Introduction
Breast cancer (BC) is a prevalent malignant disease
worldwide that mainly affects women (1). In the US, 30% of all new cancer cases
among women are related to BC; in 2021, there were an estimated
281,550 newly diagnosed cases and 43,600 deaths from BC (2). Male BC cases (MBCs) are rare; in the
US, they account for <1% of newly identified cases every year
(3). Most cases of BC and the
creation of new treatment options are directed towards female
patients with BC due to the extremely low prevalence of MBC.
According to additional estimates, 3.7 million women
in the US had BC in 2018 (4).
Patients with early-stage BC that has not metastasized have a
5-year survival rate of >90%; however, once metastatic tumours
have formed, the 5-year survival rate decreases to <20%
(5), and ~50% of those diagnosed
with BC will progress (6).
Although BC can spread to nearly every part of the
body, it most commonly metastasizes to the cerebral cortex, liver,
lymphatic system and bones (7).
Among the most common sites of solid malignant tumour metastases is
the liver. Globally, BC liver metastasis (BCLM) therapy is a major
concern, and there is no standardized treatment (8). The use of chemotherapy, immunotherapy
(for triple-negative disease), radiation, human epidermal growth
factor receptor 2 (HER-2)-targeted treatment, endocrine therapy and
palliative therapy are among the therapeutic options (9).
The present case report, a 55-year-old male patient
diagnosed with BCLM 5 years after BC surgery is described. The
present study aimed to assess the details of this MBC case and the
possible underlying mechanism. Through this case, we hope to
improve clinical understanding of BCLM and clinical experience and
treatment.
Case report
A 55-year-old male patient presented to Xuanc
Xuancheng Hospital Affiliated to Wannan Medical College (Xuancheng,
China) in September 2023 and complained of fever, sputum and
pressure in the chest for >10 days while coughing. The patient
was administered postoperative routine chemotherapy (doxorubicin
hydrochloride, cyclophosphamide, Docetaxel) after BC surgery 5
years ago. After BC surgery, the patient underwent breast
examination every year. The patient had no history of any other
significant illnesses. Upon examination, the right chest
auscultation breath sound was quiet, and the percussion sound was
loud. Besides the chest scars from the breast surgery, there were
no other notable physical examination results.
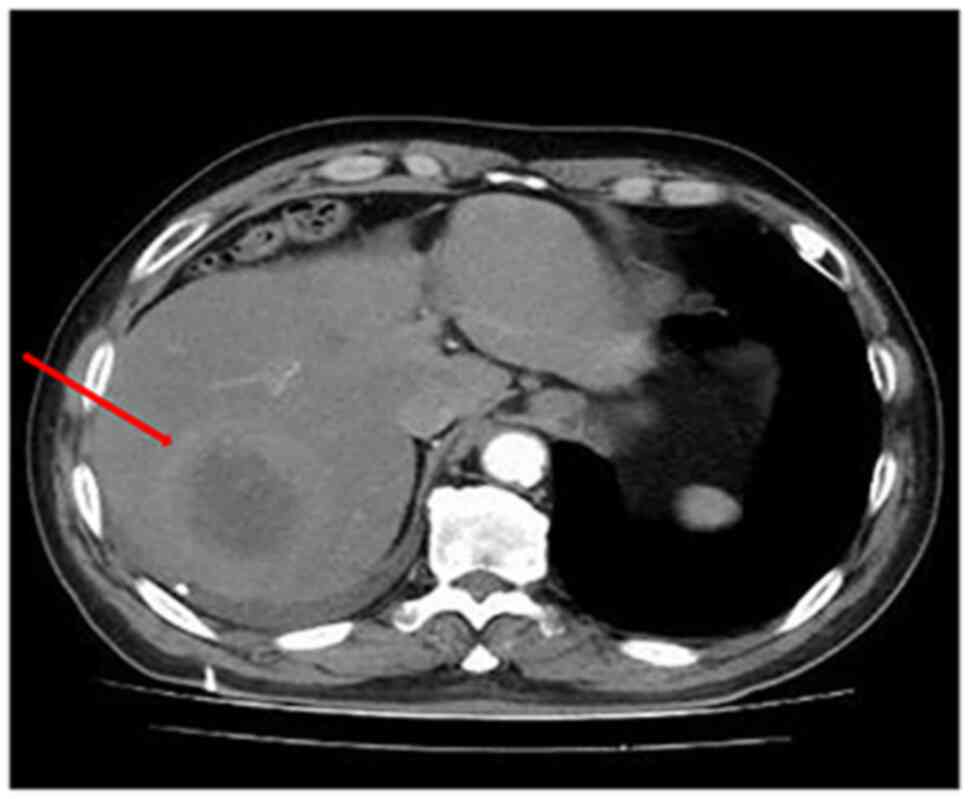
After patient admission, the CEA levels were
examined, which were elevated (9.34 µg/l; reference value, 0-0.5
µg/l). The other laboratory indicators showed no clinically
significant abnormalities. Chest CT scans revealed that the right
pleural effusion with expansion of the right lower lobe of the lung
was not complete, the upper abdominal enhanced CT-visible liver
density was not uniform and the liver had a mass (Fig. 1); therefore, further examination was
recommended. Bone and CT scans of the abdomen demonstrated no
notable abnormality.
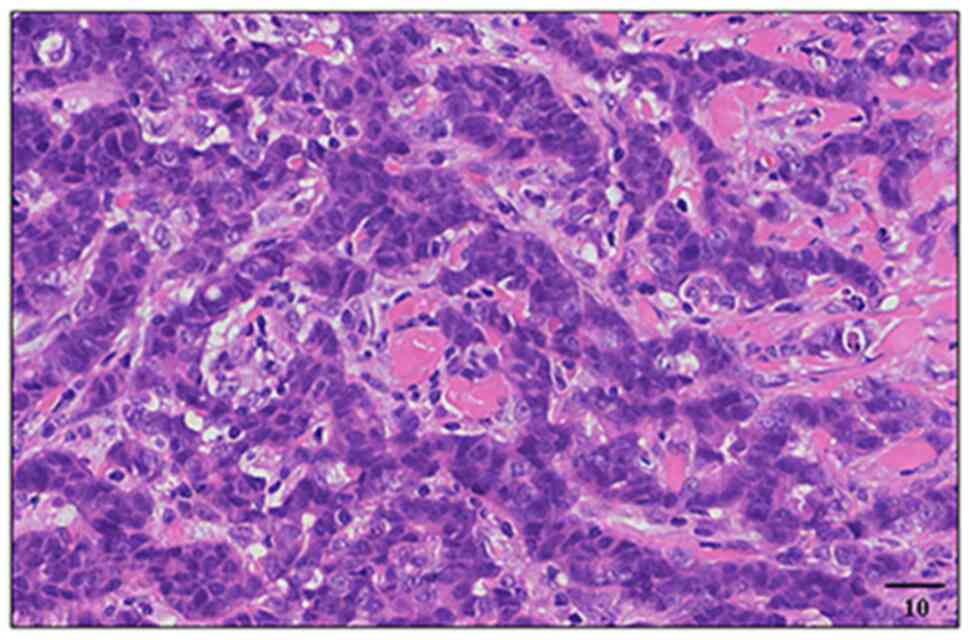
A coarse needle biopsy of the liver masses was
carried out under ultrasound guidance. Microscopically, invasive
tumour cells in the stroma were detected by haematoxylin-eosin
staining (Fig. 2). For 48 h, 4%
formalin-fixed at 4°C. Deparaffinization and a 10-min wash with
Xylene (Sigma-Aldrich; Merck KGaA). A two-minute wash cycle was
performed on 100% ethanol (AppliChem, Darmstadt), 100, 97, 70%
ethanol, and dH2O. Staining was performed for an hour at room
temperature using hematoxylin solution. Sections were so washed for
five minutes under running tap water. The slides were then rinsed
with water after being incubated with eosin for one minute at room
temperature. Digital images were captured by a light microscope and
analysed by Axio Vision Rel 4.8 software
(softadvice.informer.com/Axiovision_Rel_4.8_Software).
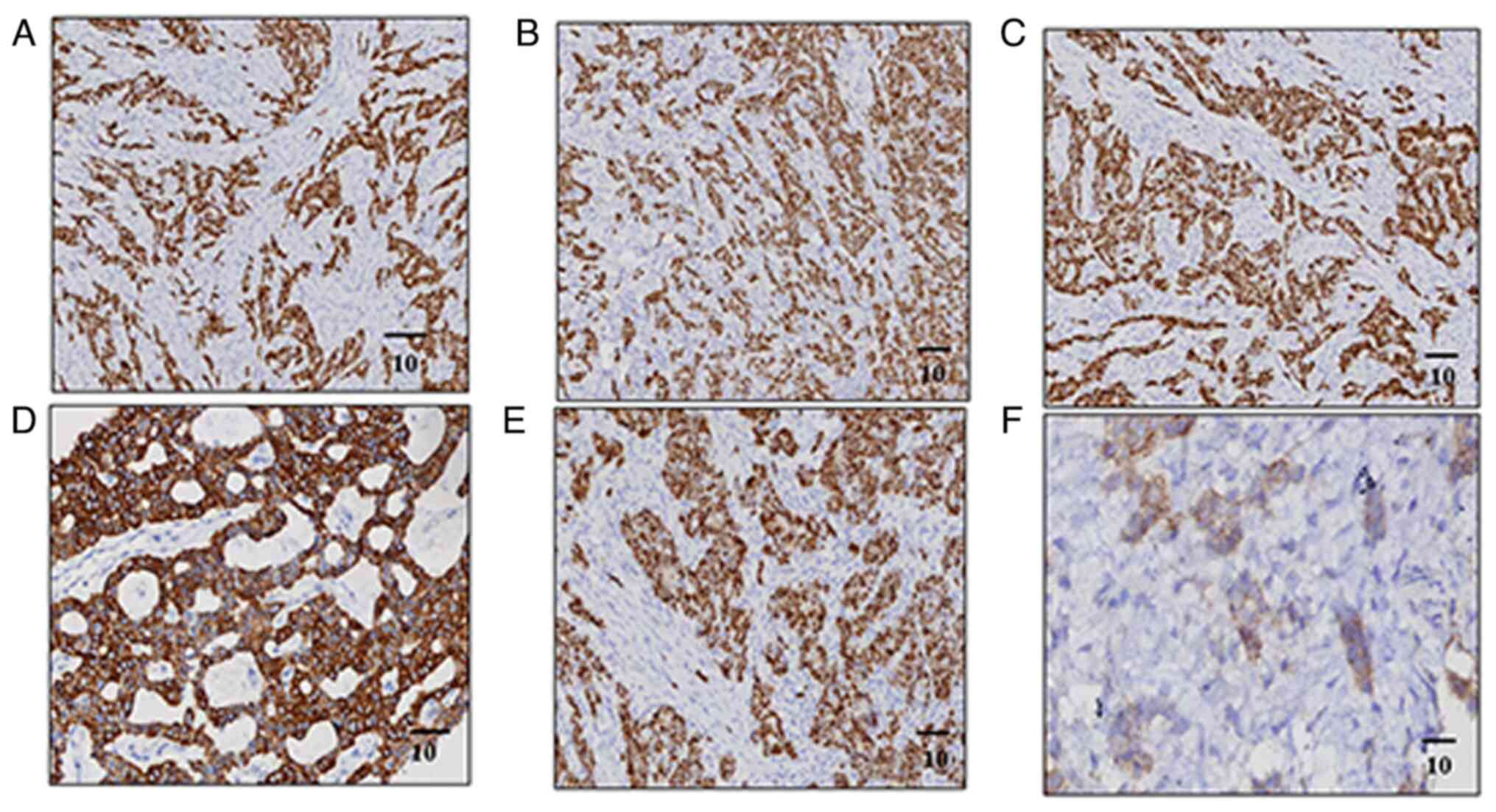
IHC staining was used to determine the amount and
the localization of the target proteins 5 µm paraffin-embedded
sections were deparaffinized, rehydrated and then immersed in
citrate buffer (pH 6.0) in a steam cooker. Subsequently, endogenous
peroxidases were blocked via immersing slides in 30%
(H2O2) for 10 min. Next, 2.5% Goat Serum
(Sigma, Steinheim, 12352203) was utilized to block nonspecific
binding 30 min at room temperatures. All the marker antibodies
E-cadherin (Sigma-Aldrich; Merck KGaA; cat. no. 12352202), GATA-3
(Abcam, ab268065), ER (Sigma, Steinheim, 51111800), PR (Sigma,
Steinheim, 12352203), HER-2 (Abcam, ab219208) and CK7 (Sigma,
Steinheim, 12352203) were diluted 1:200 in blocking solution and
applied onto the surface of tissue sections overnight at 4°C in a
humidified chamber. Following washing with PBST (PBS, 0.05% Tween
20) [slides were incubated with horseradish peroxidase (HRP)-linked
secondary antibodies (Sigma, Steinheim, 32160702) for 2 h at room
temperature. DAB, Sigma, Steinheim, 12352200] detection kit was
used to stain HRP and nuclei were counterstained with Mayer's
haematoxylin. Lastly, all stained slides were dehydrated through an
increasing ethanol concentration for 2 min each and images were
acquired using AxioVision 4.9 (Zeiss), and quantification of
targeted signals was performed by ImageJ (NIH). Upon
immunohistochemical examination of the liver biopsies, it was
determined that the patient was positive for E-cadherin, GATA-3,
ER, PR, HER-2 and CK7 (Fig. 3). The
pathological and immunohistochemical results suggested that the
patient had BCLM.
Following diagnosis, letrozole (2.5 mg oral
administration, once/day) combined with palbociclib (125 mg oral
administration, once a day) was administered orally for 3 weeks and
discontinued for 1 week. Letrozole combined with percept treatment,
not immunotherapy, is a recommended endocrine therapy for BC.
Although the necessity of adjuvant endocrine therapy was repeatedly
explained to the patient, the patient refused endocrine adjuvant
therapy for economic reasons. The patient was then treated with
standardized chemotherapy (Taxotere, 175 mg/m2 combined
with cyclophosphamide 600 mg/m2 every 2 weeks for 6
cycles of treatment.) and the tumour index, liver function and
routine blood tests were checked every month. The patient was
followed up for six months. At the most recent follow-up, the
condition was stable with no significant discomfort.
Discussion
The only cancer that affects women more frequently
than BC is non-melanoma skin cancer (10). BC remains the leading contributor to
cancer-related death worldwide for women and is the second-highest
contributor to cancer-related death among women in the USA.
Patients with metastatic disease have a shorter survival period
(3). BC accounts for >1% of all
male cancers and 1% of all cases of breast carcinoma, making it an
uncommon disease (6).
Advanced age, sex, premature menarche, late
menopause, nulliparity, no history of breastfeeding, family history
of BC, hormone treatment and previous experience with chest
radiation treatment may be risk factors associated with BC
(11). However, certain men who
develop BC do not have any known risk factors. Genetic factors,
affecting ~1 per 1000 men, pose the greatest risk for developing
MBC (12). A family history of BC
is associated with a relative risk of 2.5% in male patients.
Moreover, 20% of all men who have any type of cancer have a family
history of BC (13).
In the present study, the case of a 55-year-old male
patient with BCLM was reported. The patient underwent breast tumour
surgery 5 years prior to presenting with new symptoms. After
treatment, the patient was actively followed up regularly. Upon
recent admission, a CT examination of the patient revealed a mass
on the liver. A biopsy is necessary for confirming the accurate
identification of any suspected mass, and the Her2-neu, PR and ER
status should be examined. Laboratory evaluation, chest
radiography, bone scans and CT scans of the abdomen and pelvis were
performed as clinically appropriate. However, core biopsy is
preferred as it enables a definitive diagnosis. As determined using
microscopy, the tumour cells formed invasively in the stroma. MBCs
typically express ER, PR and HER-2 (14). The patient in the present report
tested positive for these biomarkers, and the E-cadherin positive
result indicated that the type of cancer was ductal carcinoma.
Additionally, the GATA-3 positive result indicated that the tumour
was breast-derived, and the CK7 positive result indicated
adenocarcinoma. Liver pathological examination suggested liver
metastasis of BC.
One of the most common sites of solid malignant
tumour metastases is the liver (15). After undergoing
epithelial-to-mesenchymal transition, BC cells separate from the
original tumour and enter the bloodstream by breaking through
endothelial barriers (16). The
hepatic microenvironment is pivotal for the invasion and
proliferation of metastatic BC cells and thus for the formation of
BCLMs (17). Xie et al
(18) suggested that M1 to M2
repolarization of tumour-associated macrophages can prevent
immunogenic and inflammatory responses while inducing
neoangiogenesis and matrix remodelling, promoting BC progression
and metastasis (18,19). Ingber et al (20) suggested that the relationship
between resident cell types and BC cells is crucial for the
regulation of the highly controlled hepatic milieu. Interactions
between cancer stem cells and liver microenvironment cells promote
metastasis. Additionally, the hepatic environment and stem cells
from cancer can alter to promote metastasis (21). Liver sinusoidal endothelial cells
serve as the first barrier that breast tumour cells encounter when
they enter the liver microcirculation. Kupffer cells (KCs) can
produce adhesion molecules, release proinflammatory cytokines and
facilitate the extravasation of tumour cells into the hepatic
parenchyma (22). In hepatocytes,
tumour metastasis is inhibited and promoted in part by liver
macrophages, KCs, stellate cells from the liver, myeloid-derived
suppressive cells, regulatory T cells and neutrophils (23). In the present case, the patient
underwent regular follow-up examinations and treatment for BC 5
years after surgery. The patient then presented with a liver tumour
that was pathologically derived from the breast; therefore,
considering the possible causes of the development of the tumour
microenvironment, which may manifest 5 years after BC surgery, the
development of a tumour microenvironment is the possible mechanism
of tumour formation. However, more cases may be needed to confirm
this.
The prognosis of female and male patients with BC is
similar when treated via the same approach (24). BC in men is often diagnosed by
histological criteria. Multimodal therapy involving chemotherapy,
radiation and surgery has improved the long-term survival and the
control of local disease in patients with MBC. In the present case,
the patient underwent breast tumour surgery 5 years ago and refused
further surgical treatment Hence, immunotherapy was administered as
a neoadjuvant agent. Genetic testing of the BRCA gene has a notable
role in the diagnosis of BC. BRCA status is of great importance for
the maintenance treatment of patients, especially high-risk
patients. Therefore, patients should be recommended to undergo BRCA
gene testing during subsequent treatment, however, the present
patient was not tested due to economic reasons. In the present
case, the patient declined genetic testing and was treated with
letrozole combined with percept was administered orally for 3 weeks
and then discontinued for 1 week. Because of the patient's ER, the
PR was positive, thus, this therapy is a good option for treating
BCLM in men.
In conclusion, liver metastasis in patients with BC
is a multistep and multifactor process. The development of the
premetastatic microenvironment, migration and metastasis centres in
the liver are the three key stages of the BC metastatic pathway.
Clinical symptoms, imaging and histology are typically used to
diagnose BCLM. Surgical resection is the primary treatment, but it
can also be paired with radiation therapy and chemotherapy.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Anhui Province clinical
medical research and transformation special project (grant no.
202304295107020071) and the Bethune Medical Research Fund (grant
no. B19059ET).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MJ conceptualised and designed the study and drafted
the manuscript. MJ, LL, HL and HX were involved in the patient
treatment and confirm the authenticity of all the raw data. All
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Diaby V, Tawk R, Sanogo V, Xiao H and
Montero AJ: A review of systematic reviews of the
cost-effectiveness of hormone therapy, chemotherapy, and targeted
therapy for breast cancer. Breast Cancer Res Treat. 151:27–40.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tarver T: Breast cancer facts &
figures 2021. American Cancer Society; Atlanta, GA: 2021
|
|
3
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2021. CA Cancer J Clin. 71:7–33. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
National Cancer Institute, . Cancer Stat
Facts: Female Breast Cancer. National Cancer Institute; Bethesda,
MD, USA: 2020
|
|
5
|
Atalay G, Biganzoli L, Renard F, Paridaens
R, Cufer T, Coleman R, Calvert AH, Gamucci T, Minisini A, Therasse
P, et al: Clinical outcome of breast cancer patients with liver
metastases alone in the anthracycline-taxane era: A retrospective
analysis of two prospective, randomised metastatic breast cancer
trials. Eur J Cancer. 39:2439–2449. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Eckhardt BL, Francis PA, Parker BS and
Anderson RL: Strategies for the discovery and development of
therapies for metastatic breast cancer. Nat Rev Drug Discov.
11:479–497. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Alcantara SB, Reed W, Willis K, Lee W,
Brennan P and Lewis S: Radiologist participation in
multi-disciplinary teams in breast cancer improves reflective
practice, decision making and isolation. Eur J Cancer Care (Engl).
23:616–623. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hortobagyi GN: Trastuzumab in the
treatment of breast cancer. N Engl J Med. 353:1734–1736. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Trayes KP and Cokenakes SEH: Breast cancer
treatment. Am Fam Physician. 104:171–178. 2021.PubMed/NCBI
|
|
11
|
Loibl S, Poortmans P, Morrow M, Denkert C
and Curigliano G: Breast cancer. Lancet. 397:1750–1769. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Giordano SH, Buzdar AU and Hortobagyi GN:
Breast cancer in men. Ann Intern Med. 137:678–687. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Anderson WF, Jatoi I, Tse J and Rosenberg
PS: Male breast cancer: A population-based comparison with female
breast cancer. J Clin Oncol. 28:232–239. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bartmann C, Wischnewsky M, Stüber T, Stein
R, Krockenberger M, Häusler S, Janni W, Kreienberg R, Blettner M,
Schwentner L, et al: Pattern of metastatic spread and subcategories
of breast cancer. Arch Gynecol Obstet. 295:211–223. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Battistoni A, Lantier L, di Tommaso A,
Ducournau C, Lajoie L, Samimi M, Coënon L, Rivière C, Epardaud M,
Hertereau L, et al: Nasal administration of recombinant Neospora
caninum secreting IL-15/IL-15Rα inhibits metastatic melanoma
development in lung. J Immunother Cancer. 11:e0066832023.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nieto MA: Epithelial plasticity: A common
theme in embryonic and cancer cells. Science. 342:12348502013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ma R, Feng Y, Lin S, Chen J, Lin H, Liang
X, Zheng H and Cai X: Mechanisms involved in breast cancer liver
metastasis. J Transl Med. 13:642015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Xie L, Yang Y, Meng J, Wen T, Liu J and Xu
H: Cationic polysaccharide spermine-pullulan drives tumor
associated macrophage towards M1 phenotype to inhibit tumor
progression. Int J Biol Macromol. 123:1012–1019. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu C, Mohan SC, Wei J, Seki E, Liu M,
Basho R, Giuliano AE, Zhao Y and Cui X: Breast cancer liver
metastasis: Pathogenesis and clinical implications. Front Oncol.
12:1043772022.
|
|
20
|
Ingber DE: Can cancer be reversed by
engineering the tumour microenvironment? Semin Cancer Biol.
18:356–364. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lau EY, Ho NP and Lee TK: Cancer stem
cells and their microenvironment: Biology and therapeutic
implications. Stem Cells Int. 2017:37141902017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Osborne N, Sundseth R, Gay MD, Cao H,
Tucker RD, Nadella S, Wang S, Liu X, Kroemer A, Sutton L, et al:
Vaccine against gastrin, a polyclonal antibody stimulator,
decreases pancreatic cancer metastases. Am J Physiol Gastrointest
Liver Physio. 317:G682–G693. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gucalp A, Traina TA, Eisner JR, Parker JS,
Selitsky SR, Park BH, Elias AD, Baskin-Bey ES and Cardoso F: Male
breast cancer: A disease distinct from female breast cancer. Breast
Cancer Res Treat. 173:37–48. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ou J, Peng Y, Deng J, Miao H, Zhou J, Zha
L, Zhou R, Yu L, Shi H and Liang H: Endothelial cell-derived
fibronectin extra domain A promotes colorectal cancer metastasis
via inducing epithelial-mesenchymal transition. Carcinogenesis.
35:1661–1670. 2014. View Article : Google Scholar : PubMed/NCBI
|