Introduction
Skin adnexal carcinomas (SACs) represent a diverse
range of cancerous growths originating from the appendages of the
skin. According to the World Health Organization categorization of
skin carcinomas, adnexal adenocarcinoma of ‘not otherwise
specified’ type is a primary skin adenocarcinoma characterized by
ductal or glandular differentiation, lacking distinct histological
features for more specific classification (1).
SACs are exceedingly rare malignancies (2,3), and
exhibit diverse patterns and differentiations, with over 15
distinct histologies. These carcinomas stem from three different
structures: The pilosebaceous unit, the eccrine sweat glands and
the apocrine glands. Due to their rarity and challenges in
recognition, coupled with their potential aggressive behavior,
treating SACs poses a significant challenge (4,5).
Primarily, SACs manifest in individuals with fair
skin, predominantly affecting the head and neck (65%), followed by
the extremities (17%) and trunk (17%). However, the incidence of
SAC increases significantly with advancing age, reaching its peak
during the eighth decade of life (6,7). These
tumors have also been documented in different ethnic groups,
including African-American, Asian and Pacific Islander individuals
(8,9). Typically, SACs present as slowly
growing masses, appearing either skin-colored or red. In most
cases, SACs are asymptomatic and rarely induce itching, bleeding or
pain. While most SACs exhibit only local aggressiveness, they
possess the capability for regional and distant metastasis
(10). The exact cause of SACs
remains unidentified. Certain factors, such as ultraviolet
radiation, immunosuppression, organ transplant and genetic
disorders, may play a role (10–13).
The present study describes a rare case of adnexal
carcinoma of no specific differentiation in the right eyelid
treated with a combination of chemotherapy and radiotherapy. The
case report aimed to avoid citing predatory publications based on
Kscien's list (14).
Case report
Patient information
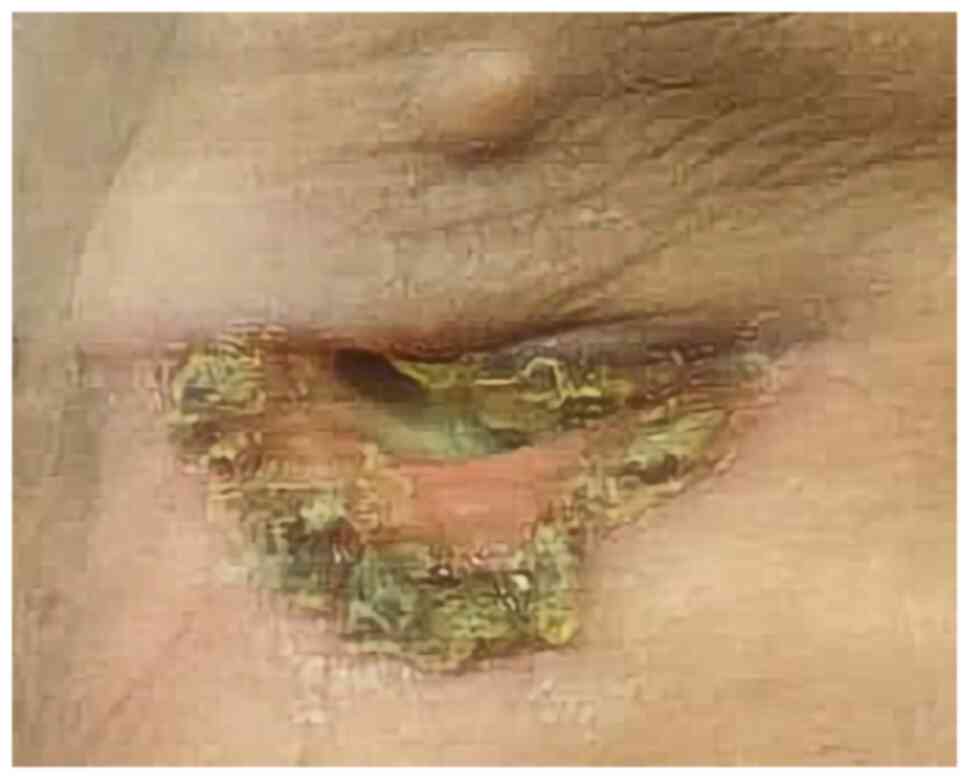
A 70-year-old male with fair skin presented to Smart
Health Tower (Sulaymaniyah, Iraq) in December 2023 with swelling
and redness around the right eye, extending to cover the eye, along
with skin desquamation (Fig. 1).
Based on the description from the patient, the lesion first
appeared as a minor redness around the eye nearly 19 years ago.
However, it is unlikely that the current lesion was the same one
due to its long existence. It is possible that the patient might
have mistaken the timeline or the lesion could be a different
benign skin growth. In recent years, the lesion recurred
intermittently and developed slight scaling over time. Despite
topical treatments, the lesion persisted and eventually grew in
size, forming a wound prone to bleeding. Notably, there was no
family history of malignancies, but the patient had a history of
excessive sunlight exposure. The patient had twice undergone an
inguinal hernia repair, first in 2002 and then again in 2010. Prior
to arriving at Smart Health Tower, the patient visited the Oncology
Teaching Hospital (Baghdad, Iraq), in May 2023 for the same
condition. A histopathological examination was carried out (please
see below) at the National Center for Educational Laboratories
(Baghdad, Iraq). Following the diagnosis, the patient decided to
seek treatment at Smart Health Tower.
Clinical findings
All vital signs were within the normal ranges. An
ulcer with swelling involving the right lower eyelid was apparent.
The patient's vision in the right eye was obstructed by swelling
that covered the eye.
Diagnostic approach
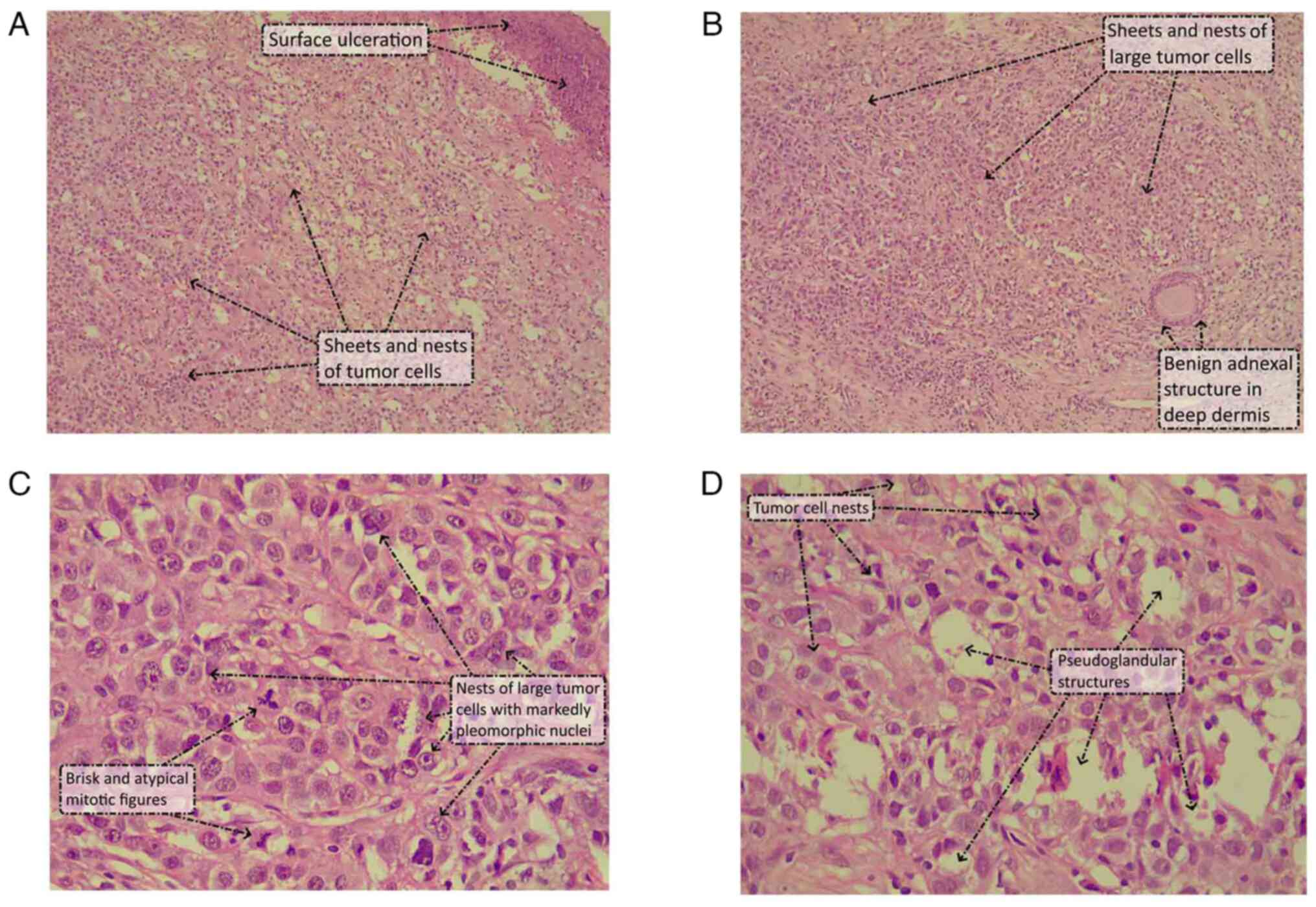
Before the patient presented at Smart Health Tower,
an incisional biopsy was performed in May 2023 at the Oncology
Teaching Hospital, followed by a histopathological examination at
the National Center for Educational Laboratories (Baghdad, Iraq).
The hematoxylin and eosin-stained sections showed a skin biopsy
with a proliferation of cells underneath an ulcerated epidermis
extending to the dermis and around the benign adnexal structures.
The tumor cells were arranged in sheets, nests and occasional
pseudo-glandular structures. The cells were large and had an
abundant lightly eosinophilic to clear cytoplasm, with markedly
pleomorphic, large nuclei that had vesicular chromatin, prominent
eosinophilic nucleoli and irregular nuclear outlines. There was
brisk mitosis with atypical (tripolar) mitotic figures. There was
no squamous, apocrine, sebaceous or any other form of distinct
histogenetic differentiation in any area of the tumor in the
incisional biopsy (Fig. 2). A panel
of immunohistochemical stains was performed on the biopsy, which
showed positive reactivity of the tumor cells to pan-keratin
(AE1/AE3), cytokeratin (CK)7, vimentin and CD15. Stains for CK20,
Melan-A, human melanoma black-45, S100, gross cystic disease fluid
protein 15 and carcinoembryonic antigen were all negative. The
combined histological and immunohistochemical picture supported the
diagnosis of a poorly differentiated SAC with no specific
histogenetic line of differentiation.
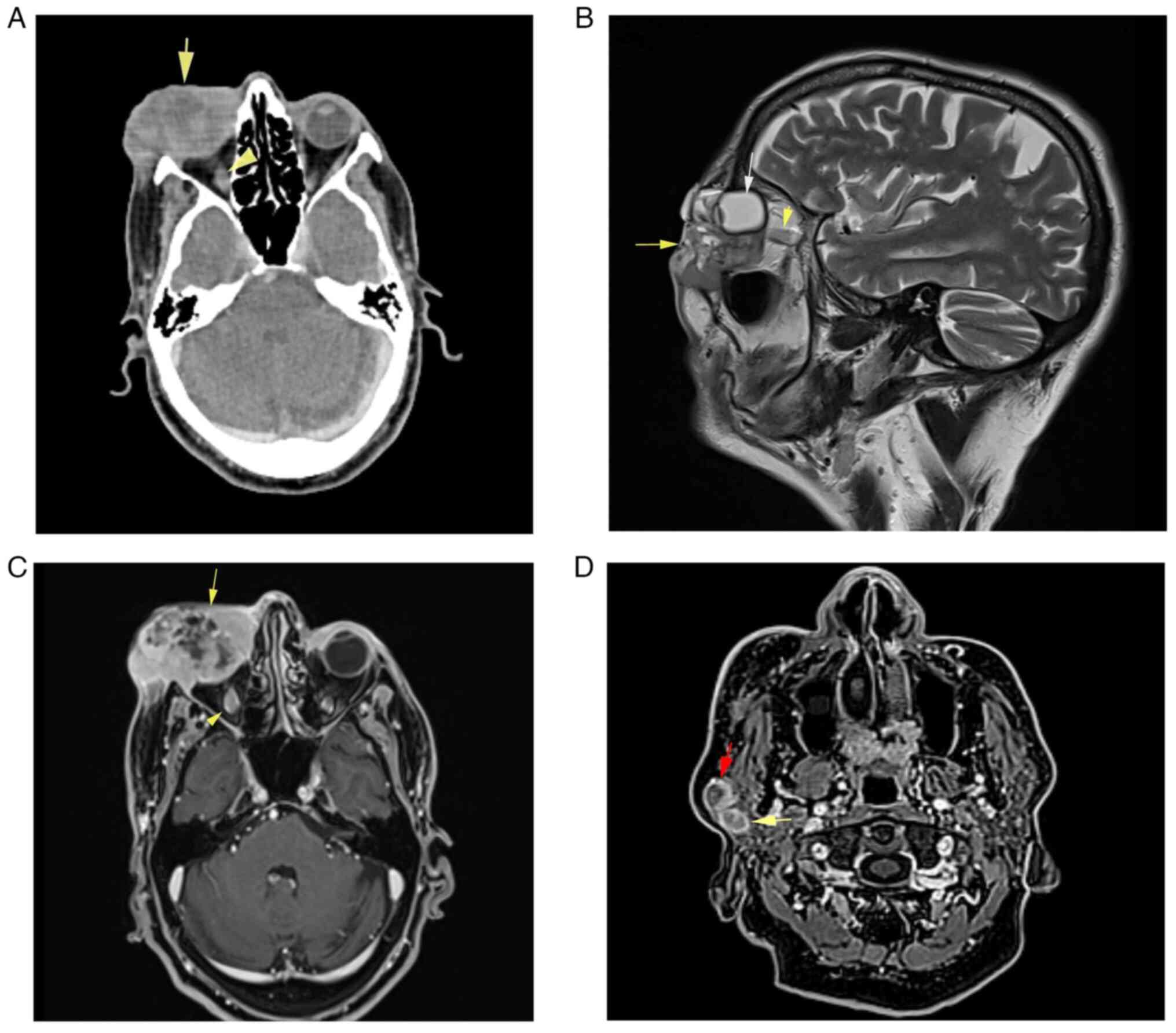
Subsequent imaging studies conducted at Smart Health
Tower included a computed tomography (CT) scan of the head and
neck, revealing an ill-defined, heterogeneously enhancing
soft-tissue mass occupying the skin, lateral canthus, right
lacrimal gland, lower eyelid and preseptal space, measuring
44×54×32 mm (Fig. 3A). This mass
extended to the medial canthus and intraconal space, infiltrating
the lateral and inferior recti muscles of the right eye. No
calcification or bone destruction was observed. Furthermore,
multiple right intraparotid lymph nodes with rounded contours and
central necrosis, the largest measuring 16×15 mm, were noted,
indicative of lymph node infiltration (Fig. 3D).
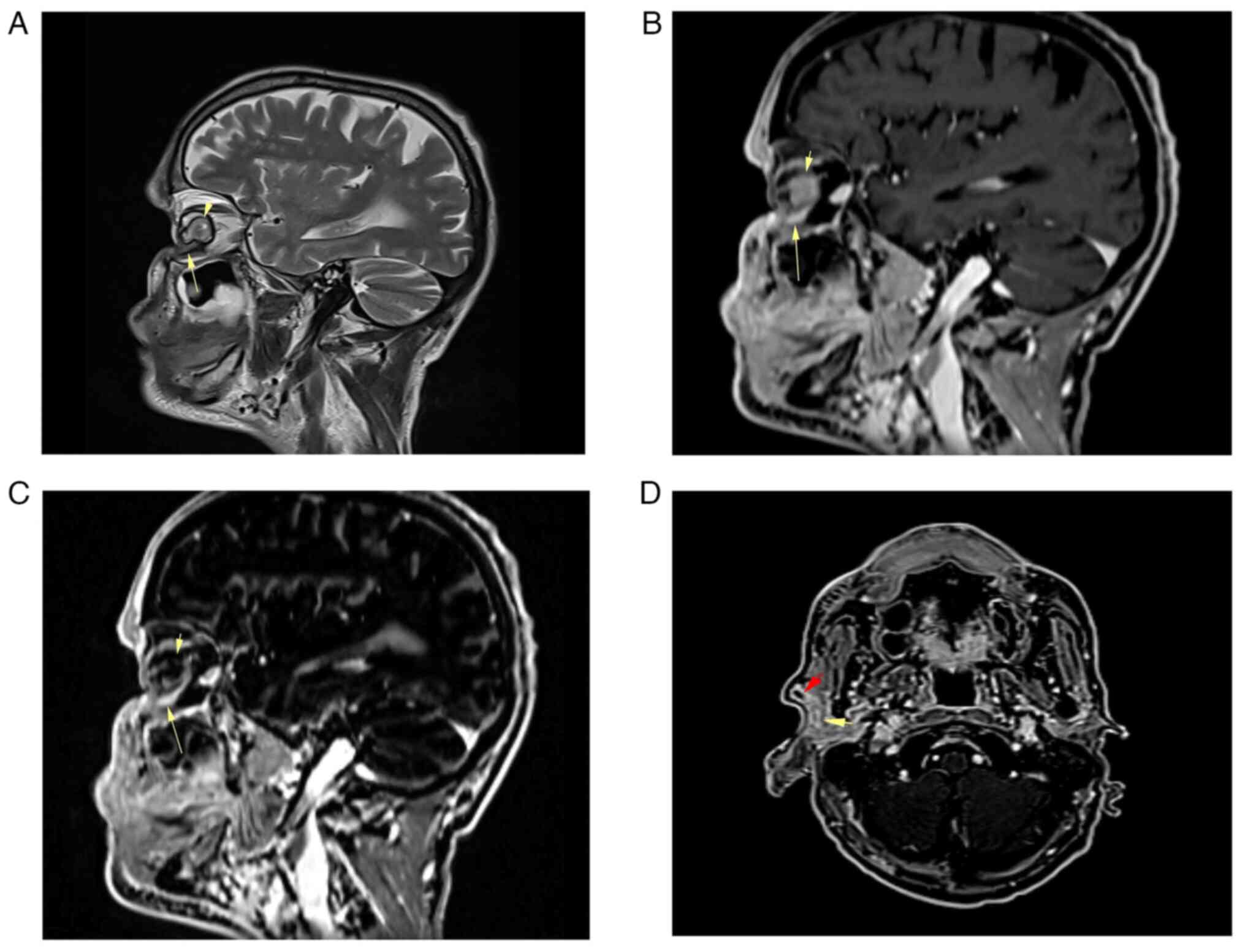
Magnetic resonance imaging (MRI) of the neck and
base of the skull with contrast revealed the presence of a large,
well-defined heterogeneous mass involving the right orbit and
periorbital tissue, measuring 62×38×43 mm (Fig. 3). The tumor partially encroached
upon the right orbit and the right lacrimal gland, with invasion
noted into the peri-orbital muscles but excluding the superior
rectus muscle. There was no evidence of bone invasion or extension
into the paranasal sinuses, and the integrity of the optic nerve
was preserved. Incidentally, mild involutional brain changes were
observed. Furthermore, two pathological lymph nodes measuring
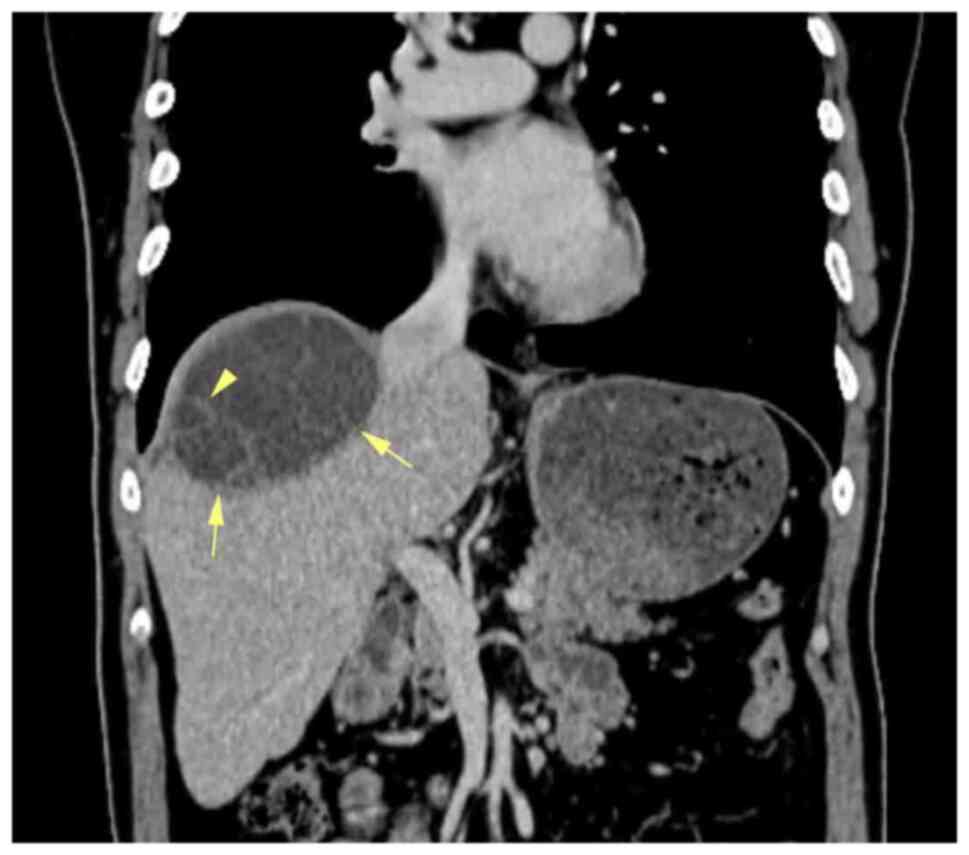
<14 mm were detected within the right parotid gland. A CT scan
of the chest and abdomen revealed multiple cystic lesions in the
liver, with the largest measuring 73×70 mm in segment VII. These
lesions appeared multilocular, containing multiple enhanced septa
suggestive of multiple hydatid cysts (Fig. 4).
Therapeutic intervention
The patient refused any form of surgical
intervention for the tumor apart from the incisional biopsy.
Chemotherapy consisting of carboplatin and paclitaxel was
administered weekly for 6 weeks, employing a regimen of carboplatin
with an area under the curve (AUC) value of 2 in conjunction with
paclitaxel dosed at 50 mg/m2, followed by curative
radiotherapy utilizing volumetric modulated arc therapy. The
radiation was focused on the primary target volume (PTV)1,
encompassing the right cervical regions 2 and 3 and the entire
parotid gland, with a cumulative dose of 5,940 cGY delivered over a
total of 33 fractions spanning 33 days; this led to a reduction in
swelling and ulceration around the affected eye (Fig. 5). Additionally, a PTV2 covering the
eye and including the gross tumor volume of the lymph nodes within
the intraparotid region, with a total dose of 6,996 cGY, was
administered over the same 33 fractions and days. After this
combined modality therapy, the patient underwent an additional
three cycles of carboplatin and paclitaxel chemotherapy
administered at intervals of 21 days. The paclitaxel was dosed at
175 mg/m2, while carboplatin was capped at a maximum of
750 mg, with a target AUC of 5.
Follow-up and outcome
Upon follow-up, 1 month after the last chemotherapy
(Fig. 6), an MRI revealed a small,
linear-shaped focal enhancing lesion measuring 8×4 mm in the
inferior segment of the right orbital cavity. This lesion showed a
significant reduction from its initial size of 62×43×38 mm,
indicating 90% post-treatment shrinkage (Fig. 7). According to the
Tumor-Node-Metastasis (TNM) classification (8th edition) (15), the tumor was initially classified as
T4 due to its size and involvement of the orbit and periorbital
tissues. Following treatment, the significant reduction in tumor
size led to a down-staging to T1.
Additionally, diffuse volume loss and irregularity
in the right eyeball were observed, suggesting radiation-induced
changes, which resulted in vision loss in the affected eye. The
enlarged lymph nodes in the right cervical region, previously
displaying suspicious imaging features, exhibited a reduction in
size of ~40% relative to their prior assessments (Fig. 7). The patient was advised on the
option of surgery for the residual tumor but declined the
treatment. No further treatment was administered to the patient,
and the patient is scheduled for follow-up every 3 months.
Discussion
Cutaneous adnexal carcinomas are rare, accounting
for only 0.005% of all skin tumors (16). SACs typically exhibit gradual growth
and appear either red or skin-colored. Detection usually occurs
after the lesion has been present for an extended period, as SACs
are commonly symptomless. Although infrequent, SACs may
occasionally cause itching, bleeding or discomfort. SACs are
predominantly found in individuals with fair skin, mainly on the
head and neck region (6,10). The patient in the present case
report was a fair-skinned male. According to the description
provided by the patient, the lesion was first observed 19 years ago
as a small red area around the right eye, which raises some
uncertainty. Over time, the lesion intermittently diminished and
regrew multiple times. Despite attempts with topical treatments,
the lesion endured and eventually grew in size, evolving into a
wound susceptible to bleeding.
The exact cause of SACs remains largely
unidentified. While SACs frequently develop spontaneously, some may
originate from precursor lesions or preexisting benign
counterparts. Malignant transformation within benign adnexal skin
tumors has been documented, particularly in immunosuppressed
patients (11). Moreover, organ
transplant recipients demonstrate a propensity for developing SACs
(10). The presence of a genetic
basis is observed in various syndromes linked to multiple adnexal
tumors and systemic malignancies, such as sebaceous carcinoma in
Muir-Torre syndrome and cylindrocarcinoma in Brooke-Spiegler
syndrome (12,13). Ultraviolet radiation is considered a
potential etiological factor for SACs, similar to its role in other
types of skin cancer. This is supported by the tendency of SACs to
predominantly affect the head and neck region, where exposure to UV
radiation is often more marked (10). The patient described in the present
study had a history of excessive sunlight exposure, but no known
family history, syndromic manifestations or organ
transplantation.
A study involving 23 cases of SAC found that the
median age at diagnosis was 66 years (range, 46–87 years), with 61%
of patients being female and 39% male (5). Another population-based study
conducted by Stam et al (10) in the Netherlands, involving 2,220
patients with SACs, revealed that 52.70% of patients were female
and 47.30% were male. Most SACs occurred in the head and neck
region. Notable occurrences were observed in areas such as the
eyelid (9%), ear (7% for males and 3% for females) and lip (2%).
Other affected regions included the trunk (19%), extremities (15%)
and genitals (14%). The patient described in the present case
report was a 70-year-old male.
Clinically diagnosing SACs is challenging even for
experienced skin cancer specialists, as they are often mistaken for
squamous cell carcinoma, basal cell carcinoma or benign skin
tumors. This challenge in identifying SACs clinically can be
attributed to their diverse and frequently subtle manifestations
(5,17,18).
The histopathological assessment of a deep skin biopsy or
diagnostic excision is widely accepted as the primary method for
diagnosing SAC. Nevertheless, due to the diverse histopathological
characteristics of SACs, achieving an accurate histological
diagnosis can frequently pose challenges (6,18). In
the present case report, a skin tissue biopsy was obtained for
histopathological examination, revealing histological features
consistent with poorly differentiated adnexal skin carcinoma, but
without any specific features to suggest squamous, apocrine,
sebaceous or other distinct histogenetic lines of
differentiation.
Due to the scarcity of SACs, consensus regarding
their management is lacking, leading to treatments typically based
on limited case series. Surgery, commonly involving wide local
excision or Mohs surgery, has been the predominant approach for
most cases (7,9,19,20).
The patient in the present case report declined to undergo a wide
local tumor excision. Reports indicate that local or regional
recurrence occurs in up to 60% of lesions treated solely with
surgical excision for cutaneous adnexal carcinomas (4). The infiltrative nature of these
lesions often complicates the process of obtaining sufficient
margins without substantial surgical defects. Surgical series have
documented a re-excision rate of up to 30% among patients who
underwent wide local excision alone due to persistently positive
margins (19,21).
Additionally, the literature presents mixed outcomes
regarding the efficacy of radiation therapy as a standalone
treatment. In one case report, radiation alone was administered for
a lower lip lesion alongside a clinically positive submental lymph
node. After a 6-month follow-up, the patient exhibited no signs of
disease (22). However,
transformation into a more aggressive histological form has also
been documented in a case where radiation was used as the sole
treatment (23). The present case
report documents the administration of chemotherapy and
radiotherapy followed by additional cycles of chemotherapy without
surgery. Notably, the tumor showed a marked reduction in size of
>90%, while the two suspicious right cervical lymph nodes
exhibited a reduction in size of ~40%. According to the TNM
classification (8th edition), the tumor was initially classified as
T4 due to its size and involvement of the orbit and periorbital
tissues. After treatment, the marked reduction in tumor size
indicated a down-staging to T1 (15). This substantial shift from T4 to T1
underscores the effectiveness of combined chemotherapy and
radiotherapy in reducing the tumor burden, thereby making curative
surgery a viable option. However, the patient opted against this
surgery.
The limitation of the present report is the
inability to assign a specific histotype to the SAC. This is due to
the patient declining a larger tissue biopsy and surgical removal
of the mass to allow a more complete assessment of the entire
lesion. The available immunohistochemical staining results
supported the overall diagnosis, but more niche and experimental
stains were not available to favor one line of differentiation over
another. Furthermore, molecular testing and genomic profiling
studies are not readily available in Iraq to perform on the biopsy
material.
In conclusion, SAC is a rare finding and its
occurrence in the eyelid is even rarer. A combination of
chemotherapy and radiotherapy followed by additional cycles of
chemotherapy can be an effective therapeutic modality in minimizing
the size of the tumor.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
RHA and RMA were major contributors to the
conception of the study, as well as to the literature search for
related studies. RHA and ShMA were involved in the treatment of the
patient. FHK and HAN were involved in the literature review, study
design and writing the manuscript. ShMA, SaMA, RSA, SSO and BAA
were involved in the literature review, the design of the study,
the critical revision of the manuscript and the processing of the
figures. FHK and BAA confirm the authenticity of all the raw data.
AMA was the pathologist who performed the histopathological
diagnosis. All authors have read and approved the final version of
the manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Massi D, Scolyer RA and Willemze R:
Adnexal adenocarcinoma not otherwise specified. WHO classification
of skin tumours. 4th edition. International Agency for Res Cancer.
155–156. 2018.
|
|
2
|
Mohemed FM, Fatih BN, Qadir AA, Abdalla SH
and Mahmood ZH: Cancer publications in one year (2022): A
cross-sectional study. BMJ. 20:18–26. 2023.
|
|
3
|
Mingomataj E, Krasniqi M, Dedushi K,
Sergeevich KA, Kust D, Qadir AA, Abdullah AS, Ahmed MK and Fatah
GM: Cancer publications in one year (2023): A cross-sectional
study. BMJ. 2:3–11. 2024.
|
|
4
|
Wang LS, Handorf EA, Wu H, Liu JC, Perlis
CS and Galloway TJ: Surgery and adjuvant radiation for high-risk
skin adnexal carcinoma of the head and neck. Am J Clin. 40:429–432.
2017.
|
|
5
|
Stam H, van de Wiel BA, Klop WM,
Zupan-Kajcovski B, Janssens S, Karakullukcu MB, van der Noort V and
Lohuis PJFM: Skin adnexal carcinoma of the head and neck: A
retrospective study in a tertiary referral center. Eur Arch
Otorhinolaryngol. 272:1001–1010. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Martinez SR, Barr KL and Canter RJ: Rare
tumors through the looking glass: An examination of malignant
cutaneous adnexal tumors. Arch Dermatol. 147:1058–1062. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Blake PW, Bradford PT, Devesa SS and Toro
JR: Cutaneous appendageal carcinoma incidence and survival patterns
in the United States: A population-based study. Arch Dermatol.
146:625–632. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Goldstein DJ, Barr RJ and Cruz DJ:
Microcystic adnexal carcinoma: A distinct clinicopathologic entity.
Cancer. 50:566–672. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Avraham JB, Villines D, Maker VK, August C
and Maker AV: Survival after resection of cutaneous adnexal
carcinomas with eccrine differentiation: Risk factors and trends in
outcomes. J Surg Oncol. 108:57–62. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stam H, Lohuis PJ, Zupan-Kajcovski B,
Wouters MW, van der Hage JA and Visser O: Increasing incidence and
survival of a rare skin cancer in the Netherlands. A
population-based study of 2,220 cases of skin adnexal carcinoma. J
Surg Oncol. 107:822–827. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Harwood CA, McGregor JM, Swale VJ, Proby
CM, Leigh IM, Newton R, Khorshid SM and Cerio R: High frequency and
diversity of cutaneous appendageal tumors in organ transplant
recipients. J Am Acad Dermatol. 48:401–408. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lee DA, Grossman ME, Schneiderman P and
Celebi JT: Genetics of skin appendage neoplasms and related
syndromes. J Med Genet. 42:811–819. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kazakov DV, Michal M, Kacerovska D and
McKee PH: Cutaneous Adnexal Tumors. Wolters Kluwer
Health/Lippincott Williams & Wilkins. (Philadelphia, PA, p830).
2012.
|
|
14
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory Publishing Lists: A review on the ongoing battle
against fraudulent actions. BMJ. 2:26–30. 2024.
|
|
15
|
Amin MB, Greene FL, Edge SB, Compton CC,
Gershenwald JE, Brookland RK, Meyer L, Gress DM, Byrd DR and
Winchester DP: The eighth edition AJCC cancer staging manual,
continuing to build a bridge from a population-based to a more
‘personalized’ approach to cancer staging. CA Cancer J Clin.
67:93–99. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cotton D: Troublesome tumours. 1: Adnexal
tumours of the skin. J Clin Pathol. 44:543–548. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Batsakis JG, el-Naggar AK and Weber RS:
Two perplexing skin tumors: Microcystic adnexal carcinoma and
keratoacanthoma. Ann Otol Rhinol Laryngol. 103:829–832. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Allee JE, Cotsarelis G, Solky B and Cook
JL: Multiply recurrent trichilemmal carcinoma with perineural
invasion and cytokeratin 17 positivity. Dermatol Surg. 29:886–889.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chiller K, Passaro D, Scheuller M, Singer
M, McCalmont T and Grekin RC: Microcystic adnexal carcinoma:
Forty-eight cases, their treatment, and their outcome. Arch
Dermatol. 136:1355–1359. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wetter R and Goldstein GD: Microcystic
adnexal carcinoma: A diagnostic and therapeutic challenge. Dermatol
Ther. 21:452–458. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pugh TJ, Lee NY, Pacheco T and Raben D:
Microcystic adnexal carcinoma of the face treated with radiation
therapy: A case report and review of the literature. Head Neck.
34:1045–1050. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gulmen S and Pullon PA: Sweat gland
carcinoma of the lips. Oral Surg Oral Med Oral Pathol. 41:643–649.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Stein JM, Ormsby A, Esclamado R and Bailin
P: The effect of radiation therapy on microcystic adnexal
carcinoma: A case report. Head Neck. 25:251–254. 2003. View Article : Google Scholar : PubMed/NCBI
|