Introduction
The first use of rotationplasty was documented by
Borggreve (1) in 1930 and it was
applied to treat lower limb shortening caused by knee joint
tuberculosis infection. In 1975, Kristen et al (2) applied rotationplasty to treat the
recurrence of osteosarcoma in the distal femur. Rotationplasty is a
limb salvage surgery that provides a postoperative function similar
to that of below-knee amputation. The type of rotationplasty is
dependent on the initial reconstruction of the distal femur (type
AI), the proximal tibia (type AII) or the proximal femur involving
the acetabulum (type BII) (3).
During this surgical procedure, the tumor is excised in its
entirety, while preserving the neurovascular bundle, the distal
portion of the tibia and the foot. The tibia and foot are then
rotated by 180° to attach on backwards to the limb salvage portion
of the distal femur. It has been reported that this method can help
in avoiding complications, such as phantom pain, and reduce
infection rates. Following surgery, the rotated ankle joint can
function as a knee joint with the assistance of special prostheses
(4).
Pediatric and adolescent patients are at a high risk
of developing malignant bone tumors, including osteosarcoma and
Ewing's sarcoma. Amputation has conventionally been considered as a
prevailing approach for managing these types of tumors. However,
the 5-year survival rates fall short of the desired outcomes
(5). Nevertheless, the advent of
more sophisticated surgical techniques and the utilization of
neoadjuvant chemotherapy has led to a notable increase in the
5-year survival rate of patients, which currently stands at ~70%
worldwide (6). Furthermore, the
importance of functional recovery following surgery has become more
pronounced. Previous studies indicated that patients who underwent
rotationplasty tended to achieve better functional outcomes
compared with those who were subjected to knee amputation or
endoprosthesis replacement (7,8).
Benedetti et al (9)
emphasized the importance of rehabilitation following
rotationplasty for improving postoperative functional outcomes.
Morri and Forni (10) outlined the
rehabilitation methods and expected outcomes of an adult patient
who underwent rotationplasty and showed a favorable outcome. In
recent years, there has been a growing interest in functional
rehabilitation following rotationplasty. However, there is a clear
need for the development of standardized and effective
rehabilitation guidance. Therefore, the present study aimed to
develop a series of rehabilitation strategies for functional
recovery at distinct stages of the postoperative period. These
strategies were then longitudinally evaluated to assess functional
recovery rates and the quality of life of patients. The findings of
the current study could serve as a reference for patients seeking
to efficiently recover function.
Materials and methods
Participants
A total of 12 patients, including 7 males (58%) and
5 females (42%), with a mean age at surgery of 6.58±1.73 years
(range, 4–10 years), who were admitted to the Fourth Medical Center
of Chinese People's Liberation Army (PLA) General Hospital
(Beijing, China) between March 2014 and March 2019, were included.
The disease duration from onset to consultation was 3–5 months
(mean, 4.50±0.67 months). All patients are still alive today, with
a follow-up period of 60–120 months (mean, 89.83±17.55 months). In
terms of pathological subtypes, 4 patients suffered from
osteoblastic osteosarcoma (33%), 2 from chondroblastic osteosarcoma
(17%), 3 from mixed osteosarcoma (25%) and 3 from Ewing's sarcoma
(25%). The inclusion criteria were as follows: i) Peripheral
malignant bone tumor of the knee joint confirmed by preoperative
biopsy and postoperative pathology; ii) Enneking stage IIB disease
(11), with AI-type rotationplasty
(3) performed; iii) postoperative
rehabilitation for 6 months; and iv) a follow-up period of ≥5
years. Patients with multiple tumors or metastases and those who
refused to participate in the study were excluded. The present
retrospective study was approved by the Institutional Review Board
of the Fourth Medical Center of the Chinese PLA General Hospital
(approval no. 2023KY037-KS001). All patients and their duly
authorized representatives provided written informed consent for
the study to be published. All methods were performed according to
the relevant guidelines and regulations.
Surgery and treatment
All patients underwent 7–9 cycles of pre- and
post-operative chemotherapy following the protocol of the Fourth
Medical Center of the Chinese PLA General Hospital (12). This regimen included ifosfamide (2
g/m2 on days 1–5), methotrexate (8 g/m2 on
day 3) and doxorubicin (100 mg/m2 on day 5). A typical
preoperative chemotherapy regimen comprised three courses, whereas
the postoperative regimen consisted of six courses. Each course had
a duration of 5 days, with a 3-week interval between courses. Prior
and during chemotherapy, both hydration and alkalization were
employed, involving a daily fluid intake exceeding 3,000 ml.
Additionally, urine volume and pH were closely monitored to sustain
a urine pH level of between 7 and 8. In cases where the patient
exhibited a white blood cell count of <2.0×109/l, a
daily subcutaneous injection of 300 µg granulocyte
colony-stimulating factor was administered. All patients were
informed of the potential risks associated with the treatment and
provided written informed consent. The rotationplasty was performed
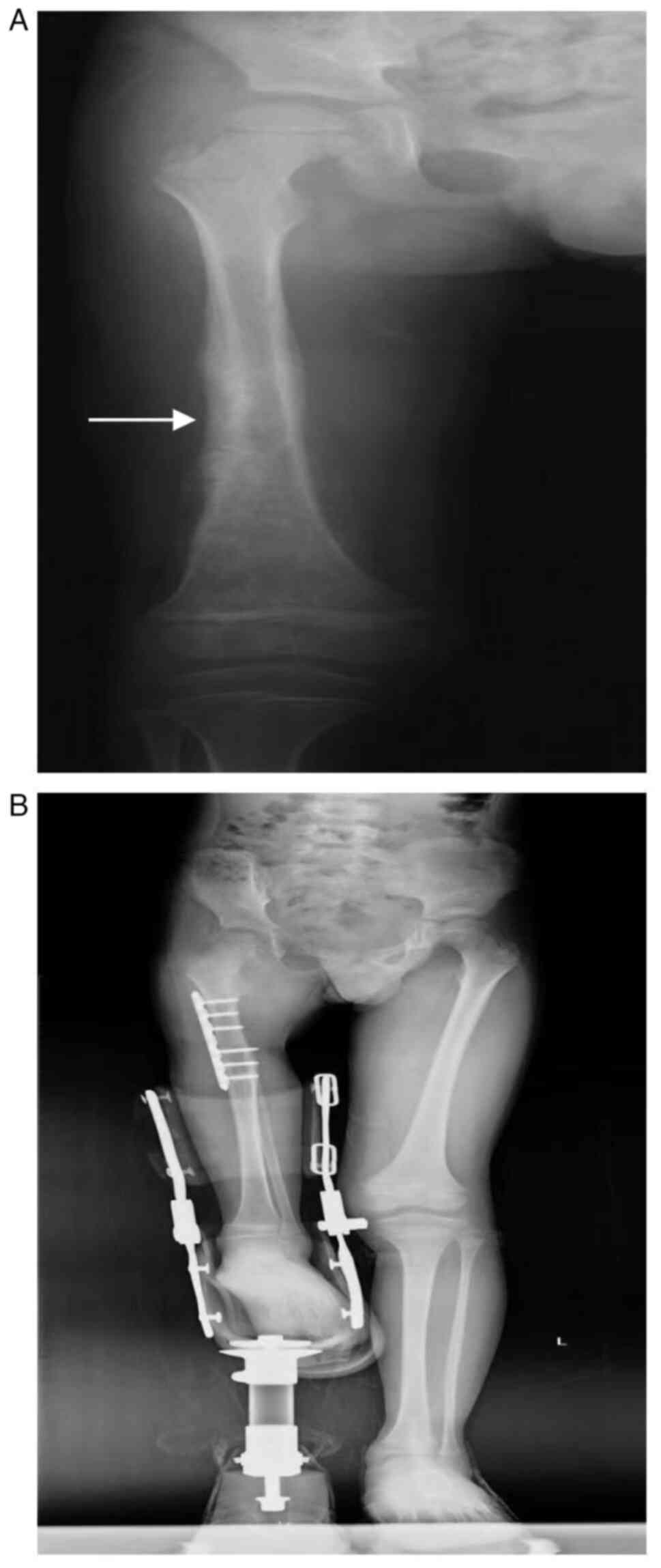
under general anesthesia. The pre- and 1-year post-surgery X-rays
of a representative patient who underwent rotationplasty are shown
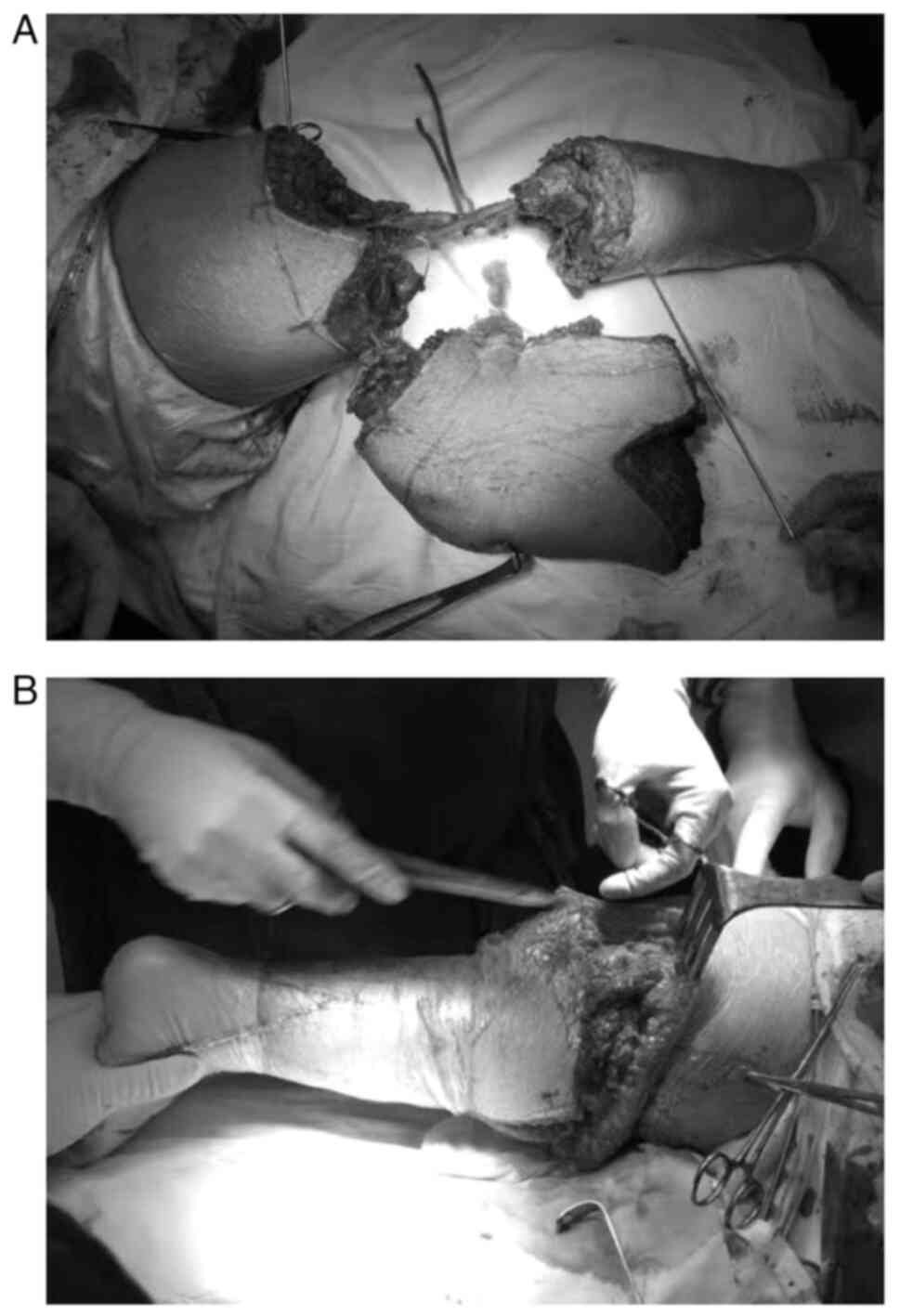
in Fig. 1. The surgical procedure
is displayed in Fig. 2. Following
surgery, the patients were required to undergo a 6-month program of
postoperative rehabilitation, either as outpatients or in the
hospital. This program involved one session per day, for 50 min,
and five sessions per week. Upon discharge, the patients continued
to receive symptomatic treatment and were scheduled for regular
follow-up appointments. These were conducted at 3-monthly intervals
during the 5-year postoperative period, and annually
thereafter.
Rehabilitation strategies
In the initial phase, spanning from the first to
third week following surgery, patients underwent immediate
rehabilitation treatment. The objectives of this stage were to
facilitate wound healing, prevent deep vein thrombosis in the lower
limbs and restore joint mobility, in preparation for prosthesis
fitting. The particular training approach included isometric
contractions of the gluteal and anterior muscles on the affected
side, as well as active and passive dorsiflexion and plantarflexion
exercises of the knee (ankle) joint on the affected side. The
exercises were carried out under pain-free conditions. The patient
was instructed to perform isometric contractions of the gluteal and
anterior muscles in the supine position. Each contraction lasted
for 5–10 sec, with a 3-sec rest interval between each one. A total
of three sets of 20 repetitions were completed, with a 1-min rest
between each set. In terms of knee (ankle) joint mobility training,
each repetition consisted of a single cycle of 3 sec of
dorsiflexion and plantarflexion, with a 1-sec rest interval between
each cycle. A total of three sets of 20 repetitions were completed,
with a 1-min rest between each set.
In the second stage, 4 weeks to 3 months after
surgery, the objective was to enhance the muscle strength, balance
and coordination of the patient. The training regimen included
progressive resistance training of the anterior muscle group and
weight-shifting exercises. During progressive resistance training
of the affected lower limb, the patient was placed in a supine
position on the bed, actively lifting the affected leg to a
position 30° above the bed surface. The therapist applied
appropriate resistance at the end of the affected limb, holding the
position for 5–10 sec, with a 3-sec rest between each repetition. A
total of three sets of 10 repetitions were completed, with a 1-min
rest between each set. The patient used an assistive device to
facilitate standing and perform weight-shifting training. In
addition, the patient was instructed to maintain a shoulder-width
stance with eyes fixed straight ahead. Each patient was then asked
to shift their weight to the healthy side, followed by the affected
side, while ensuring that they remained pain-free. During the
training session, the patient had to maintain an upright upper body
position, thus preventing lateral bending of the trunk and heel
lift. A total of three sets of 40 repetitions were completed, with
a 1-min rest interval between each set.
In the third stage, which lasted from the fourth to
the sixth month following surgery, the patients underwent
additional gait and stair climbing training, based on the second
stage training, to restore the basic lower limb function, which was
required for daily activities. The gait training program included
the stance phase, the swing phase and the simulation of daily life
scenarios. The stance phase training progressed from bilateral hand
support with handrails to single hand support on the unaffected
side and subsequently to a no support state. The swing phase of
gait training was primarily associated with the experience of
changes in body weight during walking. The training program
included simulated daily life scenarios, including uphill and
downhill training. Additionally, the patient utilized a
stair-climbing trainer for ascending and descending stairs. Prior
to commencing the training program, the stair handrails were
adjusted to a height that was suitable for the patient.
Furthermore, the principle of stepping up with the unaffected limb
first and then stepping down with the affected limb was
applied.
Evaluation indicators
To assess the range of motion (ROM) of the knee
(ankle) joint, the patient was instructed to assume a supine
position and then flex and extend the knee (ankle) joint as far as
possible to the maximum angle. The ROM of the knee (ankle) joint
was then measured with a manual articular goniometer (13).
The maximal strength of the anterior muscle groups
was quantified using the manual muscle test. For this, the patients
were seated and instructed to extend the knee (ankle) joint, either
with or without gravity, or against an increasing resistance force
applied by a physiotherapist. A scale ranging from 0 (no muscular
contraction) to 5 (full range of motion against manually applied
resistance force) was employed to assess the level of muscular
contraction (14).
Furthermore, the Musculoskeletal Tumor Society
scoring system, including six distinct parameters, was employed to
assess patient outcomes. These parameters included limb pain,
active function, psychological endurance, bracing, walking and
gait. Each parameter was graded on a scale of 0–5 points, with
higher scores indicating better limb recovery (15). In addition, to evaluate the degree
of autonomy acquired and perceived in daily life, the Toronto
Extremity Salvage Score was employed. The score comprises 30 items,
with each parameter rated on a scale ranging from 0 to 5 points. A
higher score indicates a greater level of autonomy (16).
The 6-min walk test was applied to assess walking
endurance. Patients were requested to walk as far as possible at
their preferred speed for 6 min, and the walking distance was then
recorded and measured (17). Motor
performance was evaluated using the timed up and go test, which
records the time taken for the patient to stand up, walk for 3
meters, turn around, return to the starting position and sit down
again (18).
Finally, the quality of life was evaluated utilizing
the 36-item Short Form Health Survey score, which incorporates the
following eight distinct parameters: Physical functioning,
role-physical (RP), bodily pain, general health, vitality, social
functioning, role-emotional and mental health. The assessment
yielded scores for the physical and mental functions of the
patients, with a higher score indicating superior overall health
and quality of life (19).
Literature search and selection
A systematic search of the Medline (https://medline.nlm.nih.gov/), Scopus (http://www.scopus.com/), Embase (https://www.embase.com/) and Cochrane (https://www.cochranelibrary.com/) databases was
conducted until 31 March, 2024, to identify eligible studies. The
objective was to ascertain the functional rehabilitation outcomes
associated with rotationplasty. The search algorithm comprised the
following terms: ‘rehabilitation’, ‘quality of life’, ‘malignant
bone tumors’, ‘limb salvage’ and ‘rotationplasty’. The titles and
abstracts of articles were screened by two independent
investigators, and potentially eligible reports were sought for
retrieval and full-text assessment. In the event of a discrepancy
between the two investigators regarding eligibility, a third
investigator would be consulted to evaluate the article in
question. The inclusion criteria comprised patients who had
undergone rotationplasty subsequent to the resection of a lower
limb tumor and those who had undergone an evaluation of functional
or quality of life. Conversely, articles were excluded if lower
limb tumors were not cited as the indication for rotationplasty, if
studies did not present findings from assessments of functional or
quality of life, and if they were in languages other than
English.
Statistical analysis
The statistical analysis was conducted using IBM
SPSS Statistics v.21 (IBM Corp.). The numerical data are expressed
as the mean ± standard deviation, while categorical data are
expressed as proportions or percentages. To assess the linear trend
relationship between time variables and functional outcomes and
quality of life, a P-value was utilized. Parametric data were
analyzed using repeated measures ANOVA to assess differences among
multiple groups. In the event of a significant difference between
groups, pairwise comparisons were conducted using Bonferroni's post
hoc test. Non-parametric data were evaluated across groups using
the Friedman test, and in case of significant differences, pairwise
comparisons were performed using Nemenyi's post hoc test. P<0.05
was considered to indicate a statistically significant
difference.
Results
The baseline data and clinical characteristics of
the patients included in the present study are listed in Table I. All patients underwent
rotationplasty due to tumor pathology. The extent of resection of
the limb segment that contained the tumor ranged from 12 to 20 cm
(mean, 16.5±2.32 cm), with the knee (ankle) joint extension length
ranging from 3–8 cm (mean, 4.92±1.62 cm). The follow-up period
ranged from 60–120 months (mean, 89.83±17.55 months). A patient
with a case of non-union (8%) showed healing after 1 month of
dressing changes. Another 2 cases of calluses and ulceration (17%)
exhibited improvement after 1 month of physiotherapy and prosthetic
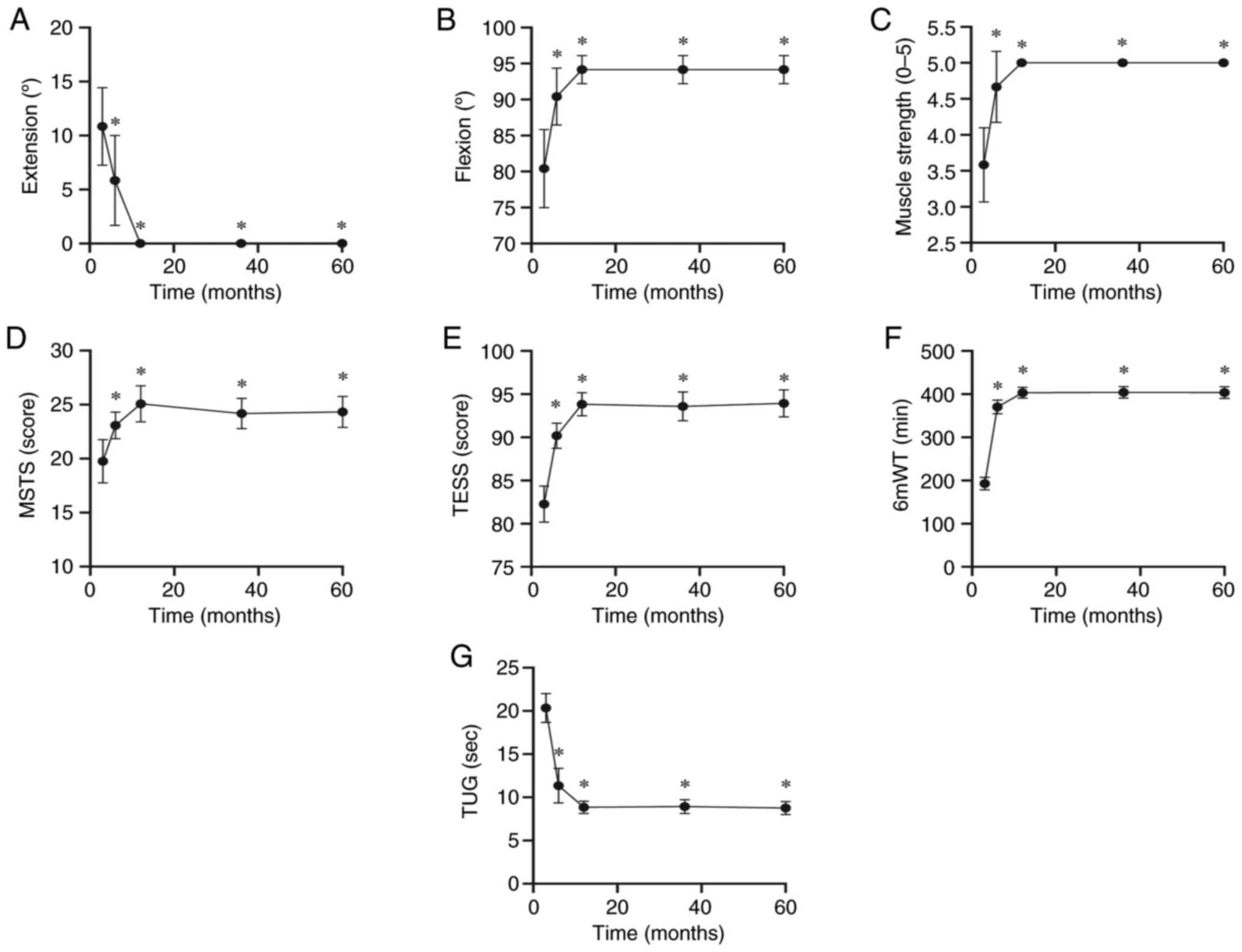
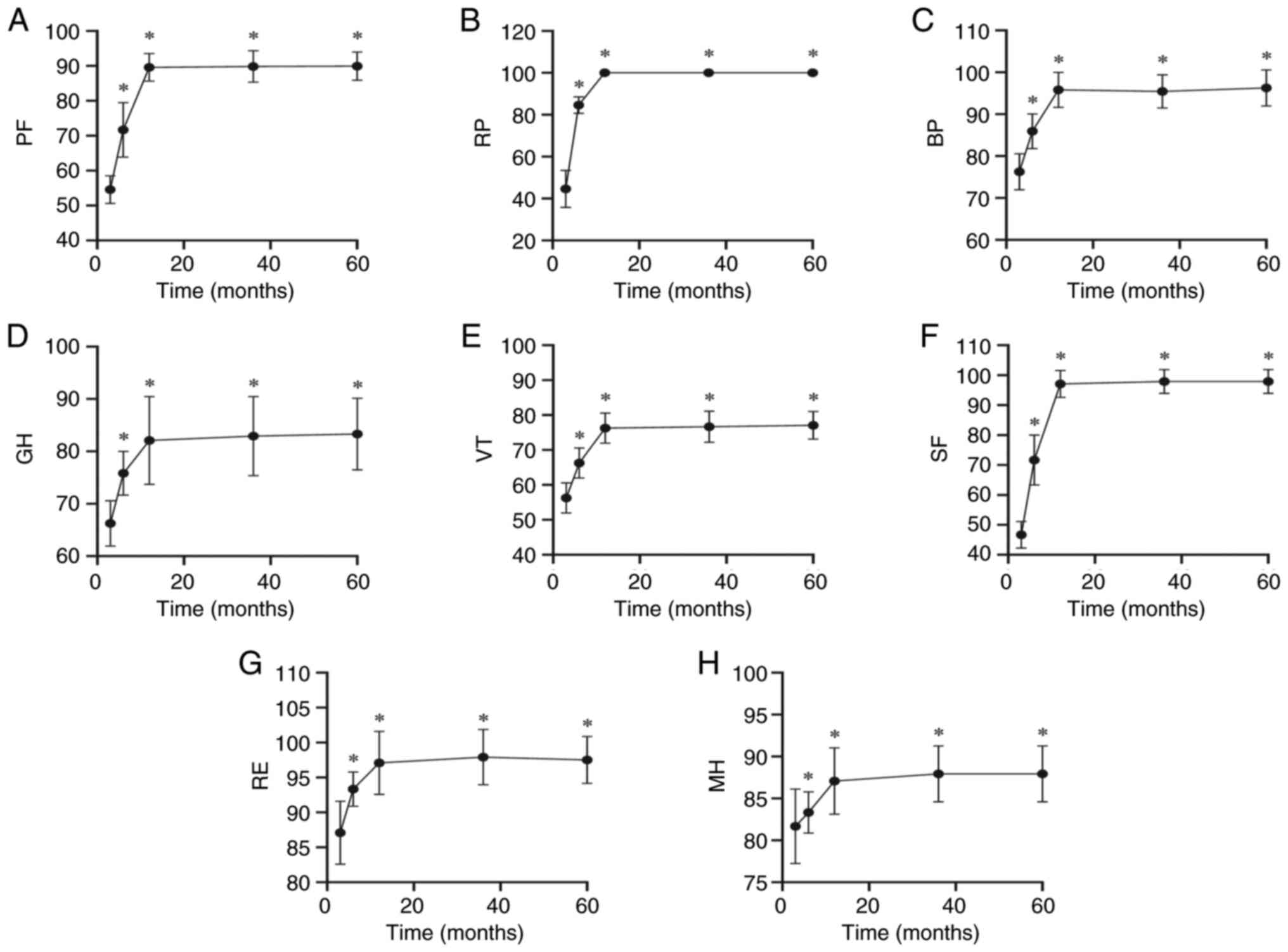
adjustments. Figs. 3 and 4 depict the postoperative functional
recovery and quality of life of the patients. At 1 year
post-surgery, there was a significant improvement in limb function
and quality of life (P<0.05), which remained stable thereafter
(Tables II and III). Post hoc testing revealed no
statistically significant differences in limb function and quality
of life between the groups at 12 months, 3 years and 5 years
postoperatively. A comparative analysis of several literature
sources indicated that rehabilitation could play an important role
in the functional recovery and quality of life of patients
following rotationplasty (Tables
IV and V). The results of the
present study also demonstrated that the functional outcomes of
patients at 1 year post-surgery were superior to those reported in
previous studies, particularly in terms of knee (ankle) joint
mobility and muscle strength recovery. At 1-year postoperatively,
the mean score for each indicator of the quality-of-life scores of
the patients was 91, representing a greater improvement than the 78
reported in the literature during the same period. Furthermore, the
patients' PF scores at 1-year postoperatively were higher than
those in all other studies.
 | Table I.Demographic characteristics of
participants (n=12). |
Table I.
Demographic characteristics of
participants (n=12).
| Characteristic | Value |
|---|
| Age,
yearsa | 6.58±1.73 |
| Sex, n (%) |
|
|
Male | 7 (58.33) |
|
Female | 5 (41.67) |
| Course of disease,
monthsa | 4.50±0.67 |
| Pathology, n
(%) |
|
|
Osteoblastic osteosarcoma | 4 (33.33) |
|
Chondroblastic
osteosarcoma | 2 (16.67) |
| Mixed
osteosarcoma | 3 (25.00) |
| Ewing's
sarcoma | 3 (25.00) |
| Length of tumor
resection, cma | 16.5±2.32 |
| Extension length of
knee (ankle) joint, cma | 4.92±1.62 |
| Follow-up time,
monthsa | 89.83±17.55 |
| Complications, n
(%) |
|
|
Unhealed wound | 1 (8.33) |
|
Calluses and ulceration | 2 (16.67) |
 | Table II.Functional outcomes of patients after
rotationplasty. |
Table II.
Functional outcomes of patients after
rotationplasty.
|
| Follow-up time
post-surgery |
|
| 95% Confidence
interval |
|---|
|
|
|
|
|
|
|---|
| Functional
indicators | 3 months | 6 months | 12 months | 3 years | 5 years | F-value | P-value | Minimum | Maximum |
|---|
| Knee (ankle) joint
extension, ° | 10.83 (3.95) | 5.83 (4.17) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 71.53 | <0.001 | −0.16 | −0.10 |
| Knee (ankle) joint
Flexion, ° | 80.42 (5.42) | 90.42 (3.96) | 94.17 (1.95) | 94.17 (1.95) | 94.17 (1.95) | 62.65 | <0.001 | 0.07 | 0.12 |
| Muscle strength
(0–5) | 3.58 (0.51) | 4.67 (0.49) | 5.00 (0.00) | 5.00 (0.00) | 5.00 (0.00) | 38.91 | <0.001 | 4.17 | 4.67 |
| MSTS score | 19.75 (2.01) | 23.08 (1.24) | 25.08 (1.68) | 24.17 (1.40) | 24.33 (1.44) | 60.67 | <0.001 | 0.18 | 0.30 |
| TESS score | 82.25 (2.09) | 90.17 (1.47) | 93.83 (1.34) | 93.58 (1.68) | 93.92 (1.56) | 214.33 | <0.001 | 0.13 | 0.17 |
| 6mWT, meters | 192.92 (14.68) | 370.08 (15.97) | 403.08 (12.52) | 403.75 (13.44) | 403.50 (13.31) | 733.28 | <0.001 | 290.01 | 354.05 |
| TUG, sec | 20.33 (1.67) | 11.33 (2.02) | 8.83 (0.72) | 8.92 (0.79) | 8.75 (0.75) | 178.85 | <0.001 | 11.73 | 15.27 |
 | Table III.Quality of life of patients after
rotationplasty. |
Table III.
Quality of life of patients after
rotationplasty.
|
| Follow-up time
post-surgery |
|
| 95% Confidence
interval |
|---|
|
|
|
|
|
|
|---|
| SF-36 | 3 months | 6 months | 12 months | 3 years | 5 years | F-value | P-value | Minimum | Maximum |
|---|
| Physical
health |
|
|
|
|
|
|
|
|
|
| PF | 54.58 (3.96) | 71.67 (7.78) | 89.58 (3.96) | 89.83 (4.51) | 89.92 (4.08) | 119.80 | <0.001 | 66.71 | 77.17 |
| RP | 84.58 (8.91) | 84.58 (3.96) | 100.00 (0.00) | 100.00 (0.00) | 100.00 (0.00) | 309.78 | <0.001 | 68.16 | 84.61 |
| BP | 76.25 (4.33) | 85.92 (4.17) | 95.83 (4.17) | 95.42 (3.96) | 96.25 (4.33) | 64.48 | <0.001 | 82.93 | 89.07 |
| GH | 66.25 (4.33) | 75.83 (4.17) | 82.08 (8.38) | 82.92 (7.53) | 83.33 (6.85) | 21.51 | <0.001 | 71.75 | 77.69 |
| Mental health |
|
|
|
|
|
|
|
|
|
| VT | 56.25 (4.33) | 66.25 (4.33) | 76.25 (4.33) | 76.67 (4.44) | 77.08 (3.96) | 64.00 | <0.001 | 63.11 | 69.39 |
| SF | 46.67 (4.44) | 71.67 (8.35) | 97.08 (4.50) | 97.92 (3.96) | 97.50 (3.37) | 208.62 | <0.001 | 64.47 | 79.14 |
| RE | 87.08 (4.50) | 93.33 (2.46) | 97.92 (3.96) | 89.83 (4.51) | 89.92 (4.08) | 25.32 | <0.001 | 90.82 | 94.74 |
| MH | 81.67 (4.44) | 83.33 (2.46) | 87.08 (3.96) | 87.97 (3.34) | 87.92 (3.34) | 6.68 | <0.001 | 82.58 | 85.48 |
 | Table IV.Literature review of functional
outcomes following rotationplasty. |
Table IV.
Literature review of functional
outcomes following rotationplasty.
| First author,
year | No. of
patients | Mean age,
years | Mean follow-up,
years | Rehabilitation
type | Knee (ankle) joint
ROM, ° | Muscle strength
(0–5) | MSTS score | TESS | 6mWT, meters | TUG, sec | (Refs.) |
|---|
| Winkelmann,
2000 | 8 | 5.9 | 5.3 | Physiotherapy | 0-80 | Not available | 22.5 | Not available | Not available | Not available | (29) |
| Hahn et al,
2003 | 26 | 21.4 | 4.8 | Not available | −11-80 | Not available | Not available | Not available | Not available | Not available | (31) |
| Hopyan et
al, 2006 | 5 | 10.4 | 8.6 | Not available | Not available | Not available | 20.1 | 88.9 | Not available | Not available | (30) |
| Ginsberg et
al, 2007 | 4 | 14.5 | 4.3 | Not available | Not available | Not available | 27.5 | 95.6 | Not available | 5.6 | (32) |
| Bekkering et
al, 2012 | 7 | 14.9 | 2.0 | Not available | Not available | Not available | Not available | 85.0 | 430.0 | Not available | (28) |
| Gradl et al,
2015 | 12 | 19.0 | 14.0 | Not available | Not available | Not available | 19.2 | Not available | Not available | Not available | (33) |
| Morri and Forni,
2017 | 1 | 31.0 | 1.0 | Physiotherapy | 0-95 | 4.5 | 24.0 | 87.0 | 365.0 | 7.7 | (10) |
| Benedetti et
al, 2016 | 25 | 9.3 | 15.0 | Not available | Not available | Not available | 24.0 | Not available | Not available | Not available | (34) |
| Gulia et al,
2023 | 14 | 24.0 | 11.1 | Active and passive
ankle joint activity training and crutch walking | Not available | Not available | 26.0 | Not available | Not available | Not available | (23) |
| Grimsrud et
al, 2020 | 8 | 11.6 | 18.4 | Not available | Not available | Not available | 19.6 | 90.0 | Not available | Not available | (37) |
 | Table V.Literature review of 36-item Short
Form Health Survey scores following rotationplasty. |
Table V.
Literature review of 36-item Short
Form Health Survey scores following rotationplasty.
| First author,
year | No. of
patients | Mean age,
years | Mean follow-up,
years | Rehabilitation
type | Physical
health | Mental health |
|
|---|
|
|
|
|---|
| PF | RP | BP | GH | VT | SF | RE | MH | (Refs.) |
|---|
| Forni et al,
2012 | 20 | 26.9 | 17.2 | Not available | 89.3 | 81.3 | 88.2 | 83.6 | 71.8 | 81.2 | 83.3 | 80.8 | (36) |
| Harris et
al, 2013 | 1 | 10.0 | 3.0 | Progressive
weight-bearing, basketball and shooting | 85.0 | 100.0 | 100.0 | 85.0 | 80.0 | 100.0 | 100.0 | 84.0 | (35) |
| Gradl et al,
2015 | 12 | 19.0 | 14.0 | Not available | 80.4 | 78.1 | 74.1 | 71.8 | 75.0 | 98.9 | 88.2 | 89.6 | (33) |
| Morri and Forni,
2017 | 1 | 31.0 | 1.0 | Physiotherapy | 60.0 | 50.0 | 100.0 | 76.0 | 80.0 | 75.0 | 100.0 | 84.0 | (10) |
| Grimsrud et
al, 2020 | 8 | 11.6 | 18.4 | Not available | 45.1 | 51.8 | 50.1 | 48.3 | 49.9 | 53.1 | 55.3 | 53.3 | (37) |
Discussion
It has been reported that rotationplasty exhibits
better gait outcomes compared with above-knee amputation or knee
joint replacement for patients with malignant bone tumors of the
knee, since these patients can even run and climb stairs after
surgery. More particularly, young patients with bone tumors of the
knee who undergo rotationplasty can have almost normal lower limb
function after the procedure, thus showing higher satisfaction
rates (20,21). Currently, rotationplasty is commonly
considered as an alternative to above-knee amputation for pediatric
and infant knee joint malignant tumors (22–24). A
previous study also demonstrated that patients who received
rotationplasty could participate in high-level sports (25). Due to the complexity and seriousness
of bone tumors, postoperative rehabilitation faces enormous
challenges. One of the main rehabilitation tasks in the field is
managing patient expectations. The present study provided a
detailed description of a postoperative rehabilitation strategy and
evaluated the long-term functional outcomes and quality of life of
patients after rotationplasty. To address the expectations and
concerns of patients and their families, the present study aimed to
establish a rehabilitation guidance strategy for the postoperative
functional recovery of patients and depict a timeline of functional
changes.
Abdelgawad et al (26) suggested that knee joint amputation
could result in extensive bone and muscle structure loss, thus
leading to significant sensory-motor shock, which could in turn
affect neurological motor control and balance function. In the
present study, the postoperative rehabilitation process consisted
of three stages. Training content and difficulty were gradually
increased based on the postoperative physical rehabilitation of the
patient, until their limb function reached optimal levels. After
the patient regained consciousness, the status of the affected
foot's nervous system, skin color and pulse was examined. At the
same time, early muscle lengthening and pain-free training for knee
(ankle) joint mobility were performed to promote the establishment
of new neural pathways and restore foot sensory nervous systems.
The focus of early rehabilitation for patients is to adapt to the
new knee (ankle) joint and the replacement of its function by the
rotated ankle joint. Additionally, it also aims to restore the
patient's proprioception and enhance the strength of the affected
foot's sole muscles. Therefore, training methods should be gentle
and slow, and not affect wound healing or cause damage. Gait
training simulates daily life scenarios, thus enhancing the ability
of the patient to perform daily activities and improving their
quality of life. Stability of the pelvis and knee (ankle) joint is
very important when walking (27).
During initial tissue healing, particularly within 3 months
postoperatively, walker-assisted standing rehabilitation training
was carried out to improve the stability of the pelvis and knee
(ankle) joint.
Consistent with the results of the present study,
previous studies indicated that patients who underwent
rotationplasty displayed good lower limb function (28–34)
and a higher quality of life (35–37).
However, the present study found that patients could achieve
similar functional outcomes at 6 months after surgery compared with
the reported results found at 1 year after surgery in a previous
study (9). In the present study, at
1 year postoperatively, the functional outcome of the patients was
superior compared with that observed in other studies, particularly
in terms of the knee (ankle) mobility and muscle strength recovery,
which reached near-normal levels. The quality-of-life scores at 1
year postoperatively were also higher compared with those reported
in previous studies. Furthermore, the patients exhibited a high
degree of acceptance of their physical appearance, with a mean RP
score of 100, indicating a high level of satisfaction. Therefore,
early rehabilitation is necessary and formulating appropriate
rehabilitation programs for patients can promote the effective and
rapid recovery of the lower limb function. Importantly, the results
also demonstrated that lower limb function and quality of life
improved rapidly in the early postoperative period, while no
statistically significant differences were observed at all time
points after ~1 year post-surgery.
Different tumor types, chemotherapy protocols and
the patient health status exhibit significant effects on the
outcomes of rehabilitation. Different types of tumors are
characterized by different growth patterns, metastatic tendencies
and prognoses. Therefore, the rehabilitation process should also
take into account the effect of these factors and match the
clinical treatment to them (38).
Chemotherapy is commonly associated with the occurrence of several
adverse effects, such as nausea, vomiting and fatigue. These
effects can negatively affect both the physical and psychological
well-being of patients. It is crucial to implement appropriate
strategies to minimize the impact of these side effects on the
overall well-being and quality of life of affected patients
(39). Furthermore, the basic
health status and immune function of the patient are vital factors
that can affect rehabilitation outcomes (40). In order to guarantee the most
favorable outcomes, the duration of muscle contraction was
calibrated to the patient's level of discomfort and their actual
condition throughout the rehabilitation process. This
individualized approach enabled the creation of a personalized
rehabilitation program for each patient. In the current study, the
variability and complexity of tumor rehabilitation were considered
as significant challenges and key areas of focus.
In summary, rotationplasty is an effective surgical
method for treating malignant bone tumors of the lower limb, thus
preserving lower limb function and improving the quality of life
for patients. Therefore, rotationplasty deserves to be established
in clinical practice. Rehabilitation strategies should be
individualized based on the patient's actual condition, and the
early selection of the appropriate rehabilitation strategy is of
great significance. The longitudinal evaluation of postoperative
functional outcomes could assist clinical physicians to analyze the
results obtained, and provide more effective guidance and
management for patients undergoing postoperative
rehabilitation.
Functional rehabilitation following rotationplasty
has a profound effect on clinical practice. Rehabilitation not only
improves physical function recovery and quality of life, but also
assists patients in reintegrating into social life and the
workplace, and reduces social isolation and disease-induced
psychological issues (41,42). However, future studies should
prioritize the exploration of personalized rehabilitation protocols
that consider patient-specific individual differences.
Additionally, further research is needed on the development of
innovative rehabilitation techniques and strategies for long-term
rehabilitation and relapse prevention. These efforts could
ultimately contribute to the establishment of an evidence-based
guideline for rehabilitation after rotationplasty, eventually
improving rehabilitation outcomes and quality of life.
Although the present study yielded valuable
findings, it is important to acknowledge that several limitations
could affect the interpretation of the results. The rarity of
rotationplasty has resulted in a scarcity of literature on the
subject. In the previous literature, few studies have described
specific rehabilitation methods, making it difficult to
systematically and accurately compare the methodology of this study
with others. A total of 12 participants were included in the
present study, each with a satisfactory outcome. However, to verify
the reliability of the results, a larger sample size is needed.
Therefore, future studies with a larger sample size should be
carried out for a more comprehensive investigation of the 5-year
survival and cure rates, thus verifying the results of the current
study. Given the significant heterogeneity among patients with
tumors, further research is needed to comprehensively explore and
understand these confounding factors in greater detail. This could
help to improve patient outcomes and quality of life.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural Science
Foundation of China (grant no. H0911-82071413).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
ND and XZ contributed to conception and data
collection. ND, JD and JY designed and conducted the study. ND, MX
and YS analyzed and interpreted the data, and wrote the manuscript.
ND, XZ, JD, JY, MX and YS confirm the authenticity of all the raw
data. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
This retrospective study was approved by the
Institutional Review Board of the Fourth Medical Center of the
Chinese People's Liberation Army General Hospital (approval no.
2023KY037-KS001; Beijing, China). All patients and their duly
authorized representatives provided written informed consent to
participate in the study. All methods were performed in accordance
with relevant guidelines and regulations.
Patient consent for publication
All patients and their duly authorized
representatives provided written informed consent for the study to
be published.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Borggreve, . Kniegelenksersatz durch das
in der Beinlängsachse um 180° gedrehte Fußgelenk. Arch Orthop
Unfallchir. 28:175–178. 1930. View Article : Google Scholar
|
|
2
|
Kristen H, Knahr K and Salzer M: Atypical
amputations of bone tumors of the lower extremity (author's
transl). Arch Orthop Unfallchir. 83:91–107. 1975.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hillmann A, Gosheger G, Hoffmann C, Ozaki
T and Winkelmann W: Rotationplasty-surgical treatment modality
after failed limb salvage procedure. Arch Orthop Trauma Surg.
120:555–558. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Deloge C, Allington N and Rondia J:
Rotationplasty as an alternative to amputation. Rev Med Liege.
76:262–267. 2021.(In French). PubMed/NCBI
|
|
5
|
Ding WZ, Liu K, Li Z and Chen SR: A
meta-analysis of prognostic factors of osteosarcoma. Eur Rev Med
Pharmacol Sci. 24:4103–4112. 2020.PubMed/NCBI
|
|
6
|
Panez-Toro I, Muñoz-García J,
Vargas-Franco JW, Renodon-Cornière A, Heymann MF, Lézot F and
Heymann D: Advances in osteosarcoma. Curr Osteoporos Rep.
21:330–343. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huynh THN, Kuruvilla DR, Nester MD,
Zervoudakis G, Letson GD, Joyce DM, Binitie OT and Lazarides AL:
Limb amputations in cancer: Modern perspectives, outcomes, and
alternatives. Curr Oncol Rep. 25:1457–1465. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen ZX, Guo XW, Hong HS, Zhang C, Xie W,
Sha M and Ding ZQ: Rotationplasty type BIIIb as an effective
alternative to limb salvage procedure in adults: Two case reports.
World J Clin Cases. 11:6877–6888. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Benedetti MG, Coli M, Campanacci L and
Manfrini M: Postural control skills, proprioception, and risk of
fall in long-term survivor patients treated with knee
rotationplasty. Int J Rehabil Res. 42:68–73. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morri M and Forni C: Rotationplasty in
adult cancer patients: What is the rehab strategy and what results
can be expected? A case study. Prosthet Orthot Int. 41:517–521.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Enneking WF, Spanier SS and Goodman MA: A
system for the surgical staging of musculoskeletal sarcoma. Clin
Orthop Relat Res. 153:106–120. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Huang J, Cheng J, Bi W, Xu M, Jia J, Han G
and Wang W: Neoadjuvant Chemotherapy and expandable prosthesis
reconstruction to treat osteosarcoma around the knee in children.
Orthop Surg. 15:162–168. 2023. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kinoshita H, Yonemoto T, Kamoda H,
Hagiwara Y, Tsukanishi T, Inoue M, Terakawa F, Ohtori S and Ishii
T: Effectiveness of salvage knee rotationplasty on sarcoma around
the knee in adolescents and young adults. Anticancer Res.
41:1041–1046. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bittmann FN, Dech S, Aehle M and Schaefer
LV: Manual muscle testing-force profiles and their reproducibility.
Diagnostics (Basel). 10:9962020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Enneking WF, Dunham W, Gebhardt MC,
Malawar M and Pritchard DJ: A system for the functional evaluation
of reconstructive procedures after surgical treatment of tumors of
the musculoskeletal system. Clin Orthop Relat Res. 286:241–246.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Davis AM, Wright JG, Williams JI,
Bombardier C, Griffin A and Bell RS: Development of a measure of
physical function for patients with bone and soft tissue sarcoma.
Qual Life Res. 5:508–516. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Agarwala P and Salzman SH: Six-minute walk
test: Clinical role, technique, coding, and reimbursement. Chest.
157:603–611. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hendriks S, Huisman MG, Ghignone F, Vigano
A, de Liguori Carino N, Farinella E, Girocchi R, Audisio RA, van
Munster B, de Bock GH and van Leeuwen BL: Timed up and go test and
long-term survival in older adults after oncologic surgery. BMC
Geriatr. 22:9342022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ware JE Jr and Sherbourne CD: The MOS
36-item short-form health survey (SF-36). I. Conceptual framework
and item selection. Med Care. 30:473–483. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Benedetti MG, Tarricone I, Monti M,
Campanacci L, Regazzi MG, De Matteis T, Platano D and Manfrini M:
Psychological well-being, self-esteem, quality of life and gender
differences as determinants of post-traumatic growth in long-term
knee rotationplasty survivors: A cohort study. Children (Basel).
10:8672023.PubMed/NCBI
|
|
21
|
Floccari LV, Jeans KA, Herring JA,
Johnston CE and Karol LA: Comparison of outcomes by reconstructive
strategy in patients with prostheses for proximal femoral focal
deficiency. J Bone Joint Surg Am. 103:1817–1825. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gotta J, Bielack S, Hecker-Nolting S, Sorg
B, Kevric M, Salzmann-Manrique E and Klingebiel T: When your ankle
becomes a knee-long-term functional outcome and quality of life
with a rotationplasty after resection of malignant limb tumors.
Klin Padiatr. 234:154–162. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gulia A, Prajapati A, Gupta S, Exner U and
Puri A: Rotationplasty after failed limb salvage: An alternative to
amputation. Eur J Orthop Surg Traumatol. 33:1683–1689. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fukushima T, Okita Y, Watanabe N, Yokota
S, Nakano J, Tanaka Y and Kawai A: Progress in muscle strength of
the reconstructed knee and quality of life of the patient after
knee rotationplasty: A case report. Prosthet Orthot Int.
47:651–654. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hillmann A, Weist R, Fromme A, Völker K
and Rosenbaum D: Sports activities and endurance capacity of bone
tumor patients after rotationplasty. Arch Phys Med Rehabil.
88:885–890. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Abdelgawad MA, Parambi DGT, Ghoneim MM,
Alotaibi NH, Alzarea AI, Hassan AH and Abdelrahim MEA: A
meta-analysis comparing efficiency of limb-salvage surgery vs
amputation on patients with osteosarcoma treated with neoadjuvant
chemotherapy. Int Wound J. 19:1616–1624. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Filis P, Varvarousis D, Ntritsos G,
Dimopoulos D, Filis N, Giannakeas N, Korompilias A and Ploumis A:
Rotationplasty outcomes assessed by gait analysis following
resection of lower extremity bone neoplasms. Bone Jt Open.
4:817–824. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bekkering WP, Vliet Vlieland TP, Koopman
HM, Schaap GR, Beishuizen A, Anninga JK, Wolterbeek R, Nelissen RG
and Taminiau AH: A prospective study on quality of life and
functional outcome in children and adolescents after malignant bone
tumor surgery. Pediatr Blood Cancer. 58:978–985. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Winkelmann WW: Type-B-IIIa hip
rotationplasty: An alternative operation for the treatment of
malignant tumors of the femur in early childhood. J Bone Joint Surg
Am. 82:814–828. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hopyan S, Tan JW, Graham HK and Torode IP:
Function and upright time following limb salvage, amputation, and
rotationplasty for pediatric sarcoma of bone. J Pediatr Orthop.
26:405–408. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hahn SB, Park HJ, Kim HS, Kim SH and Shin
KH: Surgical treatment of malignant and aggressive bone tumors
around the knee by segmental resection and rotationplasty. Yonsei
Med J. 44:485–492. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ginsberg JP, Rai SN, Carlson CA, Meadows
AT, Hinds PS, Spearing EM, Zhang L, Callaway L, Neel MD, Rao BN and
Marchese VG: A comparative analysis of functional outcomes in
adolescents and young adults with lower-extremity bone sarcoma.
Pediatr Blood Cancer. 49:964–969. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Gradl G, Postl LK, Lenze U,
Stolberg-Stolberg J, Pohlig F, Rechl H, Schmitt-Sody M, von
Eisenhart-Rothe R and Kirchhoff C: Long-term functional outcome and
quality of life following rotationplasty for treatment of malignant
tumors. BMC Musculoskelet Disord. 16:2622015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Benedetti MG, Okita Y, Recubini E, Mariani
E, Leardini A and Manfrini M: How much clinical and functional
impairment do children treated with knee rotationplasty experience
in adulthood? Clin Orthop Relat Res. 474:995–1004. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Harris JD, Trinh TQ, Scharschmidt TJ and
Mayerson JL: Exceptional functional recovery and return to
high-impact sports after Van Nes rotationplasty. Orthopedics.
36:e126–e131. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Forni C, Gaudenzi N, Zoli M, Manfrini M,
Benedetti MG, Pignotti E and Chiari PE: Living with
rotationplasty-quality of life in rotationplasty patients from
childhood to adulthood. J Surg Oncol. 105:331–336. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Grimsrud C, Killen C, Murphy M, Wang H and
McGarry S: Long-term outcomes of rotationplasty patients in the
treatment of lower extremity sarcomas with cost analysis. J Clin
Orthop Trauma. 11 (Suppl 1):S149–S152. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Taefehshokr S, Parhizkar A, Hayati S,
Mousapour M, Mahmoudpour A, Eleid L, Rahmanpour D, Fattahi S,
Shabani H and Taefehshokr N: Cancer immunotherapy: Challenges and
limitations. Pathol Res Pract. 229:1537232022. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ouyang Z, Trent S, McCarthy C, Cosker T,
Stuart R, Pratap S, Whitwell D, White HB, Tao H, Guo X and Maxime
Gibbons CL: The incidence, risk factors and outcomes of wound
complications after preoperative radiotherapy and surgery for high
grade extremity soft tissue sarcomas: A 14-year retrospective
study. Eur J Surg Oncol. 49:1070862023. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Potiaumpai M, Schleicher EA, Wang M,
Campbell KL, Sturgeon K and Schmitz KH: Exercise during
chemotherapy: Friend or foe? Cancer Med. 12:10715–10724. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Heywood SE, Connaughton J, Kinsella R,
Black S, Bicchi N and Setchell J: Physical therapy and mental
health: A scoping review. Phys Ther. 102:pzac1022022. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Morales Rodríguez E, Lorenzo Calvo J,
Granado-Peinado M, Pérez-Bilbao T and San Juan AF: Effects of
exercise programs on psychoemotional and quality-of-life factors in
adult patients with cancer and hematopoietic stem cell
transplantation or bone marrow transplantation: A systematic
review. Int J Environ Res Public Health. 19:158962022. View Article : Google Scholar : PubMed/NCBI
|