Introduction
A lung abscess (LA) represents a serious respiratory
infectious condition marked by elevated occurrence and fatality
rates. Despite the introduction of antibiotic therapy, the
mortality rate of lung abscesses remains high at 10–20% (1). Furthermore, a recent study indicated
that the mortality rate of patients with lung abscesses in the
intensive care unit may reach up to 52% (2). LAs present as necrotic lesions within
the lung parenchyma, induced by microorganisms, resulting in the
development of abscess cavities containing necrotic or liquefied
substances, frequently exhibiting a liquid-gas level (3). With continuous progress in the
clinical utilization of antibiotics, a significant portion of LA
cases can be efficiently managed. Nevertheless, in cases of LAs
showing resistance to conservative therapies, surgical intervention
remains imperative. Large-scale prospective investigations are
warranted to establish evidence-based protocols for surgical and
antibiotic interventions (4).
In recent years, the occurrence of lung cancer
combined with LA has been rising in clinical settings. A study
examining the clinical features of 222 patients with LA revealed
that 7% presented with coexisting pulmonary malignancies (5). Subsequent investigations suggest that
tumor-related immunosuppressive signaling and impaired immune
function could exacerbate bacterial infections in the presence of
tumors, thereby escalating the seriousness of LAs (6). Hence, the concomitance of LA and lung
cancer warrants substantial consideration. The combination of LA
and lung cancer poses an increased risk of therapeutic inefficacy
and postoperative mortality attributed to the complexities in
surgical scheduling, thereby exerting notable detrimental impacts
on patient outcomes (7).
Conversely, in the diagnosis and management of this condition, the
sudden emergence of LAs may overshadow the identification and
treatment of primary lung cancer, potentially leading to diagnostic
errors, oversight and subsequent treatment delays for lung cancer
(8). Moreover, the presence of LAs
markedly heightens the likelihood of postoperative infections
subsequent to lung cancer therapy (9), presenting notable complexities for
clinicians in treatment strategizing and surgical scheduling.
Fever is a physiological response to infection,
commonly associated with the activation of the immune system,
signifying its effort to combat pathogens (10). However, surgical procedures can
temporarily compromise immune function, thereby increasing the
patient's susceptibility to infections (10). Moreover, fever can influence the
metabolism and distribution of drugs, potentially complicating
anesthesia management and thereby affecting the overall
effectiveness of the surgery (11).
For patients with lung cancer, concurrent acute LAs and a history
of fever, scheduling surgery soon after the body temperature has
normalized may be a more appropriate approach than continuing
conservative treatment with antibiotics. The objective of the
present case report is to provide insights into the diagnosis and
management of these conditions, and to offer practical guidance for
clinical application.
Case report
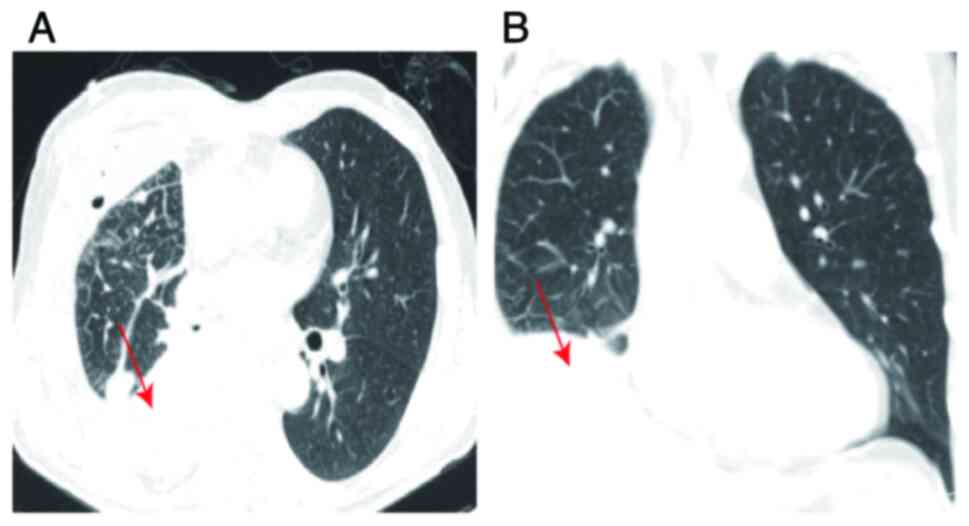
A 64-year-old male patient exhibited blood-tinged
sputum of unknown etiology in April 2022. The blood appeared bright
red, with an estimated volume of ~5 ml, and no systematic
intervention was administered. Subsequently, in May, the patient
encountered a recurring episode of hemoptysis with similar
attributes and volume, prompting the performance of a chest
computed tomography (CT) scan at Xingyi People's Hospital (Xingyi,
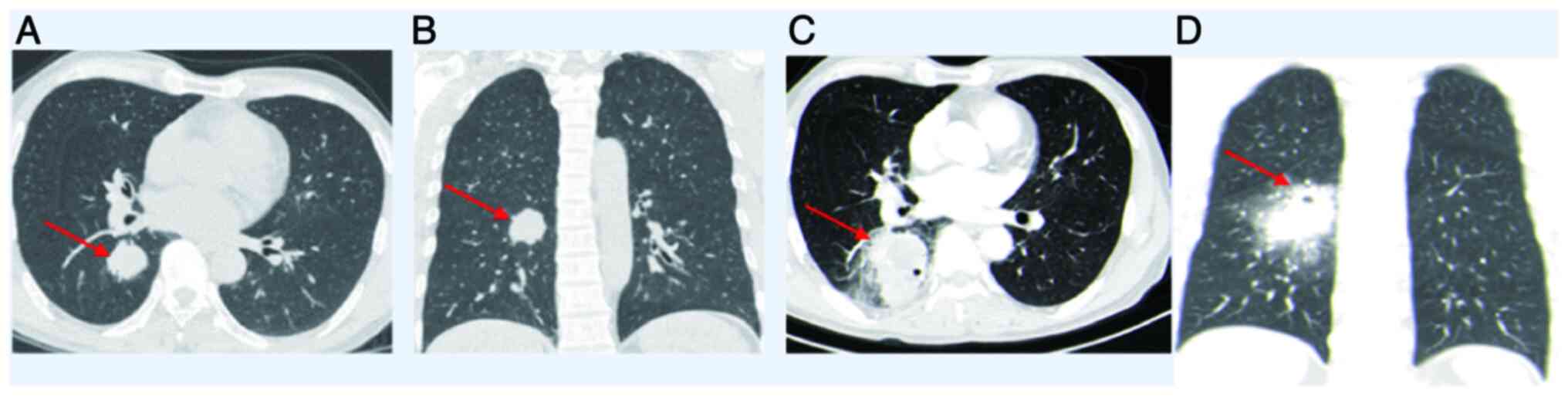
China). The imaging examination identified a lesion in the
posterior segment of the right lower lobe, accompanied by slight
bronchial dilation and distal infection, measuring ~2.8×3.2 cm
(Fig. 1A and B). Despite the
administration of antitussive (10 mg codeine, taken orally twice
daily), hemostatic (10 units posterior pituitary hormone dissolved
in 250 ml 10% glucose solution for intravenous infusion) and
anti-infective therapies (1.5 g cefuroxime sodium in 100 ml 0.9%
sodium chloride solution administered via intravenous infusion,
once every 8 h), the patient's clinical status did not demonstrate
any notable improvement.
At 6 days post-recurrence of hemoptysis, the patient
was transferred to the Affiliated Hospital of Guizhou Medical
University (Guiyang, China) for additional evaluation and
management. The patient had a clean medical record, devoid of prior
medical conditions or notable medical history. The patient had a
smoking history of >40 years, consuming ~15 cigarettes daily,
and had abstained from smoking for 1 week. Upon admission, a
focused physical examination revealed diminished breath sounds on
the right side, without any additional notable findings. Diagnostic
workup: Throughout the hospitalization, a series of blood cell
evaluations were performed, and the inflammatory marker results,
including white blood cells (normal value,
3.5–9.5×109/l), absolute neutrophils (normal value,
1.8–6.3×109/l) and neutrophil percentage (normal range,
40–75%), which were higher than normal before surgery, are
presented in Table I. Coagulation
parameters, pulmonary function tests, whole-body bone scintigraphy
and cranial CT findings all exhibited normal results. The chest CT
scan exhibited patchy opacities in the right lower lobe with the
presence of a cavity, measuring ~5.7×4.5 cm (Fig. 1C and D). Following imaging
assessments, the observed lesion was suspected to be indicative of
lung cancer. At 2 days post-admission, the patient developed a high
fever, with a maximum temperature reaching 39.2°C. Empirical
antibiotic therapy with cefuroxime sodium was initiated (1.5 g
cefuroxime sodium in 100 ml 0.9% sodium chloride solution
administered via intravenous infusion, once every 8 h). From day 3
post-admission, the treatment was switched to piperacillin for
infection control (4.5 g piperacillin sodium in 100 ml 0.9% sodium
chloride solution administered via intravenous infusion, once every
8 h), but the fever persisted and the temperature did not return to
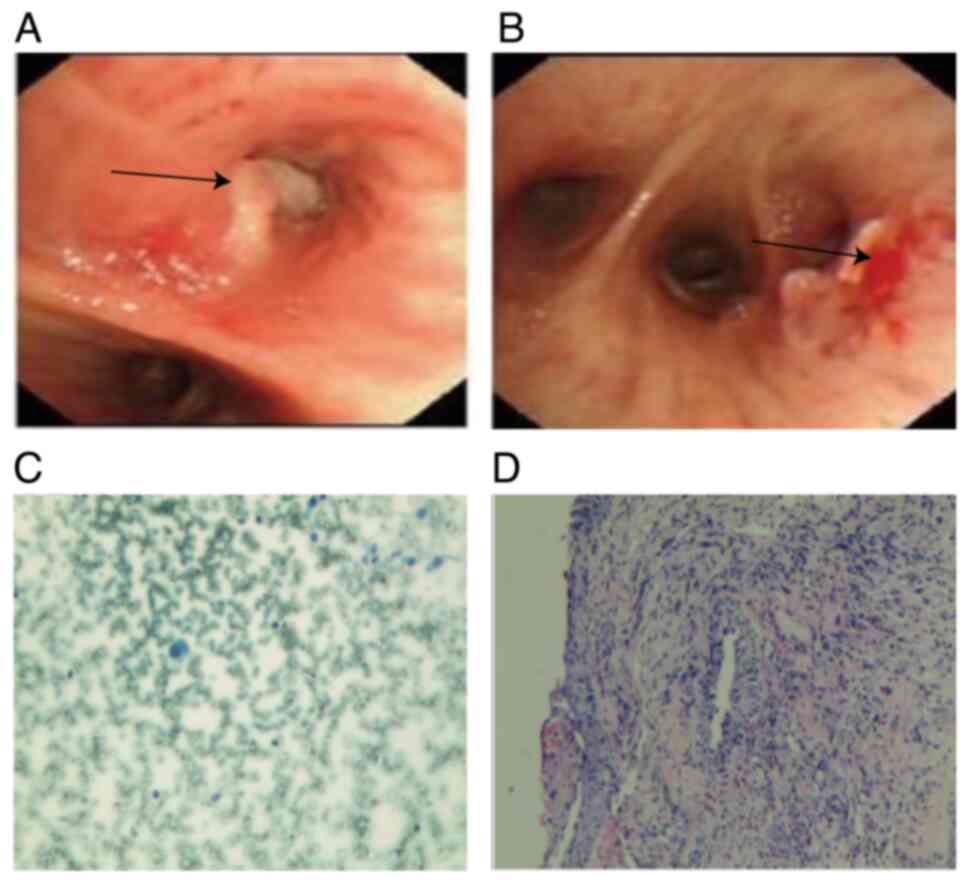
normal. On day 3 post-admission, the patient underwent bronchoscopy
procedures, during which biopsies were obtained from the middle
right bronchus and the posterior segment of the right lower lobe;
however, the findings did not definitively establish a diagnosis of
lung cancer (Fig. 2). On the day 6
post-admission, meropenem was introduced (1 g meropenem sodium in
100 ml 0.9% sodium chloride solution administered via intravenous
infusion, once every 8 h), leading to gradual temperature control
and stabilization at normal levels. The sputum culture and
sensitivity test results on the day 11 post-admission revealed that
the Klebsiella pneumoniae strain causing the infection was
resistant to amoxicillin and cefuroxime sodium, but sensitive to
levofloxacin, imipenem and meropenem. This explains why the fever
gradually came under control after switching to meropenem.
 | Table I.Statistical table of
inflammation-related indices in blood cell analysis
examination. |
Table I.
Statistical table of
inflammation-related indices in blood cell analysis
examination.
| Date
post-admission | White blood cells,
×109/l (normal value, 3.5–9.5×109/l) | Absolute neutrophils,
×109/l (normal value, 1.8–6.3×109/l) | Neutrophil percentage
(normal range, 40.00–75.00%) |
|---|
| Day 1 | 16.64 | 13.07 | 78.40 |
| Day 4 | 23.69 | 21.34 | 90.00 |
| Day 8 | 18.57 | 15.90 | 85.60 |
| Day 11 | 18.60 | 15.80 | 84.90 |
| Day 14 | 20.99 | 18.72 | 89.20 |
| Day 17 | 10.98 | 8.80 | 80.10 |
| Day 22 | 4.63 | 3.23 | 69.70 |
| Day 24 | 5.13 | 3.42 | 66.70 |
| Day 28 | 9.64 | 7.21 | 74.80 |
Despite the inconclusive outcomes of the
bronchoscopy, a thorough assessment of the patient's medical
history involving blood-tinged sputum and chest CT results
indicated a strong likelihood of lung cancer, potentially
complicated by a secondary acute LA attributed to bronchial
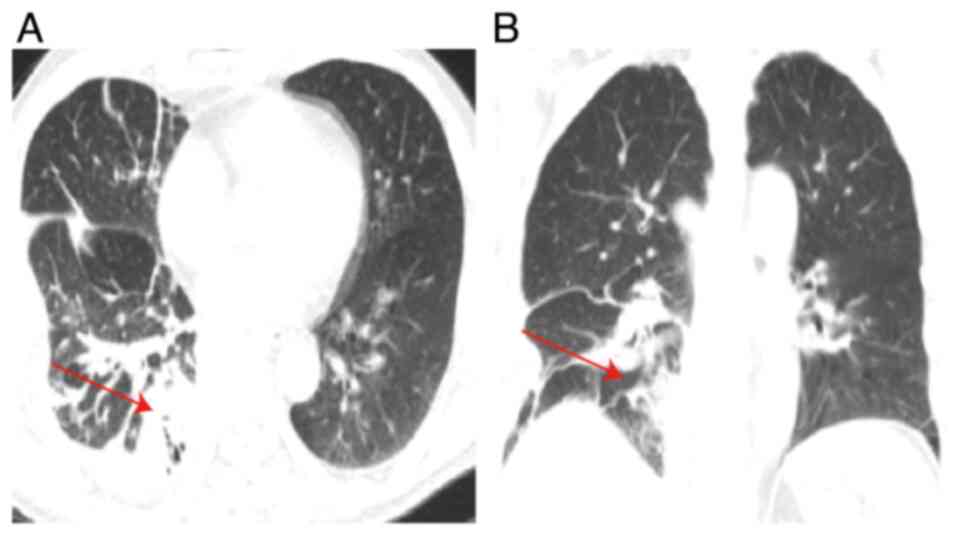
obstruction by the tumor. A follow-up chest CT scan 8 days later
demonstrated a decrease in the lesion size within the right lower
lobe relative to the previous imaging assessment (Fig. 3). However, the full blood count
conducted after another 2 days revealed an elevated white blood
cell count 20.99×109/l (normal value 3.5–9.5×109/l),
neutrophil count 18.72×109/l (normal value
1.8–6.3×109/l) and neutrophil percentage 89.20% (normal range
40–75%), suggesting inadequate control of the infection. After the
patient's temperature normalized, surgical intervention was
scheduled to remove the lesion in a timely manner. The patient
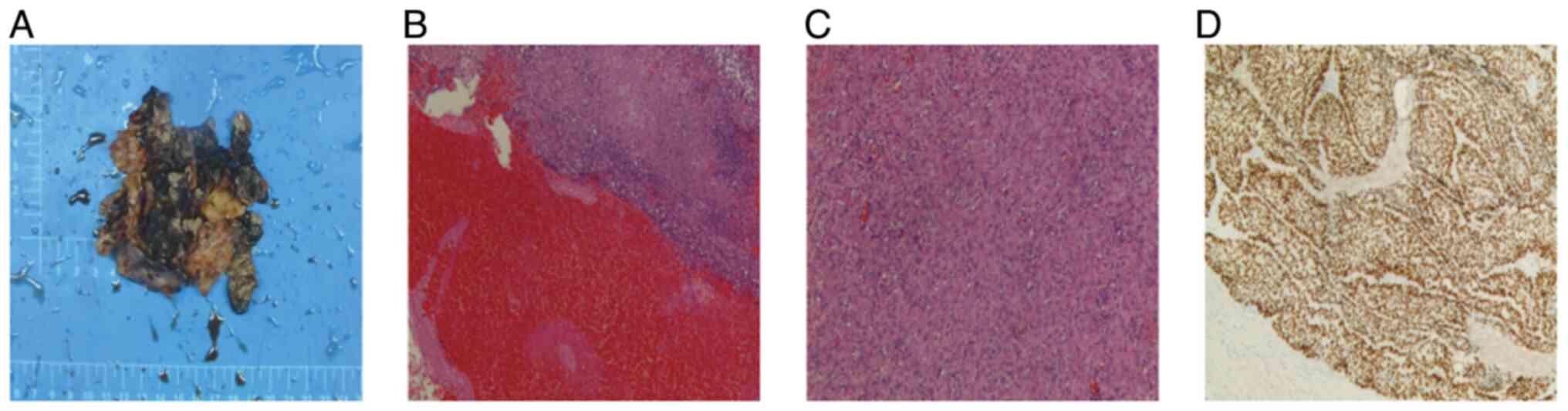
underwent video-assisted thoracoscopic surgery involving a right
lower lobectomy, decortication and systematic lymph node dissection
under anesthesia. Subsequent histopathological and
immunohistochemical analyses (Data S1; Table SI) verified the presence of
moderately differentiated squamous cell carcinoma in the right
lower lobe (Fig. 4). The tumor
cells were cytokeratin (CK)(+), epithelial membrane
antigen(partially +), vimentin(−), CK7(−), p63(+), p40(+),
CK5/6(+), CK20(−), thyroid transcription factor-1(−), napsin A(−),
CD56(−), synaptophysin(−), chromogranin A(−) and Ki-67(+; ~80%).
Notably, all examined lymph nodes were negative, and the tumor
exhibited dimensions of 4×3 cm without evidence of distant
metastasis. Consequently, according to the Tumor-Node-Metastasis
staging system for Non-Small Cell Lung Cancer (NSCLC) in the 8th
edition the tumor was determined as T2aN0M0, Ib (12).
Within 4 days of surgery, the patient received
levofloxacin at a dose of 0.2 g in 250 ml 0.9% sodium chloride
solution administered via intravenous infusion, twice a day.
Reexamination revealed that infection markers were stable and had
returned to normal, while the symptoms of cough and hemoptysis
gradually subsided. Apart from fat liquefaction at the surgical
site, no other complications were reported in the postoperative
period. The patient was diagnosed with early stage squamous cell
carcinoma, and no adjuvant antineoplastic treatment was prescribed
following the surgical procedure. Subsequent to the intervention,
the postoperative chest CT scan, depicted in Fig. 5, exhibited no notable abnormalities.
Regular follow-up assessments were conducted post-discharge,
including chest CT scans every 3 months, all of which demonstrated
no significant abnormalities. By the time of the follow-up chest CT
in March 2024, the patient had shown substantial recovery.
Discussion
The present study describes a case of lung cancer
complicated by an acute LA. Advancements in medical technology and
public health awareness, notably through low-dose CT screening for
high-risk lung cancer populations, have led to the simultaneous
detection of lung infections. This early identification enables
prompt treatment interventions to prevent the escalation of
complications (13,14). However, in clinical practice,
primary lung tumors can be missed due to the presence of LAs,
potentially resulting in misdiagnosis as benign LAs. Furthermore,
malignant LAs exhibit clinical and radiographic characteristics
akin to those of benign LAs, thereby presenting substantial
obstacles in the diagnosis and treatment of lung cancer complicated
by LA (15). Therefore, it is
essential to differentiate between these conditions before
establishing a definitive pathological diagnosis. In pulmonary
cryptococcosis, chest X-rays commonly reveal lung masses
predominantly situated in the lower lobes, accompanied by
indications of parenchymal consolidation and diffuse interstitial
infiltration (16–18). The radiographic characteristics of
pulmonary actinomycosis may encompass atelectasis and cavitation;
however, it typically manifests as multiple, indistinct nodules or
mass-like shadows (19). LAs
resulting from aspergillomas exhibit radiographic similarities to
malignant tumors, featuring a distinct mass within the cavity; they
can be identified by the presence of thick-walled, round or oval
cavities (20). Therefore, in
individuals presenting with LAs, maintaining vigilance for
potential concurrent lung cancer is essential to prevent
overlooking the optimal treatment window, which could detrimentally
impact prognosis (7).
The treatment of lung cancer complicated by acute LA
centers on efficiently tackling both the infection stemming from
the LA and the prompt handling of the primary lung tumor. Benign
LAs are usually responsive to antibiotic therapy or percutaneous
drainage, with surgical intervention being uncommon (7,21).
Nevertheless, in cases of lung cancer accompanied by LA,
conservative treatment alone may prove inadequate in addressing the
condition. Abscesses developed within the tumor pose challenges in
effectively managing infections through antibiotic therapy
(22), and the effectiveness of
percutaneous drainage for abscesses linked to malignant tumors is
limited (7). Conversely, as lung
cancer advances, relying solely on conservative management for LAs
may lead to missing the opportune treatment window for lung cancer.
Currently, there is a lack of definitive guidelines for managing
lung cancer complicated by LA. Previous studies suggest an initial
approach involving anti-infective therapy followed by subsequent
anticancer treatment once the infection is fully controlled
(8,23). Nonetheless, the presence of
concurrent lung cancer prolongs the duration required to manage the
infection, yielding suboptimal outcomes. The clinical rationale of
deferring lung cancer treatment until full resolution of pulmonary
infection appears compelling. Hence, early surgical intervention
following diagnosis or during a high suspicion scenario may
represent a viable new treatment approach for lung cancer
accompanied by pulmonary abscess.
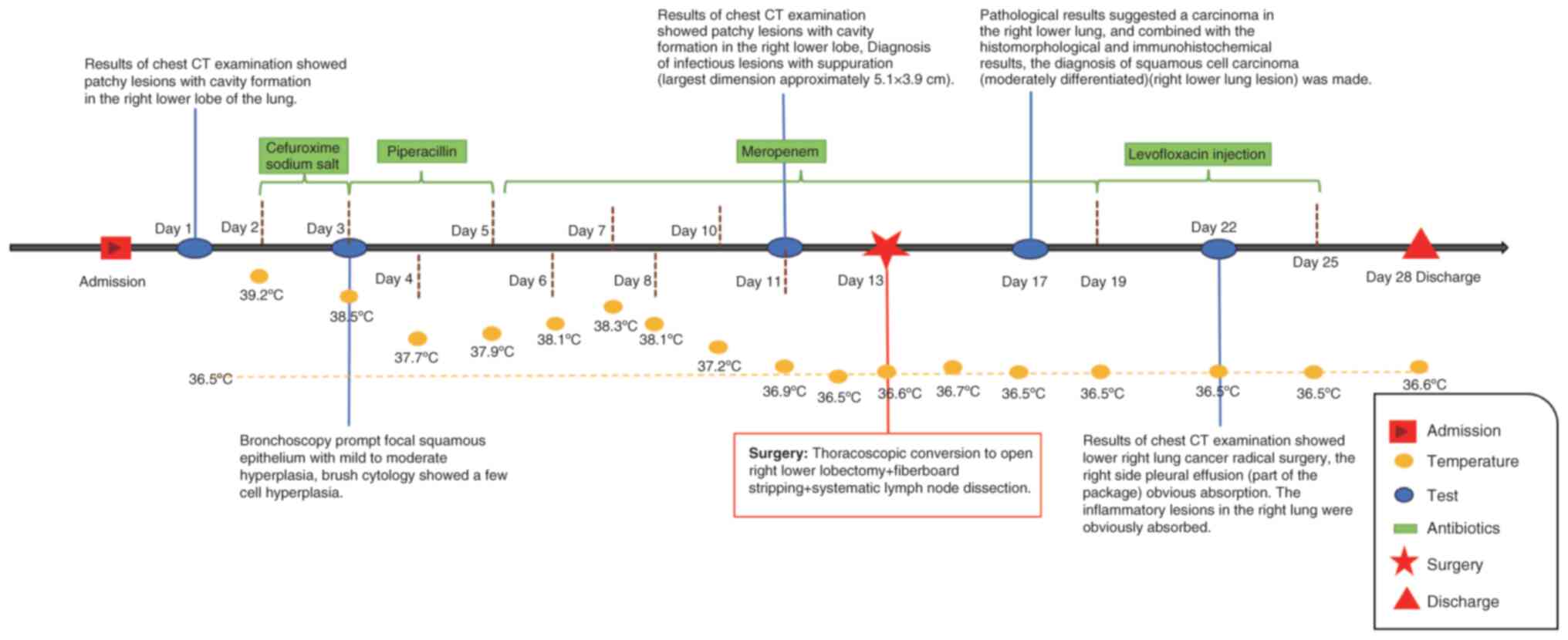
Determining the optimal timing for surgery in cases
of lung cancer complicated by LA is a topic deserving further
investigation. Studies suggest that patients exhibiting relatively
stable vital signs also demonstrate a favorable prognosis (24). Delaying surgery until vital signs
stabilize while the primary lung tumor advances may lead to missed
optimal surgical timing in lung cancer cases, attributable to
hesitancy. Thus, the primary focus is on actively managing the
patient's temperature and infection indicators, enhancing overall
patient condition, and conducting surgery under optimal
circumstances. Even in individuals with advanced non-small cell
lung cancer complicated by LA, a favorable prognosis can be
attained through thorough preoperative preparation and judicious
selection of the surgical timing (25). The diagnostic and treatment
timelines of the present case are illustrated in Fig. 6.
Throughout the hospitalization period, the patient
presented with a sustained high fever, with initial assessments
indicating potential inadequacy in infection management with the
broad-spectrum antibiotic cefuroxime sodium, alongside
complications stemming from the coexistence of lung cancer and an
LA. Research has indicated that the combination of a tumor
complicated by an LA, coupled with pathogen resistance to
antibiotics, represents the primary factor contributing to the
ineffectiveness of conservative antibiotic therapy for LAs
(26). At 11 days post-admission,
sputum bacterial culture and susceptibility testing revealed that
the patient's Serratia marcescens infection was resistant to
amoxicillin, cefuroxime and cefotaxime, while being susceptible to
ceftriaxone, ceftazidime, levofloxacin, imipenem, and meropenem.
The resistance of Serratia marcescens to cefuroxime sodium
resulted in a delayed reduction in the patient's temperature.
Following a switch to meropenem for a 3-day course of
anti-infective therapy, a gradual decline in the patient's
temperature was observed. Nevertheless, as the primary infection
site was not entirely eradicated, the infection remained
incompletely controlled. Following the normalization of the
patient's temperature, surgical intervention was promptly
conducted. Despite the inflammatory markers not exhibiting a
decrease at that juncture, the persistent nature of the infection,
attributed to lung cancer, posed challenges in achieving control.
With the lung cancer advancing, delaying surgery risked missing the
optimal timing; consequently, surgery was performed on the 14th day
post-admission. Following the surgery, the patient experienced
amelioration in the cough and hemoptysis symptoms, alongside a
gradual normalization of infection markers. Subsequently, the
patient was discharged at 2 weeks post-surgery. Research has
indicated that early screening and surgical intervention for lung
cancer complicated by LA can yield favorable outcomes (7,14).
Given the favorable prognosis observed in the patient, the surgical
timing in this instance appears to have been appropriately chosen.
Following discharge, the patient received regular follow-up care
and maintained a normal lifestyle, undergoing periodic
reevaluations. Subsequent reexaminations revealed no discernible
abnormalities, the absence of tumor recurrence and the absence of
any postoperative adverse events. The imaging data from the
surgical intervention were not adequately retained, and so cannot
provide a comprehensive visualization of the entire lung within the
thoracic cavity. Consequently, there remains a deficiency in
evidence-based medical data to substantiate the study conclusions.
This summary encapsulates the treatment experience in this unique
case and juxtaposes it with similar cases from the past, with the
goal of proposing a novel clinical treatment approach for this
disease subtype to enhance patient outcomes. From a clinical
perspective, further research and data are imperative to
substantiate or identify improved treatment modalities.
In conclusion, we recommend that in cases of lung
cancer complicated by LA, prompt surgical intervention should be
considered once the body temperature normalizes and the infection
is partially controlled, as this approach may lead to improved
prognostic outcomes.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This research was supported by grants from the National Natural
Science Foundation of China (Regional Foundation) (no.
gyfyhsfc-2022-40) and the Department of Science and Technology of
Guizhou Province [Qianhe Foundation-ZK no. (2023) General 363].
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JL and YBL guided the conception and design of the
study. YBL, XSL and YPT collected and analyzed clinical data and
figures. YBL was responsible for writing the draft. XSL and YPT
revised the manuscript. YBL conducted the second round of image
acquisition and modifications. JL, YBL, XSL and YPT confirm the
authenticity of all the raw data. All authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
the publication of this case report and associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yazbeck MF, Dahdel M, Kalra A, Browne AS
and Pratter MR: Lung abscess: Update on microbiology and
management. Am J Ther. 21:217–221. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hraiech S, Ladjal K, Guervilly C, Hyvernat
H, Papazian L, Forel JM, Lopez A, Peres N, Dellamonica J, Leone M
and Gragueb-Chatti I: Lung abscess following ventilator-associated
pneumonia during COVID-19: A retrospective multicenter cohort
study. Crit Care. 27:3852023. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kuhajda I, Zarogoulidis K, Tsirgogianni K,
Tsavlis D, Kioumis I, Kosmidis C, Tsakiridis K, Mpakas A,
Zarogoulidis P, Zissimopoulos A, et al: Lung abscess-etiology,
diagnostic and treatment options. Ann Transl Med.
3:1832015.PubMed/NCBI
|
|
4
|
Sperling S, Dahl VN and Floe A: Lung
abscess: An update on the current knowledge and call for future
investigations. Curr Opin Pulm Med. 30:229–234. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Vaarst JK, Sperling S, Dahl VN, Floe A,
Laursen CB, Gissel TN, Gjoerup PH and Bendstrup E: Lung abscess:
Clinical characteristics of 222 Danish patients diagnosed from 2016
to 2021. Respir Med. 216:1073052023. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang H, Liu Q, Lei Y, Zhou J, Jiang W,
Cui Y, He Q, Zhu J, Zhu Z, Sun Y and Ke Z: Direct interaction
between CD155 and CD96 promotes immunosuppression in lung
adenocarcinoma. Cell Mol Immunol. 18:1575–1577. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee JH, Hong H, Tamburrini M and Park CM:
Percutaneous transthoracic catheter drainage for lung abscess: A
systematic review and meta-analysis. Eur Radiol. 32:1184–1194.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang S, Wu L and Xu L, Huang X, Sun X,
Yang L and Xu L: Lung abscess secondary to lung cancer with a
coinfection of Granulicatellaadiacens and other bacteria: A case
report. BMC Infect Dis. 21:pp. 6622021, View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rivera C, Arame A, Pricopi C, Riquet M,
Mangiameli G, Abdennadher M, Dahan M and Le Pimpec Barthes F:
Pneumonectomy for benign disease: Indications and postoperative
outcomes, a nationwide study. Eur J Cardiothorac Surg. 48:435–440.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Evans SS, Repasky EA and Fisher DT: Fever
and the thermal regulation of immunity: The immune system feels the
heat. Nat Rev Immunol. 15:335–349. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sulyok I, Fleischmann E, Stift A, Roth G,
Lebherz-Eichinger D, Kasper D, Spittler A and Kimberger O: Effect
of preoperative fever-range whole-body hyperthermia on
immunological markers in patients undergoing colorectal cancer
surgery. Br J Anaesth. 109:754–761. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Goldstraw P, Chansky K, Crowley J,
Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P,
Mitchell A, Bolejack V, et al: The IASLC lung cancer staging
project: Proposals for revision of the TNM stage groupings in the
forthcoming (Eighth) edition of the TNM classification for lung
cancer. J Thorac Oncol. 11:39–51. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wood DE, Kazerooni EA, Baum SL, Eapen GA,
Ettinger DS, Hou L, Jackman DM, Klippenstein D, Kumar R, Lackner
RP, et al: Lung cancer screening, version 3.2018, NCCN clinical
practice guidelines in oncology. J Natl Compr Canc Netw.
16:412–441. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sidorenkov G, Stadhouders R, Jacobs C,
Mohamed Hoesein FAA, Gietema HA, Nackaerts K, Saghir Z, Heuvelmans
MA, Donker HC, Aerts JG, et al: Multi-source data approach for
personalized outcome prediction in lung cancer screening: Update
from the NELSON trial. Eur J Epidemiol. 38:445–454. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rolston KVI and Nesher L: Post-obstructive
pneumonia in patients with cancer: A review. Infect Dis Ther.
7:29–38. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shirley RM and Baddley JW: Cryptococcal
lung disease. Curr Opin Pulm Med. 15:254–260. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sui X, Huang Y, Song W, Zheng F, Wang X,
Xu X, Wang Z, Jiang J and Jin Z: Clinical features of pulmonary
cryptococcosis in thin-section CT in immunocompetent and non-AIDS
immunocompromised patients. Radiol Med. 125:31–38. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Neacşu F, Vârban AŞ, Simion G, Şurghie R,
Pătraşcu OM, Sajin M, Dumitru M and Vrînceanu D: Lung cancer
mimickers-a case series of seven patients and review of the
literature. Rom J Morphol Embryol. 62:697–704. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Han JY, Lee KN, Lee JK, Kim YH, Choi SJ,
Jeong YJ, Roh MS and Choi PJ: An overview of thoracic
actinomycosis: CT features. Insights Imaging. 4:245–252. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ngu S, Narula N, Abureesh M, Li JJ and
Chalhoub M: Endobronchial aspergilloma-a comprehensive literature
review with focus on diagnosis and treatment modalities. Eur J Clin
Microbiol Infect Dis. 39:601–605. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Baker RR: The treatment of lung abscess.
Current concepts. Chest. 87:709–710. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hou GJ, He Y and Zhao P: Video-assisted
thoracoscopic left upper lobectomy and broncho-and-angioplasty for
a giant central lung cancer complicated with intratumoral abscess:
One case report. J Thorac Dis. 10:pp. 4484–4486. 2018, View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hu L, Lin J, Li J, Cao Y and Lin L: Lung
abscess secondary to lung cancer with Eikenella corrodens and
Streptococcus anginosus: A case report. BMC Infect Dis. 20:pp.
3512020, View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Reimel BA, Krishnadasen B, Cuschieri J,
Klein MB, Gross J and Karmy-Jones R: Surgical management of acute
necrotizing lung infections. Can Respir J. 13:369–373. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yamanashi K, Okumura N, Takahashi A,
Nakashima T and Matsuoka T: Surgical and survival outcomes of lung
cancer patients with intratumoral lung abscesses. J Cardiothorac
Surg. 12:442017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Desai H and Agrawal A: Pulmonary
emergencies: Pneumonia, acute respiratory distress syndrome, lung
abscess, and empyema. Med Clin North Am. 96:1127–1148. 2012.
View Article : Google Scholar : PubMed/NCBI
|