Introduction
Papillary thyroid carcinoma (PTC) is the most
prevalent type of thyroid cancer, accounting for 80–85% of all
thyroid malignancies globally. Recent data indicate that the
incidence of thyroid cancer, particularly PTC, has been increasing
worldwide, with a significant rise observed, where the age-adjusted
incidence rate increased from 4.9 per 100,000 in 1975 to 14.5 per
100,000 in 2013. This rise is attributed largely to the increased
detection of small, indolent tumors through advanced imaging
techniques (1,2). PTC is characterized by a typically
indolent clinical behavior, a good prognosis and high long-term
survival rates, especially when diagnosed early (2,3). The
most common clinical presentation is a solitary thyroid nodule.
However, in rare cases, PTC can present with unusual symptoms, such
as a painful neck mass (4,5). The spectrum of PTC presentations is
not limited solely to these conventional patterns. In rare
instances, PTC may deviate from the expected clinical course,
posing diagnostic challenges to clinicians. One such atypical
presentation reported in only a handful of cases is the development
of a metastatic cystic lesion within the neck, representing an
uncommon manifestation of PTC (6,7).
The primary objective of the present study is to
present a unique case of a young female patient with a longstanding
swelling on the left side of the neck, initially diagnosed as a
cystic lesion, which was later revealed to be metastatic PTC. This
report adheres to ethical publishing standards by avoiding the
referencing of predatory journals (8).
Case report
Patient information
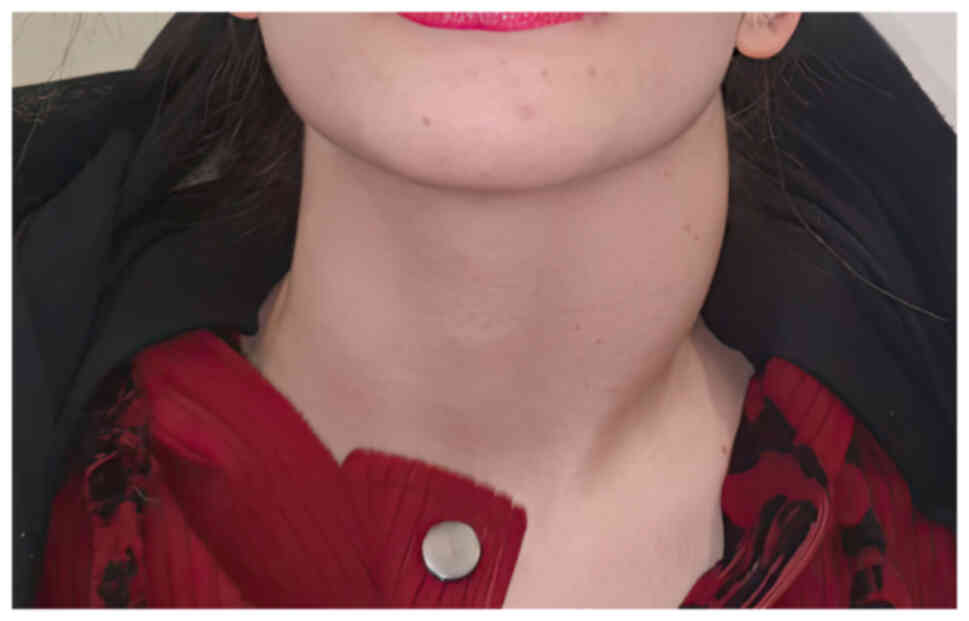
A 21-year-old woman presented to Smart Health Tower
(Sulaymaniyah, Iraq) in April 2022 with a 3-year history of a
left-sided neck swelling (Fig. 1).
The patient had no prior medical history or family history of the
same condition and had not undergone any previous surgeries. The
patient had no smoking history.
Clinical examination
During the clinical examination, a firm, non-tender
mass was palpable on the left side of the neck, with no signs of
inflammation. The thyroid examination was normal, and there were no
other palpable lymph nodes in the neck.
Diagnostic assessment
Thyroid function tests were within the normal range
[thyroid-stimulating hormone, 1.83 µIU/ml (normal range, 0.4–4.0
µIU/ml); free T4, 16.48 pmol/l (normal range, 12–22 pmol/l]. A
previous computed tomography (CT) scan in May 2019 showed a
well-defined cystic lesion extending from level C2 to C5, measuring
4.5×3.4×2.5 cm, which was suggestive of a left posterior triangle
hemangioma or possibly a branchial cleft cyst, with lymphangioma
being less likely. A fine-needle aspiration cytology (FNAC)
examination performed in 2019 yielded negative results for
malignancy, which may have been due to the limitations of FNAC in
detecting malignancy in cystic lesions or the absence of malignant
cells in the aspirated sample. The patient visited the Smart Health
Tower Head and Neck Clinic in April 2022, and a neck ultrasound
revealed a suspicious cystic lesion on the left side. Additionally,
a small, moderately suspicious (Thyroid Imaging Reporting And Data
System 4) (9) nodule measuring 9×5
mm was found on the left thyroid lobe. A CT scan of the neck showed
a thin-walled cystic lesion lateral to the carotid vessels,
compressing the jugular vein and the medial sternomastoid muscle,
measuring ~6.6×3.5 cm, suggestive of a benign cyst with an
enhancing mural cyst. FNAC was repeated for both the neck lesion
and the thyroid nodule, and the results indicated PTC of the
thyroid lobe with metastasis to the left-sided cystic lesion.
Therapeutic approach
After extensive discussion within a
multidisciplinary team, a total thyroidectomy was recommended with
a left lateral neck dissection. Under general anesthesia, through a
J-shaped incision, a total thyroidectomy with a left lateral neck
dissection was performed that included all nodal groups, 2, 3, 4, 5
and 6, along with a left central neck dissection. All important
structures such as the accessary nerve, recurrent laryngeal nerves
and parathyroid glands were identified and preserved during the
surgery. Although imaging studies showed compression of the jugular
vein, the decision was made not to open the carotid sheath as the
compression was external, and there was no evidence of involvement
or infiltration of these structures by the tumor. Postoperative
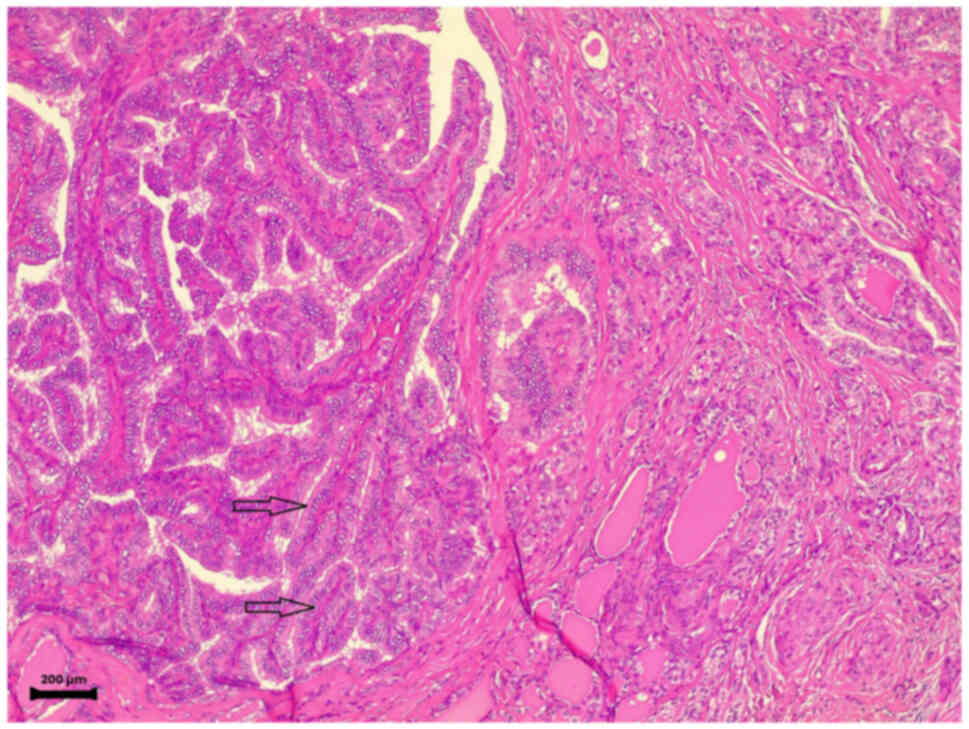
histopathological examination confirmed the presence of PTC of the
thyroid lobe (Fig. 2) and
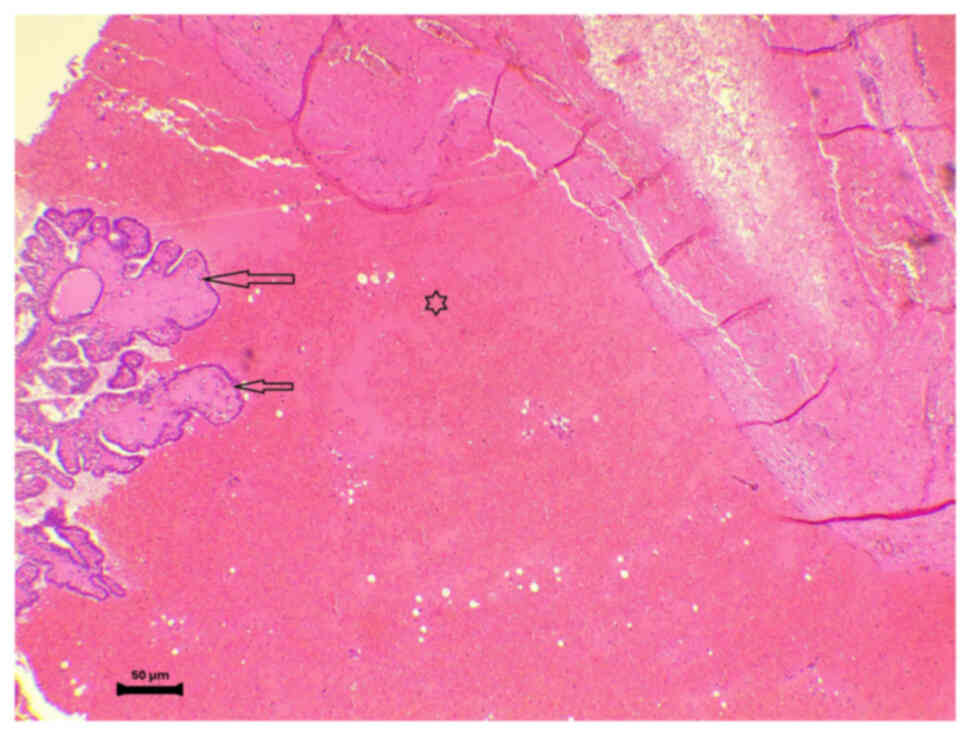
metastatic PTC of the cystic lymph node (Fig. 3). The tissue samples were fixed in
10% neutral-buffered formalin at room temperature for 24 h.
Sections were cut at a thickness of 4 µm and stained with
hematoxylin and eosin at room temperature. The staining process
involved immersing the sections in hematoxylin for 5 min, followed
by eosin for 2 min. The slides were then examined using a light
microscope. Fig. 2 was captured at
a magnification of ×10, showing complex papillary projections
covered by follicular epithelial cells with nuclear features of
papillary thyroid carcinoma. Fig. 3
was captured at a magnification of ×40, revealing a cystic space
containing papillary structures lined by follicular epithelial
cells, with nuclear features of papillary thyroid carcinoma. The
patient recovered well immediately after the operation.
Follow-up
The patient was discharged home 12 h after surgery
without signs of infection or hematoma. The discharge decision was
based on the patient's stable condition, proximity to the hospital
and preference for an early discharge. The patient received
detailed postoperative care instructions and scheduled follow-up
visits to monitor for any complications. The patient was also sent
to receive radioactive iodine treatment ~6 weeks after surgery. The
treatment involved administering a therapeutic dose of radioactive
iodine to target any residual thyroid cancer cells and metastases.
This treatment is commonly used for its ability to destroy
remaining cancerous tissue and to help prevent recurrence. At the
6-month follow-up, there were no signs of recurrence. Regular
follow-up will continue to monitor for any potential recurrence or
progression of the disease, so the patient was scheduled for
further follow-up every 6 months especially for the first few
years.
Discussion
The rarity of metastatic PTC presenting as a cystic
lesion emphasizes the importance of a comprehensive diagnostic
approach. In the present case, the initial misinterpretation of the
cystic lesion as a likely hemangioma or branchial cleft cyst
underscores the challenges in diagnosing unusual presentations of
thyroid malignancies. The incorporation of FNAC and subsequent
imaging studies led to the correct identification of metastatic
disease. Initially, FNAC performed in 2019 did not detect
malignancy. However, with the recurrence of symptoms and new
imaging studies in 2022, a repeat FNAC was conducted, which, along
with updated imaging findings, confirmed the presence of metastatic
PTC. This highlights the importance of repeated diagnostic
evaluations and imaging in cases where initial results may not
fully capture the nature of the disease.
Thyroid carcinoma is a relatively rare malignancy in
the United States, constituting <1% of all cancer cases. Within
this category, PTC is the most prevalent subtype (10,11).
PTC primarily affects individuals under the age of 40 years, with a
notable predilection for females (2.3:1 ratio) (12). PTC typically manifests between the
ages of 20 and 50 years, and is characterized by indolent clinical
behavior (13). Cystic neck masses
are a common clinical entity, often attributed to benign
conditions, such as dermoid cysts, branchial cleft cysts,
epidermoid cysts, teratomas and cystic hygromas. In the context of
a para-median cystic lesion, additional differential diagnoses
should include conditions such as second branchial cleft cysts and
lymphangiomas, which can present as lateral neck masses. In recent
years, the rise in oropharyngeal carcinoma incidence has raised the
possibility that cystic neck masses may also represent metastases
from tumors in the oropharyngeal or tonsillar region (1,11,13).
Notably, PTC rarely presents as a cystic neck mass without any
palpable lesions in the thyroid gland, making its diagnosis
particularly challenging (14).
Sonographically, PTC typically appears as a
hypoechoic solid lesion with a smooth or irregular contour,
intrinsic vascularity and a lack of a hypoechoic halo. However, it
is important to note that only a small fraction of PTC cases (5%)
present as purely cystic lesions, with the majority exhibiting
features of intrinsic hypervascularity (69%) and perinodal
hypervascularity (20%) (15,16).
The sonographic features of cystic PTC or metastatic cystic nodes
include the presence of multiple or solitary cysts with internal
septations, calcifications and internal nodules (13). In the current case, a large cystic
lesion (8.5×5.5×2.6 cm) was observed on the left side of the neck,
accompanied by an echogenic focus, internal vascularity and two
papillary components, A CT scan of the neck showed a thin-walled
cystic lesion lateral to the carotid vessels, measuring ~6.6×3.5
cm.
FNAC is a common diagnostic tool; however, it
carries a false-negative rate of 45% in diagnosing cystic PTC.
Sampling error is the primary culprit for this high level of
false-negatives, rather than cytological misdiagnosis. The accuracy
of FNAC can be enhanced by obtaining material from the wall and
solid components of the cyst under ultrasound guidance (17). In the present case, FNAC was
performed on both the thyroid lobe and the neck mass, both yielding
evidence of PTC. It is important to note that the initial FNAC
conducted in 2019 did not identify malignancy, and the diagnosis of
PTC was only confirmed upon repeat FNAC during the subsequent
evaluation in 2022. The role of thyroglobulin analysis in aspirated
fluid should not be underestimated. Studies have shown that
elevated thyroglobulin levels in aspirated fluid can be indicative
of cystic PTC. Furthermore, intranodal concentrations of
thyroglobulin may correlate with high attenuation on CT and
inhomogeneous intracystic signal changes on magnetic resonance
imaging (18,19). For patients with a negative FNAC,
excisional biopsy is a crucial consideration to detect PTC.
Suspicious clinical or radiological features of malignancy warrant
frozen section analysis, which can guide decisions on total
thyroidectomy with modified radical neck dissection (13).
Following confirmation of cystic PTC, the definitive
treatment involves the removal of the cyst along with all thyroid
tissue and accessible lymph nodes to improve the prognosis.
Postoperative radioiodine ablation of the thyroid remnant, coupled
with suppressive thyroxine dosing, helps reduce the risk of
recurrences (13,20). The long-term prognosis for patients
with metastatic cystic lymph nodes from PTC is generally favorable,
especially when the disease is localized and amenable to surgical
resection and radioactive iodine therapy. However, careful and
vigilant follow-up is crucial to detect and manage recurrences
promptly. PTC generally exhibits a favorable prognosis, boasting a
survival rate of >90% at the 20-year mark. Nonetheless, when
extra-thyroidal extension occurs, survival rates notably decline to
54% at 15 years and further to 29% at 30 years (13).
The present case report underscores the clinical
significance of recognizing metastatic PTC presenting as a cystic
neck lesion, highlighting the importance of a comprehensive
diagnostic approach. The rarity of this manifestation adds a
distinctive dimension to the understanding of thyroid malignancies.
The successful treatment outcome, involving a total thyroidectomy
with a left lateral neck dissection followed by radioactive iodine
treatment, reinforces the efficacy of the chosen therapeutic
strategy. This case underscores the importance of considering
metastatic disease in the differential diagnosis of cystic neck
lesions in patients with a history of PTC.
One limitation of the present study was the decision
not to pursue scintigraphic analysis for the suspected cystic
lesion, which was based on established clinical protocols in the
Smart Health Tower. Another limitation in this case is that
specific images cannot be provided from the scans and ultrasound
due to data storage and access limitations within the institutional
database. However, the findings and diagnostic outcomes have been
detailed comprehensively. In conclusion, the rarity of metastatic
PTC presenting as a cystic lesion emphasizes the importance of a
comprehensive diagnostic approach.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AMS was a major contributor to the conception of the
study, as well as to the literature search for related studies. ZAM
and FHK were involved in the literature review, study design and
writing the manuscript. HMD, ASM, YAS, SHH, MNH and IJH were
involved in the literature review, the design of the study, the
critical revision of the manuscript and the processing of the
figures. FHK and SHH confirm the authenticity of all the raw data.
AJQ was the radiologist who assessed the case imaging. AMA was the
pathologist who performed the histopathological diagnosis. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Abdullah AM, Qaradakhy AJ, Saeed YA, Salih
AM, Karim S, Ali OA, Hassan SH, Nasraldeen SA, Mohammed SH and
Kakamad FH: Papillary thyroid carcinoma associated with
non-functioning parathyroid carcinoma with Warthin's tumor of the
parotid gland: A case report and brief literature review. Med Int
(Lond). 3:262023.PubMed/NCBI
|
|
2
|
Lim H, Devesa SS, Sosa JA, Check D and
Kitahara CM: Trends in thyroid cancer incidence and mortality in
the United States, 1974–2013. JAMA. 317:1338–1348. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ito Y, Miyauchi A, Kihara M, Fukushima M,
Higashiyama T and Miya A: Overall survival of papillary thyroid
carcinoma patients: A single-institution long-term follow-up of
5897 patients. World J Surg. 42:615–622. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chiang KY, Zhuang YL, Li WY and Lin CZ:
Occult papillary thyroid carcinoma presenting as huge cervical
metastasis with cystic pattern. Tzu Chi Med J. 20:140–143. 2008.
View Article : Google Scholar
|
|
5
|
Mahattanapreut A, Aroonroch R, Chintrakarn
C and Sriphrapradang C: Deep neck infection: Atypical presentation
of papillary thyroid cancer. Case Rep Otolaryngol.
2021:14792012021.PubMed/NCBI
|
|
6
|
Yang J, Ma Y, Gong Y, Gong R, Li Z and Zhu
J: Multiple simultaneous rare distant metastases as the initial
presentation of papillary thyroid carcinoma: A case report. Front
Endocrinol (Lausanne). 10:7592019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gholami S, Bakhshi M, Atarbashi-Moghadam
S, Mir Mohammad Sadeghi H and Rahimzamani A: Mandibular metastasis
of silent papillary thyroid carcinoma: A rare case report with
review of the literature. Case Rep Dent.
2020:86834652020.PubMed/NCBI
|
|
8
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, OmarD A, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
9
|
Tessler FN, Middleton WD, Grant EG, Hoang
JK, Berland LL, Teefey SA, Cronan JJ, Beland MD, Desser TS, Frates
MC, et al: ACR thyroid imaging, reporting and data system
(TI-RADS): White paper of the ACR TI-RADS committee. J Am Coll
Radiol. 14:587–595. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mingomataj E, Krasniqi M, Dedushi K,
Sergeevich KA, Kust D, Qadir AA, Abdullah AS, Ahmed MK and Fatah
GM: Cancer publications in one year (2023): A cross-sectional
study. Barw Med J. 2:3–11. 2024.
|
|
11
|
Seven H, Gurkan A, Cinar U, Vural C and
Turgut S: Incidence of occult thyroid carcinoma metastases in
lateral cervical cysts. Am J Otolaryngol. 25:11–17. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dobrinja C, Troian M, Cipolat Mis T, Rebez
G, Bernardi S, Fabris B, Piscopello L, Makovac P, Di Gregorio F and
de Manzini N: Rationality in prophylactic central neck dissection
in clinically node-negative (cN0) papillary thyroid carcinoma: Is
there anything more to say? A decade experience in a single-center.
Int J Surg. 41 (Suppl 1):S40–S47. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Patil VS, Vijayakumar A and Natikar N:
Unusual presentation of cystic papillary thyroid carcinoma. Case
Rep Endocrinol. 2012:7327152012.PubMed/NCBI
|
|
14
|
Subha ST, Bakri MA, Salleh H, Doi M and
Nordin AJ: Papillary thyroid carcinoma presenting as a cystic neck
lesion: Case series. Iran J Otorhinolaryngol. 30:49–54.
2018.PubMed/NCBI
|
|
15
|
Jun P, Chow LC and Jeffrey RB: The
sonographic features of papillary thyroid carcinomas: Pictorial
essay. Ultrasound Q. 21:39–45. 2005.PubMed/NCBI
|
|
16
|
Chan BK, Desser TS, McDougall IR, Weigel
RJ and Jeffrey RB Jr: Common and uncommon sonographic features of
papillary thyroid carcinoma. J Ultrasound Med. 22:1083–1090. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
American Thyroid Association (ATA)
Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid
Cancer, . Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL,
Mandel SJ, Mazzaferri EL, McIver B, Pacini F, et al: Revised
American thyroid association management guidelines for patients
with thyroid nodules and differentiated thyroid cancer. Thyroid.
19:1167–1214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Som PM, Brandwein M, Lidov M, Lawson W and
Biller HF: The varied presentations of papillary thyroid carcinoma
cervical nodal disease: CT and MR findings. AJNR Am J Neuroradiol.
15:1123–1128. 1994.PubMed/NCBI
|
|
19
|
King AD, Ahuja AT, To EW, Tse GM and
Metreweli C: Staging papillary carcinoma of the thyroid: Magnetic
resonance imaging vs ultrasound of the neck. Clin Radiol.
55:222–226. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Andersen PE, Kinsella J, Loree TR, Shaha
AR and Shah JP: Differentiated carcinoma of the thyroid with
extrathyroidal extension. Am J Surg. 170:467–470. 1995. View Article : Google Scholar : PubMed/NCBI
|