henderson CE, Hall S, Jenkins SA, Paulin-Curlee GG, Clymer JW and Nagle DA: A novel powered circular stapler designed for creating secure anastomoses. Med Device Diagn Eng. 2:94–100. 2017. View Article : Google Scholar
|
|
15
|
Kono E, Tada M, Kouchi M, Endo Y, Tomizawa Y, Matsuo T and Nomura S: Ergonomic evaluation of a mechanical anastomotic stapler used by Japanese surgeons. Surg Today. 44:1040–1047. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kasai R, Mizushima I, Muto T, Matsuo T, Tomizawa Y and Takeda S: Ergonomic Assessment of a Laparoscopic Stapler. Adv Biomed Eng. 2:11–16. 2013. View Article : Google Scholar
|