Introduction
The incidence of multiple primary cancers (MPC) is
rising in the general population (1) and accounts for 2–17% of all cancer
cases (2,3). The pathogenesis of MPC is complex and
multifactorial. The pathogenesis involves genetic susceptibility,
environmental exposures, lifestyle factors, immune system
abnormalities and treatment-related side effects (4). Due to the rarity and complexity of
MPC, available data and literature are limited, leading to a lack
of unified guidelines and consensus on its diagnosis and treatment.
Accurate histopathological classification and staging of MPC are
crucial, as they provide the foundation for individualized
treatment strategies tailored to each tumor type (5). This approach helps address the
challenges posed by MPC and improves treatment outcomes and quality
of life of patients.
Cervical cancer is one of the most prevalent
malignancies of the female reproductive system, and the incidence
of synchronous double primary malignancies in patients with
cervical cancer is relatively low (6). According to the literature, cervical
cancer may coexist with various other cancer types, including
endometrial, ovarian, breast, colorectal and lung cancer (6–8).
However, the simultaneous occurrence of primary lymphoma in
patients with cervical cancer is exceedingly rare. The present
report aims to highlight a rare case involving a 46-year-old female
patient diagnosed with dual primary malignancies: Cervical cancer
and FL. The specific objective of this case report is to address
the diagnostic challenges and clinical significance encountered
when evaluating cervical cancer patients with isolated para-aortic
lymph node enlargement. Through this case, we seek to emphasize the
importance of surgical intervention, which is crucial for
differentiating between lymph node metastasis and the presence of a
second primary tumor, thereby impacting treatment decisions and
patient outcomes.
Case report
In September 2023, a 46-year-old female patient
presented to Xiangyang First People's Hospital (Xiangyang, China),
with a chief complaint of vaginal bleeding lasting 28 days. The
female patient had previously experienced regular menstrual cycles
but reported changes over the past 6 months, with cycles starting
7–15 days earlier than usual. However, there were no marked changes
in the duration or volume of menstrual flow; thus, it did not raise
any concern. Over the past month, the patient experienced
continuous vaginal bleeding, which resembled menstrual flow. The
gynecological examination, including a bimanual examination,
revealed an enlarged cervix with erosive changes (3.0×2.0
cm2) and active bleeding upon contact. The uterus was
retroverted and irregularly shaped (7.0×6.0×6.0 cm3),
with no abnormalities in the surrounding area. A cervical biopsy
and endocervical curettage were subsequently performed under
colposcopic guidance. Cervical curettage samples were fixed in 4%
formalin at room temperature for 12 h, embedded in paraffin at 60°C
for 15 min, sectioned to a thickness of 4 µm, stained with
hematoxylin and eosin for 5 min at room temperature, and then
observed under a light microscope, confirming the diagnosis of
squamous cell carcinoma (Fig. S1).
Laboratory tests showed that the tumor marker CA-125 was elevated
at 112.5 IU/ml (normal range: 0–35 IU/ml), and the squamous cell
carcinoma antigen (SCC) was 5.27 ng/ml (normal range: 0–1.5 ng/ml),
both exceeding the normal range. Real-time fluorescence
quantitative PCR for human papillomavirus (HPV) nucleic acid typing
indicated a positive result for the high-risk subtype HPV 16.
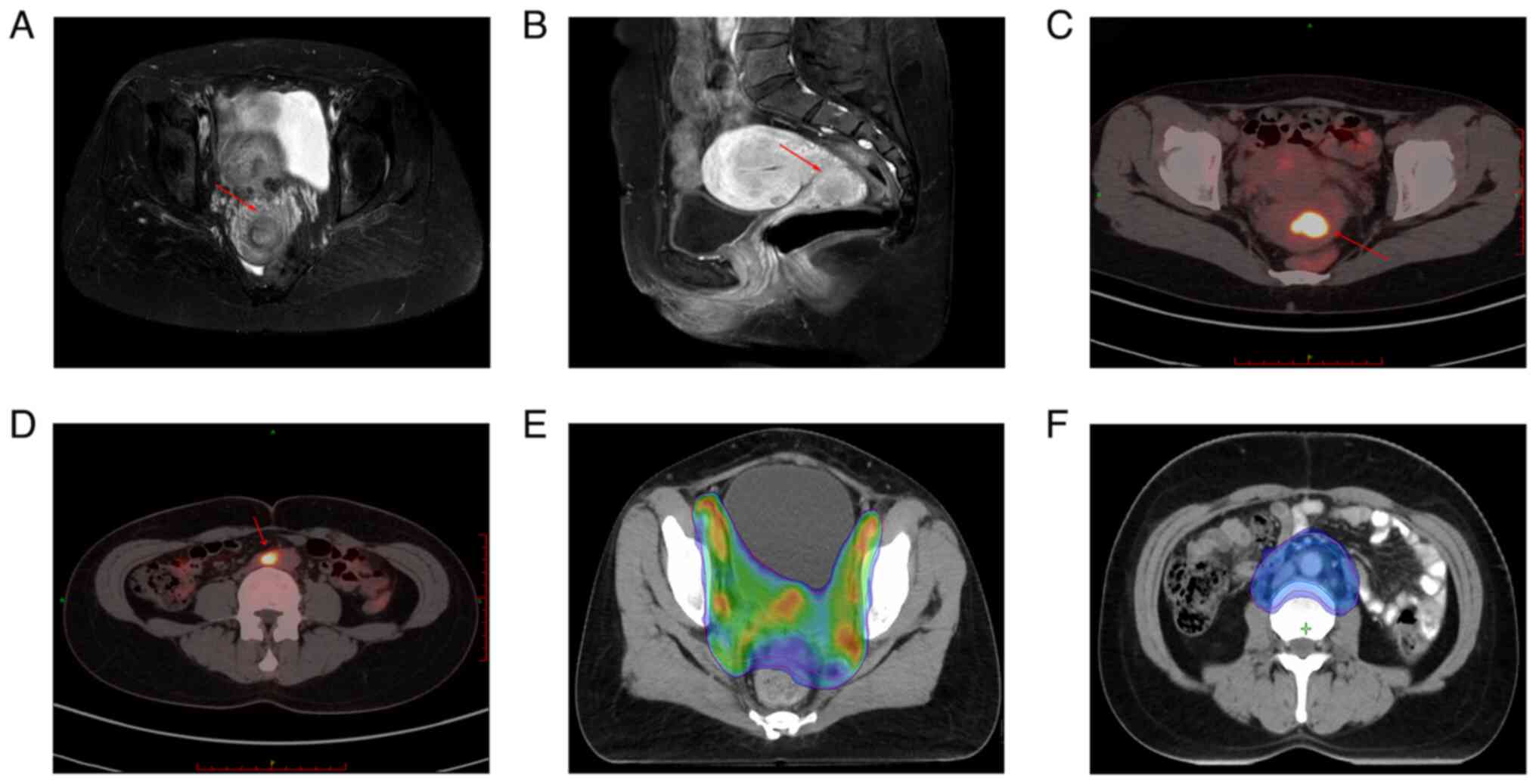
Pelvic enhanced magnetic resonance imaging revealed a slightly
hyperintense lesion in the cervix, which was ~2.1×2.4×2.3
cm3 in size, with poorly defined boundaries (Fig. 1A and B). The lesion involved the
anterior and posterior fornices but exhibited no infiltration into
the parametrium, raising a high suspicion of cervical cancer.
Whole-body positron emission tomography-computed tomography
(PET-CT) revealed an occupying lesion in the cervical region
(Fig. 1C) and a soft tissue density
lesion between the infrarenal abdominal aorta and the inferior vena
cava, with increased abnormal metabolism, which suggested a
malignant cervical tumor with metastatic lymph nodes (Fig. 1D).
Given the relatively localized nature of the primary
cervical lesion and the isolated retroperitoneal lymph node
metastasis indicated by PET-CT, thorough discussions with the
patient and her family were performed regarding treatment options.
Two primary approaches were considered: First, surgery could be
performed to determine tumor staging through postoperative
pathology, though this option involves significant risks, including
bleeding. Should the retroperitoneal lymph nodes be confirmed to be
metastatic post-surgery, concurrent radiotherapy and chemotherapy
would follow. Alternatively, if surgery was not pursued, concurrent
radiotherapy and chemotherapy were advised for the patient's
condition. After careful consideration, the patient strongly
favored surgical intervention, culminating in a laparoscopic total
hysterectomy, high-level ligation of the ovarian vessels, bilateral
salpingo-oophorectomy, pelvic lymphadenectomy and para-aortic lymph
node excision. Cervical and lymphoid tissues were subjected to
H&E staining and immunohistochemical staining, observed using
an Olympus BX53 optical microscope. The H&E staining method
followed the protocol for cervical smear samples detailed above.
For immunohistochemical staining, tumor tissues were embedded in
paraffin and sectioned into 4-µm slices. These sections underwent
deparaffinization and rehydration. Heat-induced antigen retrieval
was performed using 10 mM citrate buffer (pH 6.0). Endogenous
peroxidase activity was blocked by incubating with 3%
H2O2 for 10 min. Sections were permeabilized
with 0.1% Triton X-100. To prevent non-specific binding, sections
were incubated for 25 min at room temperature in PBS-T (QuickBlock™
Blocking Buffer; Beyotime Institute of Biotechnology) containing
10% goat serum. The following primary antibodies were then applied
and incubated overnight at 4°C: For cervical tissue, cytokeratin
5/6 (CK5/6; cat. no. PA6040; dilution, 1:100), P40 (cat. no.
PA7069; dilution, 1:200), P16 (cat. no. PA6909; dilution, 1:50);
for lymphoid tissue, CD20 (cat. no. PA6149; dilution, 1:200),
paired box 5 (PAX-5; cat. no. PA6688; dilution, 1:50), CD10 (cat.
no. PA6911; dilution, 1:100) and Bcl-2 (cat. no. PA7109; dilution,
1:200). Bcl-6 (cat. no. ab272859; dilution, 1:100) was supplied by
Abcam. After washing, HRP-conjugated secondary antibodies were
added at a dilution of 1:50 (cat. no. A0216; Beyotime Institute of
Biotechnology) and incubated for 20 min at room temperature. DAB
(DAB Horseradish Peroxidase Color Development Kit; cat. no. P0203;
Beyotime Institute of Biotechnology) was then applied for color
development in the dark for 30 sec to 5 min. The staining reaction
was monitored under a microscope and terminated with distilled
water. Finally, sections were counterstained with hematoxylin for
30 sec at room temperature. Images were acquired using an optical
microscope. Immunostained sections were imaged with a Leica DM4000B
fluorescence microscope (Leica Microsystems GmbH).
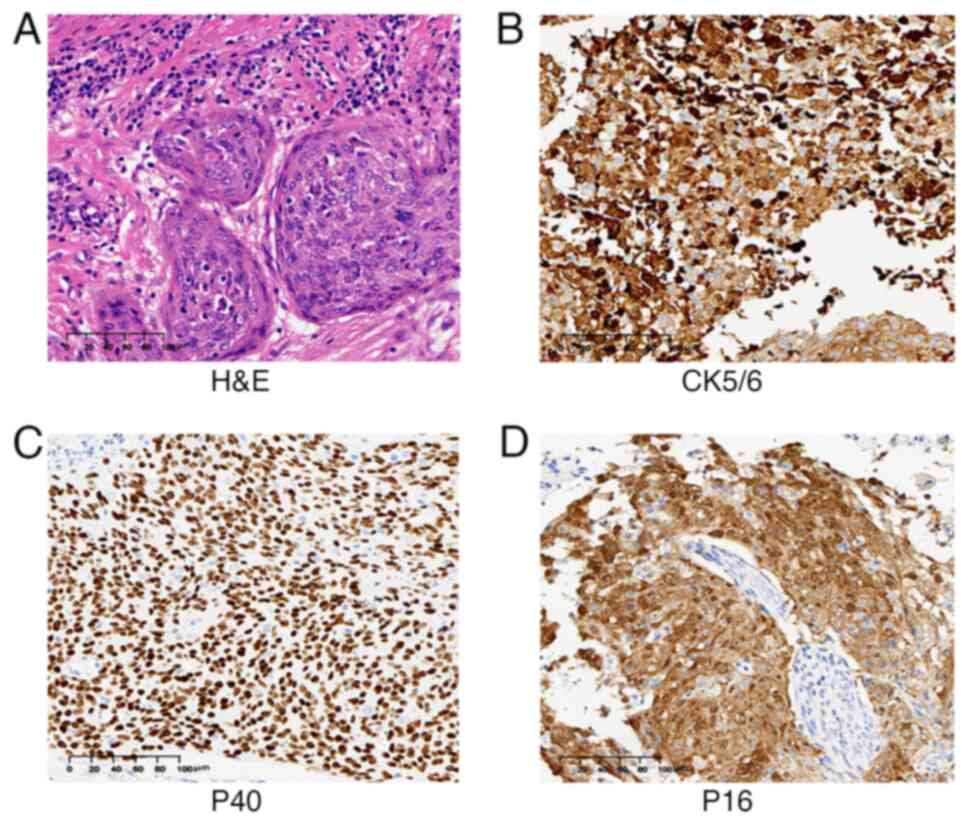
Based on the experimental methods described above,
postoperative pathological examination utilizing H&E staining
revealed prominent nuclear enlargement and irregular cellular
morphology, along with an elevated nuclear-to-cytoplasmic ratio, as
well as varying degrees of destruction in glandular and squamous
epithelial structures (9).
Additionally, immunohistochemical analysis demonstrated positive
expression of CK5/6, P40 and P16, confirming a diagnosis of
invasive squamous cell carcinoma (Fig.
2A-D). Postoperative immunohistochemical analysis showed that
the tumor had infiltrated more than two-thirds of the cervical
fibromuscular layer, with tumor emboli present in blood vessels but
no evidence of neural invasion. The stromal tissue was involved. No
cancer infiltration was observed in the bilateral parametrium,
adnexa or vaginal margins, and there was no lymph node metastasis
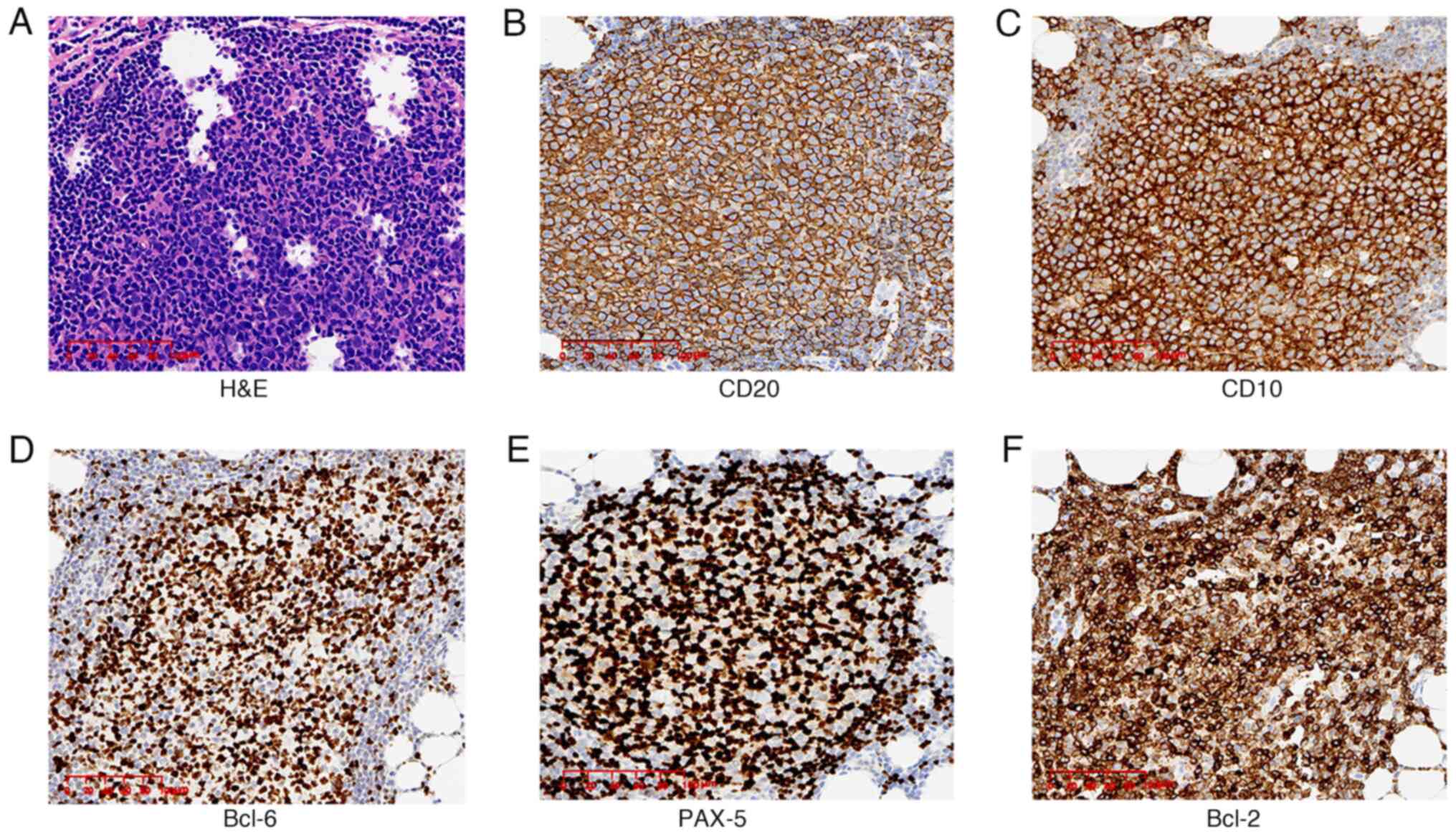
in the pelvic or para-aortic lymph nodes. Notably, the
retroperitoneal lymph nodes exhibited lymphoid follicle
hyperplasia, with some follicles irregularly fused and losing
polarity under microscopic examination (Fig. 3A). Immunohistochemical analysis
demonstrated positivity for CD20, PAX-5, CD10, Bcl-6 and Bcl-2
(Fig. 3B-F), with a Ki-67 index of
20%. Based on the morphological and histopathological findings
(10), a final diagnosis of
para-aortic FL, grade 1–2, was made. The FL International
Prognostic Index-2 scoring system for prognostic evaluation was
utilized (11,12), which includes the following factors:
Age, whether the hemoglobin level is <120 g/l, the normality of
β2-microglobulin, the presence of bone marrow involvement and
whether the largest lymph node diameter exceeds 6 cm. According to
these scoring criteria, the hemoglobin level was 93 g/l, which is
below 120 g/l, resulting in a score of 1. The final prognosis was
classified as intermediate risk. During clinical assessment,
genetic testing and fluorescence in situ hybridization
analysis were recommended. However, due to financial
considerations, the patient opted not to proceed with these
additional tests. The final diagnosis was therefore double primary
tumors: i) Cervical squamous cell carcinoma, stage IB2 (according
to the 2018 FIGO staging) (13);
and ii) FL, grade 1–2, stage I.
According to the National Comprehensive Cancer
Network (NCCN) B-cell Lymphoma Guidelines (2023.6 Edition)
(14), for patients with stage I
and grade1-2FL, adjuvant radiotherapy can be administered following
surgical treatment to enhance local control rates and reduce the
risk of recurrence. The patient received adjuvant radiotherapy 1
month after surgery. Intensity-modulated radiation therapy was
delivered to the retroperitoneal lymph node drainage area, with a
planned total dose of 30.6 Gy administered in 17 fractions, each
delivering a dose of 1.8 Gy. Radiation treatment was conducted from
Monday to Friday, with weekends off, targeting planning volume 1
(Fig. 1E). According to the NCCN
Cervical Cancer Guidelines (2020 Version 1) (15), if a patient has undergone radical
surgical resection and the pathological results indicate the
presence of vascular cancer emboli and risk factors such as an
invasive depth greater than 2/3 of the fibromuscular layer, pelvic
external beam radiation therapy may be considered. For the residual
vaginal and lymph node drainage areas, the prescribed dose was 46.8
Gy delivered in 28 fractions to the planning target volume 2
(Fig. 1F). Following the respective
disease-specific guidelines, no additional treatment is required at
this stage, with the focus primarily on regular follow-up. As of
January 2025, the patient returns to the hospital every 3 months
for abdominal MRIs, chest CT scans and tumor marker tests, during
which no tumor progression has been observed, and the patient is
recovering well.
Discussion
MPC refers to the simultaneous or sequential
occurrence of two or more distinct types of cancers in the same
individual. The concept of MPC was first described in 1921
(16). Warren and Gates (17) established three criteria for
diagnosing MPC: Each tumor must have distinct histological
characteristics, each tumor must exhibit well-defined malignant
features and the possibility that one tumor is a metastatic lesion
from another must be excluded. The simultaneous occurrence of
cervical squamous cell carcinoma and FL as MPC is extremely rare.
To the best of our knowledge, the present report was the first to
describe a case of MPC involving both cervical squamous cell
carcinoma and low-grade FL.
The pathogenesis of MPC is not fully understood;
however, it is considered to involve complex, multifactorial
processes, including genetic predisposition, immune deficiencies,
immune evasion by cancer cells, accumulation of gene mutations and
abnormal gene expression, as well as exposure to radiation therapy,
chemotherapy and certain medications (18,19).
Cervical cancer, a common tumor type in MPC, has been extensively
studied to investigate its underlying mechanisms (20,21).
The coexistence of endometrial and cervical cancers is not
uncommon, possibly due to their occurrence in adjacent sites within
the reproductive system (6,22). The simultaneous presence of cervical
cancer and breast or ovarian cancer may involve shared driver gene
mutations, such as those in BRCA1 and BRCA2 (23,24).
The coexistence of colorectal and cervical cancers may be
attributed to shared embryonic origins and underlying genetic
factors (25). HPV infection can
induce cell proliferation and mutation, and can potentially promote
cancer development through mechanisms such as interference with
cell cycle control, inhibition of apoptosis and activation of
proliferation signaling pathways (26). HPV types 16 and 18 are particularly
known for their oncogenic potential, leading to the transformation
of cervical epithelial cells and the subsequent development of
cervical intraepithelial neoplasia and invasive cervical cancer
(27). It is estimated that >99%
of cervical cancers are associated with HPV infection (28). Lymphoma occurrence is also closely
related to viral infections, with Epstein-Barr virus infection
being common in Hodgkin lymphoma, natural killer/T-cell lymphoma
and diffuse large B-cell lymphoma (29). Previous literature has suggested a
possible association between HPV infection and certain types of
lymphoma, notably detecting HPV DNA positivity in cases of Hodgkin
lymphoma and some diffuse large B-cell lymphomas (30,31).
Animal studies have demonstrated that immune system alterations
resulting from HPV infection may affect lymphocyte function,
thereby increasing susceptibility to lymphoma development,
particularly in immunocompromised individuals such as those with
HIV/acquired immunodeficiency syndrome (32,33).
This suggests that HPV may serve a role in the pathogenesis of
lymphoma. The female patient in the present case study also had an
HPV infection, specifically a high-risk subtype. While the
potential relationship between HPV and lymphoma has not been fully
elucidated, the role of HPV infection in the development of
cervical cancer and FL warrants further investigation.
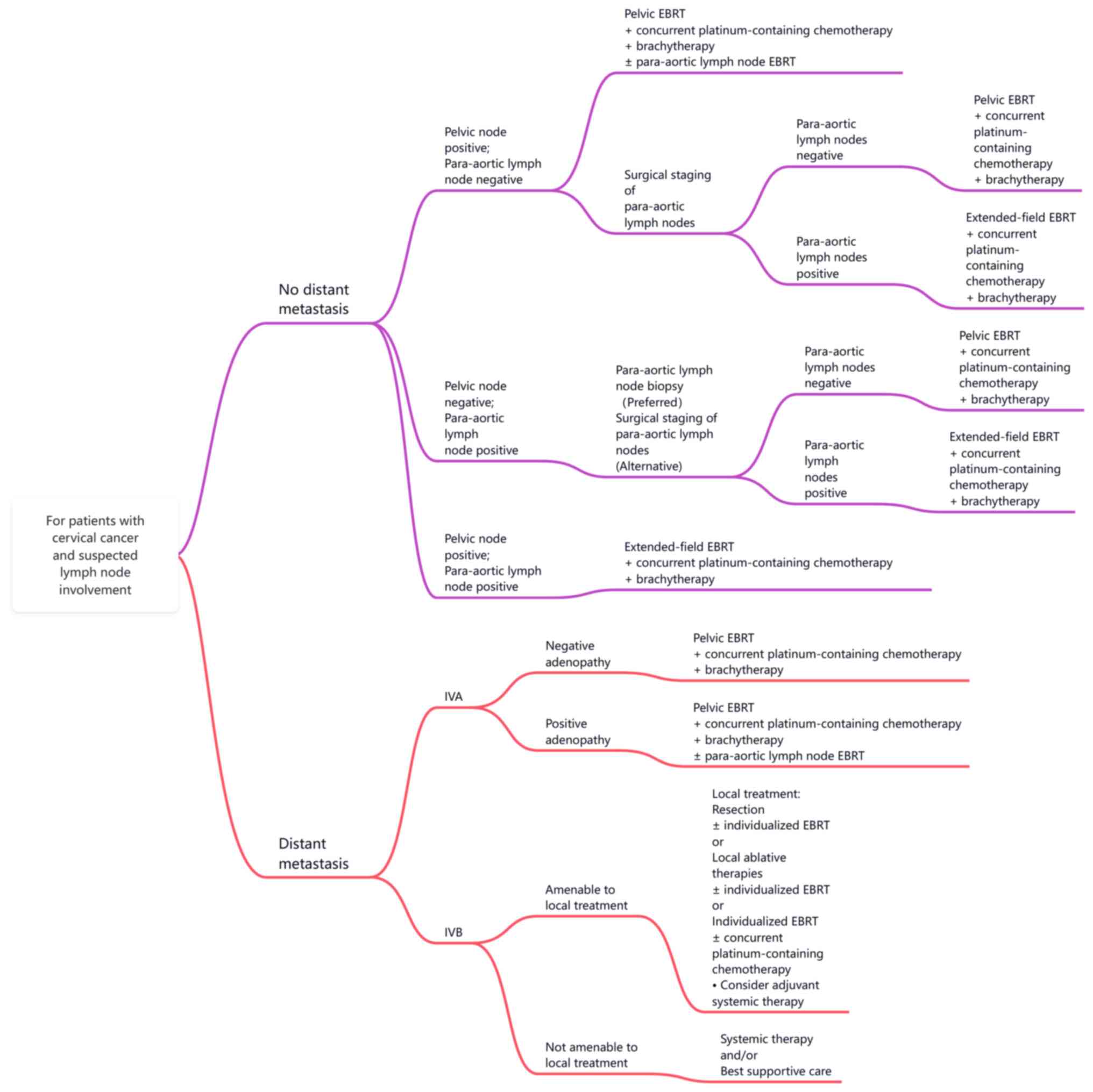
In the absence of a definitive diagnosis of MPC, the
primary challenge in managing the patient was deciding whether to
perform surgery first or to proceed with concurrent
chemoradiotherapy. According to the revised International
Federation of Gynaecology and Obstetrics 2018 staging criteria for
cervical cancer, the presence of lymph node metastasis in the
para-aortic region is a crucial factor for treatment
decision-making and prognosis in patients with cervical cancer
(34). According to the NCCN
Cervical Cancer Guidelines (2020 Version 1) (15), if the para-aortic lymph nodes were
deemed metastatic, the patient would be classified as having stage
III C2 invasive cervical squamous cell carcinoma, thus
necessitating concurrent chemoradiotherapy as the primary treatment
modality. Conversely, in the absence of para-aortic lymph node
metastasis, the patient would be diagnosed with stage IB2 disease,
making surgical resection the main therapeutic approach. Clinicians
face challenges in determining whether para-aortic lymph node
enlargement is due to metastasis or represents a primary
lesion.
Kostov et al (35) introduced a three-tier lymph node
staging system for cervical cancer: Tier one includes the
para-uterine, obturator, internal iliac and external iliac lymph
nodes; tier two encompasses the common iliac and presacral lymph
nodes; and tier three consists of the para-aortic lymph nodes. Most
tumor lymph node metastases typically progress sequentially from
tier one to tier two, and then to tier three. Depending on the
tumor type, approximately 5 to 10% of cases may exhibit cross-tier
metastasis (36,37). This pattern suggests that patients
with para-aortic lymph node metastasis often have concurrent
involvement of pelvic lymph nodes (38,39).
However, in the present case, the PET-CT indicated only possible
para-aortic lymph node metastasis, with no evidence of metastasis
in the pelvic lymph nodes. This represents a rare occurrence of
lymph nodes crossing tiers based solely on imaging diagnosis.
Several studies have reported the relatively low sensitivity and
negative predictive value of PET-CT in diagnosing para-aortic lymph
node metastasis, highlighting the potential for false-positive or
false-negative results (40,41).
Given the inherent limitations of imaging
examinations, such as the possibility of false negatives or
positives, there is a risk of administering either inadequate or
excessive treatment to patients. Therefore, in the context of
precision medicine, surgical staging offers a favorable approach by
providing accurate lymph node pathology results. Considering the
lack of reproductive needs of the patient and the localization of
the cervical lesion confirmed by imaging, laparoscopic total
hysterectomy and para-aortic lymph node excision were performed.
Postoperative pathology confirmed the diagnosis of MPC. Both tumors
were in the early stages, which makes surgery the most critical
treatment method. However, upon further consideration, if the
authors had proceeded with concurrent chemoradiotherapy based on a
diagnosis of stage IIIC cervical cancer, the patient would not only
have been misdiagnosed but also potentially overtreated and the
opportunity for surgery would be missed. Therefore, when patients
with cervical cancer present with a skip pattern or unusual lymph
node enlargement suspected of metastasis, surgery or biopsy is
essential. According to the recommendations of the NCCN cervical
cancer guidelines and the authors' experience (15), a diagnostic and management flowchart
for patients with suspected lymph node metastasis in cervical
cancer was developed (Fig. 4).
Another controversial issue is whether adjuvant
radiotherapy is necessary after surgery. According to the NCCN
guidelines for cervical cancer, surgery is the preferred treatment
option for patients with stages up to IIB, while concurrent
chemoradiotherapy is recommended for those beyond stage IIB
(42). In the present case, the
patient had stage IB2 cervical squamous cell carcinoma. Although
the para-aortic lymph nodes were negative, the tumor had invaded
more than two-thirds of the cervical fibromuscular layer and blood
vessels. According to the criteria of Sedlis et al (43), the patient exhibited
intermediate-risk factors. Therefore, postoperative radiotherapy to
the cervical stump and pelvic lymphatic drainage areas was
administered to reduce the risk of relapse (44). For early-stage FL, even when the
primary lesion is resected, our preference would be to administer
field radiation therapy (14).
It is worth considering whether cervical cancer and
FL occurred simultaneously or sequentially in the present case.
Previous studies suggest that in patients with MPC, FL often
appears subsequently and frequently follows cancer treatment,
especially after chemotherapy or radiotherapy (45,46).
For example, FL has been documented in patients who received
immunotherapy for lung cancer and in individuals with a history of
breast cancer who underwent radiation therapy (47,48).
To date, research specifically addressing secondary lymphomas
arising from cervical cancer is lacking. This further emphasizes
the importance of early cancer screening, raising our concern.
Managing MPC requires the collaborative efforts of a
multidisciplinary team, including surgeons, oncologists,
radiologists and pathologists (49). Effective cancer treatment must
consider key factors such as tumor stage, anatomical location and
the physical condition of the patient. In the present case, despite
the initial stage III diagnosis based on imaging, surgical
intervention was carefully performed, which ultimately confirmed
the presence of low-grade FL adjacent to the abdominal aorta. The
present case underscores the importance of lymph node biopsy for
suspected abdominal aortic lymph node metastasis and emphasizes
that MPC treatment should be individualized.
A study revealed that the prognosis of patients with
MPC is generally poorer compared with that of patients with a
solitary primary tumor (50). The
prognosis of these patients is influenced by various factors,
including tumor stage, biological characteristics, treatment
response and overall physical condition (51). Given the limited data and the rarity
of cases involving concurrent cervical cancer and FL, evaluating
the prognosis of these patients presents challenges. Therefore,
there is an urgent need to gather more similar cases, establish
standardized treatment protocols and conduct comprehensive
prognostic assessments.
A limitation of the present study is the absence of
genetic testing of the patient due to financial constraints.
Research indicates that MPC may share common driver genes, such as
KRAS or BRCA mutations identified in concurrent cases of breast and
ovarian cancer, suggesting a shared pathway in oncogenesis
(52,53). This underscores the imperative role
of genetic testing in elucidating the underlying mechanisms of
these malignancies and providing critical insights into potential
diagnostic markers and therapeutic targets. This limitation may
affect the comprehensiveness of the present findings and the
potential for personalized treatment strategies. Future studies
should prioritize genetic testing to deepen the understanding of
the relationship between synchronous tumors and improve patient
management.
In conclusion, this report presents a unique case of
concurrent cervical cancer and low-grade FL. This case provides new
clinical insights and serves as a reference in the literature on
MPC. The mechanisms underlying the simultaneous occurrence of these
two conditions remain unclear, which highlights the need for
further research to understand their etiology and develop effective
therapeutic strategies.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by National Natural Science
Foundation of China (grant no. 82200214), Foundation of Hubei
Xiangyang No. 1 People's Hospital of Youth programs (grant no.
XYYY2021Q07), the Natural Science Foundation of Hubei Province
(grant no. 2022CFB890), The Natural Science Foundation of Hubei
Provincial Department of Education (grant no. Q20212105) and Hubei
Province Health and Family Planning Scientific Research Project
(grant no. WJ2023F076).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
DZ and YD conceptualized the present study. SL, HL,
YD and HY curated the data, acquired and managed the patients and
provided the radiology images. DZ, HY and SL contributed to the
study design and analyzed and interpreted the data. SL and HY
confirm the authenticity of all the raw data. All authors helped to
write the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved (approval no.
XYYY20240074) by the Ethics and Scientific Committee of Hubei
University of Medicine (Xiangyang, China). Written informed consent
was obtained from the individual for participation in the study,
including the publication of any potentially identifiable images or
data included in this article.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of any potentially identifiable images
or data included in the present study.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
MPC
|
multiple primary cancers
|
|
FL
|
follicular lymphoma
|
|
HPV
|
human papillomavirus
|
|
NCCN
|
National Comprehensive Cancer
Network
|
References
|
1
|
Parekh JD, Kukrety S, Thandra A and
Valenta C: Multiple primary malignant neoplasms in an elderly
patient. Cureus. 10:e23842018.PubMed/NCBI
|
|
2
|
Pan SY, Huang CP and Chen WC:
Synchronous/Metachronous multiple primary malignancies: Review of
associated risk factors. Diagnostics (Basel). 12:19402022.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ye X, Liu X, Yin N, Song W, Lu J, Yang Y
and Chen X: Successful first-line treatment of simultaneous
multiple primary malignancies of lung adenocarcinoma and renal
clear cell carcinoma: A case report. Front Immunol. 13:9565192022.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Motuzyuk I, Sydorchuk O, Kovtun N, Palian
Z and Kostiuchenko Y: Analysis of trends and factors in breast
multiple primary malignant neoplasms. Breast Cancer (Auckl).
12:11782234187599592018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wilson ML, Ayers S, Berney D, Eslan A,
Guarner J, Lester S, Masia R, Moloo Z, Mutuku A, Roberts D, et al:
Improving anatomic pathology in sub-saharan africa to support
cancer care. Am J Clin Pathol. 149:310–315. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chai W, Gong F, Zhang W, Wen Y and Cui L:
Multiple primary cancer in the female genital system: Two rare case
reports and a literature review. Medicine (Baltimore).
96:e88602017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bai J, Xie Z and Sun L: Case report:
Metachronous quadruple cancers including breast cancer and triple
genital cancer. Int J Gen Med. 13:1575–1580. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Borja NA, Silva-Smith R, Calfa C, Sussman
DA and Tekin M: Triple primary cancers: An analysis of genetic and
environmental factors. Cancer Prev Res (Phila). 17:209–215. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Huang P, Tan X, Chen C, Lv X and Li Y:
AF-SENet: Classification of cancer in cervical tissue pathological
images based on fusing deep convolution features. Sensors (Basel).
21:1222020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Solal-Celigny P, Roy P, Colombat P, White
J, Armitage JO, Arranz-Saez R, Au WY, Bellei M, Brice P, Caballero
D, et al: Follicular lymphoma international prognostic index.
Blood. 104:1258–1265. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Boughan KM and Caimi PF: Follicular
lymphoma: Diagnostic and prognostic considerations in initial
treatment approach. Curr Oncol Rep. 21:632019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Smith SM: Dissecting follicular lymphoma:
High versus low risk. Hematology Am Soc Hematol Educ Program.
2013:561–567. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Saleh M, Virarkar M, Javadi S, Elsherif
SB, de Castro Faria S and Bhosale P: Cervical cancer: 2018 revised
international federation of gynecology and obstetrics staging
system and the role of imaging. AJR Am J Roentgenol. 214:1182–1195.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zelenetz AD, Gordon LI, Abramson JS,
Advani RH, Andreadis B, Bartlett NL, Budde LE, Caimi PF, Chang JE,
Christian B, et al: NCCN Guidelines® Insights: B-Cell
Lymphomas, Version 6.2023. J Natl Compr Canc Netw. 21:1118–1131.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Abu-Rustum NR, Yashar CM, Bean S, Bradley
K, Campos SM, Chon HS, Chu C, Cohn D, Crispens MA, Damast S, et al:
NCCN guidelines insights: Cervical cancer, version 1.2020. J Natl
Compr Canc Netw. 18:660–666. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guo JQ, Zou JJ, Zhu JD, Jiang C and Shao
CX: A case report of rectal adenocarcinoma with intrahepatic
cholangiocarcinoma of the liver. J Int Med Res. 47:5883–5890. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Warren S and Gates O: Multiple primary
malignant tumors: A survey of the literature and a statistical
study. Am J Cancer. 16:1358–1414. 1932.
|
|
18
|
Yang YH, Deng Q, Yang TB, Gui Y, Zhang YX,
Liu JB, Deng Q, Liu WF and Sun JJ: A case report of
cholangiocarcinoma combined with moderately differentiated gastric
adenocarcinoma. Medicine (Baltimore). 98:e163322019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhou S, Lu Z, Wu H, Gu CY, Zhang DY, Sun
WL, Ma X and Liu HC: Synchronous multiple primary gallbladder and
gastric malignancies: Report of two cases and review of the
literature. Mol Clin Oncol. 7:869–873. 2017.PubMed/NCBI
|
|
20
|
Liu Y, Yang H, Fu X, Zhong L, Xu P, Fang
F, Liu Y, Li Q, Yan Y, Wei S, et al: BRCA2, PALB2, RECQL4 germline
pathogenic variants, and somatic TP53 mutation in triple
metachronous malignancies: A case report and literature review. Int
Med Case Rep J. 17:23–29. 2024.PubMed/NCBI
|
|
21
|
Hiyama T and Fujimoto I: Epidemiological
studies on multiple primary cancers-observations on the second
primary cancers among cervical cancer and laryngeal cancer cases.
Gan No Rinsho. 30:1499–1506. 1984.(In Japanese). PubMed/NCBI
|
|
22
|
Semczuk A, Colas E, Walczyna B, Joźwik M,
Pyra A, Semczuk-Sikora A and Rechberger T: Coexistence of
homologous-type cervical carcinosarcoma with endometrioid-type G1
endometrial cancer: A case report with an immunohistochemical
study. Int J Clin Exp Pathol. 7:7191–7195. 2014.PubMed/NCBI
|
|
23
|
Studzinski Z, Filipczak A and Branicka D:
Coexistence of ovarian adenocarcinoma with tubal pregnancy and
plano-epithelial cervical cancer of uterus. Ginekol Pol.
69:805–808. 1998.(In Polish). PubMed/NCBI
|
|
24
|
Lee YC, Lee YL and Li CY: BRCA genes and
related cancers: A Meta-analysis from epidemiological cohort
studies. Medicina (Kaunas). 57:9052021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wen W, Chen WS, Xiao N, Bender R,
Ghazalpour A, Tan Z, Swensen J, Millis SZ, Basu G, Gatalica Z and
Press MF: Mutations in the kinase domain of the HER2/ERBB2 gene
identified in a wide variety of human cancers. J Mol Diagn.
17:487–495. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kajitani N, Glahder J, Wu C, Yu H, Nilsson
K and Schwartz S: hnRNP L controls HPV16 RNA polyadenylation and
splicing in an Akt kinase-dependent manner. Nucleic Acids Res.
45:9654–9678. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cho EH, Park MS, Woo HY, Park H and Kwon
MJ: Evaluation of clinical usefulness of HPV-16 and HPV-18
genotyping for cervical cancer screening. J Gynecol Oncol.
35:e722024. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Walboomers JM, Jacobs MV, Manos MM, Bosch
FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ and Muñoz N:
Human papillomavirus is a necessary cause of invasive cervical
cancer worldwide. J Pathol. 189:12–19. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Murray PG and Young LS: An etiological
role for the Epstein-Barr virus in the pathogenesis of classical
Hodgkin lymphoma. Blood. 134:591–596. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Akagi K, Symer DE, Mahmoud M, Jiang B,
Goodwin S, Wangsa D, Li Z, Xiao W, Dunn JD, Ried T, et al:
Intratumoral heterogeneity and clonal evolution induced by HPV
integration. Cancer Discov. 13:910–927. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ren X, Cheng Y, Wu S, Zeng X, Shi X, Ling
Q, Li Z, Liang Z and Wang B: Primary non-Hodgkin lymphoma of the
tongue base: The clinicopathology of seven cases and evaluation of
HPV and EBV status. Diagn Pathol. 15:302020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yang JT, Liu CZ, Domer P and Iannaccone P:
Expression of lymphomagenic oncogenes in T-cell lymphomas of HPV 16
transgenic mice. Cancer Detect Prev. 22:405–415. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Toner K, McCann CD and Bollard CM:
Applications of cell therapy in the treatment of virus-associated
cancers. Nat Rev Clin Oncol. 21:709–724. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Grigsby PW, Massad LS, Mutch DG, Powell
MA, Thaker PH, McCourt C, Hagemann A, Fuh K, Kuroki L, Schwarz JK,
et al: FIGO 2018 staging criteria for cervical cancer: Impact on
stage migration and survival. Gynecol Oncol. 157:639–643. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kostov S, Kornovski Y, Slavchev S, Ivanova
Y, Dzhenkov D, Dimitrov N and Yordanov A: Pelvic Lymphadenectomy in
gynecologic Oncology-significance of anatomical variations.
Diagnostics (Basel). 11:892021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Saeteng S, Tantraworasin A, Euathrongchit
J, Lertprasertsuke N and Wannasopha Y: Nodal involvement pattern in
resectable lung cancer according to tumor location. Cancer Manag
Res. 4:151–158. 2012.PubMed/NCBI
|
|
37
|
Suzuki R, Nakata K, Okamura S, Kanemura T,
Yanai A, Kobayashi M, Yoshioka Y, Uji K, Yoshida A, Takeno A, et
al: Case report-a long-term surviving patient who received lymph
node dissection of skip metastasis from rectosigmoid cancer to
bilateral lateral lymph nodes. Gan To Kagaku Ryoho. 37:2598–2600.
2010.(In Japanese). PubMed/NCBI
|
|
38
|
Bertelsen CA, Kirkegaard-Klitbo A, Nielsen
M, Leotta SM, Daisuke F and Gogenur I: Pattern of colon cancer
lymph node metastases in patients undergoing central mesocolic
lymph node excision: A systematic review. Dis Colon Rectum.
59:1209–1221. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhao L, Wu F, Zhou T, Lu K, Jiang K, Zhang
Y and Luo D: Risk factors of skip lateral cervical lymph node
metastasis in papillary thyroid carcinoma: A systematic review and
Meta-analysis. Endocrine. 75:351–359. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Brunette LL, Bonyadlou S, Ji L, Groshen S,
Shuster D, Mehta A, Sposto R, Matsuo K, Lin YG and Roman LD:
Predictive value of FDG PET/CT to detect lymph node metastases in
cervical cancer. Clin Nucl Med. 43:793–801. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Khebbeb S, Rathat G, Serrand C, Bourdon A,
Ferrer C and Duraes M: Interest of para-aortic lymphadenectomy for
locally advanced cervical cancer in the era of PET scanning. Eur J
Obstet Gynecol Reprod Biol. 272:234–239. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Abu-Rustum NR, Yashar CM, Arend R, Barber
E, Bradley K, Brooks R, Campos SM, Chino J, Chon HS, Crispens MA,
et al: NCCN Guidelines® Insights: Cervical Cancer,
Version 1.2024. J Natl Compr Canc Netw. 21:1224–1233. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Sedlis A, Bundy BN, Rotman MZ, Lentz SS,
Muderspach LI and Zaino RJ: A randomized trial of pelvic radiation
therapy versus no further therapy in selected patients with stage
IB carcinoma of the cervix after radical hysterectomy and pelvic
lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol.
73:177–183. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Huang H, Feng YL, Wan T, Zhang YN, Cao XP,
Huang YW, Xiong Y, Huang X, Zheng M, Li YF, et al: Effectiveness of
sequential chemoradiation vs concurrent chemoradiation or radiation
alone in adjuvant treatment after hysterectomy for cervical cancer:
The STARS phase 3 randomized clinical trial. JAMA Oncol. 7:361–369.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Saleem T, Mi K, Pathak R, Yari K and Lu K:
Concurrent breast carcinoma and follicular lymphoma: A case series.
Am J Case Rep. 22:e9317722021. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Zhu Z, Zhou N, Yu S, Gao X, Cheng X, Wang
Y and Bai C: Successful treatment of concurrent follicular lymphoma
and Triple-negative breast cancer using rituximab plus
Nab-paclitaxel and cisplatin: A case report and literature review.
Onco Targets Ther. 16:905–911. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Marumo Y, Kusumoto S, Masaki A, Nakashima
T, Kikuchi T, Mori F, Komatsu H, Inagaki H, Iida S and Inagaki A:
Newly diagnosed follicular lymphoma during pembrolizumab treatment
for lung cancer. Int J Hematol. 114:280–285. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Hahm MH, Kim HJ, Shin KM, Cho SH, Park JY,
Jung JH, Jeong JY and Bae JH: Concurrent invasive ductal carcinoma
of the breast and malignant follicular lymphoma, initially
suspected to be metastatic breast cancer: A case report. J Breast
Cancer. 17:91–97. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Rosler W, Altenbuchinger M, Baeßler B,
Beissbarth T, Beutel G, Bock R, von Bubnoff N, Eckardt JN, Foersch
S, Loeffler CML, et al: An overview and a roadmap for artificial
intelligence in hematology and oncology. J Cancer Res Clin Oncol.
149:7997–8006. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Tanjak P, Suktitipat B, Vorasan N,
Juengwiwattanakitti P, Thiengtrong B, Songjang C, Therasakvichya S,
Laiteerapong S and Chinswangwatanakul V: Risks and cancer
associations of metachronous and synchronous multiple primary
cancers: A 25-year retrospective study. BMC Cancer. 21:10452021.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Liu S, Jia Y, Chai J, Ge H, Huang R, Li A
and Cheng H: A predictive model for the early death of breast
cancer with synchronous liver metastases: A Population-based study.
Cancer Control. 30:107327482312028512023. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Pilarski R, Patel DA, Weitzel J, McVeigh
T, Dorairaj JJ, Heneghan HM, Miller N, Weidhaas JB, Kerin MJ,
McKenna M, et al: The KRAS-variant is associated with risk of
developing double primary breast and ovarian cancer. PLoS One.
7:e378912012. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Cvelbar M, Hocevar M, Vidmar G and Teugels
E: BRCA1/2 status and clinicopathologic characteristics of patients
with double primary breast and ovarian cancer. Neoplasma.
58:198–204. 2011. View Article : Google Scholar : PubMed/NCBI
|