Introduction
Cisplatin (CDDP), an anticancer drug containing
platinum, is widely used in the treatment of solid tumors, such as
testicular, ovarian, cervical, bladder, head and neck, and
non-small cell lung cancers (NSCLC) (1). CDDP has been used as a key drug for
chemotherapy against NSCLC for more than 20 years. However, the
overall response rate to cisplatin used as a single agent is
reported to be no more than 20% in patients with NSCLC (2). Furthermore, development of resistance
to CDDP is common during treatment of NSCLC and is therefore a
significant factor to be considered by clinical oncologists.
Subsequently, exploration of a chemoresistance marker is crucial.
The mechanisms underlying the development of CDDP resistance
include decreased drug accumulation, enhanced detoxification and
increased DNA repair efficiency. However, previous studies have
been limited mainly to the in vitro or in vivo level.
Additionally, no study has shown factors that have been validated
as common contributors to clinical CDDP resistance and prognosis in
NSCLC patients (1).
Copper-transporting P-type adenosine triphosphatase
A (ATP7A) plays a significant role in copper distribution within
cells. ATP7A is expressed in the intestinal epithelium as well as
in most other tissues apart from the liver (3–7).
Binding of Cu to ATP7A triggers highly regulated subcellular
relocalization that involves movement from the basal position in
the trans-Golgi network to the plasma membrane (3,8).
Defective function of ATP7A causes Menkes disease, and the
pathology of Menkes disease reflects the inadequate mobilization of
Cu from a number of tissues. Previous studies suggested that the
copper export system also functions as an efflux transporter for
platinum drugs. These studies also showed an association between
ATP7A expression and resistance to platinum drugs in malignancies
(9–11). However, the ATP7A expression level
and its impact on CDDP resistance in NSCLC has yet to be adequately
elucidated.
The present study aimed to investigate the
predictive value of ATP7A gene expression for the in vitro
chemosensitivity of NSCLC to CDDP using surgically resected
specimens from patients with NSCLC.
Materials and methods
Study population
Eligible patients included those with a histologic
diagnosis of NSCLC, and who had undergone surgical resection but
had received no previous chemotherapy or radiotherapy. Patient
specimens were subjected to a chemosensitivity test between 2005
and 2007 at the Teikyo University Hospital and Tokai University
Hospital. Eligible patients who gave informed consent were
recruited for the study. The patients consisted of 16 males and 5
females, ranging in age from 54 to 79 years (mean 68). A total of 9
tumors were confirmed to be adenocarcinomas, 8 were squamous cell
carcinomas, 3 were large-cell carcinomas and 1 was confirmed to be
poorly differentiated NSCLC.
In vitro chemosensitivity test
In vitro chemosensitivity was examined using
the collagen gel-droplet embedded culture drug sensitivity test
(CD-DST) method, as described by Kobayashi et al (12,13)
and Kawamura et al (14),
with minor modifications. Briefly, surgically resected specimens
were finely minced using a scalpel and digested in cell dispersion
enzyme solution EZ (Nitta Gelatin Inc.). The dispersed cancer cells
were then washed and filtered through a nylon mesh with a pore size
of 200 mm, collected by centrifugation, suspended in PCM-1 medium
(Nitta Gelatin Inc.) and incubated in a CO2 incubator at
37°C for 24 h. Viable cells were collected and re-suspended in
reconstituted type I collagen solution with a final cell density of
1×105 cells/ml. Three drops of the collagen-cell mixture
(30 ml/drop) were placed in each well of a 6-well multiplate and
allowed to gel overnight at 37°C. Cisplatin (CDDP) (Bristol-Myers
Squibb Inc.) was then added at a final concentration of 2 mg/ml,
and the plates were incubated for 24 h. Following removal of the
medium containing the anticancer drugs, each well was rinsed twice,
overlaid with PCM-2 medium (Nitta Gelatin Inc.) and incubated for 7
days. At the end of the incubation period, the colonies were
stained with neutral red (50 mg/ml, 3 h). Each collagen droplet was
then fixed with 10% neutral formalin buffer, washed in water,
air-dried and quantified using imaging analysis. The in
vitro sensitivity was expressed as the growth inhibition rate
(GIR): (1 - T/C) × 100 (%), where T is the total volume of the
treated group and C is the total volume of the control group.
In this study, a tumor was judged as ‘resistant’
when the GIR was <61% and ‘sensitive’ when the GIR was ≥61%.
Cell line
The human colorectal cancer HCT8 cell line was
obtained from Riken (Saitama, Japan). The cell line was cultured at
37°C in Dulbecco's modified Eagle's medium (containing 10% bovine
serum) in a 5% CO2 atmosphere.
Quantitative evaluation of ATP7A mRNA
expression
Total RNA was extracted from the tumor samples and
the cell line using the acid guanidinium
thiocyanate-phenol-chloroform extraction method. Complementary DNA
(cDNA) was synthesized from 1 μg of total RNA as previously
described (15–17).
Real-time PCR assays were run on an ABI PRISM 7000
Sequence Detection system (Perkin-Elmer Applied Biosystems) in
accordance with the manufacturer's instructions and those of
previously published studies (15–17).
Briefly, a total volume of 50 μl of a reaction mixture containing 1
μl of the cDNA template, 25 μl of TaqMan Universal PCR Master Mix
(Perkin-Elmer Applied Biosystems) and 2.5 μl of a primer probe
mixture for ATP7A and β-actin was amplified using the following
protocol: after initial denaturation (2 min at 95°C), amplification
was performed for 50 cycles of 15 sec at 95°C and 60 sec at 60°C.
The primer probe mixture for ATP7A (TaqMan® Gene
Expression Assays, assay ID: Hs00163707_m1) and β-actin (human
ACTB, 4310881E) (both from Perkin-Elmer Applied Biosystems) were
purchased as part of the commercial provider's kit.
To precisely quantify the ATP7A gene transcripts,
β-actin transcripts were used as a quantitative control, and each
sample was normalized based on its β-actin transcript content.
Standard curves for ATP7A and β-actin mRNA were generated using
serially diluted solutions (1/5, 1/25, 1/125 and 1/625) of HCT8
cDNA. After determination of the threshold cycle (Ct) which was
defined as the PCR cycle number at which point the fluorescent
intensity exceeded the threshold, the target gene expression level
was calculated using the standard curve, and the quantitative
normalization of cDNA in each sample was performed using the
expression of the β-actin gene as an internal control. Finally, the
ATP7A mRNA levels were represented as a ratio to the β-actin mRNA
levels. Real-time PCR assays were conducted in duplicate on one
dish for each sample, and the mean value was used to calculate the
mRNA expression levels.
Statistical analysis
Categorical variables were analyzed using the
Fisher's exact test. Continuous variables were compared using the
Mann-Whitney U test. All reported P-values were two-sided.
P<0.05 was considered to be statistically significant.
Results
In vitro chemosensitivity test
The GIR values ranged from 0 to 68.6% (mean ±
standard deviation, 38.0±18.4%). According to the protocol
described in Materials and methods, 11 tumors were judged as
‘resistant (R)’ to CDDP, while the remaining 10 tumors were judged
as being ‘sensitive (S)’ to CDDP.
No significant correlation was observed between the
in vitro CDDP sensitivity and any of the clinical patient
characteristics, including age, gender and histology (Table I).
 | Table IRelationship between in vitro
CDDP sensitivity and patient characteristics. |
Table I
Relationship between in vitro
CDDP sensitivity and patient characteristics.
| In vitro CDDP
sensitivitya | |
|---|
|
| |
|---|
| Characteristics | R | S | P-valueb |
|---|
| Age (mean ± SD,
years) | 69±7 | 68±8 | 0.60 |
| Gender |
| Male | 7 | 9 | 0.30 |
| Female | 4 | 1 | |
| Histology |
| Adenocarcinoma | 7 | 2 | 0.08 |
|
Non-adenocarcinomac | 4 | 8 | |
ATP7A mRNA expression
The ATP7A mRNA expression levels varied from 0.12 to
1.55 (0.56±0.33). Table II shows
the relationship between the ATP7A expression levels and the
clinical patient characteristics, including age, gender and
histology. No significant correlation was observed between the
ATP7A mRNA expression level and age (p=0.90, Mann-Whitney U
test).
 | Table IIRelationship between the ATP7A mRNA
expression level and patient characteristics. |
Table II
Relationship between the ATP7A mRNA
expression level and patient characteristics.
| Characteristics | ATP7A gene expression
level (mean ± SD) | P-valuea |
|---|
| Age |
| >70 | 0.61±0.38 | 0.90 |
| ≤70 | 0.54±0.30 | |
| Gender |
| Male | 0.87±0.42 | 0.04 |
| Female | 0.46±0.25 | |
| Histology |
| Adenocarcinoma | 0.74±0.38 | 0.03 |
|
Non-adenocarcinomab | 0.42±0.22 | |
The ATP7A mRNA expression level in the male group
was significantly higher than that in the female group (p=0.04,
Mann-Whitney U test), and the ATP7A mRNA expression level in the
adenocarcinoma group was significantly higher than that in the
non-adenocarcinoma group (p=0.03, Mann-Whitney U test).
Relationship between ATP7A expression and
CDDP sensitivity
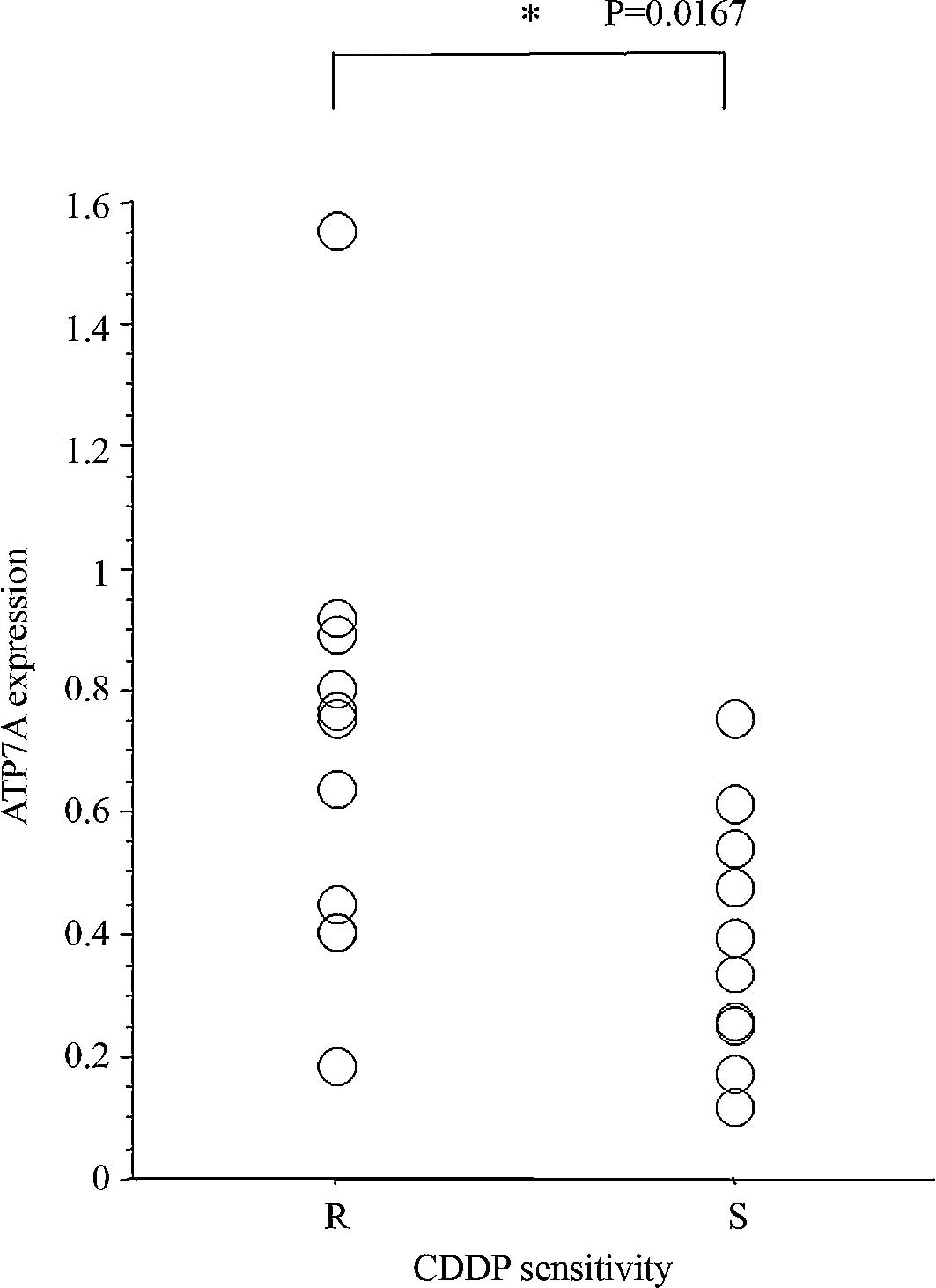
The difference in the ATP7A mRNA expression level
between the CDDP-resistant (R group, n=11) and CDDP-sensitive
tumors (S group, n=10) was evaluated. The ATP7A mRNA expression
levels in the R group were significantly higher than those in the S
group (p=0.017, Mann-Whitney U test; Fig. 1).
Discussion
ATP7A expression was reported to be associated with
the sensitivity of ovarian carcinoma cells to platinum drugs
(9,10). Overexpression of ATP7A in ovarian
carcinoma cells has been shown to be associated with higher levels
of platinum drug accumulation, Additionally, ATP7A-overexpressing
cells exhibit a significantly enhanced degree of resistance to
platinum drugs (10). Analysis of
the expression of ATP7A in ovarian carcinoma patients before and
after treatment with a platinum drug-containing regimen
demonstrated that in certain patients, treatment caused an
enrichment of ATP7A-expressing cells in the tumors, resulting in a
poor patient outcome (9). However,
the ATP7A expression levels and their clinical significance in
NSCLC have yet to be adequately elucidated.
The present study examined the association between
the ATP7A mRNA expression levels and in vitro
chemosensitivity to CDDP, using surgically resected specimens of
NSCLC. The results revealed significantly higher expression levels
of ATP7A mRNA in the CDDP-resistant tumors than in the
CDDP-sensitive tumors.
Little is known regarding the differences in the
ATP7A expression levels according to gender and histological
subtype in NSCLC patients. In this study, significant correlations
between the ATP7A expression levels and gender and histological
subtypes were observed. Further study is needed to confirm and
clarify the clinicopathological significance of this
observation.
In conclusion, although the data presented in this
study were based only on an in vitro assay, our results
suggest that the ATP7A gene expression level is correlated with
resistance to CDDP in NSCLC and that the ATP7A expression level may
be a useful marker of chemoresistance to cisplatin.
Abbreviations:
|
NSCLC
|
non-small cell lung cancer
|
|
CDDP
|
cisplatin
|
|
CD-DST
|
collagen gel-droplet embedded culture
drug sensitivity test
|
|
PCR
|
polymerase chain reaction
|
|
GIR
|
growth inhibition rate
|
References
|
1
|
Perez RP: Cellular and molecular
determinants of cisplatin resistance. Eur J Cancer. 34:1535–1542.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tiseo M, Franciosi V, Grossi F and
Ardizzoni A: Adjuvant chemotherapy for non-small cell lung cancer:
ready for clinical practice? Eur J Cancer. 42:8–16. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Terada K, Nakako T, Yang XL, et al:
Restoration of holoceruloplasmin synthesis in LEC rat after
infusion of recombinant adenovirus bearing WND cDNA. J Biol Chem.
273:1815–1820. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chelly J, Tumer Z, Tonnesen T, et al:
Isolation of a candidate gene for Menkes disease that encodes a
potential heavy metal binding protein. Nat Genet. 3:14–19. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mercer JF, Livingston J, Hall B, et al:
Isolation of a partial candidate gene for Menkes disease by
positional cloning. Nat Genet. 3:20–25. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vulpe C, Levinson B, Whitney S, Packman S
and Gitschier J: Isolation of a candidate gene for Menkes disease
and evidence that it encodes a copper-transporting ATPase. Nat
Genet. 3:7–13. 1993. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Safaei R, Holzer AK, Katano K, Samimi G
and Howell SB: The role of copper transporters in the development
of resistance to Pt drugs. J Inorg Biochem. 98:1607–1613. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Petris MJ, Strausak D and Mercer JF: The
Menkes copper transporter is required for the activation of
tyrosinase. Hum Mol Genet. 9:2845–2851. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Samimi G, Varki NM, Wilczynski S, Safaei
R, Alberts DS and Howell SB: Increase in expression of the copper
transporter ATP7A during platinum drug-based treatment is
associated with poor survival in ovarian cancer patients. Clin
Cancer Res. 9:5853–5859. 2003.PubMed/NCBI
|
|
10
|
Samimi G, Safaei R, Katano K, et al:
Increased expression of the copper efflux transporter ATP7A
mediates resistance to cisplatin, carboplatin, and oxaliplatin in
ovarian cancer cells. Clin Cancer Res. 10:4661–4669. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Safaei R, Katano K, Samimi G, et al:
Cross-resistance to cisplatin in cells with acquired resistance to
copper. Cancer Chemother Pharmacol. 53:239–246. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kobayashi H, Higashiyama M, Minamigawa K,
et al: Examination of in vitro chemosensitivity test using collagen
gel droplet culture method with colorimetric endpoint
quantification. Jpn J Cancer Res. 92:203–210. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kobayashi H: Development of a new in vitro
chemosensitivity test using collagen gel droplet embedded culture
and image analysis for clinical usefulness. Recent Results Cancer
Res. 161:48–61. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kawamura M, Gika M, Abiko T, et al:
Clinical evaluation of chemosensitivity testing for patients with
unresectable non-small cell lung cancer (NSCLC) using collagen gel
droplet embedded culture drug sensitivity test (CD-DST). Cancer
Chemother Pharmacol. 59:507–513. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nakagawa T, Inoue Y, Kodama H, et al:
Expression of copper-transporting P-type adenosine triphosphatase
(ATP7B) correlates with cisplatin resistance in human non-small
cell lung cancer xenografts. Oncol Rep. 20:265–270. 2008.PubMed/NCBI
|
|
16
|
Nishi M, Abe Y, Fujimori S, et al: The
modifier subunit of glutamate cysteine ligase relates to cisplatin
resistance in human small-cell lung cancer xenografts in
vivo. Oncol Rep. 14:421–424. 2005.PubMed/NCBI
|
|
17
|
Fujimori S, Abe Y, Nishi M, et al: The
subunits of glutamate cysteine ligase enhance cisplatin resistance
in human non-small cell lung cancer xenografts in vivo. Int
J Oncol. 25:413–418. 2004.PubMed/NCBI
|