|
1
|
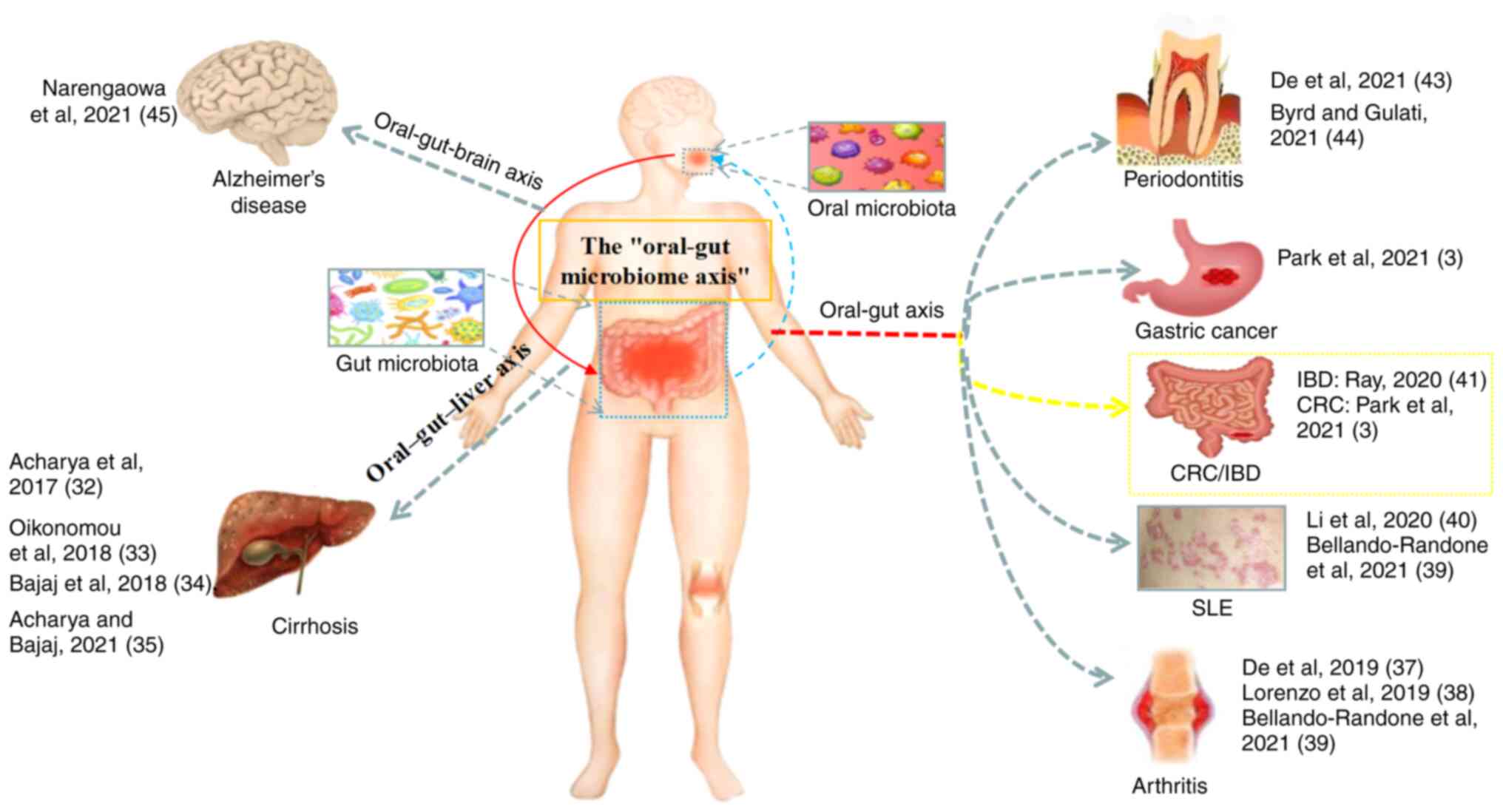
Siegel RL, Miller KD, Goding Sauer A,
Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA and Jemal
A: Colorectal cancer statistics, 2020. CA Cancer J Clin.
70:145–164. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
NIH HMP Working Group, . Peterson J,
Garges S, Giovanni M, McInnes P, Wang L, Schloss JA, Bonazzi V,
McEwen JE, Wetterstrand KA, et al: The NIH human microbiome
project. Genome Res. 19:2317–2323. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
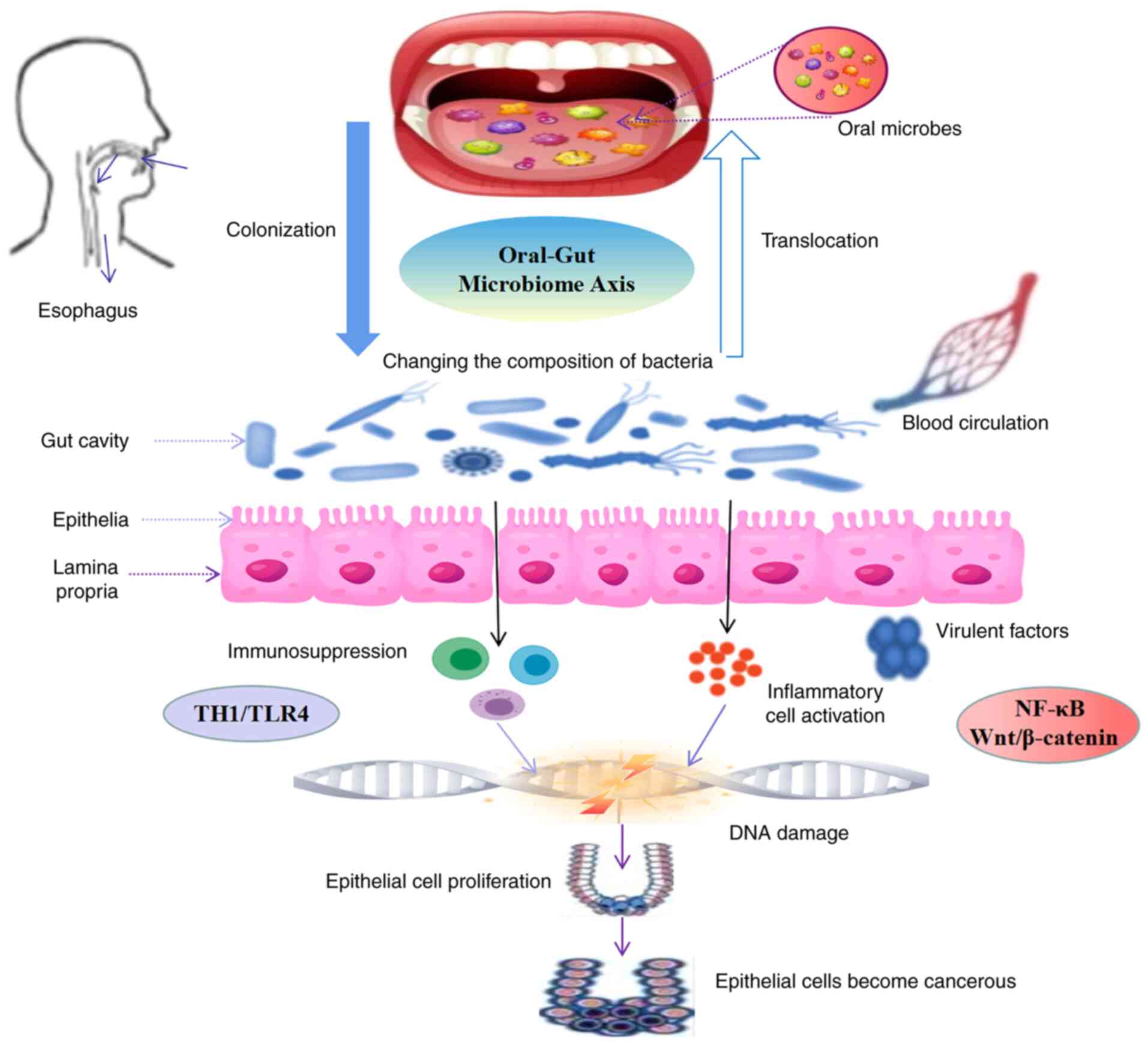
3
|
Park SY, Hwang BO, Lim M, Ok SH, Lee SK,
Chun KS, Park KK, Hu Y, Chung WY and Song NY: Oral-gut microbiome
axis in gastrointestinal disease and cancer. Cancers (Basel).
13:21242021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shi C, Lin L, Xie T, et al: Based on the
‘lung-gut’ axis to explore the influence of lung and gut
microecology on lung diseases. J Nanjing Univ Tradit Chin Med.
02:168–173. 2020.https://t.cnki.net/kcms/detail?v=3uoqIhG8C44YLTlOAiTRKgchrJ08w1e7mYRGNWDareZlYKpvhaXcgDMecYtweZkXRiOLhIZAUMCDDjKrapSPMVkJLBTMn0eV&uniplatform=NZKPT&uid=WEEvREdxOWJmbC9oM1NjYkcyTjdROWp3THN6dy9lNCtTTG4zd1MwcFFNeDg=$R1yZ0H6jyaa0en3RxVUd8df-oHi7XMMDo7mtKT6mSmEvTuk11l2gFA!!
|
|
5
|
Cerdó T, Ruíz A, Suárez A and Campoy C:
Probiotic, prebiotic, and brain development. Nutrients. 9:12472017.
View Article : Google Scholar
|
|
6
|
Muller PA, Schneeberger M, Matheis F, Wang
P, Kerner Z, Ilanges A, Pellegrino K, Del Mármol J, Castro TBR,
Furuichi M, et al: Microbiota modulate sympathetic neurons via a
gut-brain circuit. Nature. 583:441–446. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schmidt TS, Hayward MR, Coelho LP, Li SS,
Costea PI, Voigt AY, Wirbel J, Maistrenko OM, Alves RJ, Bergsten E,
et al: Extensive transmission of microbes along the
gastrointestinal tract. Elife. 8:e426932019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lamont RJ, Koo H and Hajishengallis G: The
oral microbiota: Dynamic communities and host interactions. Nat Rev
Microbiol. 16:745–759. 2018. View Article : Google Scholar
|
|
9
|
Mark Welch JL, Ramírez-Puebla ST and
Borisy GG: Oral microbiome geography: Micron-scale habitat and
niche. Cell Host Microbe. 28:160–168. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li Y: Comparison and analysis of oral
flora structure in patients with gingival cancer and periodontitis:
Commonalities and differences. China Med Univ. 2020.https://t.cnki.net/kcms/detail?v=3uoqIhG8C475KOm_zrgu4lQARvep2SAkJrOyyi_z7N8gBvuHP4X-Bqg6NwePhrlvgbwoWSsn9prYQqxr4×Vg8WYkOENyNYHk&uniplatform=NZKPT&uid=WEEvREdxOWJmbC9oM1NjYkcyTjdROWp3THN6dy9lNCtTTG4zd1MwcFFNeDg=$R1yZ0H6jyaa0en3RxVUd8df-oHi7XMMDo7mtKT6mSmEvTuk11l2gFA!!
|
|
11
|
Chukkapalli SS, Easwaran M, Rivera-Kweh
MF, Velsko IM, Ambadapadi S, Dai J, Larjava H, Lucas AR and
Kesavalu L: Sequential colonization of periodontal pathogens in
induction of periodontal disease and atherosclerosis in LDLRnull
mice. Pathog Dis. 75:ftx0032017. View Article : Google Scholar
|
|
12
|
Segata N, Haake SK, Mannon P, Lemon KP,
Waldron L, Gevers D, Huttenhower C and Izard J: Composition of the
adult digestive tract bacterial microbiome based on seven mouth
surfaces, tonsils, throat and stool samples. Genome Biol.
13:R422012. View Article : Google Scholar
|
|
13
|
Ridlon JM, Kang DJ, Hylemon PB and Bajaj
JS: Bile acids and the gut microbiome. Curr Opin Gastroenterol.
30:332–338. 2014. View Article : Google Scholar
|
|
14
|
Huh JW and Roh TY: Opportunistic detection
of Fusobacterium nucleatum as a marker for the early gut
microbial dysbiosis. BMC Microbiol. 20:2082020. View Article : Google Scholar
|
|
15
|
Del Castillo E, Meier R, Chung M, Koestler
DC, Chen T, Paster BJ, Charpentier KP, Kelsey KT, Izard J and
Michaud DS: The microbiomes of pancreatic and duodenum tissue
overlap and are highly subject specific but differ between
pancreatic cancer and noncancer subjects. Cancer Epidemiol
Biomarkers Prev. 28:370–383. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gevers D, Kugathasan S, Denson LA,
Vázquez-Baeza Y, Van Treuren W, Ren B, Schwager E, Knights D, Song
SJ, Yassour M, et al: The treatment-naive microbiome in new-onset
Crohn's disease. Cell Host Microbe. 15:382–392. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Atarashi K, Suda W, Luo C, Kawaguchi T,
Motoo I, Narushima S, Kiguchi Y, Yasuma K, Watanabe E, Tanoue T, et
al: Ectopic colonization of oral bacteria in the intestine drives
TH1 cell induction and inflammation. Science.
358:359–365. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kong X, Liu J, Cetinbas M, Sadreyev R, Koh
M, Huang H, Adeseye A, He P, Zhu J, Russell H, et al: New and
preliminary evidence on altered oral and gut microbiota in
individuals with autism spectrum disorder (ASD): Implications for
ASD diagnosis and subtyping based on microbial biomarkers.
Nutrients. 11:21282019. View Article : Google Scholar
|
|
19
|
Ding HT, Taur Y and Walkup JT: Gut
microbiota and autism: Key concepts and findings. J Autism Dev
Disord. 47:480–489. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Luna RA, Oezguen N, Balderas M,
Venkatachalam A, Runge JK, Versalovic J, Veenstra-VanderWeele J,
Anderson GM, Savidge T and Williams KC: Distinct
microbiome-neuroimmune signatures correlate with functional
abdominal pain in children with autism spectrum disorder. Cell Mol
Gastroenterol Hepatol. 3:218–230. 2016. View Article : Google Scholar
|
|
21
|
Gargari G, Taverniti V, Gardana C, Cremon
C, Canducci F, Pagano I, Barbaro MR, Bellacosa L, Castellazzi AM,
Valsecchi C, et al: Fecal clostridiales distribution and
short-chain fatty acids reflect bowel habits in irritable bowel
syndrome. Environ Microbiol. 20:3201–3213. 2018. View Article : Google Scholar
|
|
22
|
Sasaki M, Shimoyama Y, Ishikawa T, Kodama
Y, Tajika S and Kimura S: Contribution of different adherent
properties of Granulicatella adiacens and Abiotrophia defectiva to
their associations with oral colonization and the risk of infective
endocarditis. J Oral Sci. 62:36–39. 2020. View Article : Google Scholar
|
|
23
|
Nakatsu G, Li X, Zhou H, Sheng J, Wong SH,
Wu WK, Ng SC, Tsoi H, Dong Y, Zhang N, et al: Gut mucosal
microbiome across stages of colorectal carcinogenesis. Nat Commun.
6:87272015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xia M, Jin Z, Zheng C, et al: Intervention
of traditional Chinese medicine on colitis-cancer transformation
based on oral micro-ecology. China J Tradit Chin Med Pharm.
06:2566–2570. 2019.https://t.cnki.net/kcms/detail?v=3uoqIhG8C44YLTlOAiTRKgchrJ08w1e7CoKB_BvAJUQwzoapsKG3EAOyzzGLBX35huQLjuJ1cPcmeJlWp_hGquH37rR5bVDu&uniplatform=NZKPT&uid=WEEvREdxOWJmbC9oM1NjYkcyTjdROWp3THN6dy9lNCtTTG4zd1MwcFFNeDg=$R1yZ0H6jyaa0en3RxVUd8df-oHi7XMMDo7mtKT6mSmEvTuk11l2gFA!!
|
|
25
|
Toda K, Hisata K, Satoh T, Katsumata N,
Odamaki T, Mitsuyama E, Katayama T, Kuhara T, Aisaka K, Shimizu T
and Xiao JZ: Neonatal oral fluid as a transmission route for
bifidobacteria to the infant gut immediately after birth. Sci Rep.
9:86922019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Iwauchi M, Horigome A, Ishikawa K, Mikuni
A, Nakano M, Xiao JZ, Odamaki T and Hironaka S: Relationship
between oral and gut microbiota in elderly people. Immun Inflamm
Dis. 7:229–236. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Odamaki T, Kato K, Sugahara H, Hashikura
N, Takahashi S, Xiao JZ, Abe F and Osawa R: Age-related changes in
gut microbiota composition from newborn to centenarian: A
cross-sectional study. BMC Microbiol. 16:902016. View Article : Google Scholar
|
|
28
|
Shaffer M and Lozupone C: Prevalence and
source of fecal and oral bacteria on infant, child, and adult
hands. mSystems. 3:e00192–17. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
De Graaf M, Beck R, Caccio SM, Duim B,
Fraaij P, Le Guyader FS, Lecuit M, Le Pendu J, de Wit E and
Schultsz C: Sustained fecal-oral human-to-human transmission
following a zoonotic event. Curr Opin Virol. 22:1–6. 2017.
View Article : Google Scholar
|
|
30
|
Bui D, Brown HE, Harris RB and Oren E:
Serologic evidence for fecal-oral transmission of Helicobacter
pylori. Am J Trop Med Hyg. 94:82–88. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bertolini M and Dongari-Bagtzoglou A: The
relationship of Candida albicans with the oral bacterial
microbiome in health and disease. Adv Exp Med Biol. 1197:69–78.
2019. View Article : Google Scholar
|
|
32
|
Acharya C, Sahingur SE and Bajaj JS:
Microbiota, cirrhosis, and the emerging oral-gut-liver axis. JCI
Insight. 2:e944162017. View Article : Google Scholar
|
|
33
|
Oikonomou T, Papatheodoridis GV, Samarkos
M, Goulis I and Cholongitas E: Clinical impact of microbiome in
patients with decompensated cirrhosis. World J Gastroenterol.
24:3813–3820. 2018. View Article : Google Scholar
|
|
34
|
Bajaj JS, Matin P, White MB, Fagan A, Deeb
JG, Acharya C, Dalmet SS, Sikaroodi M, Gillevet PM and Sahingur SE:
Periodontal therapy favorably modulates the oral-gut-hepatic axis
in cirrhosis. Am J Physiol Gastrointest Liver Physiol.
315:G824–G837. 2018. View Article : Google Scholar
|
|
35
|
Acharya C and Bajaj JS: Is it time to
spit? More evidence for the oral-gut-liver axis in liver disease.
Hepatol Int. 15:4–5. 2021. View Article : Google Scholar
|
|
36
|
Imai J, Kitamoto S and Kamada N: The
pathogenic oral-gut-liver axis: New understandings and clinical
implications. Expert Rev Clin Immunol. 17:727–736. 2021. View Article : Google Scholar
|
|
37
|
Du Teil Espina M, Gabarrini G, Harmsen
HJM, Westra J, van Winkelhoff AJ and van Dijl JM: Talk to your gut:
The oral-gut microbiome axis and its immunomodulatory role in the
etiology of rheumatoid arthritis. FEMS Microbiol Rev. 43:1–18.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lorenzo D, GianVincenzo Z, Carlo Luca R,
Karan G, Jorge V, Roberto M and Javad P: Oral-gut microbiota and
arthritis: Is there an evidence-based axis? J Clin Med. 8:2019.
|
|
39
|
Bellando-Randone S, Russo E, Venerito V,
Matucci-Cerinic M, Iannone F, Tangaro S and Amedei A: Exploring the
oral microbiome in rheumatic diseases, state of art and future
prospective in personalized medicine with an AI approach. J Pers
Med. 11:6252021. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Li BZ, Zhou HY, Guo B, Chen WJ, Tao JH,
Cao NW, Chu XJ and Meng X: Dysbiosis of oral microbiota is
associated with systemic lupus erythematosus. Arch Oral Biol.
113:1047082020. View Article : Google Scholar
|
|
41
|
Ray K: The oral-gut axis in IBD. Nat Rev
Gastroenterol Hepatol. 17:5322020. View Article : Google Scholar
|
|
42
|
Xiang Z, Koo H, Chen Q, Zhou X, Liu Y and
Simon-Soro A: Potential implications of SARS-CoV-2 oral infection
in the host microbiota. J Oral Microbiol. 13:18534512020.
View Article : Google Scholar
|
|
43
|
De Oliveira AM, Lourenço TGB and Colombo
APV: Impact of systemic probiotics as adjuncts to subgingival
instrumentation on the oral-gut microbiota associated with
periodontitis: A randomized controlled clinical trial. J
Periodontol. 93:31–44. 2022. View Article : Google Scholar
|
|
44
|
Byrd KM and Gulati AS: The ‘Gum-Gut’ axis
in inflammatory bowel diseases: A hypothesis-driven review of
associations and advances. Front Immunol. 12:6201242021. View Article : Google Scholar
|
|
45
|
Narengaowa, Kong W, Lan F, Awan UF, Qing H
and Ni J: The oral-gut-brain axis: The influence of microbes in
Alzheimer's disease. Front Cell Neurosci. 15:6337352021. View Article : Google Scholar
|
|
46
|
Yamashita Y and Takeshita T: The oral
microbiome and human health. J Oral Sci. 59:201–206. 2017.
View Article : Google Scholar
|
|
47
|
Kilian M, Chapple IL, Hannig M, Marsh PD,
Meuric V, Pedersen AM, Tonetti MS, Wade WG and Zaura E: The oral
microbiome-an update for oral healthcare professionals. Br Dent J.
221:657–666. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zarco MF, Vess TJ and Ginsburg GS: The
oral microbiome in health and disease and the potential impact on
personalized dental medicine. Oral Dis. 18:109–120. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Gao L, Xu T, Huang G, Jiang S, Gu Y and
Chen F: Oral microbiomes: More and more importance in oral cavity
and whole body. Protein Cell. 9:488–500. 2018. View Article : Google Scholar
|
|
50
|
Wade WG: The oral microbiome in health and
disease. Pharmacol Res. 69:137–143. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Flemer B, Warren RD, Barrett MP, Cisek K,
Das A, Jeffery IB, Hurley E, O'Riordain M, Shanahan F and O'Toole
PW: The oral microbiota in colorectal cancer is distinctive and
predictive. Gut. 67:1454–1463. 2018. View Article : Google Scholar
|
|
52
|
Gaiser RA, Halimi A, Alkharaan H, Lu L,
Davanian H, Healy K, Hugerth LW, Ateeb Z, Valente R, Fernández Moro
C, et al: Enrichment of oral microbiota in early cystic precursors
to invasive pancreatic cancer. Gut. 68:2186–2194. 2019. View Article : Google Scholar
|
|
53
|
Kitamoto S, Nagao-Kitamoto H, Jiao Y,
Gillilland MG III, Hayashi A, Imai J, Sugihara K, Miyoshi M, Brazil
JC, Kuffa P, et al: The intermucosal connection between the mouth
and gut in commensal pathobiont-driven colitis. Cell.
182:447–462.e14. 2020. View Article : Google Scholar
|
|
54
|
Bullman S, Pedamallu CS, Sicinska E,
Clancy TE, Zhang X, Cai D, Neuberg D, Huang K, Guevara F, Nelson T,
et al: Analysis of Fusobacterium persistence and antibiotic
response in colorectal cancer. Science. 358:1443–1448. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Casasanta MA, Yoo CC, Udayasuryan B,
Sanders BE, Umaña A, Zhang Y, Peng H, Duncan AJ, Wang Y, Li L, et
al: Fusobacterium nucleatum host-cell binding and invasion
induces IL-8 and CXCL1 secretion that drives colorectal cancer cell
migration. Sci Signal. 13:eaba91572020. View Article : Google Scholar
|
|
56
|
Brennan CA and Garrett WS:
Fusobacterium nucleatum-symbiont, opportunist and
oncobacterium. Nat Rev Microbiol. 17:156–166. 2019. View Article : Google Scholar
|
|
57
|
Gopalakrishnan V, Helmink BA, Spencer CN,
Reuben A and Wargo JA: The influence of the gut microbiome on
cancer, immunity, and cancer immunotherapy. Cancer Cell.
33:570–580. 2018. View Article : Google Scholar
|
|
58
|
Wei Z, Cao S, Liu S, Yao Z, Sun T, Li Y,
Li J, Zhang D and Zhou Y: Could gut microbiota serve as prognostic
biomarker associated with colorectal cancer patients' survival? A
pilot study on relevant mechanism. Oncotarget. 7:46158–46172. 2016.
View Article : Google Scholar
|
|
59
|
Rubinstein MR, Wang X, Liu W, Hao Y, Cai G
and Han YW: Fusobacterium nucleatum promotes colorectal
carcinogenesis by modulating E-cadherin/β-catenin signaling via its
FadA adhesin. Cell Host Microbe. 14:195–206. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Kostic AD, Chun E, Robertson L, Glickman
JN, Gallini CA, Michaud M, Clancy TE, Chung DC, Lochhead P, Hold
GL, et al: Fusobacterium nucleatum potentiates intestinal
tumorigenesis and modulates the tumor-immune microenvironment. Cell
Host Microbe. 14:207–215. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Arumugam M, Raes J, Pelletier E, Le
Paslier D, Yamada T, Mende DR, Fernandes GR, Tap J, Bruls T, Batto
JM, et al: Enterotypes of the human gut microbiome. Nature.
473:174–180. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Chong ES: A potential role of probiotics
in colorectal cancer prevention: Review of possible mechanisms of
action. World J Microbiol Biotechnol. 30:351–374. 2014. View Article : Google Scholar
|
|
63
|
Biedermann L and Rogler G: The intestinal
microbiota: Its role in health and disease. Eur J Pediatr.
174:151–167. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Arthur JC, Perez-Chanona E, Mühlbauer M,
Tomkovich S, Uronis JM, Fan TJ, Campbell BJ, Abujamel T, Dogan B,
Rogers AB, et al: Intestinal inflammation targets cancer-inducing
activity of the microbiota. Science. 338:120–123. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ray K: IBD. Gut microbiota in IBD goes
viral. Nat Rev Gastroenterol Hepatol. 12:1222015. View Article : Google Scholar
|
|
66
|
Raisch J, Rolhion N, Dubois A,
Darfeuille-Michaud A and Bringer MA: Intracellular colon
cancer-associated Escherichia coli promote protumoral
activities of human macrophages by inducing sustained COX-2
expression. Lab Invest. 95:296–307. 2015. View Article : Google Scholar
|
|
67
|
Gagnière J, Raisch J, Veziant J, Barnich
N, Bonnet R, Buc E, Bringer MA, Pezet D and Bonnet M: Gut
microbiota imbalance and colorectal cancer. World J Gastroenterol.
22:501–518. 2016. View Article : Google Scholar
|
|
68
|
Rossi M, Mirbagheri SEYEDS, Keshavarzian A
and Bishehsari F: Nutraceuticals in colorectal cancer: A
mechanistic approach. Eur J Pharmacol. 833:396–402. 2018.
View Article : Google Scholar
|
|
69
|
Li Q, Ding C, Meng T, Lu W, Liu W, Hao H
and Cao L: Butyrate suppresses motility of colorectal cancer cells
via deactivating Akt/ERK signaling in histone deacetylase dependent
manner. J Pharmacol Sci. 135:148–155. 2017. View Article : Google Scholar
|
|
70
|
de Martel C, Ferlay J, Franceschi S,
Vignat J, Bray F, Forman D and Plummer M: Global burden of cancers
attributable to infections in 2008: A review and synthetic
analysis. Lancet Oncol. 13:607–615. 2012. View Article : Google Scholar
|
|
71
|
Yu L, Ge S, Feng X, et al: Research
progress of Porphyromonas gingivalis. J Prev Treat Stomatol
Dis. 05:314–317. 2016.https://t.cnki.net/kcms/detail?v=3uoqIhG8C44YLTlOAiTRKgchrJ08w1e7bFPagIuZu8mSNNqTzqA10SmLmWs9SCrXF-1zbj6qv97WC8n64gYCrTahio_5NDeO&uniplatform=NZKPT&uid=WEEvREdxOWJmbC9oM1NjYkcyTjdROWp3THN6dy9lNCtTTG4zd1MwcFFNeDg=$R1yZ0H6jyaa0en3RxVUd8df-oHi7XMMDo7mtKT6mSmEvTuk11l2gFA!!
|
|
72
|
Zhao L: Discussion on the treatment of
extraintestinal symptoms and complications in patients with
inflammatory bowel disease. Clin Res Pract. 2:142–143. 2017.
|
|
73
|
Barton MK: Evidence accumulates indicating
periodontal disease as a risk factor for colorectal cancer or
lymphoma. CA Cancer J Clin. 67:173–174. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Yang Y, Weng W, Peng J, Hong L, Yang L,
Toiyama Y, Gao R, Liu M, Yin M, Pan C, et al: Fusobacterium
nucleatum increases proliferation of colorectal cancer cells
and tumor development in mice by activating Toll-like receptor 4
signaling to nuclear factor-κB, and up-regulating expression of
MicroRNA-21. Gastroenterology. 152:851–866.e24. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Yamaoka Y, Suehiro Y, Hashimoto S, Hoshida
T, Fujimoto M, Watanabe M, Imanaga D, Sakai K, Matsumoto T,
Nishioka M, et al: Fusobacterium nucleatum as a prognostic
marker of colorectal cancer in a Japanese population. J
Gastroenterol. 53:517–524. 2018. View Article : Google Scholar
|
|
76
|
Yang CY, Yeh YM, Yu HY, Chin CY, Hsu CW,
Liu H, Huang PJ, Hu SN, Liao CT, Chang KP and Chang YL: Oral
microbiota community dynamics associated with oral squamous cell
carcinoma staging. Front Microbiol. 9:8622018. View Article : Google Scholar
|