Introduction
Osteosarcoma is a mesenchymal tumor of the bones,
typically occurring in the long bones of the extremities.
Osteosarcoma in the long bones of the extremities accounts for
~80–90% of all cases of osteosarcoma (1). By contrast, two of the rarest sites
for this disease to be diagnosed are the hand and the foot,
representing ~1% of all diagnosed osteosarcomas (2–4). The
rarity of osteosarcoma of the hand and foot has led to frequent
misdiagnosis, delayed diagnosis or inappropriate treatment of
patients, which can have fatal consequences (5). The uncommon occurrence of osteosarcoma
of the hand and foot, its similar appearance to benign lesions and
the general lack of awareness of this disease may result in
physicians not immediately suspecting osteosarcoma when evaluating
patients. Delays in diagnosing and treating peripheral osteosarcoma
can have a negative impact on patient outcomes. These delays may
reduce treatment options and diminish the possibility of
limb-sparing procedures, potentially affecting the overall
prognosis and quality of life of patients. Previous studies have
raised contradictions about the prognosis and treatment of hand and
foot osteosarcoma when compared with that at other common sites
(6). This condition primarily
affects adolescents and young adults, with the majority of cases
occurring between the ages of 10 and 25. However, it can also
affect older adults (7). Outcomes
for this disease typically have a favorable prognosis, but there
are currently few reports on hand and foot osteosarcoma (8). In the hand and foot, salvaging the
limb is typically the treatment of choice, and with the use of
chemotherapy (CHT), 60–65% of patients with osteosarcoma can be
cured without amputation (1,9).
Currently, there is a lack of comprehensive
understanding and published data regarding the diagnosis, treatment
and outcomes of osteosarcoma in the hand and foot, as these cases
represent ~1% of all osteosarcomas. Due to its rarity, misdiagnosis
and treatment delays are common, yet detailed reviews and analyses
of such cases are limited. To build upon the limited existing
literature, the present study conducted a series of single-center
case reports on a group of patients treated at the Masaryk Memorial
Cancer Institute Sarcoma Center (Brno, Czechia). The present
retrospective cohort study aimed to review and analyze cases of
osteosarcoma located in the hand and foot. Furthermore, certain
patient cases were described to highlight key educational points,
including unexpected outcomes, misdiagnoses and failed
interventions. These case reports may offer valuable insights into
treatment efficacy, diagnostic challenges and rare complications of
hand and foot osteosarcoma. By identifying common misdiagnoses and
raising awareness of the rarity of hand and foot osteosarcoma, the
present study may contribute to more accurate and timely diagnoses,
preventing delays in treatment.
Materials and methods
Study design and patient
selection
The present retrospective study selected data from
patients diagnosed with osteosarcoma of the hand and foot. Between
January 2007 and January 2019, 11 patients were treated at the
Masaryk Memorial Cancer Institute Sarcoma Center, with 5 cases
involving the hand and 6 involving the foot (Table I).
 | Table I.Patient demographics. |
Table I.
Patient demographics.
| Demographic | Value |
|---|
| Total number of
patients, n | 11 |
| Mean age at inclusion
(SD), years | 30.9 (16.74) |
| Sex, n (%) |
|
| Male | 6 (54.5) |
|
Female | 5 (45.5) |
| Mean follow-up period
(SD), months | 90.36 (66.14) |
| Comorbidities, n
(%) |
|
|
Yes | 2 (18.2) |
| No | 9 (81.8) |
| Mean symptom
duration (SD), months | 8.91 (3.80) |
Patient cohort and data
collection
The present study included 6 male patients and 5
female patients, with a mean age of 30.9±16.74 years. Clinical
features, outcomes, and related treatments were examined. The
disease-free survival period and overall survival rate were
calculated.
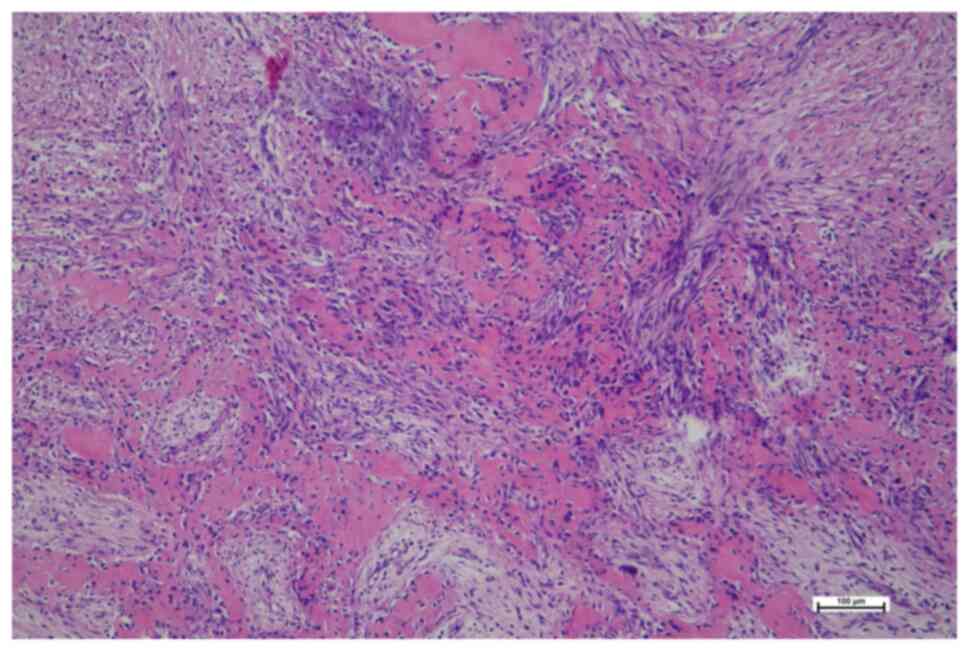
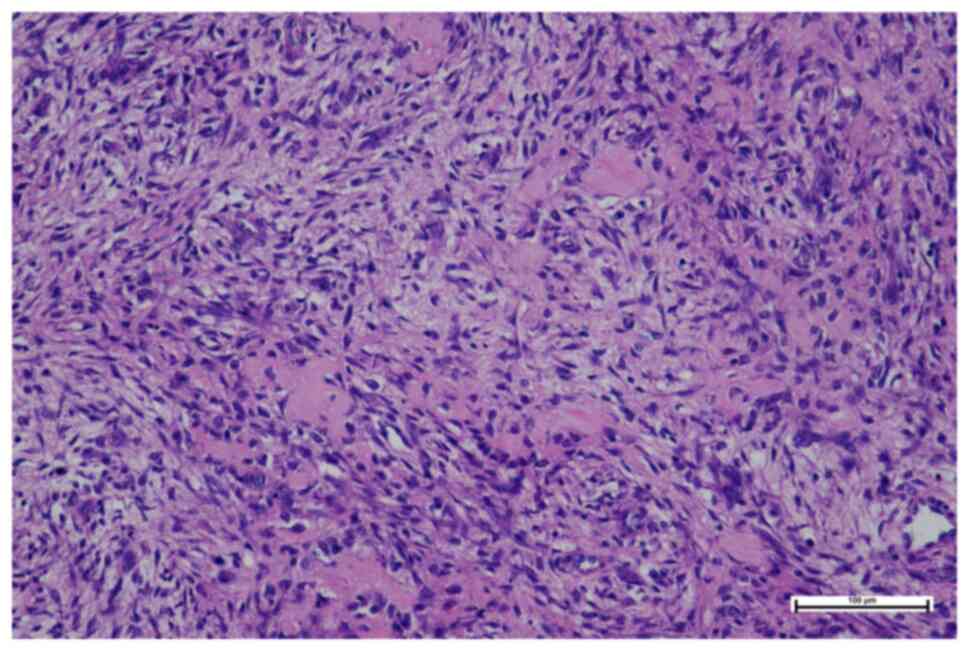
Histopathological review
Histological diagnoses were reviewed by an
experienced musculoskeletal oncology pathologist. The diagnoses
were confirmed using hematoxylin and eosin and immunohistochemical
(IHC) staining.
The received tissue was macroscopically inspected,
and representative samples were fixed in 10% neutral buffered
formalin for 24 h. Subsequently, the tissue samples were processed
using the Tissue Processor TPC15 (Bamed sro), involving alcohol,
isopropylene and xylene washes, followed by embedding in paraffin
at a constant temperature of 60°C. The entire process took 14.25 h,
with paraffin embedding taking the final 3.75 h. Calcified/ossified
components were decalcified by submerging them in a 10% EDTA
solution for 2–3 days before embedding.
The FFPE tissue was then sectioned into 4-µm thick
sections and routinely processed with hematoxylin-eosin staining
for 104 min at 60°C using Automatic stainer and coverslipper E7 or
Staining apparatus Medite TST44 in combination with Film
coverslipper Medite Twister (all Bamed sro). The stained tissue was
subsequently examined under a standard light microscope (Olympus
BX45; Olympus Corporation) at ×20, ×40, ×100 and ×200
magnification.
IHC analysis of SATB2, S100, Histone H3G34W and p63
expression was performed on tumor tissue sections using the
Automated IHC/ISH Slide Staining System BenchMarkXT (• Roche Tissue
Diagnostics). The ultraView Universal DAB Detection Kit (Roche
Tissue Diagnostics) was used for staining according to the
manufacturer's instructions. The 4-µm thick tumor tissue sections
were applied to positively charged TOMO® slides
(Matsunami Glass Ind., Ltd.). The following antibodies and
conditions were used for staining: i) SATB2 Rabbit Monoclonal
Antibody (clone EP281; cat. no. 384R-16; Cell Marque;
MilliporeSigma) at 1:100 dilution; cell conditioning Ultra CC1 for
36 min at 95°C; antibody incubation for 32 min at 37°C. ii) S100
Rabbit Polyclonal Antibody (cat. no. Z0311; Dako; Agilent
Technologies, Inc.) at 1:1,000 dilution; cell conditioning Ultra
CC1 for 20 min at 95°C; antibody incubation for 28 min at 37°C.
iii) Histone H3G34W Antibody (clone RM263; cat. no. 31-1145-00-S;
RevMAb Biosciences USA, Inc.) at 1:200 dilution; cell conditioning
Ultra CC1 for 76 min at 95°C; antibody incubation for 32 min at
37°C. iv) p63 Antibody (clone 4A4; cat. no. 05867061001; Roche
Diagnostics GmbH), ready-to-use; cell conditioning Ultra CC1 for 72
min at 100°C; antibody incubation for 36 min at 37°C.
The ultraView Universal DAB Detection Kit (Roche
Diagnostics GmbH) was used to detect expression for all the
aforementioned antibodies. Each run included a system of negative
and positive controls. Negative controls were prepared by
incubating samples without the primary antibody, while positive
control tissue samples were used to verify the staining. The
positive tissue controls were taken from residual tissue samples
obtained via biopsy/autopsy from different (already closed) cases.
All IHC results were evaluated using a uniform microscope and
camera setting (Olympus BX45 microscope and Olympus DR72 camera;
Olympus Corporation).
Follow-up and assessment
Postoperative follow-up assessments were conducted
at regular intervals every 3 months during the first 2 years, every
6 months for the next 3 years and annually thereafter. Each
follow-up included a clinical examination, plain radiographs of the
primary tumor site, chest CT scans, and, as needed based on the
clinical examination and radiograph findings, MRI of the primary
tumor site. Patients underwent follow-up appointments for a minimum
of 5 years, with a mean follow-up duration of 90.36 (±66.14)
months.
Ethical considerations and treatment
planning
The institutional review board approved the present
retrospective study, and written consent was obtained from all
patients or their legal guardians. Each case was presented to the
multidisciplinary Musculoskeletal Tumor Committee for treatment
planning and management.
Statistical analysis
Statistical analysis was performed using R software
(version 4.0.5; Posit Software, PBC) in the RStudio development
environment. Descriptive statistics were used to summarize patient
demographics, clinical characteristics, tumor size,
histopathological findings and survival rates. Categorical
variables, such as sex, tumor grade and histological type, were
reported as frequencies and percentages. Continuous variables,
including patient age, follow-up duration and tumor size, were
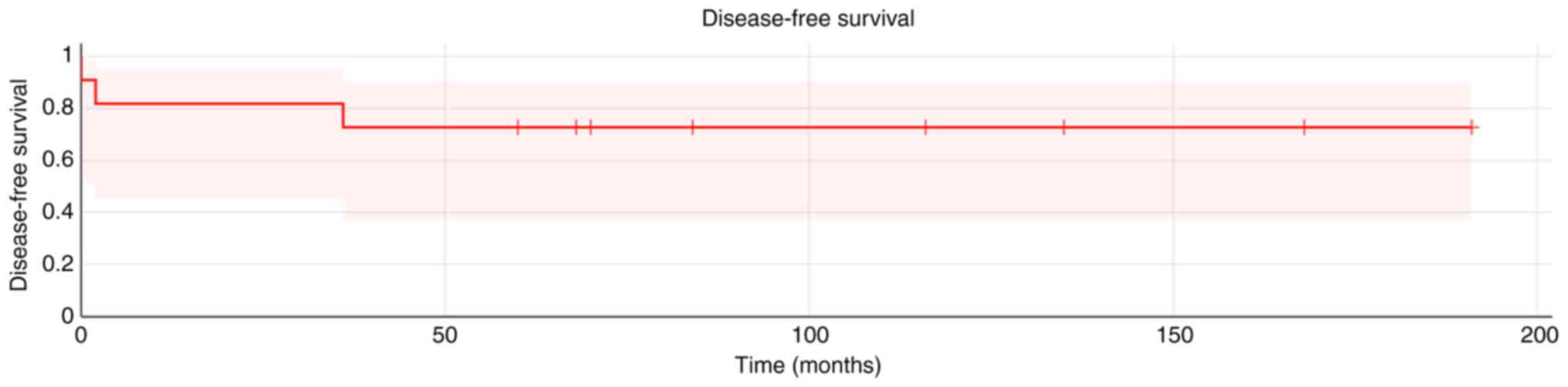
expressed as the mean ± SD. The Kaplan-Meier method was used to
estimate overall survival and disease-free survival rates. Mean
survival times and their corresponding 95% CIs were calculated.
Patients were censored at their last known follow-up date or time
of death.
Results
Clinical and pathological
outcomes
The mean tumor size detected during diagnosis was
4.29±1.81 cm. Osteoblastic osteosarcoma was the most common
histopathological type, accounting for 4 cases (33.4%). A majority
of the osteosarcomas were identified as high-grade (81.8%). Only 1
patient exhibited lung metastasis and lymph node infiltration upon
diagnosis (Table II). A total of 5
patients experienced misdiagnoses following the initial biopsy,
with two initially receiving treatment outside the Masaryk Memorial
Cancer Institute Sarcoma Center. The most frequently encountered
misdiagnosis was giant-cell tumor of bone (GCTB). Of the
misdiagnosed patients, 4 patients initially underwent an
intralesional procedure. Only 3 patients received CHT before their
procedure and 3 patients underwent limb amputation. A total of 4
patients underwent ray resection, and 4 underwent en bloc
resection, including an astragalectomy. A total of 2 patients
developed lung metastasis and succumbed to the disease (Table III). The disease-free survival
period was 82.83±60.05 months, while the overall survival rate was
72%, with a mean survival time of 90.36±56.73 months (Fig. 1). The overall survival rate for the
patients with high-grade osteosarcomas was 66%, with a mean
survival time of 85.11±55.89 months.
 | Table II.Tumor characteristics. |
Table II.
Tumor characteristics.
| Tumor feature | Value |
|---|
| Number of tumors,
n | 11 |
| Location, n
(%) |
|
|
Hand | 5 (45.5) |
|
Foot | 6 (54.5) |
| Mean size (SD),
cm | 4.29 (±1.81) |
| Histology, n
(%) |
|
|
Osteoblastic | 4 (33.4) |
|
Giant-cell rich | 3 (27.3) |
|
Fibroblastic | 1 (9.1) |
|
Telangiectatic | 1 (9.1) |
|
Chondroblastic | 1 (9.1) |
|
Periosteal | 1 (9.1) |
| Grade, n (%) |
|
|
Low | 1 (9.1) |
|
Intermediate | 1 (9.1) |
|
High | 9 (81.8) |
| Stage, n (%) |
|
| I | 2 (18.2) |
| II | 7 (63.6) |
|
III | 2 (18.2) |
| Lymph node
involvement at diagnosis, n (%) | 1 (9.1) |
| Metastasis at
diagnosis | 1 (9.1) |
 | Table III.Summary of 11 cases of hand or foot
osteosarcoma from the present study. |
Table III.
Summary of 11 cases of hand or foot
osteosarcoma from the present study.
| Patient | Age at diagnosis,
years | Sex | Misdiagnosis | Misdiagnosis
treatment | Histology | Tumor size, cm | Tumor site | Grade | Stage | Metastasis at
diagnosis | Neoadjuvant
CHT | Type of
surgery | Adjuvant CHT | Meta stasis | Event | Additional
therapy | Eventfree survival,
months | Overall survival,
months | Patient status at
time of writing |
|---|
| 1 | 46 | M | Malignant GCTB | N/A | Giantcell rich | 7.0 | IV. MTC | High | III | Lung and
skeletal | N/A | Amputation | N/A | N/A | Death | Palliative CHT | N/A | 12 | Died |
| 2 | 38 | M | N/A | N/A | Fibroblastic | 5.0 | Calca neus | High | II | N/A | N/A | Amputation | Yes | Lung | Death | N/A | 36 | 70 | Died |
| 3 | 11 | F | N/A | N/A | Periosteal | 3.0 | V.MTT | Intermediate | I | N/A | N/A | En bloc
resection and allograft | N/A | N/A | N/A | Suspected local
recurrence biopsy | 60 | 60 | Free of
disease |
| 4 | 26 | F | N/A | N/A | Osteoblastic | 2.5 | III. Digit of the
hand | High | II | N/A | N/A | Ray resection | Yes | N/A | N/A | N/A | 68 | 68 | Free of
disease |
| 5 | 52 | M | Aneurysmal bone
cyst | Astragalectomy | Telangiectatic | 6.5 | Talus | High | II | N/A | Yes | Ampu tation | Yes | N/A | N/A | N/A | 135 | 135 | Free of
disease |
| 6 | 19 | M | Enchondroma | Cure ttage and bone
grafting | Chondro
blastic | 2.5 | V. MTC | High | II | N/A | N/A | Ray resection | Yes | N/A | N/A | N/A | 84 | 84 | Free of
disease |
| 7 | 50 | M | GCTB | Curettage and
cementoplasty | Giantcell rich | 4.0 | Talus | High | III | N/A | N/A | Astraga
lectomy | Yes | Lung | Death | Palliative CHT | 2 | 20 | Died |
| 8 | 17 | M | N/A | N/A | Osteo blastic | 6.0 | IV. MTT | High | II | N/A | Yes | En bloc
resection | Yes | N/A | N/A | N/A | 191 | 191 | Free of
disease |
| 9 | 14 | F | GCTB | Curettage and bone
grafting | Osteo blastic | 2.0 | II. MTT | Low | I | N/A | N/A | Ray resection | N/A | N/A | N/A | N/A | 168 | 168 | Free of
disease |
| 10 | 34 | F | N/A | N/A | Osteoblastic | 3.0 | IV. digit of the
hand | High | II | N/A | N/A | Ray resection | Yes | N/A | N/A | N/A | 70 | 70 | Free of
disease |
| 11 | 19 | F | N/A | N/A | Giantcell rich | 3.0 | II. MTT | High | II | N/A | Yes | En bloc
resection | Yes | N/A | N/A | N/A | 116 | 116 | Free of
disease |
Case presentation
Case 1
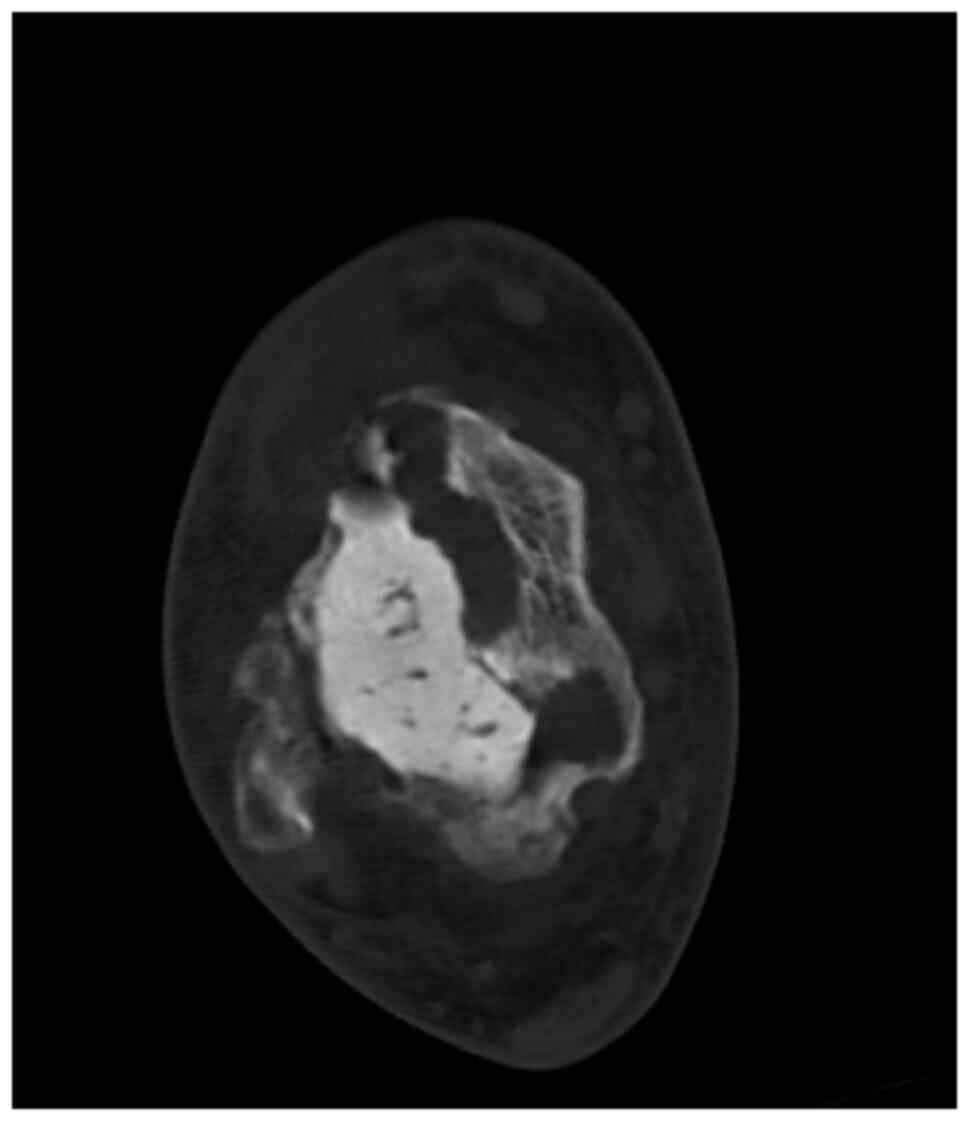
A 26-year-old female patient presented to a local
surgical department in the Moravian-Silesian region with a 3-month
history of persistent pain and swelling in the middle finger of
their left hand. An incision was made under local anesthesia, but
the lesion eventually ulcerated and in March 2018, the patient was
referred to the Masaryk Memorial Cancer Institute Sarcoma Center
(Brno, Czechia) for further evaluation. CT scans demonstrated an
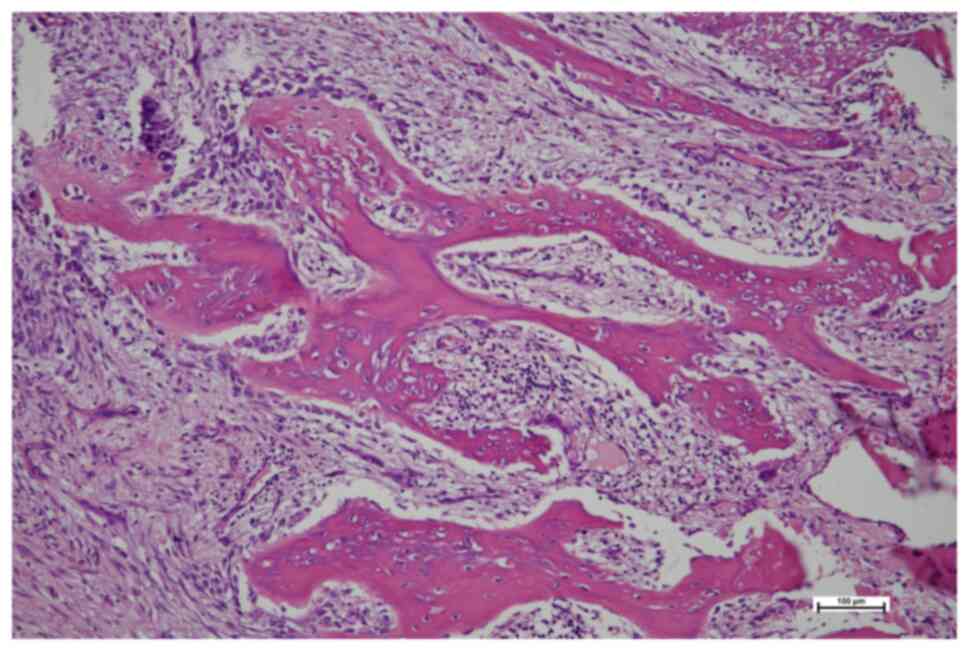
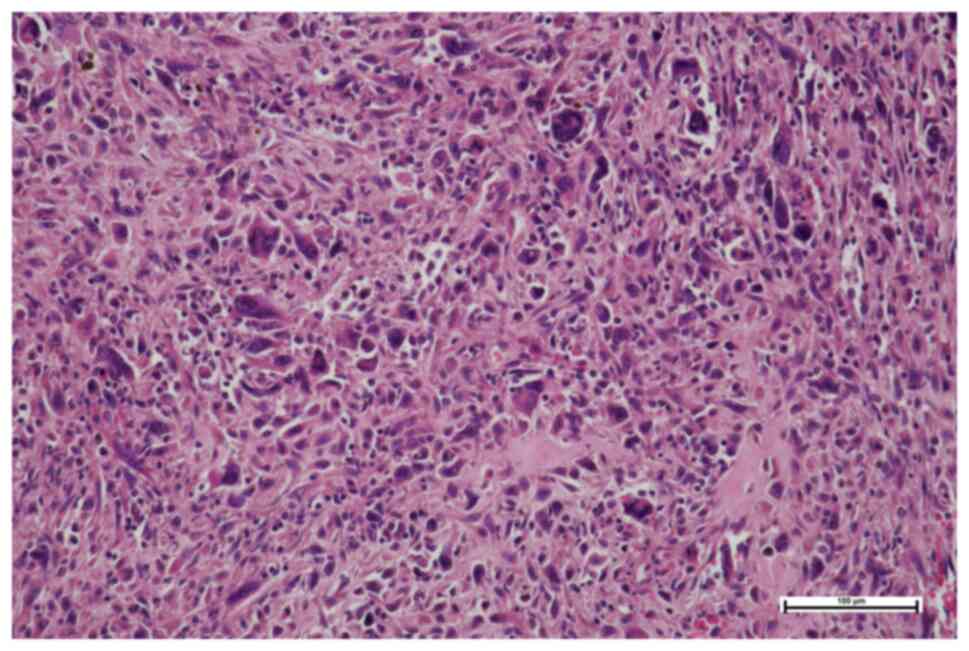
osteoblastic lesion in the middle phalanx (Fig. 2) and histopathology confirmed the
diagnosis of high-grade parosteal osteosarcoma (Fig. 3). The Musculoskeletal Tumor
Committee recommended resection of the third ray, which was
performed successfully (Fig. 4).
The final histopathology report indicated high-grade osteoblastic
osteosarcoma and a complete resection (Fig. 5). Following the surgery, the patient
underwent four cycles of the standard combination CHT regimen
(10), comprising high-dose
methotrexate (12 g/m2), doxorubicin (75
mg/m2) and cisplatin (120 mg/m2). However,
due to toxicity, the regimen was interrupted. Treatment was then
adjusted to two additional cycles of monotherapy, with doxorubicin
reduced (50 mg/m2) and methotrexate continued at 12
g/m2. At follow-up examinations, the patient remained
disease free. However, 5 years after the surgical procedure, the
patient died due to a sudden cardiac arrest, which was potentially
related to the cardiotoxic effects of the CHT.
Case 2
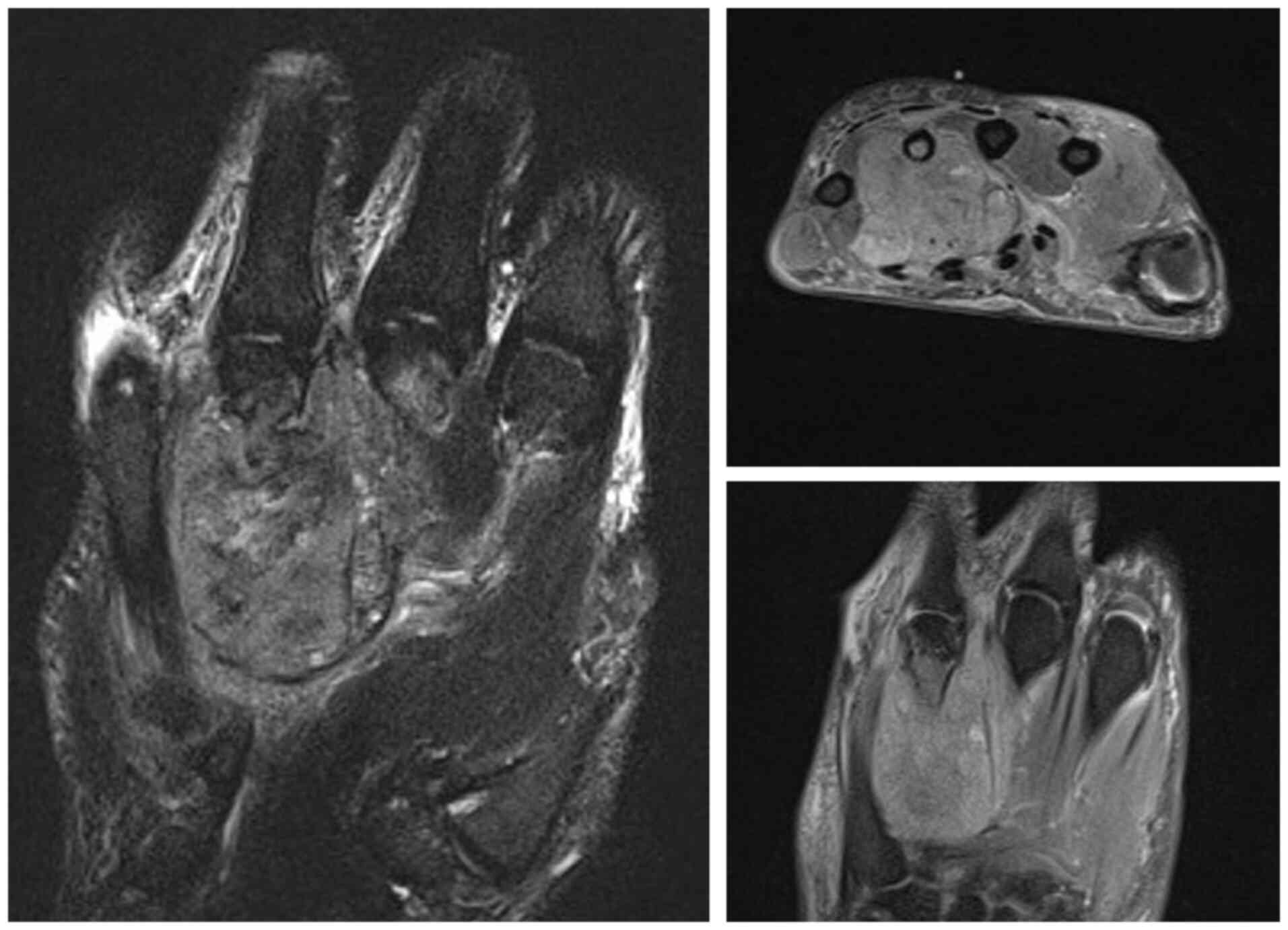
In September 2019, a 46-year-old male patient
presented to the Masaryk Memorial Cancer Institute Sarcoma Center
(Brno, Czechia) with a 3-month history of pain and swelling in the
left hand and wrist. Computed radiography (CR) and MRI scans showed
an osteolytic lesion on the base of the fourth metacarpal bone and
carpal bones (Fig. 6). The
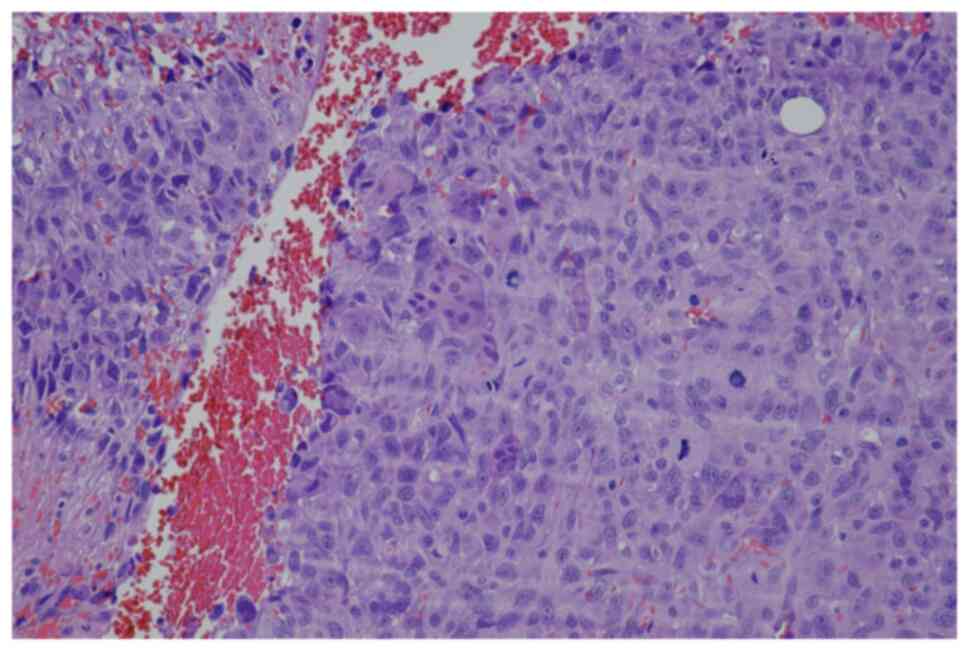
histopathology report indicated a primary malignant GCTB (Fig. 7). CT scans and radiographic imaging
showed infiltration of lymph nodes, as well as metastases to the
lungs (Fig. 8) and skeleton
(Fig. 9). The Musculoskeletal Tumor
Committee recommended a radical approach, suggesting amputation of
the affected area followed by palliative CHT. The final
histopathology report confirmed the presence of a 55-mm high-grade
giant cell-rich osteosarcoma (Fig.
10), which was successfully removed through complete resection.
The patient passed away 1-year after the surgery.
Case 3
In January 2019, an 11-year-old female was referred
to the Masaryk Memorial Cancer Institute Sarcoma Center with a
2-month history of pain in the right foot. MRI scans showed a 3 cm
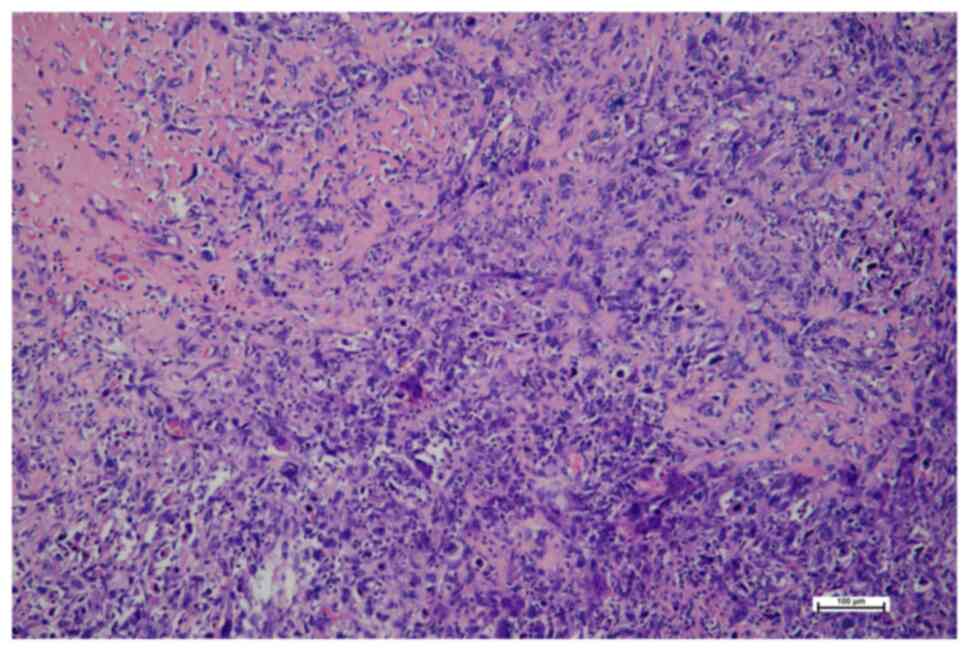
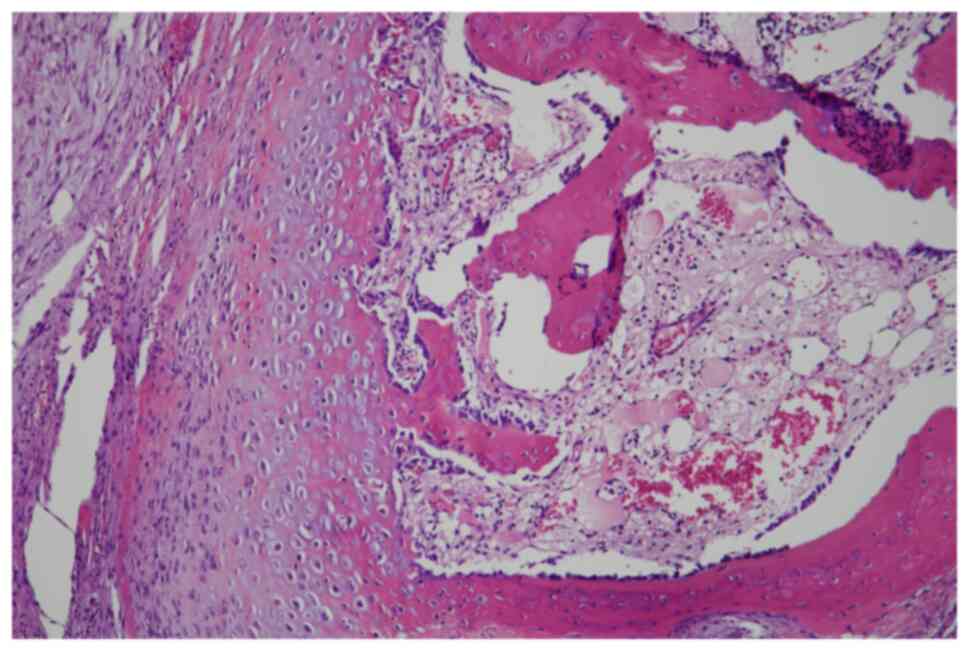
thickening of the bone in the V. metatarsal diaphysis (Fig. 11). The histopathology report showed
an intermediate-grade periosteal osteosarcoma (Fig. 12). The patient had no lymph node
involvement or metastases. The Musculoskeletal Tumor Committee
recommended en bloc resection with bone allograft
reconstruction using a plate. The final histopathology report
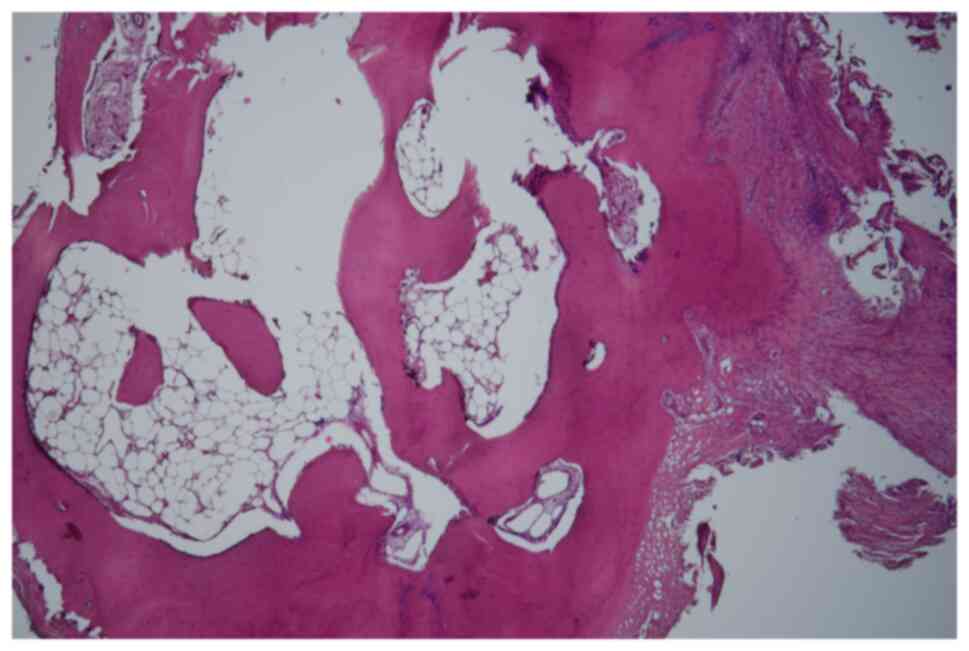
confirmed the initial findings from the biopsy (Fig. 13). After 2 years, a follow-up plain
radiographs showed ossification on the allograft surface (Fig. 14), leading to a biopsy to check for
any signs of local recurrence. The biopsy results showed no
evidence of malignancy (Fig. 15).
At the time of writing, the patient completed 5 years of follow-up
appointments with no signs of disease recurrence.
Case 4
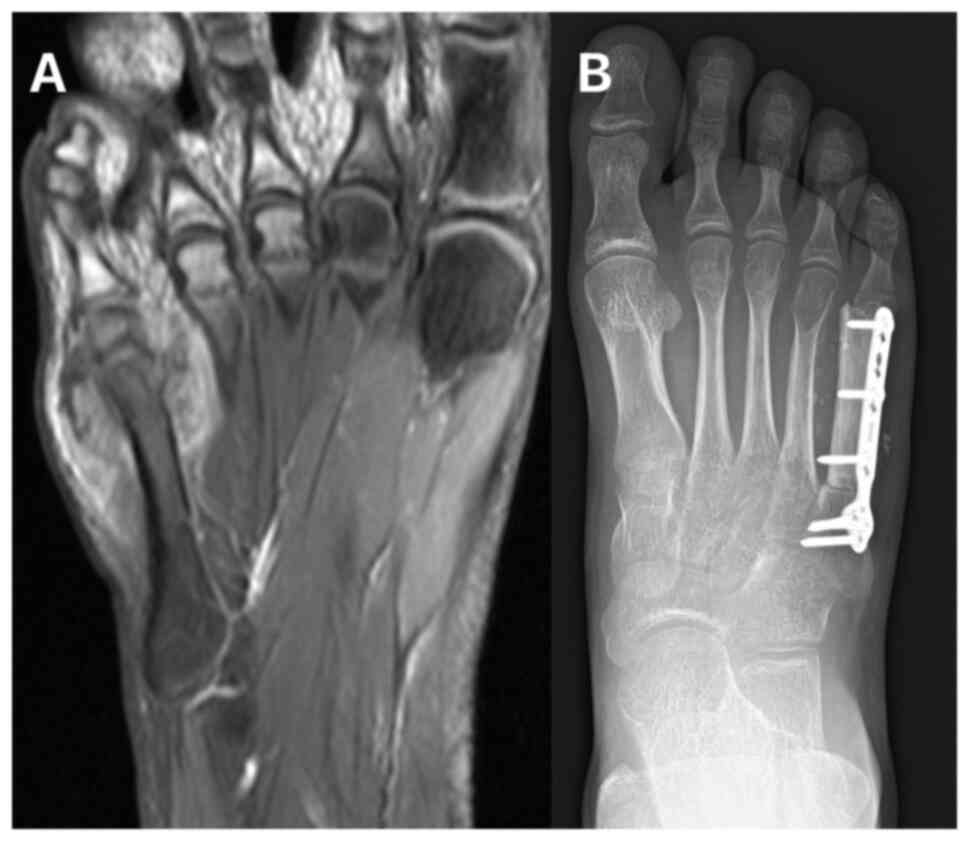
In June 2007, a 50-year-old male presented to the
Masaryk Memorial Cancer Institute Sarcoma Center, with a 1-month
history of persistent pain in the right ankle. Further
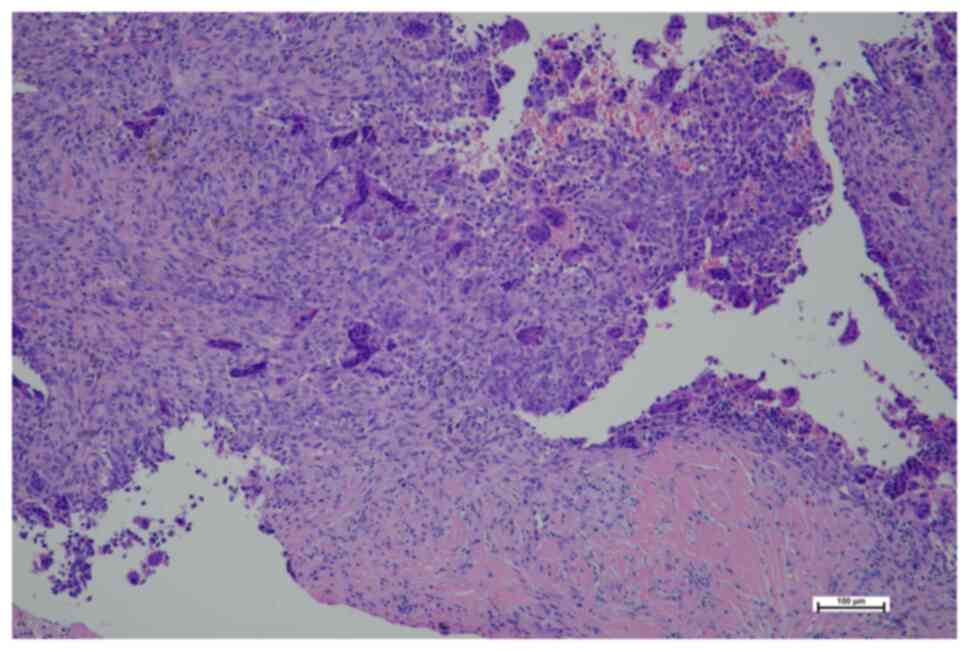
investigations showed a cystic lesion of the talus on a CR scan,
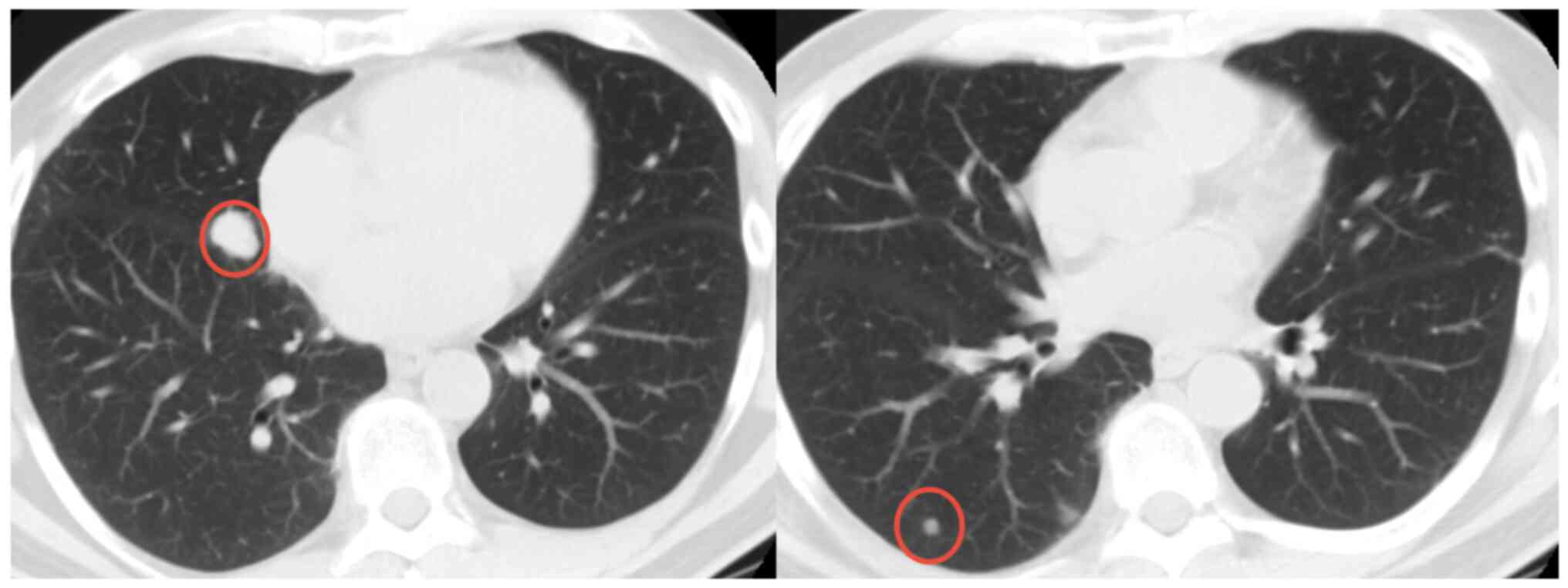
which was later confirmed by a supplementary CT scan (Fig. 16). The histopathology report
diagnosed GCTB with a secondary aneurysmal cyst of the talus
(Fig. 17), leading to a
recommendation for intralesional resection with bone cement
augmentation. After receiving the recommended treatment, the
patient returned 5 months later with swelling and increased pain in
the ankle. A follow-up CT scan showed destruction of the bone
surrounding the bone cement, as well as osteolysis of the calcaneus
and the presence of an extraosseous mass proximally (Figs. 16 and 18). Due to the extent of osteolysis, the
patient required an astragalectomy. Subsequent histopathology
reports showed a diagnosis of giant-cell rich osteosarcoma,
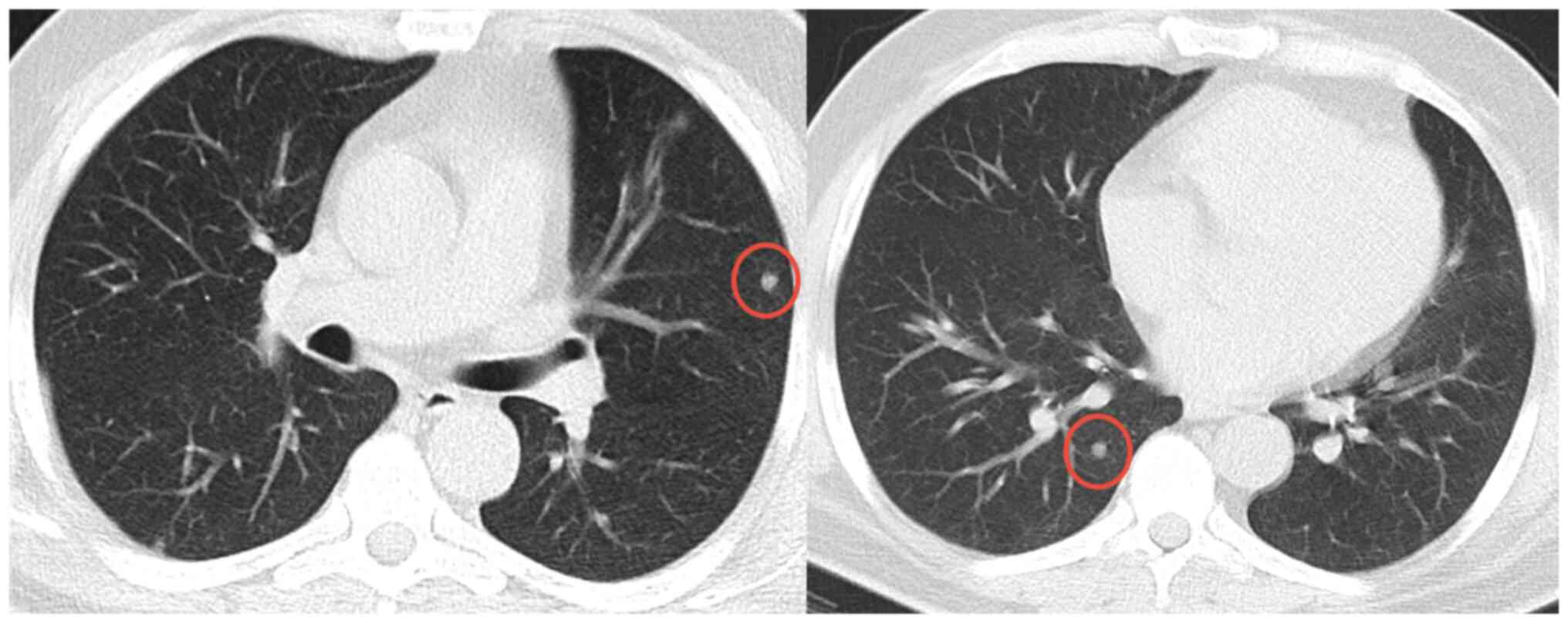
contradicting the initial findings (Fig. 19). Further staging scans indicated
the presence of lung metastases (Fig.
20). The Musculoskeletal Tumor Committee recommended
metastasectomy followed by adjuvant CHT. Despite the successful
removal of 12 lung metastases, the patient developed additional
lung metastases within two months. Despite palliative care efforts,
the patient died 6 months later.
Discussion
The occurrence of osteosarcoma in the hand and foot
regions is a rare clinical presentation, and patients with this
presentation of disease are diagnosed at an average age of nearly
10 years older than patients with osteosarcoma of the long bones.
This aligns with the general trend of osteosarcoma affecting an
older demographic in these specific body areas (11). Upon histological examination, low
grade (9.1%) and intermediate (9.1%) osteosarcomas are more common
in the distal extremities, in contrast to the typical distribution
observed in conventional osteosarcoma (11,12).
The occurrence of sarcomas in atypical anatomical locations has
been documented in previous reports (13,14).
There is a notable difference in the duration of
symptoms before diagnosis. Typically, osteosarcomas present
symptoms for <6 months in most cases (15). However, the findings of the present
study showed an average symptomatic duration of 9 months, which was
longer than the typical duration of symptoms for this disease.
Diagnostic delays for osteosarcomas in the distal skeleton have
been reported, with a number of patients being treated initially
for other conditions, such as GCTB (16,17).
In the present study, 1 patient presented with
metastatic disease at the time of diagnosis, which represented a
higher rate than previously reported (16). All patients who died from the
disease had high-grade osteosarcomas. The overall survival rate for
high-grade variants was 66%, similar to those reported for
osteosarcomas of the long bones. Development of distant metastases
occurred regardless of the surgical approach used (18). The treatment for high-grade
osteosarcomas in the hands and feet should include neoadjuvant and
adjuvant CHT, along with aggressive surgery (12). A number of patients in the present
study required amputation, with the procedure being performed in
27.3% of cases.
The present study had several limitations. The first
was the study's retrospective design. The second was the small size
of the cohort, which included 11 cases, due to the rare nature of
the diagnosis of osteosarcoma of the hands and feet, which
restricted the generalizability of the findings. The present study
was conducted in a specific department with particular surgical
practices and patient populations. This may potentially limit the
applicability of the results to other settings or patient
demographics. However, osteosarcoma of the hand and foot is
particularly rare, and the majority of publications on peripheral
osteosarcoma consist of case reports or studies with ≤23 cases.
Multicenter studies also feature a limited number of patients
(16,19). The present study contributes to the
limited literature on peripheral osteosarcoma with practical
implications for treating cases involving the hand and foot. By
identifying common misdiagnoses and raising awareness about the
existence of osteosarcoma in these locations, even with a small
cohort, the present study could potentially enhance diagnostic
accuracy and timeliness, thereby preventing delays in
treatment.
Future perspectives on osteosarcoma diagnosis and
management could be advanced significantly by integrating
artificial intelligence (AI). AI-powered algorithms can be used to
analyze medical imaging modalities with greater accuracy and
efficiency compared with conventional methods that rely on human
expertise and interpretation (20).
Machine learning models, trained to recognize subtle patterns and
abnormalities in bone structures, may enable the earlier detection
of osteosarcoma, identifying indicators that may elude human
interpretation. Furthermore, AI-driven robotic systems can enhance
surgical precision, minimizing human error and improving outcomes
for patients undergoing bone resection and reconstruction (21).
In summary, a study was conducted on a case series
of 11 patients diagnosed with osteosarcoma of the hand and foot.
The present study described the treatment approach, clinical
characteristics and outcomes of these patients. A total of four
case studies of patients with osteosarcoma in these locations were
also presented. The present study demonstrated that misdiagnosis of
osteosarcoma of the hand and foot often led to patients being
administered with an incorrect treatment initially. The prognosis
of patients in the present study aligned with existing literature
and was favorable compared with that of osteosarcomas in other
anatomical regions. The present study adds valuable information to
the existing literature on osteosarcoma of the hand and foot by
providing essential data on clinical outcomes from a sarcoma
center, which may potentially help guide clinicians towards
effective treatment strategies for these patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MM, VA, DA, PM and DZ were responsible for the
writing and editing of the manuscript, and geneated the graph and
tables. MM, DA and PM were responsible for the methodology and data
collection. DA and MM were responsible for supervision of the
project. MM obtained resources and performed formal data analysis,
and VA was responsible for conceptualization of the study and
performing formal data analysis. LP and ISZ were responsible for
data collection and visualization and performing the methodology.
DZ contributed to the methodology, as well as the acquisition and
interpretation of data. TT was responsible for the
conceptualization, supervision methodology and formal data
analysis. MM and TT confirm the authenticity of all the raw data.
All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki and approved by the St.
Anne's University Hospital Ethics Committee (approval no.
EK-FNUSA-01/2024; Brno, Czech Republic). Written informed consent
was obtained from the patients or legal guardians.
Patient consent for publication
Patients or their legal guardians provided written
informed consent for publication of the present study.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript, and subsequently, the authors revised
and edited the content produced by the AI tools as necessary,
taking full responsibility for the ultimate content of the present
manuscript.
Glossary
Abbreviations
Abbreviations:
|
CHT
|
chemotherapy
|
|
GCTB
|
giant cell tumor of bone
|
|
CR
|
computed radiography
|
|
AI
|
artificial intelligence
|
References
|
1
|
Picci P: Osteosarcoma (Osteogenic
sarcoma). Orphanet J Rare Dis. 2:62007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Casadei R, Ferraro A, Ferruzzi A, Biagini
R and Ruggieri P: Bone tumors of the foot: Epidemiology and
diagnosis. Chir Organi Mov. 76:47–62. 1991.PubMed/NCBI
|
|
3
|
Eyre R, Feltbower RG, James PW, Blakey K,
Mubwandarikwa E, Forman D, McKinney PA, Pearce MS and McNally RJQ:
The epidemiology of bone cancer in 0–39 year olds in northern
England, 1981–2002. BMC Cancer. 10:3572010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chou LB, Ho YY and Malawer MM: Tumors of
the foot and ankle: Experience with 153 cases. Foot Ankle Int.
30:836–841. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bowen CM, Landau MJ, Badash I, Gould DJ
and Patel KM: Primary tumors of the hand: Functional and
restorative management. J Surg Oncol. 118:873–882. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brotzmann M, Hefti F, Baumhoer D and Krieg
AH: Do malignant bone tumors of the foot have a different
biological behavior than sarcomas at other skeletal sites? Sarcoma.
Mar 20–2013.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee JA, Lim J, Jin HY, Park M, Park HJ,
Park JW, Kim JH, Kang HG and Won Y-J: Osteosarcoma in adolescents
and young adults. Cells. 10:26842021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Choong PFM, Qureshi AA, Sim FH and Unni
KK: Osteosarcoma of the foot: A review of 52 patients at the Mayo
Clinic. Acta Orthop Scand. 70:361–364. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Puri A: Limb salvage in musculoskeletal
oncology: Recent advances. Indian J Plast Surg. 47:175–184. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Whelan JS, Bielack SS, Marina N, Smeland
S, Jovic S, Hook JM, Krailo M, Anninga J, Butterfass–Bahloul T,
Böhling T, et al: EURAMOS-1, an international randomised study for
osteosarcoma: Results from pre-randomisation treatment. Ann Oncol.
26:407–414. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Whelan J, McTiernan A, Cooper N, Wong YK,
Francis M, Vernon S and Strauss SJ: Incidence and survival of
malignant bone sarcomas in England 1979–2007. Int J Cancer.
131:E508–E517. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Anninga JK, Picci P, Fiocco M, Kroon HMJA,
Vanel D, Alberghini M, Gelderblom H and Hogendoorn PCW:
Osteosarcoma of the hands and feet: A distinct clinico-pathological
subgroup. Virchows Arch. 462:109–120. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vrînceanu D, Dumitru M, Ştefan AA,
Mogoantă CA and Sajin M: Giant pleomorphic sarcoma of the tongue
base-A cured clinical case report and literature review. Rom J
Morphol Embryol. 61:1323–1327. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Saifuddin MSAH, Ng CY and Abdullah MS:
Skull base primary ewing sarcoma: A radiological experience of a
rare disease in an atypical location. Am J Case Rep.
22:e9303842021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Taran SJ, Taran R and Malipatil NB:
Pediatric Osteosarcoma: An Updated Review. Indian J Med Paediatr
Oncol. 38:33–43. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schuster AJ, Kager L, Reichardt P,
Baumhoer D, Csóka M, Hecker-Nolting S, Lang S, Lorenzen S,
Mayer-Steinacker R, Kalle TV, et al: High-grade osteosarcoma of the
foot: Presentation, treatment, prognostic factors, and outcome of
23 cooperative osteosarcoma study group COSS patients. Sarcoma.
2018:1–11. 2018. View Article : Google Scholar
|
|
17
|
Biscaglia R, Gasbarrini A, Böhling T,
Bacchini P, Bertoni F and Picci P: Osteosarcoma of the bones of the
foot - An easily misdiagnosed malignant tumor. Mayo Clin Proc.
73:842–847. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kager L, Zoubek A, Pötschger U, Kastner U,
Flege S, Kempf-Bielack B, Branscheid D, Kotz R, Salzer-Kuntschik M,
Winkelmann W, et al: Primary metastatic osteosarcoma: Presentation
and outcome of patients treated on neoadjuvant cooperative
osteosarcoma study group protocols. J Clin Oncol. 21:2011–2018.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Okada K, Wold LE, Beabout JW and Shives
TC: Osteosarcoma of the hand: A clinicopathologic study of 12
cases. Cancer. 72:719–725. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Khalifa M and Albadawy M: AI in diagnostic
imaging: Revolutionising accuracy and efficiency. Comput Methods
Programs Biomed Update. 5:1001462024. View Article : Google Scholar
|
|
21
|
Knudsen JE, Ghaffar U, Ma R and Hung AJ:
Clinical applications of artificial intelligence in robotic
surgery. J Robotic Surg. 18:1022024. View Article : Google Scholar : PubMed/NCBI
|