|
1
|
Lavaissiere L, Jia S, Nishiyama M, De La
Monte S, Stern AM, Wands JR and Friedman PA: Overexpression of
human aspartyl(asparaginyl)beta-hydroxylase in hepatocellular
carcinoma and cholangiocarcinoma. J Clin Invest. 98:1313–1323.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Korioth F, Gieffers C and Frey J: Cloning
and characterization of the human gene encoding aspartyl
beta-hydroxylase. Gene. 150:395–399. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dinchuk JE, Henderson NL, Burn TC, Huber
R, Ho SP, Link J, O'Neil KT, Focht RJ, Scully MS, Hollis JM, et al:
Aspartyl beta-hydroxylase (Asph) and an evolutionarily conserved
isoform of Asph missing the catalytic domain share exons with
junctin. J Biol Chem. 275:39543–39554. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang Q, VanDusen WJ, Petroski CJ, Garsky
VM, Stern AM and Friedman PA: Bovine liver aspartyl
beta-hydroxylase: Purification and characterization. J Biol Chem.
266:14004–14010. 1991.PubMed/NCBI
|
|
5
|
McGinnis K, Ku GM, VanDusen WJ, Fu J,
Garsky V, Stern AM and Friedman PA: Site-directed mutagenesis of
residues in a conserved region of bovine aspartyl (asparaginyl)
beta-hydroxylase: Evidence that histidine 675 has a role in binding
Fe2+. Biochemistry. 35:3957–3962. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stenflo J, Holme E, Lindstedt S,
Chandramouli N, Huang LH, Tam JP and Merrifield RB: Hydroxylation
of aspartic acid in domains homologous to the epidermal growth
factor precursor is catalyzed by a 2-oxoglutarate-dependent
dioxygenase. Proc Natl Acad Sci USA. 86:444–447. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pfeffer I, Brewitz L, Krojer T, Jensen SA,
Kochan GT, Kershaw NJ, Hewitson KS, McNeill LA, Kramer H, Münzel M,
et al: Aspartate/asparagine-β-hydroxylase crystal structures reveal
an unexpected epidermal growth factor-like domain substrate
disulfide pattern. Nat Commun. 10:49102019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gronke RS, VanDusen WJ, Garsky VM, Jacobs
JW, Sardana MK, Stern AM and Friedman PA: Aspartyl
beta-hydroxylase: In vitro hydroxylation of a synthetic peptide
based on the structure of the first growth factor-like domain of
human factor IX. Proc Natl Acad Sci USA. 86:3609–3613. 1989.
View Article : Google Scholar : PubMed/NCBI
|
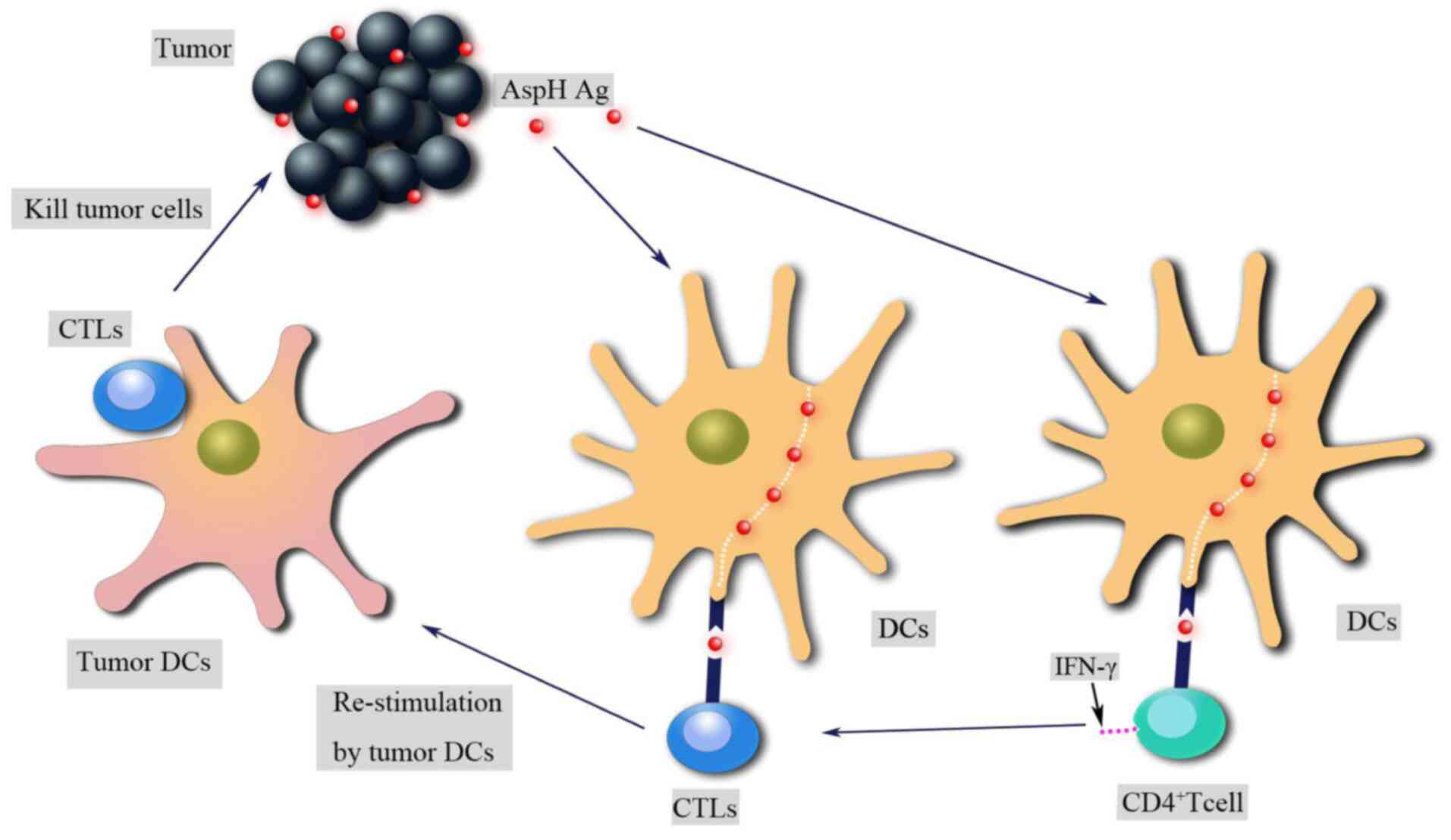
|
9
|
Jia S, VanDusen WJ, Diehl RE, Kohl NE,
Dixon RA, Elliston KO, Stern AM and Friedman PA: cDNA cloning and
expression of bovine aspartyl (asparaginyl) beta-hydroxylase. J
Biol Chem. 267:14322–14327. 1992.PubMed/NCBI
|
|
10
|
Treves S, Feriotto G, Moccagatta L,
Gambari R and Zorzato F: Molecular cloning, expression, functional
characterization, chromosomal localization, and gene structure of
junctate, a novel integral calcium binding protein of
sarco(endo)plasmic reticulum membrane. J Biol Chem.
275:39555–39568. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bruix J and Llovet JM: Prognostic
prediction and treatment strategy in hepatocellular carcinoma.
Hepatology. 35:519–524. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hong CS, Kwon SJ and Kim DH: Multiple
functions of junctin and junctate, two distinct isoforms of
aspartyl beta-hydroxylase. Biochem Biophys Res Commun. 362:1–4.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jones LR, Zhang L, Sanborn K, Jorgensen AO
and Kelley J: Purification, primary structure, and immunological
characterization of the 26-kDa calsequestrin binding protein
(junctin) from cardiac junctional sarcoplasmic reticulum. J Biol
Chem. 270:30787–30796. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Siggs OM, Souzeau E and Craig JE: Loss of
ciliary zonule protein hydroxylation and lens stability as a
predicted consequence of biallelic ASPH variation. Ophthalmic
Genet. 40:12–16. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Abarca Barriga HH, Caballero N, Trubnykova
M, Castro-Mujica MDC, La Serna-Infantes JE, Vásquez F and Hennekam
RC: A novel ASPH variant extends the phenotype of Shawaf-Traboulsi
syndrome. Am J Med Genet Part A. 176:2494–2500. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kulkarni N, Lloyd IC, Ashworth J, Biswas
S, Black GCM and Clayton-Smith J; NIHR BioResource Consortium, :
Traboulsi syndrome due to ASPH mutation: An under-recognised cause
of ectopia lentis. Clin Dysmorphol. 28:184–189. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Patel N, Khan AO, Mansour A, Mohamed JY,
Al-Assiri A, Haddad R, Jia X, Xiong Y, Mégarbané A, Traboulsi EI
and Alkuraya FS: Mutations in ASPH cause facial dysmorphism, lens
dislocation, anterior-segment abnormalities, and spontaneous
filtering blebs, or Traboulsi syndrome. Am J Hum Genet. 94:755–759.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dinchuk JE, Focht RJ, Kelley JA, Henderson
NL, Zolotarjova NI, Wynn R, Neff NT, Link J, Huber RM, Burn TC, et
al: Absence of post-translational aspartyl beta-hydroxylation of
epidermal growth factor domains in mice leads to developmental
defects and an increased incidence of intestinal neoplasia. J Biol
Chem. 277:12970–12977. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gundogan F, Elwood G, Greco D, Rubin LP,
Pinar H, Carlson RI, Wands JR and de la Monte SM: Role of
aspartyl-(asparaginyl) beta-hydroxylase in placental implantation:
Relevance to early pregnancy loss. Hum Pathol. 38:50–59. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yang H, Song K, Xue T, Xue XP, Huyan T,
Wang W and Wang H: The distribution and expression profiles of
human aspartyl/asparaginyl beta-hydroxylase in tumor cell lines and
human tissues. Oncol Rep. 24:1257–1264. 2010.PubMed/NCBI
|
|
21
|
Ince N, de La Monte SM and Wands JR:
Overexpression of human aspartyl (asparaginyl) beta-hydroxylase is
associated with malignant transformation. Cancer Res. 60:1261–1266.
2000.PubMed/NCBI
|
|
22
|
Zou Q, Hou Y, Wang H, Wang K, Xing X, Xia
Y, Wan X, Li J, Jiao B, Liu J, et al: Hydroxylase activity of ASPH
promotes hepatocellular carcinoma metastasis through
epithelial-to-mesenchymal transition pathway. EBioMedicine.
31:287–298. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Aihara A, Huang CK, Olsen MJ, Lin Q, Chung
W, Tang Q, Dong X and Wands JR: A cell-surface β-hydroxylase is a
biomarker and therapeutic target for hepatocellular carcinoma.
Hepatology. 60:1302–1313. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Artavanis-Tsakonas S, Rand MD and Lake RJ:
Notch signaling: Cell fate control and signal integration in
development. Science. 284:770–776. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Avila JL and Kissil JL: Notch signaling in
pancreatic cancer: Oncogene or tumor suppressor? Trends Mol Med.
19:320–327. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang H, Zang C, Liu XS and Aster JC: The
role of notch receptors in transcriptional regulation. J Cell
Physiol. 230:982–988. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wharton KA, Johansen KM, Xu T and
Artavanis-Tsakonas S: Nucleotide sequence from the neurogenic locus
Notch implies a gene product that shares homology with proteins
containing EGF-like repeats. Cell. 43:567–581. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Penton AL, Leonard LD and Spinner NB:
Notch signaling in human development and disease. Semin Cell Dev
Biol. 23:450–457. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dong X, Lin Q, Aihara A, Li Y, Huang CK,
Chung W, Tang Q, Chen X, Carlson R, Nadolny C, et al: Aspartate
β-hydroxylase expression promotes a malignant pancreatic cellular
phenotype. Oncotarget. 6:1231–1248. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Cantarini MC, de La Monte SM, Pang M, Tong
M, D'Errico A, Trevisani F and Wands JR: Aspartyl-asparagyl beta
hydroxylase over-expression in human hepatoma is linked to
activation of insulin-like growth factor and Notch signaling
mechanisms. Hepatology. 44:446–457. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chung W, Kim M, de la Monte S, Longato L,
Carlson R, Slagle BL, Dong X and Wands JR: Activation of signal
transduction pathways during hepatic oncogenesis. Cancer Lett.
370:1–9. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lin Q, Chen X, Meng F, Ogawa K, Li M, Song
R, Zhang S, Zhang Z, Kong X, Xu Q, et al: ASPH-notch axis guided
exosomal delivery of prometastatic secretome renders breast cancer
multi-organ metastasis. Mol Cancer. 18:1562019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Boelens MC, Wu TJ, Nabet BY, Xu B, Qiu Y,
Yoon T, Azzam DJ, Twyman-Saint Victor C, Wiemann BZ, Ishwaran H, et
al: Exosome transfer from stromal to breast cancer cells regulates
therapy resistance pathways. Cell. 159:499–513. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Luga V, Zhang L, Viloria-Petit AM,
Ogunjimi AA, Inanlou MR, Chiu E, Buchanan M, Hosein AN, Basik M and
Wrana JL: Exosomes mediate stromal mobilization of autocrine
Wnt-PCP signaling in breast cancer cell migration. Cell.
151:1542–1556. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Vaupel P, Mayer A and Höckel M: Tumor
hypoxia and malignant progression. Methods Enzymol. 381:335–354.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chen J, Imanaka N, Chen J and Griffin JD:
Hypoxia potentiates Notch signaling in breast cancer leading to
decreased E-cadherin expression and increased cell migration and
invasion. Br J Cancer. 102:351–360. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lawton M, Tong M, Gundogan F, Wands JR and
de La Monte SM: Aspartyl-(asparaginyl) beta-hydroxylase,
hypoxia-inducible factor-alpha and Notch cross-talk in regulating
neuronal motility. Oxid Med Cell Longev. 3:347–356. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sivasankaran B, Degen M, Ghaffari A, Hegi
ME, Hamou MF, Ionescu MC, Zweifel C, Tolnay M, Wasner M,
Mergenthaler S, et al: Tenascin-C is a novel RBPJkappa-induced
target gene for Notch signaling in gliomas. Cancer Res. 69:458–465.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wagner EF and Nebreda ÁR: Signal
integration by JNK and p38 MAPK pathways in cancer development. Nat
Rev Cancer. 9:537–549. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Thorpe LM, Yuzugullu H and Zhao JJ: PI3K
in cancer: Divergent roles of isoforms, modes of activation and
therapeutic targeting. Nat Rev Cancer. 15:7–24. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Engelman JA, Luo J and Cantley LC: The
evolution of phosphatidylinositol 3-kinases as regulators of growth
and metabolism. Nat Rev Genet. 7:606–619. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Giorgetti S, Ballotti R, Kowalski-Chauvel
A, Tartare S and Van Obberghen E: The insulin and insulin-like
growth factor-I receptor substrate IRS-1 associates with and
activates phosphatidylinositol 3-kinase in vitro. J Biol Chem.
268:7358–7364. 1993.PubMed/NCBI
|
|
43
|
Hermanto U, Zong CS and Wang LH:
Inhibition of mitogen-activated protein kinase kinase selectively
inhibits cell proliferation in human breast cancer cells displaying
enhanced insulin-like growth factor I-mediated mitogen-activated
protein kinase activation. Cell Growth Differ. 11:655–664.
2000.PubMed/NCBI
|
|
44
|
Vuori K and Ruoslahti E: Association of
insulin receptor substrate-1 with integrins. Science.
266:1576–1578. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
de la Monte SM, Tamaki S, Cantarini MC,
Ince N, Wiedmann M, Carter JJ, Lahousse SA, Califano S, Maeda T,
Ueno T, et al: Aspartyl-(asparaginyl)-beta-hydroxylase regulates
hepatocellular carcinoma invasiveness. J Hepatol. 44:971–983. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ngeow KC, Friedrichsen HJ, Li L, Zeng Z,
Andrews S, Volpon L, Brunsdon H, Berridge G, Picaud S, Fischer R,
et al: BRAF/MAPK and GSK3 signaling converges to control MITF
nuclear export. Proc Natl Acad Sci USA. 115:E8668–E8677. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Iwagami Y, Huang CK, Olsen MJ, Thomas JM,
Jang G, Kim M, Lin Q, Carlson RI, Wagner CE, Dong X and Wands JR:
Aspartate β-hydroxylase modulates cellular senescence through
glycogen synthase kinase 3β in hepatocellular carcinoma.
Hepatology. 63:1213–1226. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Sharma P and Allison JP: The future of
immune checkpoint therapy. Science. 348:56–61. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chen DS and Mellman I: Elements of cancer
immunity and the cancer-immune set point. Nature. 541:321–330.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Mu CY, Huang JA, Chen Y, Chen C and Zhang
XG: High expression of PD-L1 in lung cancer may contribute to poor
prognosis and tumor cells immune escape through suppressing tumor
infiltrating dendritic cells maturation. Med Oncol. 28:682–688.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Borst J, Ahrends T, Bąbała N, Melief CJM
and Kastenmüller W: CD4+ T cell help in cancer immunology and
immunotherapy. Nat Rev Immunol. 18:635–647. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Tomimaru Y, Mishra S, Safran H,
Charpentier KP, Martin W, De Groot AS, Gregory SH and Wands JR:
Aspartate-β-hydroxylase induces epitope-specific T cell responses
in hepatocellular carcinoma. Vaccine. 33:1256–1266. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Iwagami Y, Casulli S, Nagaoka K, Kim M,
Carlson RI, Ogawa K, Lebowitz MS, Fuller S, Biswas B, Stewart S, et
al: Lambda phage-based vaccine induces antitumor immunity in
hepatocellular carcinoma. Heliyon. 3:e004072017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Petrick JL and McGlynn KA: The changing
epidemiology of primary liver cancer. Curr Epidemiol Reports.
6:104–111. 2019. View Article : Google Scholar
|
|
55
|
Ryerson AB, Eheman CR, Altekruse SF, Ward
JW, Jemal A, Sherman RL, Henley SJ, Holtzman D, Lake A, Noone AM,
et al: Annual report to the nation on the status of cancer,
1975–2012, featuring the increasing incidence of liver cancer.
Cancer. 122:1312–1337. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Tomimaru Y, Koga H, Yano H, de la Monte S,
Wands JR and Kim M: Upregulation of T-cell factor-4
isoform-responsive target genes in hepatocellular carcinoma. Liver
Int. 33:1100–1112.. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wang K, Liu J, Yan ZL, Li J, Shi LH, Cong
WM, Xia Y, Zou QF, Xi T, Shen F, et al: Overexpression of
aspartyl-(asparaginyl)-β-hydroxylase in hepatocellular carcinoma is
associated with worse surgical outcome. Hepatology. 52:164–173.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Xue T, Su J, Li H and Xue X: Evaluation of
HAAH/humbug quantitative detection in the diagnosis of
hepatocellular carcinoma. Oncol Rep. 33:329–337. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Yao WF, Liu JW and Huang DS: Mir-200a
inhibits cell proliferation and EMT by down-regulating the ASPH
expression levels and affecting ERK and PI3K/Akt pathways in human
hepatoma cells. Am J Transl Res. 10:1117–1130. 2018.PubMed/NCBI
|
|
60
|
Tang C, Hou Y, Wang H, Wang K, Xiang H,
Wan X, Xia Y, Li J, Wei W, Xu S, et al: Aspartate β-hydroxylase
disrupts mitochondrial DNA stability and function in hepatocellular
carcinoma. Oncogenesis. 6:e3622017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Shimoda M, Tomimaru Y, Charpentier KP,
Safran H, Carlson RI and Wands J: Tumor progression-related
transmembrane protein aspartate-β-hydroxylase is a target for
immunotherapy of hepatocellular carcinoma. J Hepatol. 56:1129–1135.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Marzo AL, Kinnear BF, Lake RA, Frelinger
JJ, Collins EJ, Robinson BW and Scott B: Tumor-specific CD4 + T
cells have a major ‘post-licensing’ role in CTL mediated anti-tumor
immunity. J Immunol. 165:6047–6055. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Kennedy R and Celis E: Multiple roles for
CD4+ T cells in anti-tumor immune responses. Immunol Rev.
222:129–144. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Tyson GL and El-Serag HB: Risk factors for
cholangiocarcinoma. Hepatology. 54:173–184. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Weber SM, Jarnagin WR, Klimstra D,
DeMatteo RP, Fong Y and Blumgart LH: Intrahepatic
cholangiocarcinoma: Resectability, recurrence pattern, and
outcomes. J Am Coll Surg. 193:384–391. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Maeda T, Taguchi K, Aishima S, Shimada M,
Hintz D, Larusso N, Gores G, Tsuneyoshi M, Sugimachi K, Wands JR
and de la Monte SM: Clinicopathological correlates of aspartyl
(asparaginyl) beta-hydroxylase over-expression in
cholangiocarcinoma. Cancer Detect Prev. 28:313–318. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Yoo HJ, Yun BR, Kwon JH, Ahn HS, Seol MA,
Lee MJ, Yu GR, Yu HC, Hong B, Choi K and Kim DG: Genetic and
expression alterations in association with the sarcomatous change
of cholangiocarcinoma cells. Exp Mol Med. 41:102–115. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Huang CK, Iwagami Y, Aihara A, Chung W, de
la Monte S, Thomas JM, Olsen M, Carlson R, Yu T, Dong X and Wands
J: Anti-tumor effects of second generation β-hydroxylase inhibitors
on cholangiocarcinoma development and progression. PLoS One.
11:e01503362016. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Sugimachi K, Aishima S, Taguchi K, Tanaka
S, Shimada M, Kajiyama K, Sugimachi K and Tsuneyoshi M: The role of
overexpression and gene amplification of cyclin D1 in intrahepatic
cholangiocarcinoma. J Hepatol. 35:74–79. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Noda T, Shimoda M, Ortiz V, Sirica AE and
Wands JR: Immunization with aspartate-β-hydroxylase-loaded
dendritic cells produces antitumor effects in a rat model of
intrahepatic cholangiocarcinoma. Hepatology. 55:86–97. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Huang CK, Iwagami Y, Zou J, Casulli S, Lu
S, Nagaoka K, Ji C, Ogawa K, Cao KY, Gao JS, et al: Aspartate
beta-hydroxylase promotes cholangiocarcinoma progression by
modulating RB1 phosphorylation. Cancer Lett. 429:1–10. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Giacinti C and Giordano A: RB and cell
cycle progression. Oncogene. 25:5220–5227. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Narita M, Nũnez S, Heard E, Narita M, Lin
AW, Hearn SA, Spector DL, Hannon GJ and Lowe SW: Rb-mediated
heterochromatin formation and silencing of E2F target genes during
cellular senescence. Cell. 113:703–716. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2019. CA Cancer J Clin. 69:7–34. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ogawa K, Lin Q, Li L, Bai X, Chen X, Chen
H, Kong R, Wang Y, Zhu H, He F, et al: Aspartate β-hydroxylase
promotes pancreatic ductal adenocarcinoma metastasis through
activation of SRC signaling pathway. J Hematol Oncol. 12:1442019.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Ogawa K, Lin Q, Li L, Bai X, Chen X, Chen
H, Kong R, Wang Y, Zhu H, He F, et al: Prometastatic secretome
trafficking via exosomes initiates pancreatic cancer pulmonary
metastasis. Cancer Lett. 481:63–75. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Jove R and Hanafusa H: Cell transformation
by the viral src oncogene. Annu Rev Cell Biol. 3:31–56. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Hou G, Xu B, Bi Y, Wu C, Ru B, Sun B and
Bai X: Recent advances in research on aspartate β-hydroxylase
(ASPH) in pancreatic cancer: A brief update. Bosn J Basic Med Sci.
18:297–304. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Nagaoka K, Bai X, Ogawa K, Dong X, Zhang
S, Zhou Y, Carlson RI, Jiang ZG, Fuller S, Lebowitz MS, et al:
Anti-tumor activity of antibody drug conjugate targeting
aspartate-β-hydroxylase in pancreatic ductal adenocarcinoma. Cancer
Lett. 449:87–98. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Dekker E, Tanis PJ, Vleugels JLA, Kasi PM
and Wallace MB: Colorectal cancer. Lancet. 394:1467–1480. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Benelli R, Costa D, Mastracci L, Grillo F,
Olsen MJ, Barboro P, Poggi A and Ferrari N:
Aspartate-β-hydroxylase: A promising target to limit the local
invasiveness of colorectal cancer. Cancers (Basel). 12:9712020.
View Article : Google Scholar
|
|
82
|
Jackstadt R, van Hooff SR, Leach JD,
Cortes-Lavaud X, Lohuis JO, Ridgway RA, Wouters VM, Roper J,
Kendall TJ, Roxburgh CS, et al: Epithelial NOTCH signaling rewires
the tumor microenvironment of colorectal cancer to drive
poor-prognosis subtypes and metastasis. Cancer Cell. 36:319–336.e7.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Kadota M, Sato M, Duncan B, Ooshima A,
Yang HH, Diaz-Meyer N, Gere S, Kageyama S, Fukuoka J, Nagata T, et
al: Identification of novel gene amplifications in breast cancer
and coexistence of gene amplification with an activating mutation
of PIK3CA. Cancer Res. 69:7357–7365. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Shimoda M, Hori A, Wands JR, Tsunashima R,
Naoi Y, Miyake T, Tanei T, Kagara N, Shimazu K, Kim SJ and Noguchi
S: Endocrine sensitivity of estrogen receptor-positive breast
cancer is negatively correlated with aspartate-β-hydroxylase
expression. Cancer Sci. 108:2454–2461. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Wirsching HG, Galanis E and Weller M:
Glioblastoma. Handb Clin Neurol. 134:381–397. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Chen X, Zhao C, Guo B, Zhao Z, Wang H and
Fang Z: Systematic profiling of alternative mRNA splicing signature
for predicting glioblastoma prognosis. Front Oncol. 9:9282019.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Sturla LM, Tong M, Hebda N, Gao J, Thomas
JM, Olsen M and de la Monte SM: Aspartate-β-hydroxylase (ASPH): A
potential therapeutic target in human malignant gliomas. Heliyon.
2:e002032016. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Chen X, Jin P, Tang H and Zhang L:
miR-135a acts as a tumor suppressor by targeting ASPH in
endometrial cancer. Int J Clin Exp Pathol. 12:3384–3389.
2019.PubMed/NCBI
|
|
89
|
Lahousse SA, Carter JJ, Xu XJ, Wands JR
and de la Monte SM: Differential growth factor regulation of
aspartyl-(asparaginyl)-β-hydroxylase family genes in SH-Sy5y human
neuroblastoma cells. BMC Cell Biol. 7:412006. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Sepe PS, Lahousse SA, Gemelli B, Chang H,
Maeda T, Wands JR and de la Monte SM: Role of the
aspartyl-asparaginyl-beta-hydroxylase gene in neuroblastoma cell
motility. Lab Invest. 82:881–891. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Luu M, Sabo E, de la Monte SM, Greaves W,
Wang J, Tavares R, Simao L, Wands JR, Resnick MB and Wang L:
Prognostic value of aspartyl (asparaginyl)-beta-hydroxylase/humbug
expression in non-small cell lung carcinoma. Hum Pathol.
40:639–644. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Lee JH: Overexpression of humbug promotes
malignant progression in human gastric cancer cells. Oncol Rep.
19:795–800. 2008.PubMed/NCBI
|