|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Matulonis UA, Sood AK, Fallowfield L,
Howitt BE, Sehouli J and Karlan BY: Ovarian cancer. Nat Rev Dis
Primers. 2:160612016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Orr B and Edwards RP: Diagnosis and
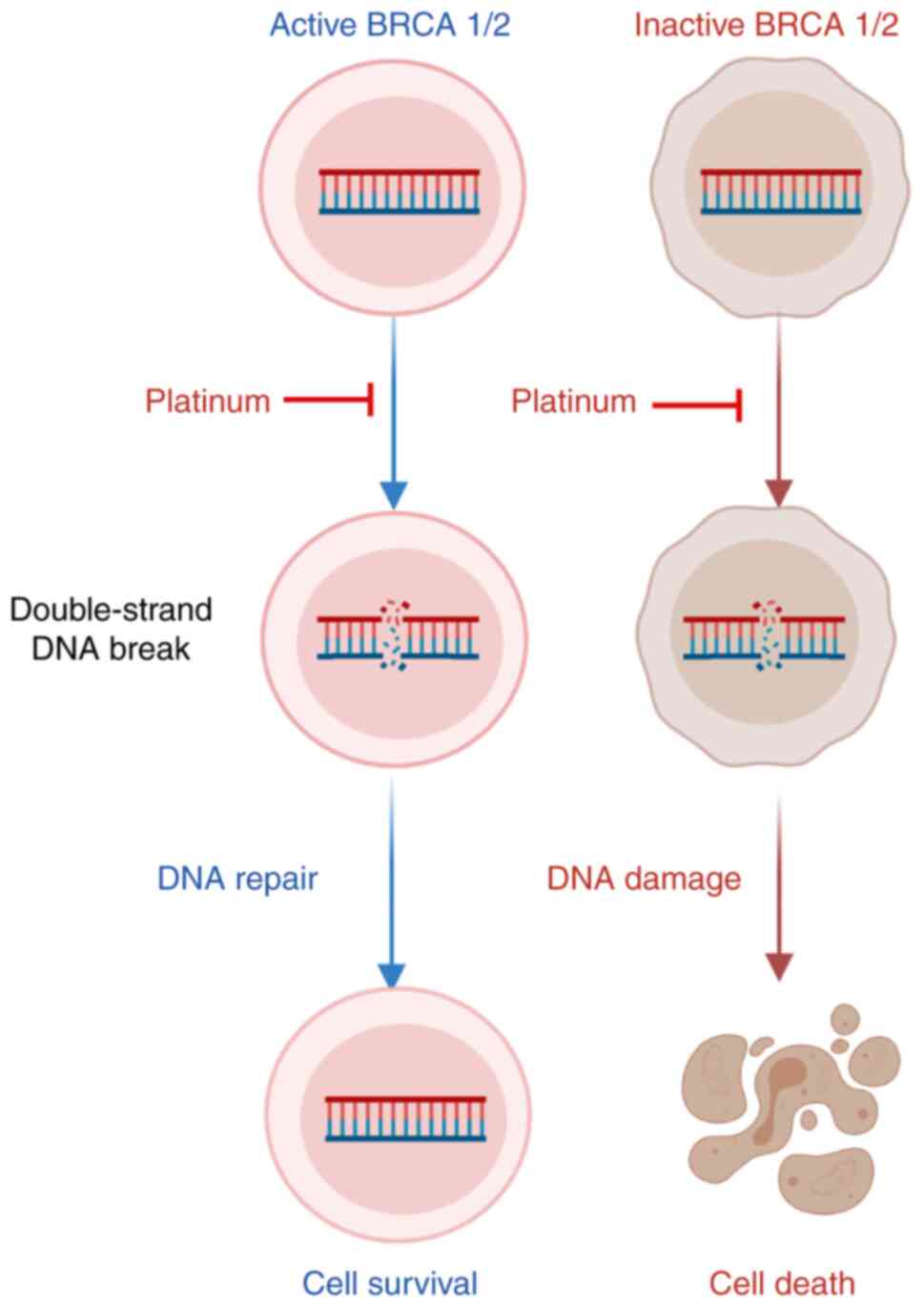
treatment of ovarian cancer. Hematol Oncol Clin North Am.
32:943–964. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gershenson DM, Bodurka DC, Lu KH, Nathan
LC, Milojevic L, Wong KK, Malpica A and Sun CC: Impact of age and
primary disease site on outcome in women with low-grade serous
carcinoma of the ovary or peritoneum: Results of a large
single-institution registry of a rare tumor. J Clin Oncol.
33:2675–2682. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Grisham RN, Sylvester BE, Won H, McDermott
G, DeLair D, Ramirez R, Yao Z, Shen R, Dao F, Bogomolniy F, et al:
Extreme outlier analysis identifies occult mitogen-activated
protein kinase pathway mutations in patients with low-grade serous
ovarian cancer. J Clin Oncol. 33:4099–4105. 2015. View Article : Google Scholar : PubMed/NCBI
|
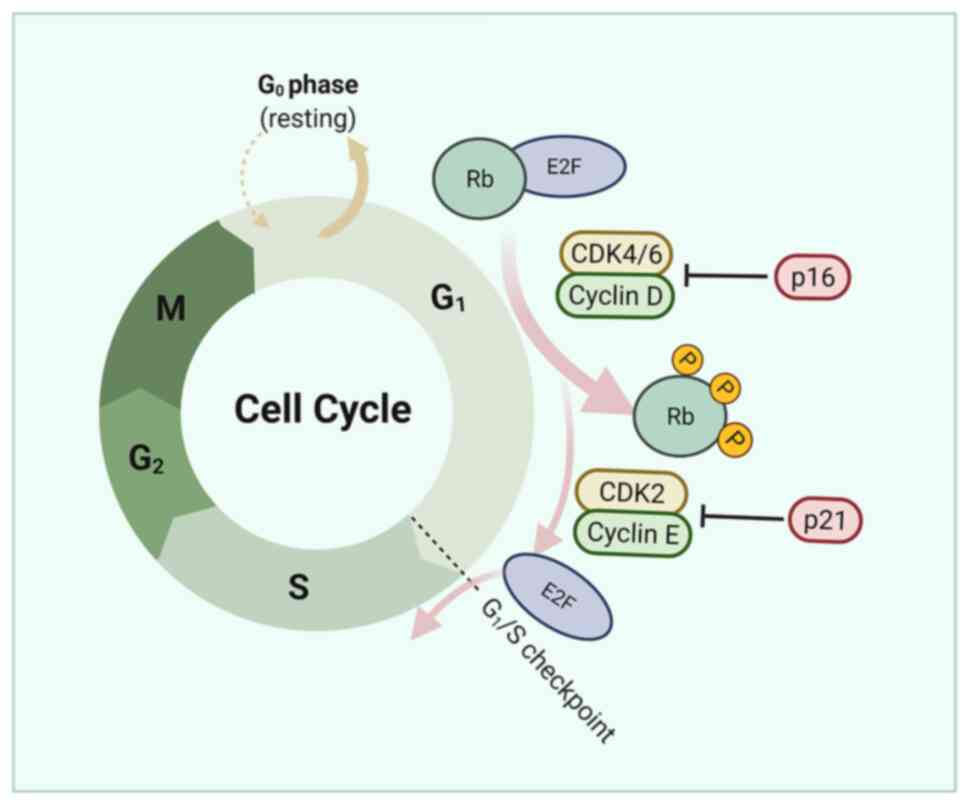
|
6
|
Chui MH, Chang JC, Zhang Y, Zehir A,
Schram AM, Konner J, Drilon AE, Da Cruz Paula A, Weigelt B and
Grisham RN: Spectrum of BRAF mutations and gene rearrangements in
ovarian serous carcinoma. JCO Precis Oncol. 5:PO.21.00055.
2021.PubMed/NCBI
|
|
7
|
Davidson B and Tropé CG: Ovarian cancer:
Diagnostic, biological and prognostic aspects. Women's Health
(Lond). 10:519–533. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Reavis HD and Drapkin R: The tubal
epigenome-An emerging target for ovarian cancer. Pharmacol Ther.
210:1075242020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Coleman RL, Duska LR, Ramirez PT, Heymach
JV, Kamat AA, Modesitt SC, Schmeler KM, Iyer RB, Garcia ME, Miller
DL, et al: Phase 1–2 study of docetaxel plus aflibercept in
patients with recurrent ovarian, primary peritoneal, or fallopian
tube cancer. Lancet Oncol. 12:1109–1117. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
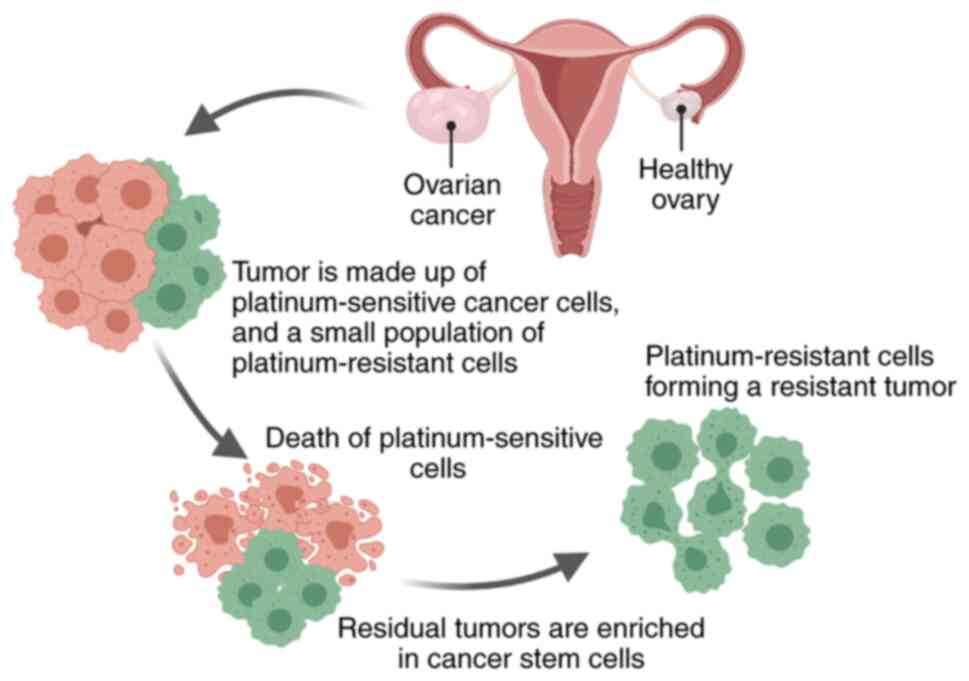
Nowak M and Klink M: The Role of
Tumor-associated macrophages in the progression and chemoresistance
of ovarian cancer. Cells. 9:12992020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Aghajanian C, Blank SV, Goff BA, Judson
PL, Teneriello MG, Husain A, Sovak MA, Yi J and Nycum LR: OCEANS: A
randomized, double-blind, placebo-controlled phase III trial of
chemotherapy with or without bevacizumab in patients with
platinum-sensitive recurrent epithelial ovarian, primary
peritoneal, or fallopian tube cancer. J Clin Oncol. 30:2039–2045.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cruz IN, Coley HM, Kramer HB, Madhuri TK,
Safuwan NA, Angelino AR and Yang M: Proteomics analysis of ovarian
cancer cell lines and tissues reveals drug resistance-associated
proteins. Cancer Genomics Proteomics. 14:35–51. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Disis ML, Taylor MH, Kelly K, Beck JT,
Gordon M, Moore KM, Patel MR, Chaves J, Park H, Mita AC, et al:
Efficacy and safety of avelumab for patients with recurrent or
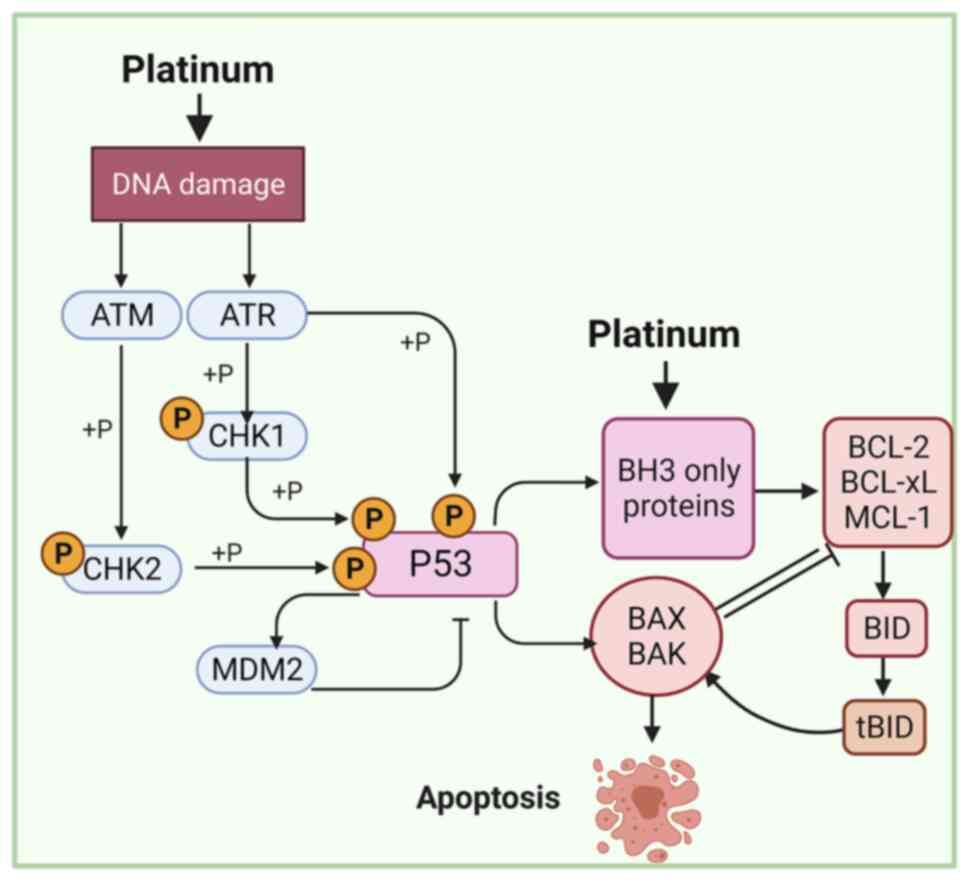
refractory ovarian cancer: Phase 1b results from the JAVELIN solid
tumor trial. JAMA Oncol. 5:393–401. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Moufarrij S, Dandapani M, Arthofer E,
Gomez S, Srivastava A, Lopez-Acevedo M, Villagra A and Chiappinelli
KB: Epigenetic therapy for ovarian cancer: Promise and progress.
Clin Epigenetics. 11:72019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ren F, Shen J, Shi H, Hornicek FJ, Kan Q
and Duan Z: Novel mechanisms and approaches to overcome multidrug
resistance in the treatment of ovarian cancer. Biochim Biophys
Acta. 1866:266–275. 2016.PubMed/NCBI
|
|
16
|
Chen AM, Zhang M, Wei D, Stueber D,
Taratula O, Minko T and He H: Co-delivery of doxorubicin and Bcl-2
siRNA by mesoporous silica nanoparticles enhances the efficacy of
chemotherapy in multidrug-resistant cancer cells. Small.
5:2673–2677. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zalewski M, Kulbacka J, Saczko J,
Drag-Zalesinska M and Choromanska A: Valspodar-modulated
chemotherapy in human ovarian cancer cells SK-OV-3 and MDAH-2774.
Bosn J Basic Med Sci. 19:234–241. 2019.PubMed/NCBI
|
|
18
|
Baekelandt M, Lehne G, Tropé CG, Szántó I,
Pfeiffer P, Gustavssson B and Kristensen GB: Phase I/II trial of
the multidrug-resistance modulator valspodar combined with
cisplatin and doxorubicin in refractory ovarian cancer. J Clin
Oncol. 19:2983–2993. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gee ME, Faraahi Z, McCormick A and
Edmondson RJ: DNA damage repair in ovarian cancer: Unlocking the
heterogeneity. J Ovarian Res. 11:502018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sengupta D, Mukhopadhyay A and Sengupta K:
Emerging roles of lamins and DNA damage repair mechanisms in
ovarian cancer. Biochem Soc Trans. 48:2317–2333. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ledermann JA, Drew Y and Kristeleit RS:
Homologous recombination deficiency and ovarian cancer. Eur J
Cancer. 60:49–58. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Christie EL and Bowtell DDL: Acquired
chemotherapy resistance in ovarian cancer. Ann Oncol. 28 (Suppl
8):viii13–viii15. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Karakashev S, Fukumoto T, Zhao B, Lin J,
Wu S, Fatkhutdinov N, Park PH, Semenova G, Jean S, Cadungog MG, et
al: EZH2 inhibition sensitizes CARM1-high, homologous recombination
proficient ovarian cancers to PARP Inhibition. Cancer Cell.
37:157–167.e6. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Moschetta M, George A, Kaye SB and
Banerjee S: BRCA somatic mutations and epigenetic BRCA
modifications in serous ovarian cancer. Ann Oncol. 27:1449–1455.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Birkbak NJ, Wang ZC, Kim JY, Eklund AC, Li
Q, Tian R, Bowman-Colin C, Li Y, Greene-Colozzi A, Iglehart JD, et
al: Telomeric allelic imbalance indicates defective DNA repair and
sensitivity to DNA-damaging agents. Cancer Discov. 2:366–375. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Du Y, Yamaguchi H, Wei Y, Hsu JL, Wang HL,
Hsu YH, Lin WC, Yu WH, Leonard PG, Lee GR IV, et al: Blocking
c-Met-mediated PARP1 phosphorylation enhances anti-tumor effects of
PARP inhibitors. Nat Med. 22:194–201. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Brown JS, O'Carrigan B, Jackson SP and Yap
TA: Targeting DNA repair in cancer: Beyond PARP inhibitors. Cancer
Discov. 7:20–37. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Alsop K, Fereday S, Meldrum C, DeFazio A,
Emmanuel C, George J, Dobrovic A, Birrer MJ, Webb PM, Stewart C, et
al: BRCA mutation frequency and patterns of treatment response in
BRCA mutation-positive women with ovarian cancer: A report from the
Australian Ovarian Cancer Study Group. J Clin Oncol. 30:2654–2663.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Iyer S, Zhang S, Yucel S, Horn H, Smith
SG, Reinhardt F, Hoefsmit E, Assatova B, Casado J, Meinsohn MC, et
al: Genetically defined syngeneic mouse models of ovarian cancer as
tools for the discovery of combination immunotherapy. Cancer
Discov. 11:384–407. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Domchek SM: Reversion mutations with
clinical use of PARP inhibitors: Many genes, many versions. Cancer
Discov. 7:937–939. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pietragalla A, Arcieri M, Marchetti C,
Scambia G and Fagotti A: Ovarian cancer predisposition beyond BRCA1
and BRCA2 genes. Int J Gynecol Cancer. 30:1803–1810. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lin KK, Harrell MI, Oza AM, Oaknin A,
Ray-Coquard I, Tinker AV, Helman E, Radke MR, Say C, Vo LT, et al:
BRCA reversion mutations in circulating tumor DNA predict primary
and acquired resistance to the PARP inhibitor rucaparib in
high-grade ovarian carcinoma. Cancer Discov. 9:210–219. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Norquist B, Wurz KA, Pennil CC, Garcia R,
Gross J, Sakai W, Karlan BY, Taniguchi T and Swisher EM: Secondary
somatic mutations restoring BRCA1/2 predict chemotherapy resistance
in hereditary ovarian carcinomas. J Clin Oncol. 29:3008–3015. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kondrashova O, Nguyen M, Shield-Artin K,
Tinker AV, Teng NNH, Harrell MI, Kuiper MJ, Ho GY, Barker H, Jasin
M, et al: Secondary somatic mutations restoring RAD51C and RAD51D
associated with acquired resistance to the PARP inhibitor rucaparib
in high-grade ovarian carcinoma. Cancer Discov. 7:984–998. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
He YJ, Meghani K, Caron MC, Yang C, Ronato
DA, Bian J, Sharma A, Moore J, Niraj J, Detappe A, et al: DYNLL1
binds to MRE11 to limit DNA end resection in BRCA1-deficient cells.
Nature. 563:522–526. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Penson RT, Valencia RV, Cibula D, Colombo
N, Leath CA III, Bidziński M, Kim JW, Nam JH, Madry R, Hernández C,
et al: Olaparib versus nonplatinum chemotherapy in patients with
platinum-sensitive relapsed ovarian cancer and a germline BRCA1/2
mutation (SOLO3): A randomized phase III trial. J Clin Oncol.
38:1164–1174. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Marzi L, Szabova L, Gordon M, Weaver Ohler
Z, Sharan SK, Beshiri ML, Etemadi M, Murai J, Kelly K and Pommier
Y: The indenoisoquinoline TOP1 inhibitors selectively target
homologous recombination-deficient and schlafen 11-positive cancer
cells and synergize with olaparib. Clin Cancer Res. 25:6206–6216.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yan S, Xuan J, Brajanovski N, Tancock MRC,
Madhamshettiwar PB, Simpson KJ, Ellis S, Kang J, Cullinane C,
Sheppard KE, et al: The RNA polymerase I transcription inhibitor
CX-5461 cooperates with topoisomerase 1 inhibition by enhancing the
DNA damage response in homologous recombination-proficient
high-grade serous ovarian cancer. Br J Cancer. 124:616–627. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Yap TA, O'Carrigan B, Penney MS, Lim JS,
Brown JS, de Miguel Luken MJ, Tunariu N, Perez-Lopez R, Rodrigues
DN, Riisnaes R, et al: Phase I trial of first-in-class ATR
Inhibitor M6620 (VX-970) as monotherapy or in combination with
carboplatin in patients with advanced solid tumors. J Clin Oncol.
38:3195–3204. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Konstantinopoulos PA, Cheng SC, Wahner
Hendrickson AE, Penson RT, Schumer ST, Doyle LA, Lee EK, Kohn EC,
Duska LR, Crispens MA, et al: Berzosertib plus gemcitabine versus
gemcitabine alone in platinum-resistant high-grade serous ovarian
cancer: A multicentre, open-label, randomised, phase 2 trial.
Lancet Oncol. 21:957–968. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nakayama N, Nakayama K, Shamima Y,
Ishikawa M, Katagiri A, Iida K and Miyazaki K: Gene amplification
CCNE1 is related to poor survival and potential therapeutic target
in ovarian cancer. Cancer. 116:2621–2634. 2010.PubMed/NCBI
|
|
42
|
Au-Yeung G, Lang F, Azar WJ, Mitchell C,
Jarman KE, Lackovic K, Aziz D, Cullinane C, Pearson RB, Mileshkin
L, et al: Selective targeting of cyclin E1-Amplified high-grade
serous ovarian cancer by cyclin-dependent kinase 2 and AKT
Inhibition. Clin Cancer Res. 23:1862–1874. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Etemadmoghadam D, Weir BA, Au-Yeung G,
Alsop K, Mitchell G, George J; Australian Ovarian Cancer Study
Group, ; Davis S, D'Andrea AD, Simpson K, et al: Synthetic
lethality between CCNE1 amplification and loss of BRCA1. Proc Natl
Acad Sci USA. 110:19489–19494. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Campbell GJ, Hands EL and Van de Pette M:
The Role of CDKs and CDKIs in murine development. Int J Mol Sci.
21:53432020. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Angius G, Tomao S, Stati V, Vici P, Bianco
V and Tomao F: Prexasertib, a checkpoint kinase inhibitor: From
preclinical data to clinical development. Cancer Chemother
Pharmacol. 85:9–20. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kim H, Xu H, George E, Hallberg D, Kumar
S, Jagannathan V, Medvedev S, Kinose Y, Devins K, Verma P, et al:
Combining PARP with ATR inhibition overcomes PARP inhibitor and
platinum resistance in ovarian cancer models. Nat Commun.
11:37262020. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Gorski JW, Ueland FR and Kolesar JM: CCNE1
amplification as a predictive biomarker of chemotherapy resistance
in epithelial ovarian cancer. Diagnostics (Basel). 10:2792020.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Gralewska P, Gajek A, Marczak A and
Rogalska A: Participation of the ATR/CHK1 pathway in replicative
stress targeted therapy of high-grade ovarian cancer. J Hematol
Oncol. 13:392020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Garsed DW, Alsop K, Fereday S, Emmanuel C,
Kennedy CJ, Etemadmoghadam D, Gao B, Gebski V, Garès V, Christie
EL, et al: Homologous recombination DNA repair pathway disruption
and retinoblastoma protein loss are associated with exceptional
survival in high-grade serous ovarian cancer. Clin Cancer Res.
24:569–580. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
da Costa AABA, do Canto LM, Larsen SJ,
Ribeiro ARG, Stecca CE, Petersen AH, Aagaard MM, de Brot L,
Baumbach J, Baiocchi G, et al: Genomic profiling in ovarian cancer
retreated with platinum based chemotherapy presented homologous
recombination deficiency and copy number imbalances of CCNE1 and
RB1 genes. BMC Cancer. 19:4222019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Shi M, Whorton AE, Sekulovski N, Paquet M,
MacLean JA, Song Y, Van Dyke T and Hayashi K: Inactivation of
TRP53, PTEN, RB1, and/or CDH1 in the ovarian surface epithelium
induces ovarian cancer transformation and metastasis. Biol Reprod.
102:1055–1064. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Dall'Acqua A, Sonego M, Pellizzari I,
Pellarin I, Canzonieri V, D'Andrea S, Benevol S, Sorio R, Giorda G,
Califano D, et al: CDK6 protects epithelial ovarian cancer from
platinum-induced death via FOXO3 regulation. EMBO Mol Med.
9:1415–1433. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Giacomini I, Ragazzi E, Pasut G and
Montopoli M: The pentose phosphate pathway and its involvement in
cisplatin resistance. Int J Mol Sci. 21:9372020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Morandi A and Indraccolo S: Linking
metabolic reprogramming to therapy resistance in cancer. Biochim
Biophys Acta Rev Cancer. 868:1–6. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Zhao Y, Butler EB and Tan M: Targeting
cellular metabolism to improve cancer therapeutics. Cell Death Dis.
4:e5322013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Butler EB, Zhao Y, Muñoz-Pinedo C, Lu J
and Tan M: Stalling the engine of resistance: Targeting cancer
metabolism to overcome therapeutic resistance. Cancer Res.
73:2709–2717. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Tennant DA, Durán RV and Gottlieb E:
Targeting metabolic transformation for cancer therapy. Nat Rev
Cancer. 10:267–277. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Yeung SJ, Pan J and Lee MH: Roles of p53,
MYC and HIF-1 in regulating glycolysis-the seventh hallmark of
cancer. Cell Mol Life Sci. 65:3981–3999. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Icard P, Shulman S, Farhat D, Steyaert JM,
Alifano M and Lincet H: How the Warburg effect supports
aggressiveness and drug resistance of cancer cells? Drug Resist
Updat. 38:1–11. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Ai Z, Lu Y, Qiu S and Fan Z: Overcoming
cisplatin resistance of ovarian cancer cells by targeting
HIF-1-regulated cancer metabolism. Cancer Lett. 373:36–44. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ricci F, Brunelli L, Affatato R, Chilà R,
Verza M, Indraccolo S, Falcetta F, Fratelli M, Fruscio R,
Pastorelli R and Damia G: Overcoming platinum-acquired resistance
in ovarian cancer patient-derived xenografts. Ther Adv Med Oncol.
11:17588359198395432019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Urpilainen E, Puistola U, Boussios S and
Karihtala P: Metformin and ovarian cancer: The evidence. Ann Transl
Med. 8:17112020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Kim TH, Suh DH, Kim MK and Song YS:
Metformin against cancer stem cells through the modulation of
energy metabolism: Special considerations on ovarian cancer. Biomed
Res Int. 2014:1327022014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Itoh K, Tong KI and Yamamoto M: Molecular
mechanism activating Nrf2-Keap1 pathway in regulation of adaptive
response to electrophiles. Free Radic Biol Med. 36:1208–1213. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Wu X, Han LY, Zhang XX and Wang L: The
study of Nrf2 signaling pathway in ovarian cancer. Crit Rev
Eukaryot Gene Expr. 28:329–336. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Gentric G, Kieffer Y, Mieulet V, Goundiam
O, Bonneau C, Nemati F, Hurbain I, Raposo G, Popova T, Stern MH, et
al: PML-regulated mitochondrial metabolism enhances
chemosensitivity in human ovarian cancers. Cell Metab.
29:156–173.e10. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Lister A, Nedjadi T, Kitteringham NR,
Campbell F, Costello E, Lloyd B, Copple IM, Williams S, Owen A,
Neoptolemos JP, et al: Nrf2 is overexpressed in pancreatic cancer:
Implications for cell proliferation and therapy. Mol Cancer.
10:372011. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
van der Wijst MG, Huisman C, Mposhi A,
Roelfes G and Rots MG: Targeting Nrf2 in healthy and malignant
ovarian epithelial cells: Protection versus promotion. Mol Oncol.
9:1259–1273. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Hou D, Liu Z, Xu X, Liu Q, Zhang X, Kong
B, Wei JJ, Gong Y and Shao C: Increased oxidative stress mediates
the antitumor effect of PARP inhibition in ovarian cancer. Redox
Biol. 17:99–111. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Kleih M, Böpple K, Dong M, Gaissler A,
Heine S, Olayioye MA, Aulitzky WE and Essmann F: Direct impact of
cisplatin on mitochondria induces ROS production that dictates cell
fate of ovarian cancer cells. Cell Death Dis. 10:8512019.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Podratz JL, Knight AM, Ta LE, Staff NP,
Gass JM, Genelin K, Schlattau A, Lathroum L and Windebank AJ:
Cisplatin induced mitochondrial DNA damage in dorsal root ganglion
neurons. Neurobiol Dis. 41:661–668. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Yang Z, Schumaker LM, Egorin MJ, Zuhowski
EG, Guo Z and Cullen KJ: Cisplatin preferentially binds
mitochondrial DNA and voltage-dependent anion channel protein in
the mitochondrial membrane of head and neck squamous cell
carcinoma: Possible role in apoptosis. Clin Cancer Res.
12:5817–5825. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Zhang J, Yang L, Xiang X, Li Z, Qu K and
Li K: A panel of three oxidative stress-related genes predicts
overall survival in ovarian cancer patients received platinum-based
chemotherapy. Aging (Albany NY). 10:1366–1379. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Verschoor ML and Singh G: Ets-1 regulates
intracellular glutathione levels: Key target for resistant ovarian
cancer. Mol Cancer. 12:1382013. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Wilson LA, Yamamoto H and Singh G: Role of
the transcription factor Ets-1 in cisplatin resistance. Mol Cancer
Ther. 3:823–832. 2004.PubMed/NCBI
|
|
76
|
Nwani NG, Condello S, Wang Y, Swetzig WM,
Barber E, Hurley T and Matei D: A Novel ALDH1A1 inhibitor targets
cells with stem cell characteristics in ovarian cancer. Cancers
(Basel). 11:5022019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Batlle E and Clevers H: Cancer stem cells
revisited. Nat Med. 23:1124–1134. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Beck B and Blanpain C: Unravelling cancer
stem cell potential. Nat Rev Cancer. 13:727–738. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Carnero A, Garcia-Mayea Y, Mir C, Lorente
J, Rubio IT and LLeonart ME: The cancer stem-cell signaling network
and resistance to therapy. Cancer Treat Rev. 49:25–36. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Maugeri-Saccà M, Vigneri P and De Maria R:
Cancer stem cells and chemosensitivity. Clin Cancer Res.
17:4942–4947. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Hu L, McArthur C and Jaffe RB: Ovarian
cancer stem-like side-population cells are tumourigenic and
chemoresistant. Br J Cancer. 102:1276–1283. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Zhang S, Balch C, Chan MW, Lai HC, Matei
D, Schilder JM, Yan PS, Huang TH and Nephew KP: Identification and
characterization of ovarian cancer-initiating cells from primary
human tumors. Cancer Res. 68:4311–4320. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Wang Y, Zhao G, Condello S, Huang H,
Cardenas H, Tanner EJ, Wei J, Ji Y, Li J, Tan Y, et al: Frizzled-7
identifies platinum-tolerant ovarian cancer cells susceptible to
ferroptosis. Cancer Res. 81:384–399. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Chen J, Cao X, An Q, Zhang Y, Li K, Yao W,
Shi F, Pan Y, Jia Q, Zhou W, et al: Inhibition of cancer stem cell
like cells by a synthetic retinoid. Nat Commun. 9:14062018.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Muñoz-Galván S, Felipe-Abrio B,
Verdugo-Sivianes EM, Perez M, Jiménez-García MP, Suarez-Martinez E,
Estevez-Garcia P and Carnero A: Downregulation of MYPT1 increases
tumor resistance in ovarian cancer by targeting the Hippo pathway
and increasing the stemness. Mol Cancer. 19:72020. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Keyvani V, Farshchian M, Esmaeili SA, Yari
H, Moghbeli M, Nezhad SK and Abbaszadegan MR: Ovarian cancer stem
cells and targeted therapy. J Ovarian Res. 12:1202019. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Baba T, Convery PA, Matsumura N, Whitaker
RS, Kondoh E, Perry T, Huang Z, Bentley RC, Mori S, Fujii S, et al:
Epigenetic regulation of CD133 and tumorigenicity of
CD133+ ovarian cancer cells. Oncogene. 28:209–218. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Cole AJ, Iyengar M, Panesso-Gómez S,
O'Hayer P, Chan D, Delgoffe GM, Aird KM, Yoon E, Bai S and
Buckanovich RJ: NFATC4 promotes quiescence and chemotherapy
resistance in ovarian cancer. JCI Insight. 5:e1314862020.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Silva IA, Bai S, McLean K, Yang K,
Griffith K, Thomas D, Ginestier C, Johnston C, Kueck A, Reynolds
RK, et al: Aldehyde dehydrogenase in combination with CD133 defines
angiogenic ovarian cancer stem cells that portend poor patient
survival. Cancer Res. 71:3991–4001. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Li SS, Ma J and Wong AST: Chemoresistance
in ovarian cancer: Exploiting cancer stem cell metabolism. J
Gynecol Oncol. 29:e322018. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Deng J, Bai X, Feng X, Ni J, Beretov J,
Graham P and Li Y: Inhibition of PI3K/Akt/mTOR signaling pathway
alleviates ovarian cancer chemoresistance through reversing
epithelial-mesenchymal transition and decreasing cancer stem cell
marker expression. BMC Cancer. 19:6182019. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Brown JR, Chan DK, Shank JJ, Griffith KA,
Fan H, Szulawski R, Yang K, Reynolds RK, Johnston C, McLean K, et
al: Phase II clinical trial of metformin as a cancer stem
cell-targeting agent in ovarian cancer. JCI Insight.
5:e1332472020.PubMed/NCBI
|
|
93
|
Bogani G, Lopez S, Mantiero M, Ducceschi
M, Bosio S, Ruisi S, Sarpietro G, Guerrisi R, Brusadelli C,
Dell'Acqua A, et al: Immunotherapy for platinum-resistant ovarian
cancer. Gynecol Oncol. 158:484–488. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Nelson BH: The impact of T-cell immunity
on ovarian cancer outcomes. Immunol Rev. 222:101–116. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Zhang L, Conejo-Garcia JR, Katsaros D,
Gimotty PA, Massobrio M, Regnani G, Makrigiannakis A, Gray H,
Schlienger K, Liebman MN, et al: Intratumoral T cells, recurrence,
and survival in epithelial ovarian cancer. N Engl J Med.
348:203–213. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Shen GH, Ghazizadeh M, Kawanami O, Shimizu
H, Jin E, Araki T and Sugisaki Y: Prognostic significance of
vascular endothelial growth factor expression in human ovarian
carcinoma. Br J Cancer. 83:196–203. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Chen CA, Cheng WF, Lee CN, Chen TM, Kung
CC, Hsieh FJ and Hsieh CY: Serum vascular endothelial growth factor
in epithelial ovarian neoplasms: Correlation with patient survival.
Gynecol Oncol. 74:235–240. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Germano G, Frapolli R, Belgiovine C,
Anselmo A, Pesce S, Liguori M, Erba E, Uboldi S, Zucchetti M,
Pasqualini F, et al: Role of macrophage targeting in the antitumor
activity of trabectedin. Cancer Cell. 23:249–262. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
An Y and Yang Q: Tumor-associated
macrophage-targeted therapeutics in ovarian cancer. Int J Cancer.
149:21–30. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Liang R, Chen X, Chen L, Wan F, Chen K,
Sun Y and Zhu X: STAT3 signaling in ovarian cancer: A potential
therapeutic target. J Cancer. 11:837–848. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Lamichhane P, Karyampudi L, Shreeder B,
Krempski J, Bahr D, Daum J, Kalli KR, Goode EL, Block MS, Cannon MJ
and Knutson KL: IL10 Release upon PD-1 blockade sustains
immunosuppression in ovarian cancer. Cancer Res. 77:6667–6678.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Wan C, Keany MP, Dong H, Al-Alem LF,
Pandya UM, Lazo S, Boehnke K, Lynch KN, Xu R, Zarrella DT, et al:
Enhanced efficacy of simultaneous PD-1 and PD-L1 immune checkpoint
blockade in high-grade serous ovarian cancer. Cancer Res.
81:158–173. 2021.PubMed/NCBI
|
|
103
|
Kalim M, Iqbal Khan MS and Zhan J:
Programmed cell death ligand-1: A dynamic immune checkpoint in
cancer therapy. Chem Biol Drug Des. 95:552–566. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Constantinidou A, Alifieris C and Trafalis
DT: Targeting programmed cell death −1 (PD-1) and Ligand (PD-L1): A
new era in cancer active immunotherapy. Pharmacol Ther. 194:84–106.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Fraser M, Leung B, Jahani-Asl A, Yan X,
Thompson WE and Tsang BK: Chemoresistance in human ovarian cancer:
The role of apoptotic regulators. Reprod Biol Endocrinol. 1:662003.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Janzen DM, Tiourin E, Salehi JA, Paik DY,
Lu J, Pellegrini M and Memarzadeh S: An apoptosis-enhancing drug
overcomes platinum resistance in a tumour-initiating subpopulation
of ovarian cancer. Nat Commun. 6:79562015. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Ni Chonghaile T, Sarosiek KA, Vo TT, Ryan
JA, Tammareddi A, Moore Vdel G, Deng J, Anderson KC, Richardson P,
Tai YT, et al: Pretreatment mitochondrial priming correlates with
clinical response to cytotoxic chemotherapy. Science.
334:1129–1133. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Baekelandt M, Kristensen GB, Nesland JM,
Tropé CG and Holm R: Clinical significance of apoptosis-related
factors p53, Mdm2, and Bcl-2 in advanced ovarian cancer. J Clin
Oncol. 17:20611999. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Baekelandt M, Holm R, Nesland JM, Tropé CG
and Kristensen GB: Expression of apoptosis-related proteins is an
independent determinant of patient prognosis in advanced ovarian
cancer. J Clin Oncol. 18:3775–3781. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Binju M, Amaya-Padilla MA, Wan G,
Gunosewoyo H, Suryo Rahmanto Y and Yu Y: Therapeutic inducers of
apoptosis in ovarian cancer. Cancers (Basel). 11:17862019.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Zervantonakis IK, Iavarone C, Chen HY,
Selfors LM, Palakurthi S, Liu JF, Drapkin R, Matulonis U, Leverson
JD, Sampath D, et al: Systems analysis of apoptotic priming in
ovarian cancer identifies vulnerabilities and predictors of drug
response. Nat Commun. 8:3652017. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Reles A, Wen WH, Schmider A, Gee C,
Runnebaum IB, Kilian U, Jones LA, El-Naggar A, Minguillon C,
Schönborn I, et al: Correlation of p53 mutations with resistance to
platinum-based chemotherapy and shortened survival in ovarian
cancer. Clin Cancer Res. 7:2984–2997. 2001.PubMed/NCBI
|
|
113
|
Lee JM, Nair J, Zimmer A, Lipkowitz S,
Annunziata CM, Merino MJ, Swisher EM, Harrell MI, Trepel JB, Lee
MJ, et al: Prexasertib, a cell cycle checkpoint kinase 1 and 2
inhibitor, in BRCA wild-type recurrent high-grade serous ovarian
cancer: A first-in-class proof-of-concept phase 2 study. Lancet
Oncol. 19:207–215. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Chui MH, Momeni Boroujeni A, Mandelker D,
Ladanyi M and Soslow RA: Characterization of TP53-wildtype
tubo-ovarian high-grade serous carcinomas: Rare exceptions to the
binary classification of ovarian serous carcinoma. Mod Pathol.
34:490–501. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Lavarino C, Pilotti S, Oggionni M, Gatti
L, Perego P, Bresciani G, Pierotti MA, Scambia G, Ferrandina G,
Fagotti A, et al: p53 gene status and response to
platinum/paclitaxel-based chemotherapy in advanced ovarian
carcinoma. J Clin Oncol. 18:3936–3945. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Jones S, Wang TL, Shih IeM, Mao TL,
Nakayama K, Roden R, Glas R, Slamon D, Diaz LA Jr, Vogelstein B, et
al: Frequent mutations of chromatin remodeling gene ARID1A in
ovarian clear cell carcinoma. Science. 330:228–231. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Wiegand KC, Shah SP, Al-Agha OM, Zhao Y,
Tse K, Zeng T, Senz J, McConechy MK, Anglesio MS, Kalloger SE, et
al: ARID1A mutations in endometriosis-associated ovarian
carcinomas. N Engl J Med. 363:1532–1543. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Guan B, Wang TL and Shih IeM: ARID1A, a
factor that promotes formation of SWI/SNF-mediated chromatin
remodeling, is a tumor suppressor in gynecologic cancers. Cancer
Res. 71:6718–6727. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Bitler BG, Wu S, Park PH, Hai Y, Aird KM,
Wang Y, Zhai Y, Kossenkov AV, Vara-Ailor A, Rauscher FJ III, et al:
ARID1A-mutated ovarian cancers depend on HDAC6 activity. Nat Cell
Biol. 19:962–973. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Saha S, Panigrahi DP, Patil S and Bhutia
SK: Autophagy in health and disease: A comprehensive review. Biomed
Pharmacother. 104:485–495. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Hu YL, Jahangiri A, Delay M and Aghi MK:
Tumor cell autophagy as an adaptive response mediating resistance
to treatments such as antiangiogenic therapy. Cancer Res.
72:4294–4299. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Yu H, Su J, Xu Y, Kang J, Li H, Zhang L,
Yi H, Xiang X, Liu F and Sun L: p62/SQSTM1 involved in cisplatin
resistance in human ovarian cancer cells by clearing ubiquitinated
proteins. Eur J Cancer. 47:1585–1594. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Zhang Y, Cheng Y, Ren X, Zhang L, Yap KL,
Wu H, Patel R, Liu D, Qin ZH, Shih IM and Yang JM: NAC1 modulates
sensitivity of ovarian cancer cells to cisplatin by altering the
HMGB1-mediated autophagic response. Oncogene. 31:1055–1064. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Huang Z, Zhou L, Chen Z, Nice EC and Huang
C: Stress management by autophagy: Implications for
chemoresistance. Int J Cancer. 139:23–32. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Follo C, Cheng Y, Richards WG, Bueno R and
Broaddus VC: Inhibition of autophagy initiation potentiates
chemosensitivity in mesothelioma. Mol Carcinog. 57:319–332. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
126
|
He J, Yu JJ, Xu Q, Wang L, Zheng JZ, Liu
LZ and Jiang BH: Downregulation of ATG14 by EGR1-MIR152 sensitizes
ovarian cancer cells to cisplatin-induced apoptosis by inhibiting
cyto-protective autophagy. Autophagy. 11:373–384. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Shteingauz A, Boyango I, Naroditsky I,
Hammond E, Gruber M, Doweck I, Ilan N and Vlodavsky I: Heparanase
enhances tumor growth and chemoresistance by promoting autophagy.
Cancer Res. 75:3946–3957. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Ashrafizadeh M, Zarrabi A, Orouei S,
Kiavash Hushmandi, Hakimi A, Amirhossein Zabolian, Daneshi S,
Samarghandian S, Baradaran B and Najafi M: MicroRNA-mediated
autophagy regulation in cancer therapy: The role in
chemoresistance/chemosensitivity. Eur J Pharmacol. 892:1736602021.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Sun C, Fang Y, Yin J, Chen J, Ju Z, Zhang
D, Chen X, Vellano CP, Jeong KJ, Ng PK, et al: Rational combination
therapy with PARP and MEK inhibitors capitalizes on therapeutic
liabilities in RAS mutant cancers. Sci Transl Med. 9:eaal51482017.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Chandarlapaty S, Sawai A, Scaltriti M,
Rodrik-Outmezguine V, Grbovic-Huezo O, Serra V, Majumder PK,
Baselga J and Rosen N: AKT inhibition relieves feedback suppression
of receptor tyrosine kinase expression and activity. Cancer Cell.
19:58–71. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Aksamitiene E, Kiyatkin A and Kholodenko
BN: Cross-talk between mitogenic Ras/MAPK and survival PI3K/Akt
pathways: A fine balance. Biochem Soc Trans. 40:139–146. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Gewinner C, Wang ZC, Richardson A,
Teruya-Feldstein J, Etemadmoghadam D, Bowtell D, Barretina J, Lin
WM, Rameh L, Salmena L, et al: Evidence that inositol polyphosphate
4-phosphatase type II is a tumor suppressor that inhibits PI3K
signaling. Cancer Cell. 16:115–125. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Carpten JD, Faber AL, Horn C, Donoho GP,
Briggs SL, Robbins CM, Hostetter G, Boguslawski S, Moses TY, Savage
S, et al: A transforming mutation in the pleckstrin homology domain
of AKT1 in cancer. Nature. 448:439–444. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Choi HJ, Heo JH, Park JY, Jeong JY, Cho
HJ, Park KS, Kim SH, Moon YW, Kim JS and An HJ: A novel PI3K/mTOR
dual inhibitor, CMG002, overcomes the chemoresistance in ovarian
cancer. Gynecol Oncol. 153:135–148. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Kim MJ, Lee SJ, Ryu JH, Kim SH, Kwon IC
and Roberts TM: Combination of KRAS gene silencing and PI3K
inhibition for ovarian cancer treatment. J Control Release.
318:98–108. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Gupta S, Nag S, Aggarwal S, Rauthan A and
Warrier N: Maintenance therapy for recurrent epithelial ovarian
cancer: Current therapies and future perspectives-a review. J
Ovarian Res. 12:1032019. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Lorusso PM, Edelman MJ, Bever SL, Forman
KM, Pilat M, Quinn MF, Li J, Heath EI, Malburg LM, Klein PJ, et al:
Phase I study of folate conjugate EC145 (Vintafolide) in patients
with refractory solid tumors. J Clin Oncol. 30:4011–4016. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Naumann RW, Coleman RL, Burger RA,
Sausville EA, Kutarska E, Ghamande SA, Gabrail NY, Depasquale SE,
Nowara E, Gilbert L, et al: PRECEDENT: A randomized phase II trial
comparing vintafolide (EC145) and pegylated liposomal doxorubicin
(PLD) in combination versus PLD alone in patients with
platinum-resistant ovarian cancer. J Clin Oncol. 31:4400–4406.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Moore KN, Martin LP, O'Malley DM,
Matulonis UA, Konner JA, Perez RP, Bauer TM, Ruiz-Soto R and Birrer
MJ: Safety and activity of mirvetuximab soravtansine (IMGN853), a
folate receptor alpha-targeting antibody-drug conjugate, in
platinum-resistant ovarian, fallopian tube, or primary peritoneal
cancer: A Phase I expansion study. J Clin Oncol. 35:1112–1118.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Holmes D: Ovarian cancer: Beyond
resistance. Nature. 527:S2172015. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Huber D, Seitz S, Kast K, Emons G and
Ortmann O: Use of oral contraceptives in BRCA mutation carriers and
risk for ovarian and breast cancer: A systematic review. Arch
Gynecol Obstet. 301:875–884. 2020. View Article : Google Scholar : PubMed/NCBI
|