|
1
|
Koshy M, Villano JL, Dolecek TA, Howard A,
Mahmood U, Chmura SJ, Weichselbaum RR and McCarthy BJ: Improved
survival time trends for glioblastoma using the SEER 17
population-based registries. J Neurooncol. 107:207–212. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fabbro-Peray P, Zouaoui S, Darlix A,
Fabbro M, Pallud J, Rigau V, Mathieu-Daude H, Bessaoud F, Bauchet
F, Riondel A, et al: Association of patterns of care, prognostic
factors, and use of radiotherapy-temozolomide therapy with survival
in patients with newly diagnosed glioblastoma: A French national
population-based study. J Neurooncol. 142:91–101. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stupp R, Mason WP, van den Bent MJ, Weller
M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn
U, et al: Radiotherapy plus concomitant and adjuvant temozolomide
for glioblastoma. N Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Louis DN, Perry A, Wesseling P, Brat DJ,
Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM,
Reifenberger G, et al: The 2021 WHO classification of tumors of the
central nervous system: A summary. Neuro Oncol. 23:1231–1251. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seles M, Posch F, Pichler GP, Gary T,
Pummer K, Zigeuner R, Hutterer GC and Pichler M: Blood platelet
volume represents a novel prognostic factor in patients with
nonmetastatic renal cell carcinoma and improves the predictive
ability of established prognostic scores. J Urol. 198:1247–1252.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yun ZY, Zhang X, Liu YS, Liu T, Liu ZP,
Wang RT and Yu KJ: Lower mean platelet volume predicts poor
prognosis in renal cell carcinoma. Sci Rep. 7:67002017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tuncel T, Ozgun A, Emirzeoglu L, Celik S,
Bilgi O and Karagoz B: Mean platelet volume as a prognostic marker
in metastatic colorectal cancer patients treated with
bevacizumab-combined chemotherapy. Asian Pac J Cancer Prev.
15:6421–6423. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kumagai S, Tokuno J, Ueda Y, Marumo S,
Shoji T, Nishimura T, Fukui M and Huang CL: Prognostic significance
of preoperative mean platelet volume in resected non-small-cell
lung cancer. Mol Clin Oncol. 3:197–201. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kilincalp S, Ekiz F, Başar O, Ayte MR,
Coban S, Yılmaz B, Altınbaş A, Başar N, Aktaş B, Tuna Y, et al:
Mean platelet volume could be possible biomarker in early diagnosis
and monitoring of gastric cancer. Platelets. 25:592–594. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang F, Chen Z, Wang P, Hu X, Gao Y and
He J: Combination of platelet count and mean platelet volume
(COP-MPV) predicts postoperative prognosis in both resectable early
and advanced stage esophageal squamous cell cancer patients. Tumour
Biol. 37:9323–3931. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gu M, Zhai Z, Huang L, Zheng W, Zhou Y,
Zhu R, Shen F and Yuan C: Pre-treatment mean platelet volume
associates with worse clinicopathologic features and prognosis of
patients with invasive breast cancer. Breast Cancer. 23:752–760.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cho SY, Yang JJ, You E, Kim BH, Shim J,
Lee HJ, Lee WI, Suh JT and Park TS: Mean platelet volume/platelet
count ratio in hepatocellular carcinoma. Platelets. 24:375–377.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Inagaki N, Kibata K, Tamaki T, Shimizu T
and Nomura S: Prognostic impact of the mean platelet
volume/platelet count ratio in terms of survival in advanced
non-small cell lung cancer. Lung Cancer. 83:97–101. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang X, Qin YY, Chen M, Wu YY and Lin FQ:
Combined use of mean platelet volume/platelet count ratio and
platelet distribution width to distinguish between patients with
nasopharyngeal carcinoma, those with benign tumors of the
nasopharynx, and healthy subjects. Cancer Manag Res.
11:10375–10382. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Feng JF, Sheng C, Zhao Q and Chen P:
Prognostic value of mean platelet volume/platelet count ratio in
patients with resectable esophageal squamous cell carcinoma: A
retrospective study. PeerJ. 7:e72462019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lin YC, Jan HC, Ou HY, Ou CH and Hu CY:
low preoperative mean platelet volume/platelet count ratio
indicates worse prognosis in non-metastatic renal cell carcinoma. J
Clin Med. 10:36762021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Giannakeas V, Kotsopoulos J, Brooks JD,
Cheung MC, Rosella L, Lipscombe L, Akbari MR, Austin PC and Narod
SA: Platelet count and survival after cancer. Cancers (Basel).
14:5492022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Giannakeas V, Kotsopoulos J, Cheung MC,
Rosella L, Brooks JD, Lipscombe L, Akbari MR, Austin PC and Narod
SA: Analysis of platelet count and new cancer diagnosis over a
10-year period. JAMA Netw Open. 5:e21416332022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Olsson AK and Cedervall J: The
pro-inflammatory role of platelets in cancer. Platelets.
29:569–573. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lievens D, Zernecke A, Seijkens T,
Soehnlein O, Beckers L, Munnix IC, Wijnands E, Goossens P, van
Kruchten R, Thevissen L, et al: Platelet CD40L mediates thrombotic
and inflammatory processes in atherosclerosis. Blood.
116:4317–4327. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Thomas MR and Storey RF: The role of
platelets in inflammation. Thromb Haemost. 114:449–458. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thompson CB, Eaton KA, Princiotta SM,
Rushin CA and Valeri CR: Size dependent platelet subpopulations:
Relationship of platelet volume to ultrastructure, enzymatic
activity, and function. Br J Haematol. 50:509–519. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen X, Li J, Zhang X, Liu Y, Wu J, Li Y,
Cui X and Jiang X: Prognostic and clinicopathological significance
of pretreatment mean platelet volume in cancer: A meta-analysis.
BMJ Open. 10:e0376142020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Detopoulou P, Panoutsopoulos GI, Mantoglou
M, Michailidis P, Pantazi I, Papadopoulos S and Rojas Gil AP:
Relation of mean platelet volume (MPV) with Cancer: A systematic
review with a focus on disease outcome on twelve types of cancer.
Curr Oncol. 30:3391–3420. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kharel S, Shrestha S, Shakya P, Rawat R
and Shilpakar R: Prognostic significance of mean platelet volume in
patients with lung cancer: A meta-analysis. J Int Med Res.
50:30006052210848742022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Louis DN, Perry A, Reifenberger G, von
Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD,
Kleihues P and Ellison DW: The 2016 World Health Organization
Classification of Tumors of the Central Nervous System: A summary.
Acta Neuropathol. 131:803–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nobusawa S, Watanabe T, Kleihues P and
Ohgaki H: IDH1 mutations as molecular signature and predictive
factor of secondary glioblastomas. Clin Cancer Res. 15:6002–6007.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Karschnia P, Young JS, Dono A, Häni L,
Sciortino T, Bruno F, Juenger ST, Teske N, Morshed RA, Haddad AF,
et al: Prognostic validation of a new classification system for
extent of resection in glioblastoma: A report of the RANO resect
group. Neuro Oncol. 25:940–954. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mor V, Laliberte L, Morris JN and Wiemann
M: The karnofsky performance status scale. An examination of its
reliability and validity in a research setting. Cancer.
53:2002–2007. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
R Core Team, . R: A language and
environment for statistical computing. R Foundation for Statistical
Computing; Vienna, Austria: 2022, Available from:. https://www.R-project.org/
|
|
31
|
Therneau TM: A Package for Survival
Analysis in R. R package. Version 3.5-5, 2023. Available from.
https://CRAN.R-project.org/package=survival
|
|
32
|
Sjoberg DD, Baillie M, Fruenchtenicht C,
Haesendonckx S and Treis T: Flexible Time-to-Event Figures. R
package. Version 1.0.0. 2023.Available from:. https://CRAN.R-project.org/package=ggsurvfit
|
|
33
|
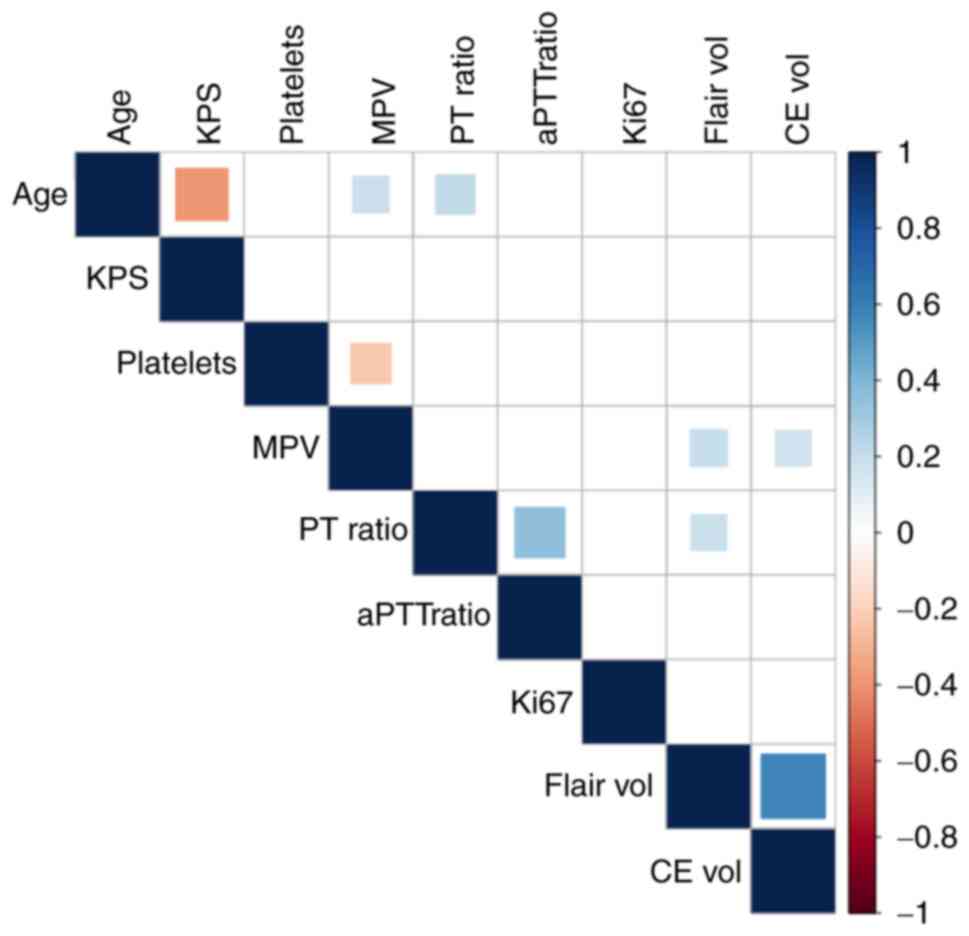
Wei T and Simko V: R package ‘corrplot’:
Visualization of a Correlation Matrix. Version 0.92. 2021.Available
from:. https://github.com/taiyun/corrplot
|
|
34
|
Wickham H: ggplot2: Elegant Graphics for
Data Analysis. Springer-Verlag New York. Version 1.0.2016.Available
from:. https://ggplot2.tidyverse.org
|
|
35
|
Sheng J, Qiu P and Geyer CJ: TSHRC: Two
Stage Hazard Rate Comparison. Version 0.1-6. 2019.Available from:.
https://CRAN.R-project.org/package=TSHRC
|
|
36
|
Tanriverdi O, Menekse S, Teker F, Oktay E,
Nur Pilanc K, Gunaldi M, Kocar M, Kacan T, Bahceci A, Avci N, et
al: The mean platelet volume may predict the development of
isolated bone metastases in patients with breast cancer: A
retrospective study of the Young Researchers Committee of the
Turkish Oncology Group (TOG). J BUON. 21:840–850. 2016.PubMed/NCBI
|
|
37
|
Sun H, Yin CQ, Liu Q, Wang F and Yuan CH:
Clinical signi fi cance of routine blood test-associated
inflammatory index in breast cancer patients. Med Sci Monit.
23:5090–5095. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Divsalar B, Heydari P, Habibollah G and
Tamaddon G: Hematological parameters changes in patients with
breast cancer. Clin Lab. 67:2021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kurtoglu E, Kokcu A, Celik H, Sari S and
Tosun M: Platelet indices may be useful in discrimination of benign
and malign endometrial lesions, and early and advanced stage
endometrial cancer. Asian Pac J Cancer Prev. 16:5397–5400. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang H, Liang K, Ke L and Tang S:
Clinical application of red cell distribution width, mean platelet
volume, and cancer antigen 125 detection in endometrial cancer. J
Clin Lab Anal. 34:e233092020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Karateke A, Kaplanoglu M and Baloglu A:
Relations of platelet indices with endometrial hyperplasia and
endometrial cancer. Asian Pac J Cancer Prev. 16:4905–4908. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Oge T, Yalcin OT, Ozalp SS and Isikci T:
Platelet volume as a parameter for platelet activation in patients
with endometrial cancer. J Obstet Gynaecol. 33:301–304. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Song J, Lai X, Zhang Y, Zheng X and Su J:
Preoperative platelet morphology parameters as prognostic
predictors for endometrial malignant carcinoma stage and
progesterone receptor. Medicine (Baltimore). 98:e178182019.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Yayla Abide C, Bostanci Ergen E, Cogendez
E, Kilicci C, Uzun F, Ozkaya E and Karateke A: Evaluation of
complete blood count parameters to predict endometrial cancer. J
Clin Lab Anal. 32:e224382018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Shen XM, Xia YY, Lian L, Zhou C, Li XL,
Han SG, Zheng Y, Gong FR, Tao M, Mao ZQ and Li W: Mean platelet
volume provides beneficial diagnostic and prognostic information
for patients with resectable gastric cancer. Oncol Lett.
12:2501–2506. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Pietrzyk L, Plewa Z, Denisow-Pietrzyk M,
Zebrowski R and Torres K: Diagnostic power of blood parameters as
screening markers in gastric cancer patients. Asian Pac J Cancer
Prev. 17:4433–4437. 2016.PubMed/NCBI
|
|
47
|
Li JY, Li Y, Jiang Z, Wang RT and Wang XS:
Elevated mean platelet volume is associated with presence of colon
cancer. Asian Pac J Cancer Prev. 15:10501–10504. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zhou X, Chen H, Zhang W, Li X, Si X and
Zhang G: Predictive value of routine blood test in patients with
early esophageal cancer: A matched case-control study. J Cancer.
12:4739–4744. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Surucu E, Demir Y and Sengoz T: The
correlation between the metabolic tumor volume and hematological
parameters in patients with esophageal cancer. Ann Nucl Med.
29:906–910. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhu X, Chen Y and Cui Y: Absolute
neutrophil count and mean platelet volume in the blood as
biomarkers to detect lung cancer. Dis Markers. 2020:13719642020.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zu R, Yu S, Yang G, Ge Y, Wang D, Zhang L,
Song X, Deng Y, He Q, Zhang K, et al: Integration of platelet
features in blood and platelet rich plasma for detection of lung
cancer. Clin Chim Acta. 509:43–51. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Goksel S, Ozcelik N, Telatar G and Ardic
C: The role of hematological inflammatory biomarkers in the
diagnosis of lung cancer and in predicting TNM Stage. Cancer
Invest. 39:514–520. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Aksoy EK, Kantarcı S, Torgutalp M, Akpınar
MY, Sapmaz FP, Yalçın GŞ, Uzman M, Şimşek GG and Nazlıgül Y: The
importance of complete blood count parameters in the screening of
gastric cancer. Prz Gastroenterol. 14:183–187. 2019.PubMed/NCBI
|
|
54
|
Huang L, Hu Z, Luo R, Li H, Yang Z, Qin X
and Mo Z: Predictive values of the selected inflammatory indexes in
colon cancer. Cancer Control. 29:107327482210913332022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Sun SY, Zhao BQ, Wang J, Mo ZX, Zhao YN,
Wang Y and He J: The clinical implications of mean platelet volume
and mean platelet volume/platelet count ratio in locally advanced
esophageal squamous cell carcinoma. Dis Esophagus. 31:2018.
View Article : Google Scholar
|
|
56
|
Pyo JS, Sohn JH and Kang G: Diagnostic and
prognostic roles of the mean platelet volume in malignant tumors: A
systematic review and meta-analysis. Platelets. 27:722–728. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Panek WK, Pituch KC, Miska J, Kim JW,
Rashidi A, Kanojia D, Lopez-Rosas A, Han Y, Yu D, Chang CL, et al:
Local application of autologous platelet-rich fibrin Patch (PRF-P)
suppresses regulatory T cell recruitment in a murine glioma model.
Mol Neurobiol. 56:5032–5040. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Neuzillet C, Tijeras-Raballand A, Cohen R,
Cros J, Faivre S, Raymond E and de Gramont A: Targeting the TGFβ
pathway for cancer therapy. Pharmacol Ther. 147:22–31. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Filippelli A, Del Gaudio C, Simonis V,
Ciccone V, Spini A and Donnini S: Scoping review on platelets and
tumor angiogenesis: Do we need more evidence or better analysis?
Int J Mol Sci. 23:134012022. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Wach J, Apallas S, Schneider M, Weller J,
Schuss P, Vatter H, Herrlinger U and Güresir E: Mean platelet
volume/platelet count ratio and risk of progression in
glioblastoma. Front Oncol. 11:6953162021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Alimohammadi E, Bagheri SR, Bostani A,
Rezaie Z and Farid M: Preoperative platelet distribution
width-to-platelet count ratio as a prognostic factor in patients
with glioblastoma multiforme. Br J Neurosurg. 38:307–313. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Campanella R, Guarnaccia L, Cordiglieri C,
Trombetta E, Caroli M, Carrabba G, La Verde N, Rampini P, Gaudino
C, Costa A, et al: Tumor-Educated platelets and angiogenesis in
glioblastoma: Another brick in the wall for novel prognostic and
targetable biomarkers, changing the vision from a localized tumor
to a systemic pathology. Cells. 9:2942020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Huang K, Wei S, Huang Z, Xie Y, Wei C, Xu
J, Dong L, Zou Q and Yang J: Effect of preoperative peripheral
blood platelet volume index on prognosis in patients with invasive
breast cancer. Future Oncol. 19:1853–186. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Maas SLN, Draaisma K, Snijders TJ, Senders
JT, Berendsen S, Seute T, Schiffelers RM, van Solinge WW, Ten Berg
MJ, Robe PA and Broekman MLD: Routine blood tests do not predict
survival in patients with glioblastoma-multivariable analysis of
497 patients. World Neurosurg. 126:e1081–e1091. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bruno F, Pellerino A, Palmiero R, Bertero
L, Mantovani C, Garbossa D, Soffietti R and Rudà R: Glioblastoma in
the Elderly: Review of molecular and therapeutic aspects.
Biomedicines. 10:6442022. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Bozdag S, Li A, Riddick G, Kotliarov Y,
Baysan M, Iwamoto FM, Cam MC, Kotliarova S and Fine HA:
Age-specific signatures of glioblastoma at the genomic, genetic,
and epigenetic levels. PLoS One. 8:e629822013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zhang K, Wang XQ, Zhou B and Zhang L: The
prognostic value of MGMT promoter methylation in Glioblastoma
multiforme: A meta-analysis. Fam Cancer. 12:449–458. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Tian M, Ma W, Chen Y, Yu Y, Zhu D, Shi J
and Zhang Y: Impact of gender on the survival of patients with
glioblastoma. Biosci Rep. 38:BSR201807522018. View Article : Google Scholar : PubMed/NCBI
|