|
1
|
Pushpanjali M, Sujata DN, Subramanyam SB and Jyothsna M: Adenoid cystic carcinoma: An unusual presentation. J Oral Maxillofac Pathol. 18:286–290. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gandhi AK, Roy S, Biswas A, Bhasker S, Sharma A, Thakar A and Mohanti BK: Adenoid cystic carcinoma of head and neck: A single institutional analysis of 66 patients treated with multi-modality approach. Indian J Med Paediatr Oncol. 36:166–171. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Romani C, Lorini L, Bozzola A, Bignotti E, Tomasoni M, Ardighieri L, Bugatti M, Battocchio S, Ravaggi A, Tomasini D, et al: Functional profiles of curatively treated adenoid cystic carcinoma unveil prognostic features and potentially targetable pathways. Sci Rep. 13:18092023. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang M, Liu Y, Yang H, Jin F and Zheng A: Breast adenoid cystic carcinoma: A report of seven cases and literature review. BMC Surg. 22:1132022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen Z, Jiang J, Fan Y and Lu H: Pulmonary adenoid cystic carcinoma: Molecular characteristics and literature review. Diagn Pathol. 18:652023. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Alhashemi M, Oubari S, Mohamad AH, Alhashemi M, Kabel O, Alhelue A and Fattal F: Adenoid cystic carcinoma (ACC) of the Bartholin's gland misdiagnosed three times: A case report. BMC Womens Health. 23:1562023. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Godge P, Sharma S and Yadav M: Adenoid cystic carcinoma of the parotid gland. Contemp Clin Dent. 3:223–226. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
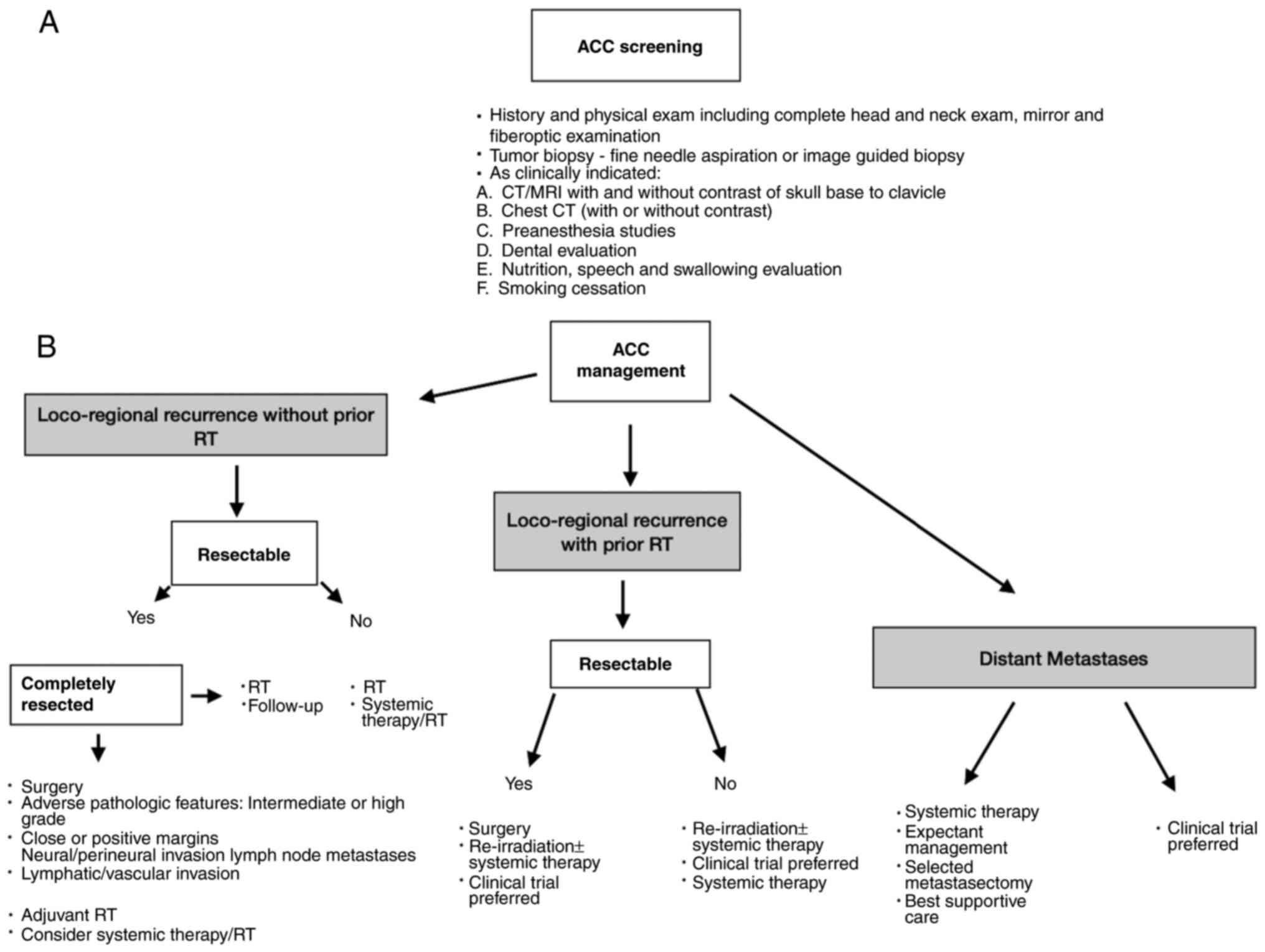
National Comprehensive Cancer Network (NCCN), . Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Head and Neck Cancer, Version 1.2025. NCCN, Plymouth Meeting, PA. 2024.https://www.nccn.org/professionals/physician_gls/default.aspx
|
|
9
|
Choi S, Sano D, Cheung M, Zhao M, Jasser SA, Ryan AJ, Mao L, Chen WT, El-Naggar AK and Myers JN: Vandetanib inhibits growth of adenoid cystic carcinoma in an orthotopic nude mouse model. Clin Cancer Res. 14:5081–5089. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Queimado L, Lopes C, Du F, Martins C, Fonseca I, Bowcock AM, Soares J and Lovett M: In vitro transformation of cell lines from human salivary gland tumors. Int J Cancer. 81:793–798. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Phuchareon J, Ohta Y, Woo JM, Eisele DW and Tetsu O: Genetic profiling reveals cross-contamination and misidentification of 6 adenoid cystic carcinoma cell lines: ACC2, ACC3, ACCM, ACCNS, ACCS and CAC2. PLoS One. 4:e60402009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Miller LE, Au V, Mokhtari TE, Goss D, Faden DL and Varvares MA: A contemporary review of molecular therapeutic targets for adenoid cystic carcinoma. Cancers (Basel). 14:9922022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Michaelides I, Künzel J, Ettl T, Beckhove P, Bohr C, Brochhausen C and Mamilos A: Adenoid cystic carcinoma of the salivary glands: A pilot study of potential therapeutic targets and characterization of the immunological tumor environment and angiogenesis. Eur Arch Otorhinolaryngol. 280:2937–2944. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Linxweiler M, Wemmert S, Braun FL, Körner S, Brust LA, Knebel M, Klamminger GG, Wagner M, Morris LGT and Kühn JP: Targeted therapy in salivary gland cancer: Prevalence of a selected panel of actionable molecular alterations in a German tertiary referral center patient cohort. Mol Diagn Ther. 1:10.1007/s40291–024-00750-w. 2024.
|
|
15
|
Chae YK, Chung SY, Davis AA, Carneiro BA, Chandra S, Kaplan J, Kalyan A and Giles FJ: Adenoid cystic carcinoma: Current therapy and potential therapeutic advances based on genomic profiling. Oncotarget. 6:37117–37134. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Belulescu IC, Margaritescu C, Dumitrescu CI, DĂguci L, Munteanu C and Margaritescu OC: Adenoid cystic carcinoma of salivary gland: A ten-year single institute experience. Curr Health Sci J. 46:56–65. 2020.PubMed/NCBI
|
|
17
|
Fang Y, Peng Z, Wang Y, Gao K, Liu Y, Fan R, Zhang H, Xie Z and Jiang W: Current opinions on diagnosis and treatment of adenoid cystic carcinoma. Oral Oncol. 130:1059452022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hong J, Choi E, Kim D, Seo MK, Kang H, Park B and Kim S: Immunological subtyping of salivary gland cancer identifies histological origin-specific tumor immune microenvironment. NPJ Precis Oncol. 8:152024. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Atallah S, Casiraghi O, Fakhry N, Wassef M, Uro-Coste E, Espitalier F, Sudaka A, Kaminsky MC, Dakpe S, Digue L, et al: A prospective multicentre REFCOR study of 470 cases of head and neck Adenoid cystic carcinoma: Epidemiology and prognostic factors. Eur J Cancer. 130:241–249. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jaber MA, Hassan M, Ingafou M and Elameen AM: Adenoid cystic carcinoma of the minor salivary glands: A systematic review and meta-analysis of clinical characteristics and management strategies. J Clin Med. 13:2672024. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saleh E and Ukwas A: Adenoid cystic carcinoma of salivary glands: A ten-year review and an assessment of the current management, surgery, radiotherapy, and chemotherapy. Int J Otolaryngol. 29:74014582023.PubMed/NCBI
|
|
22
|
Loap P, Vischioni B, Bonora M, Ingargiola R, Ronchi S, Vitolo V, Barcellini A, Goanta L, De Marzi L, Dendale R, et al: Biological rationale and clinical evidence of carbon ion radiation therapy for adenoid cystic carcinoma: A narrative review. Front Oncol. 11:7890792021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Powell SK, Kulakova K and Kennedy S: A review of the molecular landscape of adenoid cystic carcinoma of the lacrimal gland. Int J Mol Sci. 24:137552023. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu J, Shao C, Tan ML, Mu D, Ferris RL and Ha PK: Molecular biology of adenoid cystic carcinoma. Head Neck. 34:1665–1677. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zupancic M, Näsman A, Friesland S and Dalianis T: Adenoid cystic carcinoma, clinical presentation, current treatment and approaches towards novel therapies. Anticancer Res. 44:1325–1334. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Persson M, Andrén Y, Mark J, Horlings HM, Persson F and Stenman G: Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck. Proc Natl Acad Sci USA. 106:18740–18744. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
de Morais EF, de Farias Morais HG, de Almeida Freitas R and Coletta RD: Prognostic significance of histopathological parameters for salivary gland adenoid cystic carcinoma. Dent J (Basel). 11:2622023. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hoekzema CR, Massey BL, Blumin JH, Hunt BC and Bock JM: Dysphagia due to adenoid cystic carcinoma of the base of the tongue. Ann Otol Rhinol Laryngol. 121:402–406. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Marchiano E, Chin OY, Fang CH, Park RC, Baredes S and Eloy JA: Laryngeal adenoid cystic carcinoma: A systematic review. Otolaryngol Head Neck Surg. 154:433–439. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Dantas AN, Morais EF, Macedo RA, Tinôco JM and Morais ML: Clinicopathological characteristics and perineural invasion in adenoid cystic carcinoma: A systematic review. Braz J Otorhinolaryngol. 81:329–335. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ma C, Gao T, Ju J, Zhang Y, Ni Q, Li Y, Zhao Z, Chai J, Yang X and Sun M: Sympathetic innervation contributes to perineural invasion of salivary adenoid cystic carcinoma via the β2-adrenergic receptor. Onco Targets Ther. 21:1475–1495. 2019. View Article : Google Scholar
|
|
32
|
Atram MA, Shivkumar VB and Gangane NM: Intracranial remote metastasis from adenoid cystic cancer of parotid gland: Case report and review of literature. Indian J Otolaryngol Head Neck Surg. 74 (Suppl 3):S5949–S5953. 2022. View Article : Google Scholar
|
|
33
|
Zheng Y, He Y, Wu F, Liu M, Wang L and Wu J: Possible local treatment for liver metastases of adenoid cystic carcinoma (ACC): Single-centre experience and literature review. Transl Cancer Res. 9:4573–4582. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lupinetti AD, Roberts DB, Williams MD, Kupferman ME, Rosenthal DI, Demonte F, El-Naggar A, Weber RS and Hanna EY: Sinonasal adenoid cystic carcinoma: The M. D. Anderson cancer center experience. Cancer. 110:2726–2731. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Castelnuovo P and Turri-Zanoni M: Adenoid cystic carcinoma. Adv Otorhinolaryngol. 84:197–209. 2020.PubMed/NCBI
|
|
36
|
Jaso J and Malhotra R: Adenoid cystic carcinoma. Arch Pathol Lab Med. 135:511–515. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Mitani Y, Li J, Rao PH, Zhao YJ, Bell D, Lippman SM, Weber RS, Caulin C and El-Naggar AK: Comprehensive analysis of the MYB-NFIB gene fusion in salivary adenoid cystic carcinoma: Incidence, variability, and clinicopathologic significance. Clin Cancer Res. 16:4722–4731. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Skálová A, Hyrcza MD and Leivo I: Update from the 5th edition of the world health organization classification of head and neck tumors: Salivary glands. Head Neck Pathol. 16:40–53. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Choi SH, Yang AJ, Yoon SO, Kim HR, Hong MH, Kim SH, Choi EC, Keum KC and Lee CG: Role of postoperative radiotherapy in resected adenoid cystic carcinoma of the head and neck. Radiat Oncol. 17:1972022. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ishida E, Ogawa T, Rokugo M, Ishikawa T, Wakamori S, Ohkoshi A, Usubuchi H, Higashi K, Ishii R, Nakanome A and Katori Y: Management of adenoid cystic carcinoma of the head and neck: A single-institute study with over 25-year follow-up. Head Face Med. 16:142020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nakamura Y, Umekawa M, Shinya Y, Hasegawa H, Shin M, Katano A, Shinozaki-Ushiku A, Kondo K and Saito N: Stereotactic radiosurgery for skull base adenoid cystic carcinoma: A report of two cases. Surg Neurol Int. 13:5092022. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ali S, Palmer FL, Katabi N, Lee N, Shah JP, Patel SG and Ganly I: Long-term local control rates of patients with adenoid cystic carcinoma of the head and neck managed by surgery and postoperative radiation. Laryngoscope. 127:2265–2269. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Iseli TA, Karnell LH, Graham SM, Funk GF, Buatti JM, Gupta AK, Robinson RA and Hoffman HT: Role of radiotherapy in adenoid cystic carcinoma of the head and neck. J Laryngol Otol. 123:1137–1144. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Geiger JL, Ismaila N, Beadle B, Caudell JJ, Chau N, Deschler D, Glastonbury C, Kaufman M, Lamarre E, Lau HY, et al: Management of Salivary Gland Malignancy: ASCO Guideline. JCO. 39:1909–1941. 2021. View Article : Google Scholar
|
|
45
|
Sahara S, Herzog AE and Nör JE: Systemic therapies for salivary gland adenoid cystic carcinoma. Am J Cancer Res. 11:4092–4110. 2021.PubMed/NCBI
|
|
46
|
Papaspyrou G, Hoch S, Rinaldo A, Rodrigo JP, Takes RP, van Herpen C, Werner JA and Ferlito A: Chemotherapy and targeted therapy in adenoid cystic carcinoma of the head and neck: A review. Head Neck. 33:905–911. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ha H, Keam B, Ock CY and Heo DS: Efficacy of cyclophosphamide, doxorubicin, and cisplatin for adenoid cystic carcinoma, and their relationship with the pre-chemotherapy tumor growth rate. Chin Clin Oncol. 9:152020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kim HR, Lee SJ, Park S, Jung HA, Lee SH, Jeong HS, Chung MK and Ahn MJ: A single-arm, prospective, phase II study of cisplatin plus weekly docetaxel as first-line therapy in patients with metastatic or recurrent salivary gland cancer. Cancer Res Treat. 54:719–727. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Dewenter I, Otto S, Kakoschke TK, Smolka W and Obermeier KT: Recent advances, systemic therapy, and molecular targets in adenoid cystic carcinoma of the head and neck. J Clin Med. 12:14632023. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Xu LH, Zhao F, Yang WW, Chen CW, Du ZH, Fu M, Ge XY and Li SL: MYB promotes the growth and metastasis of salivary adenoid cystic carcinoma. Int J Oncol. 54:1579–1590. 2019.PubMed/NCBI
|
|
51
|
Lin QQ, Sun JL, Wang F, Zhang HZ, Zhou G and Xi Q: Current understanding of adenoid cystic carcinoma in the gene expression and targeted therapy. Holist Integ Oncol. 2:72023. View Article : Google Scholar
|
|
52
|
Pouloudi D, Sotiriadis A, Theodorakidou M, Sarantis P, Pergaris A, Karamouzis MV and Theocharis S: The impact of angiogenesis in the most common salivary gland malignant tumors. Int J Mol Sci. 21:93352020. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
He Q, Zhou X, Li S, Jin Y, Chen Z, Chen D, Cai Y, Liu Z, Zhao T and Wang A: MicroRNA-181a suppresses salivary adenoid cystic carcinoma metastasis by targeting MAPK-Snai2 pathway. Biochim Biophys Acta. 1830:5258–5466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Chen C, Choudhury S, Wangsa D, Lescott CJ, Wilkins DJ, Sripadhan P, Liu X, Wangsa D, Ried T, Moskaluk C, et al: A multiplex preclinical model for adenoid cystic carcinoma of the salivary gland identifies regorafenib as a potential therapeutic drug. Sci Rep. 7:114102017. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kim Y, Lee SJ, Lee JY, Lee SH, Sun JM, Park K, An HJ, Cho JY, Kang EJ, Lee HY, et al: Clinical trial of nintedanib in patients with recurrent or metastatic salivary gland cancer of the head and neck: A multicenter phase 2 study (Korean Cancer Study Group HN14-01). Cancer. 123:1958–1964. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Chau NG, Hotte SJ, Chen EX, Chin SF, Turner S, Wang L and Siu LL: A phase II study of sunitinib in recurrent and/or metastatic adenoid cystic carcinoma (ACC) of the salivary glands: Current progress and challenges in evaluating molecularly targeted agents in ACC. Ann Oncol. 23:1562–1570. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wagner VP, Ferrarotto R, Vargas PA, Martins MD, Bingle CD and Bingle L: Drug-based therapy for advanced adenoid cystic carcinoma: Current landscape and challenges based on an overview of registered clinical trials. Crit Rev Oncol Hematol. 181:1038862023. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Ferrarotto R, Sousa LG, Feng L, Mott F, Blumenschein G, Altan M, Bell D, Bonini F, Li K, Marques-Piubelli ML, et al: Phase II clinical trial of axitinib and avelumab in patients with recurrent/metastatic adenoid cystic carcinoma. J Clin Oncol. 41:2843–2851. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Tchekmedyian V, Sherman EJ, Dunn L, Tran C, Baxi S, Katabi N, Antonescu CR, Ostrovnaya I, Haque SS, Pfister DG and Ho AL: Phase II study of lenvatinib in patients with progressive, recurrent or metastatic adenoid cystic carcinoma. J Clin Oncol. 37:1529–1537. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Locati LD, Galbiati D, Calareso G, Alfieri S, Singer S, Cavalieri S, Bergamini C, Bossi P, Orlandi E, Resteghini C, et al: Patients with adenoid cystic carcinomas of the salivary glands treated with lenvatinib: Activity and quality of life. Cancer. 126:1888–1894. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Hanna GJ, Ahn MJ, Muzaffar J, Keam B, Bowles DW, Wong DJ, Ho AL, Kim SB, Worden F, Yun T, et al: A phase II trial of rivoceranib, an oral vascular endothelial growth factor receptor 2 inhibitor, for recurrent or metastatic adenoid cystic carcinoma. Clin Cancer Res. 29:4555–4563. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
van Boxtel W, Uijen MJM, Krens SD, Dijkema T, Willems SM, Jonker MA, Pegge SAH, van Engen-van Grunsven ACH and van Herpen CML: Excessive toxicity of cabozantinib in a phase II study in patients with recurrent and/or metastatic salivary gland cancer. Eur J Cancer. 161:128–137. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Lee SK, Kwon MS, Lee YS, Choi SH, Kim SY, Cho KJ and Nam SY: Prognostic value of expression of molecular markers in adenoid cystic cancer of the salivary glands compared with lymph node metastasis: A retrospective study. World J Surg Oncol. 11:2662012. View Article : Google Scholar
|
|
64
|
Kol A, van Scheltinga AT, Pool M, Gerdes C, de Vries E and de Jong S: ADCC responses and blocking of EGFR-mediated signaling and cell growth by combining the anti-EGFR antibodies imgatuzumab and cetuximab in NSCLC cells. Oncotarget. 8:45432–45446. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Agulnik M, Cohen EW, Cohen RB, Chen EX, Vokes EE, Hotte SJ, Winquist E, Laurie S, Hayes DN, Dancey JE, et al: Phase II study of lapatinib in recurrent or metastatic epidermal growth factor receptor and/or erbB2 expressing adenoid cystic carcinoma and non adenoid cystic carcinoma malignant tumors of the salivary glands. J Clin Oncol. 25:3978–3984. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Bossi P, Miceli R, Locati LD, Ferrari D, Vecchio S, Moretti G, Denaro N, Caponigro F, Airoldi M, Moro C, et al: A randomized, phase 2 study of cetuximab plus cisplatin with or without paclitaxel for the first-line treatment of patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck. Ann Oncol. 28:2820–2826. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Huang Y, Yu T, Fu X, Chen J, Liu Y, Li C, Xia Y, Zhang Z and Li L: EGFR inhibition prevents in vitro tumor growth of salivary adenoid cystic carcinoma. BMC Cell Biol. 14:132013. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Dillon PM, Chakraborty S, Moskaluk CA, Joshi PJ and Thomas CY: Adenoid cystic carcinoma: A review of recent advances, molecular targets, and clinical trials. Head Neck. 38:620–627. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Chintakuntlawar AV, Okuno SH and Price KA: Systemic therapy for recurrent or metastatic salivary gland malignancies. Cancers Head Neck. 1:112016. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Chew HY, De Lima PO, Cruz JL, Banushi B, Echejoh G, Hu L, Joseph SR, Lum B, Rae J, O'Donnell JS, et al: Endocytosis inhibition in humans to improve responses to ADCC-mediating antibodies. Cell. 180:895–914.e27. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Nightingale J, Lum B, Ladwa R, Simpson F and Panizza B: Adenoid cystic carcinoma: A review of clinical features, treatment targets and advances in improving the immune response to monoclonal antibody therapy. Biochim Biophys Acta Rev Cancer. 1875:1885232021. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Humtsoe JO, Kim HS, Leonard B, Ling S, Keam B, Marchionni L, Afsari B, Considine M, Favorov AV, Fertig EJ, et al: Newly identified members of fgfr1 splice variants engage in cross-talk with AXL/AKT axis in salivary adenoid cystic carcinoma. Cancer Res. 81:1001–1013. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Schvartsman G, Pinto NA, Bell D and Ferrarotto R: Salivary gland tumors: Molecular characterization and therapeutic advances for metastatic disease. Head Neck. 41:239–247. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Dillon PM, Petroni GR, Horton BJ, Moskaluk CA, Fracasso PM, Douvas MG, Varhegyi N, Zaja-Milatovic S and Thomas CY: A phase II study of dovitinib in patients with recurrent or metastatic adenoid cystic carcinoma. Clin Cancer Res. 23:4138–4145. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Mohamadpour M, Sherman EJ, Kriplani A, Fetten J, Dunn L, Michel LS, Hung KW, Baxi SS, McDonald E, Conybeare R, et al: A phase II study of lenvatinib plus pembrolizumab in patients with progressive, recurrent/metastatic adenoid cystic carcinoma. J Clin Oncol. 41:60482023. View Article : Google Scholar
|
|
76
|
Doddapaneni R, Tao W, Naranjo A, Nikpoor N, Tse DT and Pelaez D: Fibroblast growth factor receptor 1 (FGFR1) as a therapeutic target in adenoid cystic carcinoma of the lacrimal gland. Oncotarget. 10:480–493. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Cros J, Sbidian E, Hans S, Roussel H, Scotte F, Tartour E, Brasnu D, Laurent-Puig P, Bruneval P, Blons H and Badoual C: Expression and mutational status of treatment-relevant targets and key oncogenes in 123 malignant salivary gland tumours. Ann Oncol. 24:2624–2629. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Pfeffer MR, Talmi Y, Catane R, Symon Z, Yosepovitch A and Levitt M: A phase II study of Imatinib for advanced adenoid cystic carcinoma of head and neck salivary glands. Oral Oncol. 43:33–36. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Thanopoulou E and Judson I: The safety profile of imatinib in CML and GIST: Long-term considerations. Arch Toxicol. 86:1–12. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Hotte SJ, Winquist EW, Lamont E, MacKenzie M, Vokes E, Chen EX, Brown S, Pond GR, Murgo A and Siu LL: Imatinib mesylate in patients with adenoid cystic cancers of the salivary glands expressing c-kit: A princess margaret hospital phase II consortium study. J Clin Oncol. 23:585–590. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Wong SJ, Karrison T, Hayes DN, Kies MS, Cullen KJ, Tanvetyanon T, Argiris A, Takebe N, Lim D, Saba NF, et al: Phase II trial of dasatinib for recurrent or metastatic c-KIT expressing adenoid cystic carcinoma and for nonadenoid cystic malignant salivary tumors. Ann Oncol. 27:318–323. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Ghosal N, Mais K, Shenjere P, Julyan P, Hastings D, Ward T, Ryder WD, Bruce I, Homer J and Slevin NJ: Phase II study of cisplatin and imatinib in advanced salivary adenoid cystic carcinoma. Br J Oral Maxillofac Surg. 49:510–515. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
McIntyre JB, Ko JJ, Siever J, Chan AMY, Simpson RHW, Hao D and Lau HY: MYB-NFIB gene fusions identified in archival adenoid cystic carcinoma tissue employing NanoString analysis: An exploratory study. Diagn Pathol. 14:782019. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
de Almeida-Pinto YD, Costa SFDS, de Andrade BAB, Altemani A, Vargas PA, Abreu LG and Fonseca FP: t(6;9)(MYB-NFIB) in head and neck adenoid cystic carcinoma: A systematic review with meta-analysis. Oral Dis. 25:1277–1282. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Persson M, Andersson MK, Mitani Y, Brandwein-Weber MS, Frierson HF Jr, Moskaluk C, Fonseca I, Ferrarotto R, Boecker W, Loening T, et al: Rearrangements, expression, and clinical significance of MYB and MYBL1 in adenoid cystic carcinoma: A multi-institutional study. Cancers (Basel). 14:36912022. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Cicirò Y and Sala A: MYB oncoproteins: Emerging players and potential therapeutic targets in human cancer. Oncogenesis. 10:192021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Clesham K, Walf-Vorderwülbecke V, Gasparoli L, Virely C, Cantilena S, Tsakaneli A, Inglott S, Adams S, Samarasinghe S, Bartram J, et al: Identification of a c-MYB-directed therapeutic for acute myeloid leukemia. Leukemia. 36:1541–1549. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Yusenko MV, Trentmann A, Andersson MK, Ghani LA, Jakobs A, Paz MF, Mikesch JH, von Kries JP, Stenman G and Klempnauer KH: Monensin, a novel potent MYB inhibitor, suppresses proliferation of acute myeloid leukemia and adenoid cystic carcinoma cells. Cancer Lett. 479:61–70. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Klempnauer KH: Transcription factor MYB as therapeutic target: Current developments. Int J Mol Sci. 25:32312024. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Andersson MK, Åman P and Stenman G: IGF2/IGF1R signaling as a therapeutic target in MYB-positive adenoid cystic carcinomas and other fusion gene-driven tumors. Cells. 8:9132019. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Andersson MK, Afshari MK, Andrén Y, Wick MJ and Stenman G: Targeting the oncogenic transcriptional regulator MYB in adenoid cystic carcinoma by inhibition of IGF1R/AKT signaling. J Natl Cancer Inst. 1:1092017.
|
|
92
|
Calvo E, Soria JC, Ma WW, Wang T, Bahleda R, Tolcher AW, Gernhardt D, O'Connell J, Millham R, Giri N, et al: A phase I clinical trial and independent patient-derived xenograft study of combined targeted treatment with dacomitinib and figitumumab in advanced solid tumors. Clin Cancer Res. 23:1177–1185. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Mahadevan D, Sutton GR, Arteta-Bulos R, Bowden CJ, Miller PJ, Swart RE, Walker MS, Haluska P, Munster PN, Marshall J, et al: Phase 1b study of safety, tolerability and efficacy of R1507, a monoclonal antibody to IGF-1R in combination with multiple standard oncology regimens in patients with advanced solid malignancies. Cancer Chemother Pharmacol. 73:467–473. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Yusenko MV, Biyanee A, Frank D, Köhler LHF, Andersson MK, Khandanpour C, Schobert R, Stenman G, Biersack B and Klempnauer KH: Bcr-TMP, a novel nanomolar-active compound that exhibits both MYB- and microtubule-inhibitory activity. Cancers (Basel). 14:432021. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Feeney L, Hapuarachi B, Adderley H, Rack S, Morgan D, Walker R, Rauch R, Herz E, Kaye J, Harrington K and Metcalf R: Clinical disease course and survival outcomes following disease recurrence in adenoid cystic carcinoma with and without NOTCH signaling pathway activation. Oral Oncol. 133:1060282022. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Ferrarotto R and Heymach JV: Taking it up a NOTCH: A novel subgroup of ACC is identified. Oncotarget. 8:81725–81726. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Ferrarotto R, Mitani Y, Diao L, Guijarro I, Wang J, Zweidler-McKay P, Bell D, William WN Jr, Glisson BS, Wick MJ, et al: Activating NOTCH1 mutations define a distinct subgroup of patients with adenoid cystic carcinoma who have poor prognosis, propensity to bone and liver metastasis, and potential responsiveness to notch1 inhibitors. J Clin Oncol. 35:352–360. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Sun B, Wang Y, Sun J, Zhang C, Xia R, Xu S, Sun S and Li J: Establishment of patient-derived xenograft models of adenoid cystic carcinoma to assess pre-clinical efficacy of combination therapy of a PI3K inhibitor and retinoic acid. Am J Cancer Res. 11:773–792. 2021.PubMed/NCBI
|
|
99
|
Ferrarotto R, Wirth LJ, Muzaffar J, Rodriguez CP, Xia B, Perez CA, Bowles DW, Winquist E, Hotte SJ, Metcalf R, et al: 919MO ACCURACY a phase II trial of AL101, a selective gamma secretase inhibitor, in subjects with recurrent/metastatic (R/M) adenoid cystic carcinoma (ACC) harboring Notch activating mutations (Notchmut). Ann Oncol. 31:S6632020. View Article : Google Scholar
|
|
100
|
Hanna GJ, Stathis A, Lopez-Miranda E, Racca F, Quon D, Leyvraz S, Hess D, Keam B, Rodon J, Ahn MJ, et al: A phase I study of the pan-notch inhibitor CB-103 for patients with advanced adenoid cystic carcinoma and other tumors. Cancer Res Commun. 3:1853–1861. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Doi T, Tajimi M, Mori J, Asou H, Inoue K, Benhadji KA and Naito Y: A phase 1 study of crenigacestat (LY3039478), the Notch inhibitor, in Japanese patients with advanced solid tumors. Invest New Drugs. 39:469–476. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Ferrarotto R, Eckhardt G, Patnaik A, LoRusso P, Faoro L, Heymach JV, Kapoun AM, Xu L and Munster P: A phase I dose-escalation and dose-expansion study of brontictuzumab in subjects with selected solid tumors. Ann Oncol. 29:1561–1568. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Li Q, Huang P, Zheng C, Wang J and Ge M: Prognostic significance of p53 immunohistochemical expression in adenoid cystic carcinoma of the salivary glands: A meta-analysis. Oncotarget. 8:29458–29473. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Carlinfante G, Lazzaretti M, Ferrari S, Bianchi B and Crafa P: P53, bcl-2 and Ki-67 expression in adenoid cystic carcinoma of the palate. A clinico-pathologic study of 21 cases with long-term follow-up. Pathol Res Pract. 200:791–799. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Nör F, Warner KA, Zhang Z, Acasigua GA, Pearson AT, Kerk SA, Helman JI, Filho M, Wang S and Nör JE: Therapeutic inhibition of the MDM2-p53 interaction prevents recurrence of adenoid cystic carcinomas. Clin Cancer Res. 23:1036–1048. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Swiecicki P, Tang Y, Pearson AT, Muzaffar J, Fidler MJ, Winkler R, Fu T, Li M, Ahmad M, Yang D and Zhai Y: Trial in progress: A phase I/II trial of novel MDM2 inhibitor alrizomadlin (APG-115), with or without platinum chemotherapy, in patients with p53 wild-type salivary gland carcinoma. J Clin Oncol. 39:TPS6094. 2021. View Article : Google Scholar
|
|
107
|
He Y, Sun MM, Zhang GG, Yang J, Chen KS, Xu WW and Li B: Targeting PI3K/Akt signal transduction for cancer therapy. Sig Transduct Target Ther. 6:4252021. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Yu GT, Bu LL, Zhao YY, Liu B, Zhang WF, Zhao YF, Zhang L and Sun ZJ: Inhibition of mTOR reduce Stat3 and PAI related angiogenesis in salivary gland adenoid cystic carcinoma. Am J Cancer Res. 4:764–775. 2014.PubMed/NCBI
|
|
109
|
Liu H, Du L, Wang R, Wei C, Liu B, Zhu L, Liu P, Liu Q, Li J, Lu SL and Xiao J: High frequency of loss of PTEN expression in human solid salivary adenoid cystic carcinoma and its implication for targeted therapy. Oncotarget. 6:11477–11491. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Kim DW, Oh DY, Shin SH, Kang JH, Cho BC, Chung JS, Kim H, Park KU, Kwon JH, Han JY, et al: A multicenter phase II study of everolimus in patients with progressive unresectable adenoid cystic carcinoma. BMC Cancer. 14:7952014. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Harvey RD, Carthon BC, Lewis C, Hossain MS, Zhang C, Chen Z, Harris WB, Alese OB, Shaib W, Bilen MA, et al: Phase 1 safety and pharmacodynamic study of lenalidomide combined with everolimus in patients with advanced solid malignancies with efficacy signal in adenoid cystic carcinoma. Br J Cancer. 123:1228–1234. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Garg P, Pareek S, Kulkarni P, Horne D, Salgia R and Singhal SS: Next-Generation immunotherapy: Advancing clinical applications in cancer treatment. J Clin Med. 13:65372024. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Liu B, Zhou H, Tan L, Siu KTH and Guan XY: Exploring treatment options in cancer: Tumor treatment strategies. Signal Transduct Target Ther. 9:1752024. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Waldman AD, Fritz JM and Lenardo MJ: A guide to cancer immunotherapy: From T cell basic science to clinical practice. Nat Rev Immunol. 20:651–668. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Wolkow N, Jakobiec FA, Afrogheh AH, Kidd M, Eagle RC, Pai SI and Faquin WC: PD-L1 and PD-L2 expression levels are low in primary and secondary adenoid cystic carcinomas of the orbit: Therapeutic implications. Ophthalmic Plast Reconstr Surg. 36:444–450. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Dou S, Li R, He N, Zhang M, Jiang W, Ye L, Yang Y, Zhao G, Yang Y, Li J, et al: The immune landscape of chinese head and neck adenoid cystic carcinoma and clinical implication. Front Immunol. 12:6183672021. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Sato R, Yamaki H, Komatsuda H, Wakisaka R, Inoue T, Kumai T and Takahara M: Exploring immunological effects and novel immune adjuvants in immunotherapy for salivary gland cancers. Cancers (Basel). 16:12052024. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Fayette J, Even C, Digue L, Geoffrois L, Rolland F, Cupissol D, Guigay J, Tourneau CL, Dillies AF, Zanetta S, et al: NISCAHN: A phase II, multicenter nonrandomized trial aiming at evaluating nivolumab (N) in two cohorts of patients (pts) with recurrent/metastatic (R/M) salivary gland carcinoma of the head and neck (SGCHN), on behalf of the unicancer head & neck group. J Clin Oncol. 37:60832019. View Article : Google Scholar
|
|
119
|
Vos JL, Burman B, Jain S, Fitzgerald CWR, Sherman EJ, Dunn LA, Fetten JV, Michel LS, Kriplani A, Ng KK, et al: Nivolumab plus ipilimumab in advanced salivary gland cancer: A phase 2 trial. Nat Med. 29:3077–3089. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Mahmood U, Bang A, Chen YH, Mak RH, Lorch JH, Hanna GJ, Nishino M, Manuszak C, Thrash EM, Severgnini M, et al: A randomized phase 2 study of pembrolizumab with or without radiation in patients with recurrent or metastatic adenoid cystic carcinoma. Int J Radiat Oncol Biol Phys. 109:134–144. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Mosconi C, de Arruda JAA, de Farias ACR, Oliveira GAQ, de Paula HM, Fonseca FP, Mesquita RA, Silva TA, Mendonça EF and Batista AC: Immune microenvironment and evasion mechanisms in adenoid cystic carcinomas of salivary glands. Oral Oncol. 88:95–101. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Guazzo E, Cooper C, Wilkinson L, Feng S, King B, Simpson F, Porceddu S, Panizza B and Coward JIG: Therapeutic implications of immune-profiling and EGFR expression in salivary gland carcinoma. Head Neck. 43:768–777. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Chang H, Kim JS, Choi YJ, Cho JG, Woo JS, Kim A, Kim JS and Kang EJ: Overexpression of PD-L2 is associated with shorter relapse-free survival in patients with malignant salivary gland tumors. Onco Targets Ther. 10:2983–2992. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Muraro E, Romanò R, Fanetti G, Vaccher E, Turturici I, Lupato V, La Torre FB, Polesel J, Fratta E, Giacomarra V, et al: Tissue and circulating PD-L2: Moving from health and immune-mediated diseases to head and neck oncology. Crit Rev Oncol Hematol. 175:1037072022. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Pham T, Pereira L, Roth S, Galletta L, Link E, Akhurst T, Solomon B, Michael M, Darcy P, Sampurno S, et al: First-in-human phase I clinical trial of a combined immune modulatory approach using TetMYB vaccine and Anti-PD-1 antibody in patients with advanced solid cancer including colorectal or adenoid cystic carcinoma: The MYPHISMO study protocol (NCT03287427). Contemp Clin Trials Commun. 16:1004092019. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Parvez A, Choudhary F, Mudgal P, Khan R, Qureshi KA, Farooqi H and Aspatwar A: PD-1 and PD-L1: Architects of immune symphony and immunotherapy breakthroughs in cancer treatment. Front Immunol. 14:12963412023. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Cross RS, Malaterre J, Davenport AJ, Carpinteri S, Anderson RL, Darcy PK and Ramsay RG: Therapeutic DNA vaccination against colorectal cancer by targeting the MYB oncoprotein. Clin Transl Immunology. 4:e302015. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Shailesh H, Zakaria ZZ, Baiocchi R and Sif S: Protein arginine methyltransferase 5 (PRMT5) dysregulation in cancer. Oncotarget. 9:36705–36718. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Feustel K and Falchook GS: Protein arginine methyltransferase 5 (PRMT5) inhibitors in oncology clinical trials: A review. J Immunother Precis Oncol. 5:58–67. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Siu L, Rasco D, Vinay SP, Romano PM, Menis J, Opdam F, Heinhuis K, Egger J, Gorman S, Parasrampuria R, et al: METEOR-1: A phase I study of GSK3326595, a first-in-class protein arginine methyltransferase 5 (PRMT5) inhibitor, in advanced solid tumours. Ann Oncol. 30:v1592019. View Article : Google Scholar
|
|
131
|
Ferrarotto R, Swiecicki PL, Zandberg DP, Baiocchi RA, Wesolowski R, Rodriguez CP, McKean M, Kang H, Monga V, Nath R, et al: PRT543, a protein arginine methyltransferase 5 inhibitor, in patients with advanced adenoid cystic carcinoma: An open-label, phase I dose-expansion study. Oral Oncol. 149:1066342024. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Long Y, Yao DS, Wei YS and Wu GT: Effects of nerve growth factor expression on perineural invasion and worse prognosis in early-stage cervical cancer. Chin Med J (Engl). 131:2360–2363. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Chung V, Wang L, Fletcher MS, Massarelli E, Cristea MC, Kamaraju S, Alistar AT, Feng C, Li Y, Whiting RL, et al: First-time in-human study of VMD-928, an oral allosteric TrkA selective inhibitor targeting TrkA protein overexpression, in patients with solid tumors or lymphoma. J Clin Oncol. 39:30812021. View Article : Google Scholar
|
|
134
|
Sivrice ME, Yasan H, Kumbul YÇ, Ertunç O and Sayın S: The importance of prostate-specific membrane antigen expression in salivary gland tumors. Turk Arch Otorhinolaryngol. 60:206–211. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Nulent TJW, Valstar MH, Smit LA, Smeele LE, Zuithoff NPA, de Keizer B, de Bree R, van Es RJJ and Willems SM: Prostate-specific membrane antigen (PSMA) expression in adenoid cystic carcinoma of the head and neck. BMC Cancer. 20:5192020. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Lauri C, Chiurchioni L, Russo VM, Zannini L and Signore A: PSMA expression in solid tumors beyond the prostate gland: Ready for theranostic applications? J Clin Med. 11:65902022. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
van Boxtel W, Lütje S, van Engen-van Grunsven ICH, Verhaegh GW, Schalken JA, Jonker MA, Nagarajah J, Gotthardt M and van Herpen CML: 68Ga-PSMA-HBED-CC PET/CT imaging for adenoid cystic carcinoma and salivary duct carcinoma: A phase 2 imaging study. Theranostics. 10:2273–2283. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Tan BF, Tan WCC, Wang FQ, Lechner M, Schartinger VH, Tan DSW, Loke KSH and Nei WL: PSMA PET imaging and therapy in adenoid cystic carcinoma and other salivary gland cancers: A systematic review. Cancers (Basel). 14:35852022. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Revathidevi S and Munirajan AK: Akt in cancer: Mediator and more. Semin Cancer Biol. 59:80–91. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Ho AL, Foster NR, Vasudeva SD, Katabi N, Antonescu CR, Frenette GP, Pfister DG, Erlichman C and Schwartz GK: A phase 2 study of MK-2206 in patients with incurable adenoid cystic carcinoma. Cancer. 130:702–712. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
García-Regalado A, Vargas M, García-Carrancá A, Aréchaga-Ocampo E and González-De la Rosa CH: Activation of Akt pathway by transcription-independent mechanisms of retinoic acid promotes survival and invasion in lung cancer cells. Mol Cancer. 12:442013. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Sun HR, Wang S, Yan SC, Zhang Y, Nelson PJ, Jia HL, Qin LX and Dong QZ: Therapeutic strategies targeting cancer stem cells and their microenvironment. Front Oncol. 9:11042019. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Adams A, Warner K and Nör JE: Salivary gland cancer stem cells. Oral Oncol. 49:845–853. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Cojoc M, Mäbert K, Muders MH and Dubrovska A: A role for cancer stem cells in therapy resistance: Cellular and molecular mechanisms. Semin Cancer Biol. 31:16–27. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Sun S and Wang Z: ALDH high adenoid cystic carcinoma cells display cancer stem cell properties and are responsible for mediating metastasis. Biochem Biophys Res Commun. 396:843–848. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Almeida LO, Guimarães DM, Martins MD, Martins MAT, Warner KA, Nör JE, Castilho RM and Squarize CH: Unlocking the chromatin of adenoid cystic carcinomas using HDAC inhibitors sensitize cancer stem cells to cisplatin and induces tumor senescence. Stem Cell Res. 21:94–105. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Manou M, Kanakoglou DS, Loupis T, Vrachnos DM, Theocharis S, Papavassiliou AG and Piperi C: Role of histone deacetylases in the pathogenesis of salivary gland tumors and therapeutic targeting options. Int J Mol Sci. 24:100382023. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Topacio BR, Zatulovskiy E, Cristea S, Xie S, Tambo CS, Rubin SM, Sage J, Kõivomägi M and Skotheim JM: Cyclin D-Cdk4,6 drives cell-cycle progression via the retinoblastoma protein's C-Terminal Helix. Mol Cell. 74:758–770. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Esche C, Stellato C and Beck LA: Chemokines: Key players in innate and adaptive immunity. J Invest Dermatol. 125:615–628. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Shi Y, Riese DJ II and Shen J: The role of the CXCL12/CXCR4/CXCR7 chemokine axis in cancer. Front Pharmacol. 11:5746672020. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Sun X, Cheng G, Hao M, Zheng J, Zhou X, Zhang J, Taichman RS, Pienta KJ and Wang J: CXCL12/CXCR4/CXCR7 chemokine axis and cancer progression. Cancer Metastasis Rev. 29:709–722. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Nulent TJW, van Es RJJ, Valstar MH, Smeele LE, Smit LA, Gunnewiek RK, Zuithoff NPA, de Keizer B, de Bree R and Willems SM: High CXCR4 expression in adenoid cystic carcinoma of the head and neck is associated with increased risk of locoregional recurrence. J Clin Pathol. 73:476–482. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Hamshaw I, Cominetti MD, Lai WY, Searcey M and Mueller A: The development of potent, competitive CXCR4 antagonists for the prevention of cancer metastasis. Biochem Pharmacol. 218:1159212023. View Article : Google Scholar : PubMed/NCBI
|