|
1
|
Chen Q, Cao HZ and Zheng PS: LGR5 promotes
the proliferation and tumor formation of cervical cancer cells
through the Wnt/β-catenin signaling pathway. Oncotarget.
5:9092–9105. 2014.PubMed/NCBI
|
|
2
|
Dijkstra MG, Snijders PJ, Arbyn M,
Rijkaart DC, Berkhof J and Meijer CJ: Cervical cancer screening: On
the way to a shift from cytology to full molecular screening. Ann
Oncol. 25:927–935. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Armstrong EP: Prophylaxis of cervical
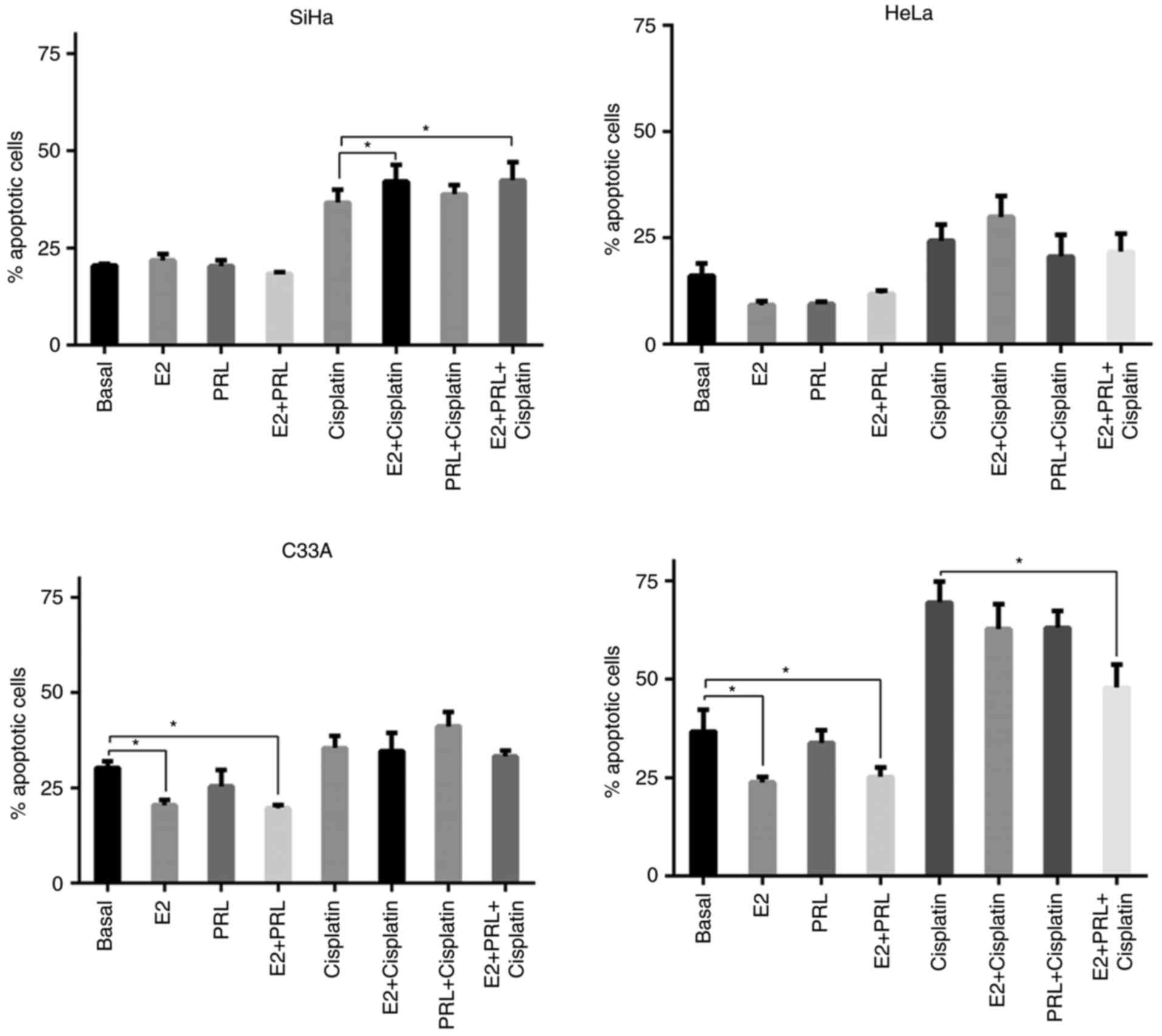
cancer and related cervical disease: A review of the
cost-effectiveness of vaccination against oncogenic HPV types. J
Manag Care Pharm. 16:217–230. 2010.PubMed/NCBI
|
|
4
|
Cunningham MS, Skrastins E, Fitzpatrick R,
Jindal P, Oneko O, Yeates K, Booth CM, Carpenter J and Aronson KJ:
Cervical cancer screening and HPV vaccine acceptability among rural
and urban women in Kilimanjaro Region, Tanzania. BMJ Open.
5:e0058282015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Son J, Park JW, Lambert PF and Chung SH:
Requirement of estrogen receptor alpha DNA-binding domain for HPV
oncogene-induced cervical carcinogenesis in mice. Carcinogenesis.
35:489–496. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chung SH, Franceschi S and Lambert PF:
Estrogen and ERalpha: Culprits in cervical cancer? Trends
Endocrinol Metab. 21:504–511. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chung SH, Shin MK, Korach KS and Lambert
PF: Requirement for stromal estrogen receptor alpha in cervical
neoplasia. Horm Cancer. 4:50–59. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kwasniewska A, Postawski K,
Gozdzicka-Jozefiak A, Kwasniewski W, Grywalska E, Zdunek M and
Korobowicz E: Estrogen and progesterone receptor expression in
HPV-positive and HPV-negative cervical carcinomas. Oncol Rep.
26:153–160. 2011.PubMed/NCBI
|
|
9
|
Ramachandran B: Functional association of
oestrogen receptors with HPV infection in cervical carcinogenesis.
Endocr Relat Cancer. 24:R99–R108. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Remoue F, Jacobs N, Miot V, Boniver J and
Delvenne P: High intraepithelial expression of estrogen and
progesterone receptors in the transformation zone of the uterine
cervix. Am J Obstet Gynecol. 189:1660–1665. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Marks M, Gravitt PE, Gupta SB, Liaw KL,
Kim E, Tadesse A, Phongnarisorn C, Wootipoom V, Yuenyao P,
Vipupinyo C, et al: The association of hormonal contraceptive use
and HPV prevalence. Int J Cancer. 128:2962–2970. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Marks MA, Gupta S, Liaw KL, Tadesse A, Kim
E, Phongnarisorn C, Wootipoom V, Yuenyao P, Vipupinyo C, Rugpao S,
et al: Prevalence and correlates of HPV among women attending
family-planning clinics in Thailand. BMC Infect Dis. 15:1592015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Roura E, Travier N, Waterboer T, de
Sanjosé S, Bosch FX, Pawlita M, Pala V, Weiderpass E, Margall N,
Dillner J, et al: The influence of hormonal factors on the risk of
developing cervical cancer and pre-cancer: Results from the EPIC
cohort. PLoS One. 11:e01470292016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gupte AA, Pownall HJ and Hamilton DJ:
Estrogen: An emerging regulator of insulin action and mitochondrial
function. J Diabetes Res. 2015:9165852015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bronowicka-Kłys DE, Lianeri M and
Jagodziński PP: The role and impact of estrogens and xenoestrogen
on the development of cervical cancer. Biomed Pharmacother.
84:1945–1953. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yamaguchi H and Sakai R: Direct
interaction between carcinoma cells and cancer associated
fibroblasts for the regulation of cancer invasion. Cancers.
7:2054–2062. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
den Boon JA, Pyeon D, Wang SS, Horswill M,
Schiffman M, Sherman M, Zuna RE, Wang Z, Hewitt SM, Pearson R, et
al: Molecular transitions from papillomavirus infection to cervical
precancer and cancer: Role of stromal estrogen receptor signaling.
Proc Natl Acad Sci USA. 112:E3255–E3264. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lopez-Pulido EI, Muñoz-Valle JF, Del
Toro-Arreola S, Jave-Suárez LF, Bueno-Topete MR, Estrada-Chávez C
and Pereira-Suárez AL: High expression of prolactin receptor is
associated with cell survival in cervical cancer cells. Cancer Cell
Int. 13:1032013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ascencio-Cedillo R, López-Pulido EI,
Muñoz-Valle JF, Villegas-Sepúlveda N, Del Toro-Arreola S,
Estrada-Chávez C, Daneri-Navarro A, Franco-Topete R, Pérez-Montiel
D, García-Carrancá A, et al: Prolactin and prolactin receptor
expression in cervical intraepithelial neoplasia and cancer. Pathol
Oncol Res. 21:241–246. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
de Arellano Ramirez A, Lopez-Pulido EI,
Martinez-Neri PA, Chávez Estrada C, González Lucano R,
Fafutis-Morris M, Aguilar-Lemarroy A, Muñoz-Valle JF and
Pereira-Suárez AL: STAT3 activation is required for the
antiapoptotic effects of prolactin in cervical cancer cells. Cancer
Cell Int. 15:832015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Trott JF, Horigan KC, Gloviczki JM, Costa
KM, Freking BA, Farmer C, Hayashi K, Spencer T, Morabito JE and
Hovey RC: Tissue-specific regulation of porcine prolactin receptor
expression by estrogen, progesterone, and prolactin. J Endocrinol.
202:153–166. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Larrea F, Martinez-Castillo A, Cabrera V,
Alcocer-Varela J, Queipo G, Cariño C and Alarcón-Segovia D: A
bioactive 60-kilodalton prolactin species is preferentially
secreted in cultures of mitogen-stimulated and nonstimulated
peripheral blood mononuclear cells from subjects with systemic
lupus erythematosus. J Clin Endocrinol Metab. 82:3664–3669. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gout PW, Beer CT and Noble RL:
Prolactin-stimulated growth of cell cultures established from
malignant Nb rat lymphomas. Cancer Res. 40:2433–2436.
1980.PubMed/NCBI
|
|
24
|
Noble RL, Beer CT and Gout PW: Evidence in
vivo and in vitro of a role for the pituitary in the growth of
malignant lymphomas in Nb rats. Cancer Res. 40:2437–2440.
1980.PubMed/NCBI
|
|
25
|
De Arellano Ramirez A, Leal Riera A,
Lopez-Pulido EI, González-Lucano LR, Macías Barragan J, Del Toro
Arreola S, García-Chagollan M, Palafox-Sánchez CA, Muñoz-Valle JF
and Pereira-Suárez AL: A 60 kDa prolactin variant secreted by
cervical cancer cells modulates apoptosis and cytokine production.
Oncol Rep. 39:1253–1260. 2018.PubMed/NCBI
|
|
26
|
Giacomini D, Páez-Pereda M, Stalla J,
Stalla GK and Arzt E: Molecular interaction of BMP-4, TGF-beta, and
estrogens in lactotrophs: Impact on the PRL promoter. Mol
Endocrinol. 23:1102–1114. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Duan R, Ginsburg E and Vonderhaar BK:
Estrogen stimulates transcription from the human prolactin distal
promoter through AP1 and estrogen responsive elements in T47D human
breast cancer cells. Mol Cell Endocrinol. 281:9–18. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gutzman JH, Miller KK and Schuler LA:
Endogenous human prolactin and not exogenous human prolactin
induces estrogen receptor alpha and prolactin receptor expression
and increases estrogen responsiveness in breast cancer cells. J
Steroid Biochem Mol Biol. 88:69–77. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Aslani Sari F, Safaei A, Pourjabali M and
Momtahan M: Evaluation of Ki67, p16 and CK17 markers in
differentiating cervical intraepithelial neoplasia and benign
lesions. Iran J Med Sci. 38:15–21. 2013.PubMed/NCBI
|
|
30
|
Kamaraddi S, Nayak A, Honnappa S and
Swarup A: Expression of Bcl-2 marker in premalignant lesions of
cervical cancer. Int J Reprod Contracept Obstet Gynecol. 5:965–969.
2016. View Article : Google Scholar
|
|
31
|
Ter Harmsel B, Smedts F, Kuijpers J,
Jeunink M, Trimbos B and Ramaekers F: BCL-2 immunoreactivity
increases with severity of CIN: A study of normal cervical
epithelia, CIN, and cervical carcinoma. J Pathol. 179:26–30. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sánchez NS and Königsberg M: Using yeast
to easily determine mitochondrial functionality with
1-(4,5-dimethylthiazol-2-yl)-3,5-diphenyltetrazolium bromide (MTT)
assay. Biochem Mol Biol Educ. 34:209–212. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Flores-Miramontes MG, Torres-Reyes LA,
Alvarado-Ruiz L, Romero-Martínez SA, Ramírez-Rodríguez V,
Balderas-Peña LM, Vallejo-Ruíz V, Piña-Sánchez P, Cortés-Gutiérrez
EI, Jave-Suárez LF, et al: Human papillomavirus genotyping by
linear array and next-generation sequencing in cervical samples
from Western Mexico. Virol J. 12:1612015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2−ΔΔCT method. Methods. 25:402–408. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chong T, Chan WK and Bernard HU:
Transcriptional activation of human papillomavirus 16 by nuclear
factor I, AP1, steroid receptors and a possibly novel transcription
factor, PVF: A model for the composition of genital papillomavirus
enhancers. Nucleic Acids Res. 18:465–470. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Mitrani-Rosenbaum S, Tsvieli R and
Tur-Kaspa R: Oestrogen stimulates differential transcription of
human papillomavirus type 16 in SiHa cervical carcinoma cells. J
Gen Virol. 70:2227–2232. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Elson DA, Riley RR, Lacey A, Thordarson G,
Talamantes FJ and Arbeit JM: Sensitivity of the cervical
transformation zone to estrogen-induced squamous carcinogenesis.
Cancer Res. 60:1267–1275. 2000.PubMed/NCBI
|
|
38
|
Chung SH, Wiedmeyer K, Shai A, Korach KS
and Lambert PF: Requirement for estrogen receptor alpha in a mouse
model for human papillomavirus-associated cervical cancer. Cancer
Res. 68:9928–9934. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Chung SH and Lambert PF: Prevention and
treatment of cervical cancer in mice using estrogen receptor
antagonists. Proc Natl Acad Sci USA. 106:19467–19472. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Fan DM, Tian XY, Wang RF and Yu JJ: The
prognosis significance of TGF-β1 and ER protein in cervical
adenocarcinoma patients with stage Ib~IIa. Tumour Biol.
35:11237–11242. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
López-Romero R, Garrido-Guerrero E,
Rangel-López A, Manuel-Apolinar L, Piña-Sánchez P, Lazos-Ochoa M,
Mantilla-Morales A, Bandala C and Salcedo M: The cervical malignant
cells display a down regulation of ER-α but retain the ER-β
expression. Int J Clin Exp Pathol. 6:1594–1602. 2013.PubMed/NCBI
|
|
42
|
Clevenger CV, Gadd SL and Zheng J: New
mechanisms for PRLr action in breast cancer. Trends Endocrinol
Metab. 20:223–229. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lim JH, Kim TY, Kim WH and Park JW: CAML
promotes prolactin-dependent proliferation of breast cancer cells
by facilitating prolactin receptor signaling pathways. Breast
Cancer Res Treat. 130:19–27. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Perrot-Applanat M, Gualillo O, Buteau H,
Edery M and Kelly PA: Internalization of prolactin receptor and
prolactin in transfected cells does not involve nuclear
translocation. J Cell Sci. 110:1123–1132. 1997.PubMed/NCBI
|
|
45
|
Kanthiya K, Khunnarong J, Tangjitgamol S,
Puripat N and Tanvanich S: Expression of the p16 and Ki67 in
cervical squamous intraepithelial lesions and cancer. Asian Pac J
Cancer Prev. 17:3201–3206. 2016.PubMed/NCBI
|
|
46
|
Kisser A and Zechmeister-Koss I: A
systematic review of p16/Ki-67 immuno-testing for triage of low
grade cervical cytology. BJOG. 122:64–70. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Aletra C, Ravazoula P, Scopa C, Kounelis
S, Sotiropoulou G, Kourounis G, Ladopoulos I and Bonikos D:
Expression of bcl-2 and bax in cervical intraepithelial neoplasia
and invasive squamous cell carcinoma of the uterine cervix. Eur J
Gynaecol Oncol. 21:494–498. 2000.PubMed/NCBI
|
|
48
|
Shukla S, Dass J and Pujani M: p53 and
bcl2 expression in malignant and premalignant lesions of uterine
cervix and their correlation with human papilloma virus 16 and 18.
South Asian J Cancer. 3:48–53. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Nair HB, Luthra R, Kirma N, Liu YG,
Flowers L, Evans D and Tekmal RR: Induction of aromatase expression
in cervical carcinomas: Effects of endogenous estrogen on cervical
cancer cell proliferation. Cancer Res. 65:11164–11173. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Llovera M, Pichard C, Bernichtein S, Jeay
S, Touraine P, Kelly PA and Goffin V: Human prolactin (hPRL)
antagonists inhibit hPRL-activated signaling pathways involved in
breast cancer cell proliferation. Oncogene. 19:4695–4705. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Doll F, Pfeilschifter J and Huwiler A:
Prolactin upregulates sphingosine kinase-1 expression and activity
in the human breast cancer cell line MCF7 and triggers enhanced
proliferation and migration. Endocr Relat Cancer. 14:325–335. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Chen KE, Bustamante K, Nguyen V and Walker
AM: Involvement of miR-106b in tumorigenic actions of both
prolactin and estradiol. Oncotarget. 8:36368–36382. 2017.PubMed/NCBI
|
|
53
|
DeBerardinis RJ, Lum JJ, Hatzivassiliou G
and Thompson CB: The biology of cancer: Metabolic reprogramming
fuels cell growth and proliferation. Cell Metab. 7:11–20. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Klinge CM: Estrogenic control of
mitochondrial function and biogenesis. J Cell Biochem.
105:1342–1351. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Ivanova MM, Radde BN, Son J, Mehta FF,
Chung SH and Klinge CM: Estradiol and tamoxifen regulate NRF-1 and
mitochondrial function in mouse mammary gland and uterus. J Mol
Endocrinol. 51:233–246. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Klinge CM: Estrogens regulate life and
death in mitochondria. J Bioenerg Biomembr. 49:307–324. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Fontecha N, Basaras M, Hernáez S, Andia D
and Cisterna R: Assessment of human papillomavirus E6/E7 oncogene
expression as cervical disease biomarker. BMC Cancer. 16:8522016.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
de Villiers EM: Relationship between
steroid hormone contraceptives and HPV, cervical intraepithelial
neoplasia and cervical carcinoma. Int J Cancer. 103:705–708. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Matos A, Castelão C, da Silva Pereira A,
Alho I, Bicho M, Medeiros R and Bicho MC: Epistatic interaction of
CYP1A1 and COMT polymorphisms in cervical cancer. Oxid Med Cell
Longev. 2016:27698042016. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Zeng Q, Chen J, Li Y, Werle KD, Zhao RX,
Quan CS, Wang YS, Zhai YX, Wang JW and Youssef M: LKB1 inhibits
HPV-associated cancer progression by targeting cellular metabolism.
Oncogene. 36:1245–1255. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Zeng Q, Zhao RX, Chen J, Li Y, Li XD, Liu
XL, Zhang WM, Quan CS, Wang YS, Zhai YX, et al: O-linked
GlcNAcylation elevated by HPV E6 mediates viral oncogenesis. Proc
Natl Acad Sci USA. 113:9333–9338. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Erickson JR, Pereira L, Wang L, Han G,
Ferguson A, Dao K, Copeland RJ, Despa F, Hart GW, Ripplinger CM, et
al: Diabetic hyperglycaemia activates CaMKII and arrhythmias by
O-linked glycosylation. Nature. 502:372–376. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Bodily JM, Mehta KP and Laimins LA: Human
papillomavirus E7 enhances hypoxia-inducible factor 1-mediated
transcription by inhibiting binding of histone deacetylases. Cancer
Res. 71:1187–1195. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Hoppe-Seyler K, Bossler F, Braun JA,
Herrmann AL and Hoppe-Seyler F: The HPV E6/E7 oncogenes: Key
factors for viral carcinogenesis and therapeutic targets. Trends
Microbiol. 26:158–168. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Costello LC and Franklin RB: Testosterone
and prolactin regulation of metabolic genes and citrate metabolism
of prostate epithelial cells. Horm Metab Res. 34:417–424. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Franklin RB, Zou J, Ma J and Costello LC:
Protein kinase C alpha, epsilon and AP-1 mediate prolactin
regulation of mitochondrial aspartate aminotransferase expression
in the rat lateral prostate. Mol Cell Endocrinol. 170:153–161.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
McMurray RW: Estrogen, prolactin, and
autoimmunity: Actions and interactions. Int Immunopharmacol.
1:995–1008. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Telleria CM, Zhong L, Deb S, Srivastava
RK, Park KS, Sugino N, Park-Sarge OK and Gibori G: Differential
expression of the estrogen receptors alpha and beta in the rat
corpus luteum of pregnancy: Regulation by prolactin and placental
lactogens. Endocrinology. 139:2432–2442. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Frasor J and Gibori G: Prolactin
regulation of estrogen receptor expression. Trends Endocrinol
Metab. 14:118–123. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Helguero LA, Faulds MH, Gustafsson JA and
Haldosén LA: Estrogen receptors alfa (ERalpha) and beta (ERbeta)
differentially regulate proliferation and apoptosis of the normal
murine mammary epithelial cell line HC11. Oncogene. 24:6605–6616.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Shappell NW: Ergovaline toxicity on Caco-2
cells as assessed by MTT, alamarBlue, and DNA assays. In Vitro Cell
Dev Biol Anim. 39:329–335. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Quent VM, Loessner D, Friis T, Reichert JC
and Hutmacher DW: Discrepancies between metabolic activity and DNA
content as tool to assess cell proliferation in cancer research. J
Cell Mol Med. 14:1003–1013. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Wang P, Henning SM and Heber D:
Limitations of MTT and MTS-based assays for measurement of
antiproliferative activity of green tea polyphenols. PLoS One.
5:e102022010. View Article : Google Scholar : PubMed/NCBI
|