|
1
|
Olawaiye AB, Cuello MA and Rogers LJ:
Cancer of the vulva: 2021 update. Int J Gynaecol Obstet. 155 (Suppl
1):7–18. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rogers LJ and Cuello MA: Cancer of the
vulva. Int J Gynaecol Obstet. 143 (Suppl 2):S4–S13. 2018.
View Article : Google Scholar
|
|
3
|
Alkatout I, Schubert M, Garbrecht N,
Weigel MT, Jonat W, Mundhenke C and Günther V: Vulvar cancer:
Epidemiology, clinical presentation, and management options. Int J
Womens Health. 7:305–313. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Capria A, Tahir N and Fatehi M: Vulva
Cancer. StatPearls. StatPearls Publishing; Treasure Island, FL:
2024, PubMed/NCBI
|
|
5
|
Bucchi L, Pizzato M, Rosso S and Ferretti
S: New insights into the epidemiology of vulvar cancer: Systematic
literature review for an update of incidence and risk factors.
Cancers (Basel). 14:3892022. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brinton LA, Thistle JE, Liao LM and
Trabert B: Epidemiology of vulvar neoplasia in the NIH-AARP Study.
Gynecol Oncol. 145:298–304. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gadducci A, Tana R, Barsotti C, Guerrieri
ME and Genazzani AR: Clinico-pathological and biological prognostic
variables in squamous cell carcinoma of the vulva. Crit Rev Oncol
Hematol. 83:71–83. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dongre HN, Elnour R, Tornaas S, Fromreide
S, Thomsen LCV, Kolseth IBM, Nginamau ES, Johannessen AC, Vintermyr
OK, Costea DE and Bjørge L: TP53 mutation and human papilloma virus
status as independent prognostic factors in a Norwegian cohort of
vulva squamous cell carcinoma. Acta Obstet Gynecol Scand.
103:165–175. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
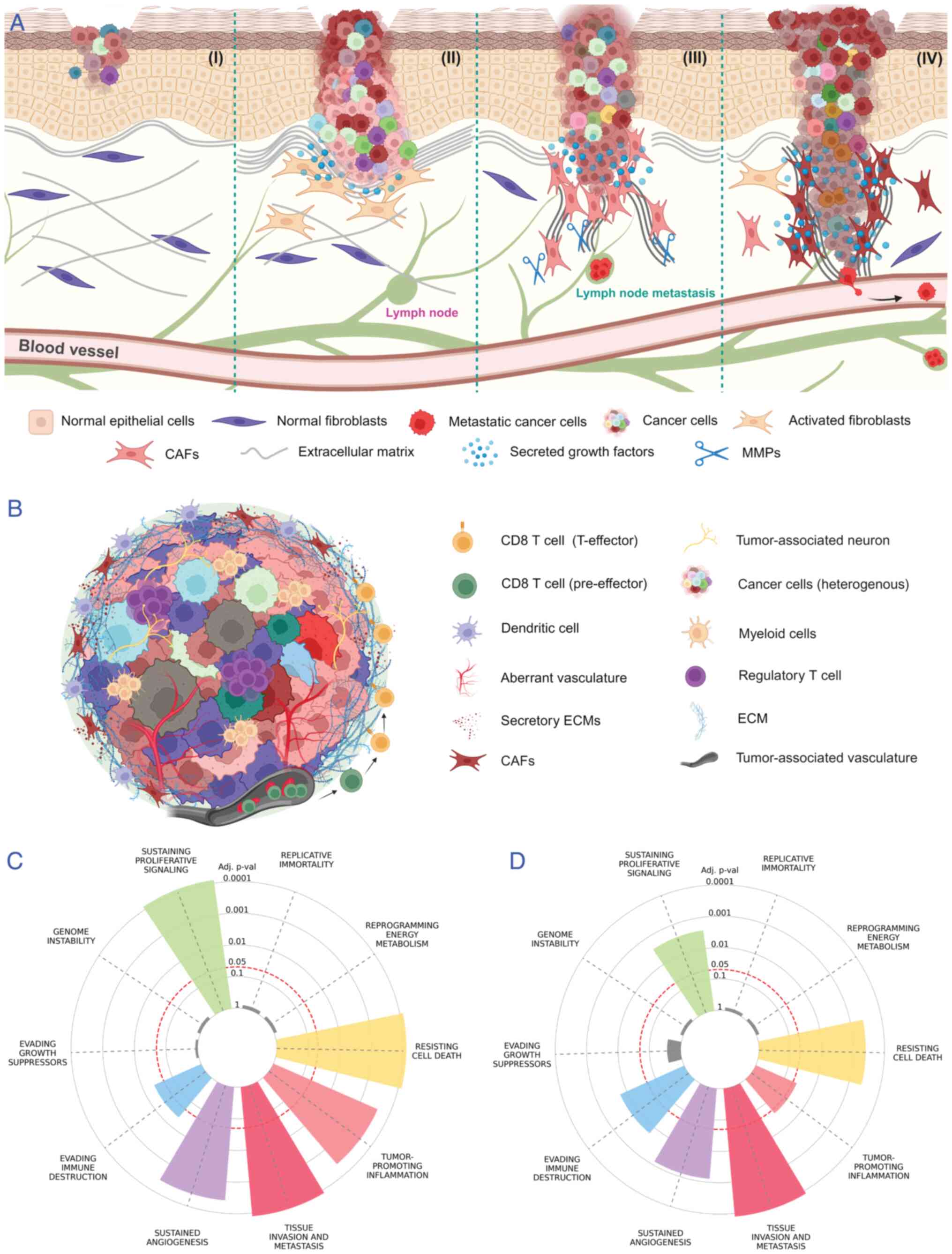
Dongre H and Costea DE: Tumor-Fibroblast
Interactions in CarcinomasBiomarkers of the Tumor Microenvironment.
Springer; New York, NY: pp. 109–124. 2022, View Article : Google Scholar
|
|
10
|
Dzobo K and Dandara C: The Extracellular
Matrix: Its composition, function, remodeling, and role in
tumorigenesis. Biomimetics (Basel). 8:1462023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pappa KI, Jacob-Hirsch J, Vlachos GD,
Christodoulou I, Partsinevelos G, Amariglio N, Markaki S, Antsaklis
A and Anagnou NP: Expression profiling of vulvar carcinoma: clues
for deranged extracellular matrix remodeling and effects on
multiple signaling pathways combined with discrete patient subsets.
Transl Oncol. 4:301–313. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sleeboom JJF, van Tienderen GS,
Schenke-Layland K, van der Laan LJW, Khalil AA and Verstegen MMA:
The extracellular matrix as hallmark of cancer and metastasis: From
biomechanics to therapeutic targets. Sci Transl Med.
16:eadg38402024. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mukherjee A and Bravo-Cordero JJ:
Regulation of dormancy during tumor dissemination: the role of the
ECM. Cancer Metastasis Rev. 42:99–112. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Popova NV and Jücker M: The functional
role of extracellular matrix proteins in cancer. Cancers (Basel).
14:2382022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Walker C, Mojares E and Del Río Hernández
A: Role of extracellular matrix in development and cancer
progression. Int J Mol Sci. 19:30282018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yue B: Biology of the extracellular
matrix: An overview. J Glaucoma. 23 (8 Suppl 1):S20–S23. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Condic M, Rohr A, Riemann S, Staerk C,
Ayub TH, Doeser A, Zillinger T, Merkelbach-Bruse S, Buettner R,
Barchet W, et al: Immune profiling of vulvar squamous cell cancer
discovers a macrophage-rich subtype associated with poor prognosis.
Cancer Res Commun. 4:861–875. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
van Esch EM, van Poelgeest MI, Trimbos JB,
Fleuren GJ, Jordanova ES and van der Burg SH: Intraepithelial
macrophage infiltration is related to a high number of regulatory T
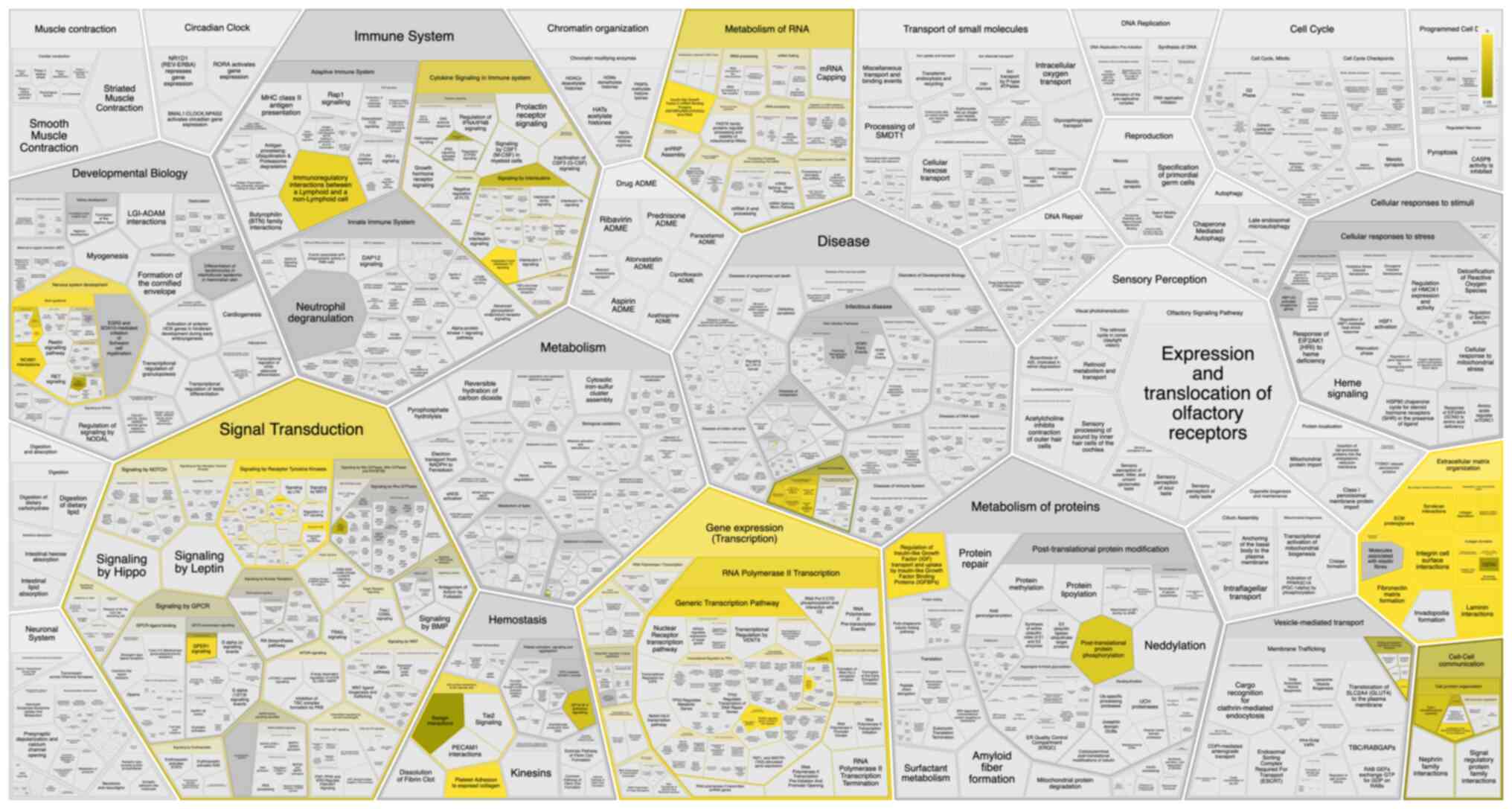
cells and promotes a progressive course of HPV-induced vulvar
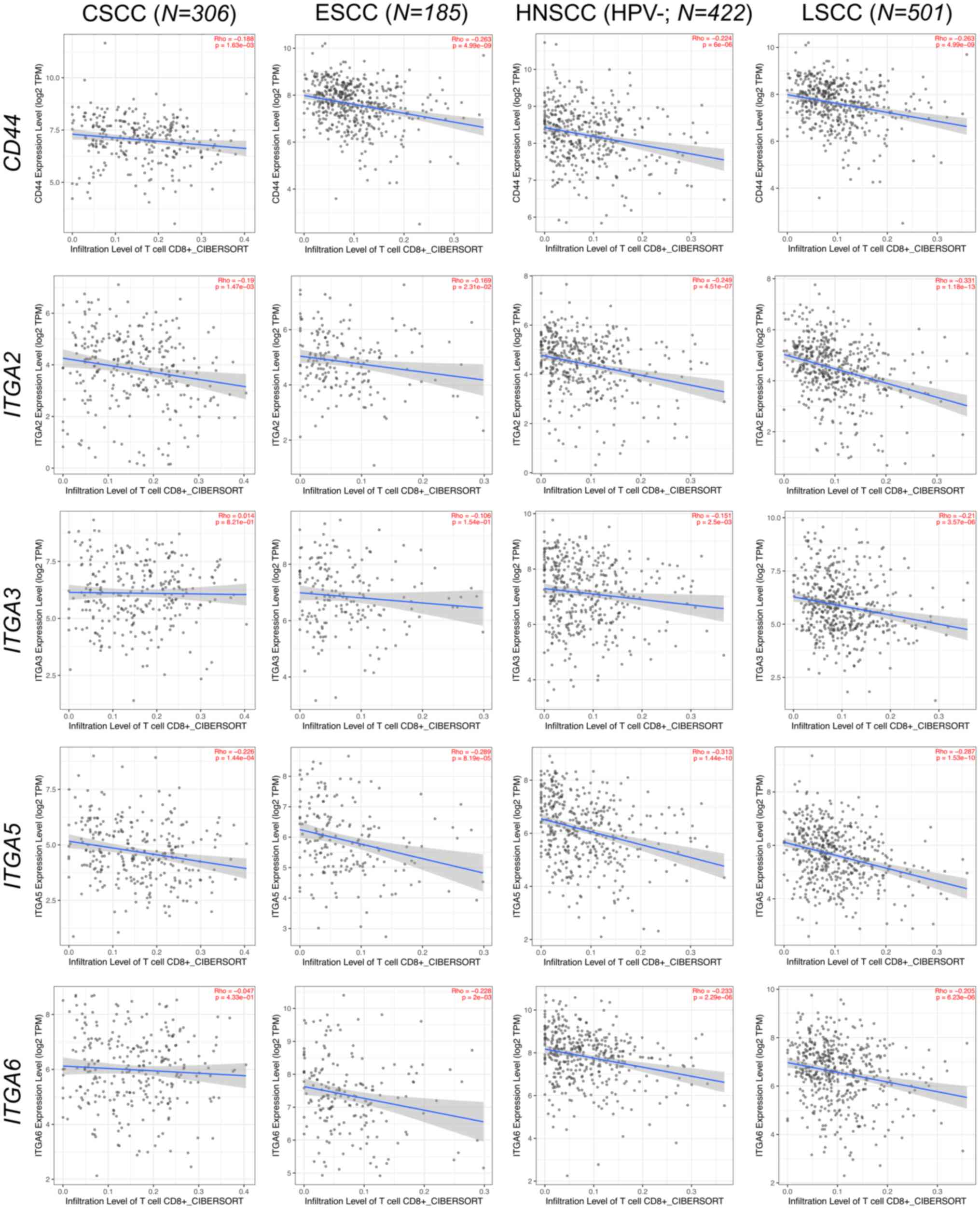
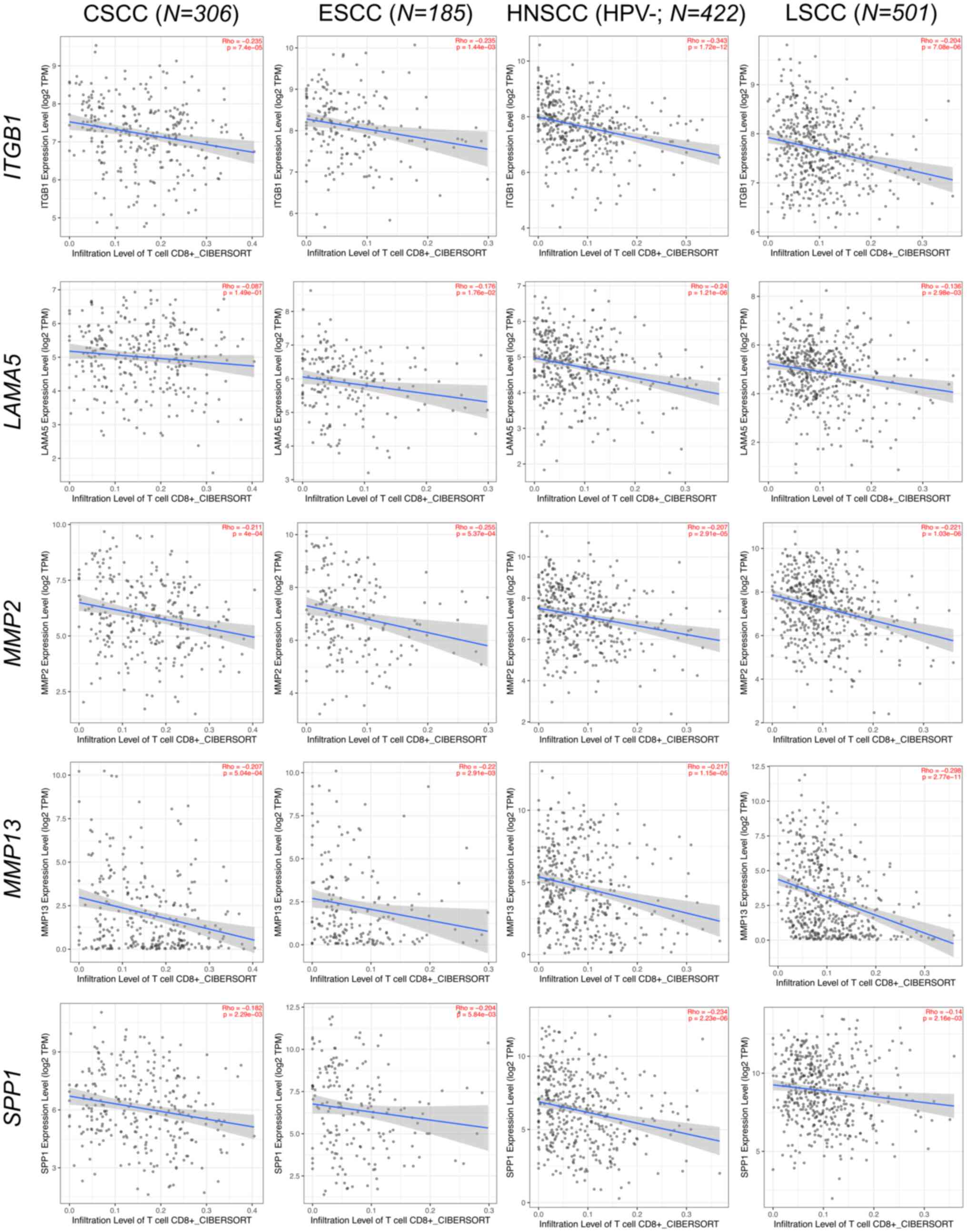
neoplasia. Int J Cancer. 136:E85–E94. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bruni S, Mercogliano MF, Mauro FL, Cordo
Russo RI and Schillaci R: Cancer immune exclusion: breaking the
barricade for a successful immunotherapy. Front Oncol.
13:11354562023. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li L, Wei JR, Dong J, Lin QG, Tang H, Jia
YX, Tan W, Chen QY, Zeng TT, Xing S, et al: Laminin γ2-mediating T
cell exclusion attenuates response to anti-PD-1 therapy. Sci Adv.
7:eabc83462021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang W, Huang X, Huang R, Zhu H, Ye P,
Lin X, Zhang S, Wu M and Jiang F: MMP1 overexpression promotes
cancer progression and associates with poor outcome in head and
neck carcinoma. Comput Math Methods Med.
2022:30583422022.PubMed/NCBI
|
|
22
|
Liu M, Hu Y, Zhang MF, Luo KJ, Xie XY, Wen
J, Fu JH and Yang H: MMP1 promotes tumor growth and metastasis in
esophageal squamous cell carcinoma. Cancer Lett. 377:97–104. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kurnia I, Rauf S, Hatta M, Arifuddin S,
Hidayat YM, Natzir R, Kaelan C, Bukhari A, Pelupessy NU and
Patelonggi IJ: Molecular Patho-mechanisms of cervical cancer
(MMP1). Ann Med Surg (Lond). 77:1034152022.PubMed/NCBI
|
|
24
|
Han L, Sheng B, Zeng Q, Yao W and Jiang Q:
Correlation between MMP2 expression in lung cancer tissues and
clinical parameters: A retrospective clinical analysis. BMC Pulm
Med. 20:2832020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Samantaray S, Sharma R, Chattopadhyaya TK,
Gupta SD and Ralhan R: Increased expression of MMP-2 and MMP-9 in
esophageal squamous cell carcinoma. J Cancer Res Clin Oncol.
130:37–44. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Azevedo Martins JM, Rabelo-Santos SH, do
Amaral Westin MC and Zeferino LC: Tumoral and stromal expression of
MMP-2, MMP-9, MMP-14, TIMP-1, TIMP-2, and VEGF-A in cervical cancer
patient survival: A competing risk analysis. BMC Cancer.
20:6602020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li H, Yang F, Chai L, Zhang L, Li S, Xu Z
and Kong L: CCAAT/Enhancer Binding Protein β-Mediated MMP3
upregulation promotes esophageal squamous cell cancer invasion in
vitro and is associated with metastasis in human patients. Genet
Test Mol Biomarkers. 23:304–309. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gkouveris I, Nikitakis NG, Aseervatham J,
Rao N and Ogbureke KUE: Matrix metalloproteinases in head and neck
cancer: Current perspectives. Metalloproteinases Med. 4:47–61.
2017. View Article : Google Scholar
|
|
29
|
Shao L, Wang X, Liu W, Zhang C, Ma W, Yu X
and Han J: The role and function of secretory protein MMP3 in
cervical cancer. researchsquare. https://doi.org/10.21203/rs.3.rs-2449297/v1
|
|
30
|
Liu D, Nakano J, Ishikawa S, Yokomise H,
Ueno M, Kadota K, Urushihara M and Huang CL: Overexpression of
matrix metalloproteinase-7 (MMP-7) correlates with tumor
proliferation, and a poor prognosis in non-small cell lung cancer.
Lung Cancer. 58:384–391. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chuang HC, Su CY, Huang HY, Huang CC,
Chien CY, Du YY and Chuang JH: Active matrix metalloproteinase-7 is
associated with invasion in buccal squamous cell carcinoma. Mod
Pathol. 21:1444–1450. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhu L, Zheng X, Du Y, Xing Y, Xu K and Cui
L: Matrix metalloproteinase-7 may serve as a novel biomarker for
cervical cancer. Onco Targets Ther. 11:4207–4220. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Li Y, Ma J, Guo Q, Duan F, Tang F, Zheng
P, Zhao Z and Lu G: Overexpression of MMP-2 and MMP-9 in esophageal
squamous cell carcinoma. Dis Esophagus. 22:664–667. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tsukamoto S, Koma YI, Kitamura Y, Tanigawa
K, Azumi Y, Miyako S, Urakami S, Hosono M, Kodama T, Nishio M, et
al: Matrix metalloproteinase 9 induced in esophageal squamous cell
carcinoma cells via close contact with tumor-associated macrophages
contributes to cancer progression and poor prognosis. Cancers
(Basel). 15:29872023. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Deraz EM, Kudo Y, Yoshida M, Obayashi M,
Tsunematsu T, Tani H, Siriwardena SB, Keikhaee MR, Qi G, Iizuka S,
et al: MMP-10/stromelysin-2 promotes invasion of head and neck
cancer. PLoS One. 6:e254382011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liu H, Qin YR, Bi J, Guo A, Fu L and Guan
XY: Overexpression of matrix metalloproteinase 10 is associated
with poor survival in patients with early stage of esophageal
squamous cell carcinoma. Dis Esophagus. 25:656–663. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhang G, Miyake M, Lawton A, Goodison S
and Rosser CJ: Matrix metalloproteinase-10 promotes tumor
progression through regulation of angiogenic and apoptotic pathways
in cervical tumors. BMC Cancer. 14:3102014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ma B, Ran R, Liao HY and Zhang HH: The
paradoxical role of matrix metalloproteinase-11 in cancer. Biomed
Pharmacother. 141:1118992021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hsin CH, Chou YE, Yang SF, Su SC, Chuang
YT, Lin SH and Lin CW: MMP-11 promoted the oral cancer migration
and Fak/Src activation. Oncotarget. 8:32783–32793. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lv FZ, Wang JL, Wu Y, Chen HF and Shen XY:
Knockdown of MMP12 inhibits the growth and invasion of lung
adenocarcinoma cells. Int J Immunopathol Pharmacol. 28:77–84. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kim JM, Kim HJ, Koo BS, Rha KS and Yoon
YH: Expression of matrix metalloproteinase-12 is correlated with
extracapsular spread of tumor from nodes with metastasis in head
and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol.
270:1137–1142. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Han F, Zhang S, Zhang L and Hao Q: The
overexpression and predictive significance of MMP-12 in esophageal
squamous cell carcinoma. Pathol Res Pract. 213:1519–1522. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kudo Y, Iizuka S, Yoshida M, Tsunematsu T,
Kondo T, Subarnbhesaj A, Deraz EM, Siriwardena SB, Tahara H,
Ishimaru N, et al: Matrix metalloproteinase-13 (MMP-13) directly
and indirectly promotes tumor angiogenesis. J Biol Chem.
287:38716–38728. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Jiao XL, Chen D, Wang JG and Zhang KJ:
Clinical significance of serum matrix metalloproteinase-13 levels
in patients with esophageal squamous cell carcinoma (ESCC). Eur Rev
Med Pharmacol Sci. 18:509–515. 2014.PubMed/NCBI
|
|
45
|
Zheng Cl, Lu Q, Zhang N, Jing PY, Zhang
JP, Wang WP and Li GZ: Comprehensive analysis of the immune and
prognostic implication of MMP14 in lung cancer. Dis Markers.
2021:59175062021. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kurahara S, Shinohara M, Ikebe T, Nakamura
S, Beppu M, Hiraki A, Takeuchi H and Shirasuna K: Expression of
MMPS, MT-MMP, and TIMPs in squamous cell carcinoma of the oral
cavity: Correlations with tumor invasion and metastasis. Head Neck.
21:627–638. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang H, Zhang Y, Zhang Y, Liu W and Wang
J: Cryptotanshinone inhibits lung cancer invasion via
microRNA-133a/matrix metalloproteinase 14 regulation. Oncol Lett.
18:2554–2559. 2019.PubMed/NCBI
|
|
48
|
Chen N, Zhang G, Fu J and Wu Q: Matrix
metalloproteinase-14 (MMP-14) downregulation inhibits esophageal
squamous cell carcinoma cell migration, invasion, and
proliferation. Thorac Cancer. 11:3168–3174. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Li M, Li S, Zhou L, Yang L, Wu X, Tang B,
Xie S, Fang L, Zheng S and Hong T: Immune Infiltration of MMP14 in
pan cancer and its prognostic effect on tumors. Front Oncol.
11:7176062021. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Fan QC, Tian H, Wang Y and Liu XB:
Integrin-α5 promoted the progression of oral squamous cell
carcinoma and modulated PI3K/AKT signaling pathway. Arch Oral Biol.
101:85–91. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Park SJ, Min HJ, Yoon C, Kim SH, Kim JH
and Lee SY: Integrin β1 regulates the perineural invasion and
radioresistance of oral squamous carcinoma cells by modulating
cancer cell stemness. Cell Signal. 110:1108082023. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Ramos DM, But M, Regezi J, Schmidt BL,
Atakilit A, Dang D, Ellis D, Jordan R and Li X: Expression of
integrin beta 6 enhances invasive behavior in oral squamous cell
carcinoma. Matrix Biol. 21:297–307. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Ishida Y, Shintani T, Nobumoto T, Sakurai
S, Hamana T, Yanamoto S and Hayashido Y: Interaction of Integrin
αvβ8 With Type I collagen promotes squamous cell carcinoma cell
motility via RAC1 activation. Anticancer Res. 43:4833–4841. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Thomas GJ, Jones J and Speight PM:
Integrins and oral cancer. Oral Oncol. 33:381–388. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hou S, Hao X, Li J, Weng S, Wang J, Zhao
T, Li W, Hu X, Deng B, Gu J and Hang Q: TM4SF1 promotes esophageal
squamous cell carcinoma metastasis by interacting with integrin α6.
Cell Death Dis. 13:6092022. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Xie YH, Ran LQ, Wu ZY, Sun C, Xu XE, Zou
HY, Fang WK and Xie JJ: Role of Integrin β1 in the progression and
chemo-resistance of esophageal squamous cell carcinoma. J Cancer.
13:2074–2085. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Xie JJ, Guo JC, Wu ZY, Xu XE, Wu JY, Chen
B, Ran LQ, Liao LD, Li EM and Xu LY: Integrin α5 promotes tumor
progression and is an independent unfavorable prognostic factor in
esophageal squamous cell carcinoma. Hum Pathol. 48:69–75. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Dmello C, Sawant S, Alam H, Gangadaran P,
Tiwari R, Dongre H, Rana N, Barve S, Costea DE, Chaukar D, et al:
Vimentin-mediated regulation of cell motility through modulation of
beta4 integrin protein levels in oral tumor derived cells. Int J
Biochem Cell Biol. 70:161–172. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Liu S, Liao G and Li G: Regulatory effects
of COL1A1 on apoptosis induced by radiation in cervical cancer
cells. Cancer Cell Int. 17:732017. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Geng Q, Shen Z, Li L and Zhao J: COL1A1 is
a prognostic biomarker and correlated with immune infiltrates in
lung cancer. PeerJ. 9:e111452021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Lin P, Tian P, Pang J, Lai L, He G, Song Y
and Zheng Y: Clinical significance of COL1A1 and COL1A2 expression
levels in hypopharyngeal squamous cell carcinoma. Oncol Lett.
20:803–809. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Li G, Jiang W, Kang Y, Yu X, Zhang C and
Feng Y: High expression of collagen 1A2 promotes the proliferation
and metastasis of esophageal cancer cells. Ann Transl Med.
8:16722020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Shen Y, Li X, Wang D, Zhang L, Li X, Su L,
Fan X and Yang X: COL3A1: Potential prognostic predictor for head
and neck cancer based on immune-microenvironment alternative
splicing. Cancer Med. 12:4882–4894. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Tian X, Sun J, Li C and Zhang K: COL4A1
promotes the proliferation and migration of oral squamous cell
carcinoma cells by binding to NID1. Exp Ther Med. 25:1762023.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Di YB, Bao Y, Guo J, Liu W, Zhang SX,
Zhang GH and Li TK: COL11A1 as a potential prognostic target for
oral squamous cell carcinoma. Medicine (Baltimore). 101:e309892022.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Sok JC, Lee JA, Dasari S, Joyce S,
Contrucci SC, Egloff AM, Trevelline BK, Joshi R, Kumari N, Grandis
JR and Thomas SM: Collagen type XI α1 facilitates head and neck
squamous cell cancer growth and invasion. Br J Cancer.
109:3049–3056. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Galiger C, Löffek S, Stemmler MP, Kroeger
JK, Mittapalli VR, Fauth L, Esser PR, Kern JS, Meiss F, Laßmann S,
et al: Targeting of cell surface proteolysis of collagen XVII
impedes squamous cell carcinoma progression. Mol Ther. 26:17–30.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Liu L, Jung SN, Oh C, Lee K, Won HR, Chang
JW, Kim JM and Koo BS: LAMB3 is associated with disease progression
and cisplatin cytotoxic sensitivity in head and neck squamous cell
carcinoma. Eur J Surg Oncol. 45:359–365. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Marangon Junior H, Rocha VN, Leite CF, de
Aguiar MC, Souza PE and Horta MC: Laminin-5 gamma 2 chain
expression is associated with intensity of tumor budding and
density of stromal myofibroblasts in oral squamous cell carcinoma.
J Oral Pathol Med. 43:199–204. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Chen J, Zhou J, Lu J, Xiong H, Shi X and
Gong L: Significance of CD44 expression in head and neck cancer: A
systemic review and meta-analysis. BMC Cancer. 14:152014.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Mirhashemi M, Sadeghi M, Ghazi N,
Saghravanian N, Dehghani M and Aminian A: Prognostic value of CD44
expression in oral squamous cell carcinoma: A meta-analysis. Ann
Diagn Pathol. 67:1522132023. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Sawant S, Ahire C, Dongre H, Joshi S,
Jamghare S, Rane P, Kane S and Chaukar D: Prognostic significance
of elevated serum CD44 levels in patients with oral squamous cell
carcinoma. J Oral Pathol Med. 47:665–673. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Kudo Y, Ogawa I, Kitajima S, Kitagawa M,
Kawai H, Gaffney PM, Miyauchi M and Takata T: Periostin promotes
invasion and anchorage-independent growth in the metastatic process
of head and neck cancer. Cancer Res. 66:6928–6935. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Maleš J, Mihalj H, Šestak A, Kralik K and
Smolić M: Osteopontin levels in patients with squamous metastatic
head and neck cancer. Medicina (Kaunas). 57:1852021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Li J, Wang X, Zheng K, Liu Y, Li J and
Wang S, Liu K, Song X, Li N, Xie S and Wang S: The clinical
significance of collagen family gene expression in esophageal
squamous cell carcinoma. PeerJ. 7:e77052019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Zhou J, Yang Y, Zhang H, Luan S, Xiao X,
Li X, Fang P, Shang Q, Chen L, Zeng X and Yuan Y: Overexpressed
COL3A1 has prognostic value in human esophageal squamous cell
carcinoma and promotes the aggressiveness of esophageal squamous
cell carcinoma by activating the NF-κB pathway. Biochem Biophys Res
Commun. 613:193–200. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Zhang B, Zhang C, Yang X, Chen Y, Zhang H,
Liu J and Wu Q: Cytoplasmic collagen XIαI as a prognostic biomarker
in esophageal squamous cell carcinoma. Cancer Biol Ther.
19:364–372. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Meng X, Chen X, Lu P, Ma W, Yue D, Song L
and Fan Q: MicroRNA-202 inhibits tumor progression by targeting
LAMA1 in esophageal squamous cell carcinoma. Biochem Biophys Res
Commun. 473:821–827. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Shen XM, Wu YP, Feng YB, Luo ML, Du XL,
Zhang Y, Cai Y, Xu X, Han YL, Zhang X, et al: Interaction of
MT1-MMP and laminin-5gamma2 chain correlates with metastasis and
invasiveness in human esophageal squamous cell carcinoma. Clin Exp
Metastasis. 24:541–550. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Liang Y, Chen X, Wu Y, Li J, Zhang S, Wang
K, Guan X, Yang K and Bai Y: LncRNA CASC9 promotes esophageal
squamous cell carcinoma metastasis through upregulating LAMC2
expression by interacting with the CREB-binding protein. Cell Death
Differ. 25:1980–1995. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Fang L, Che Y, Zhang C, Huang J, Lei Y, Lu
Z, Sun N and He J: LAMC1 upregulation via TGFβ induces inflammatory
cancer-associated fibroblasts in esophageal squamous cell carcinoma
via NF-κB-CXCL1-STAT3. Mol Oncol. 15:3125–3146. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Kamil Mohammed Al-Mosawi A, Cheshomi H,
Hosseinzadeh A and M Matin M: Prognostic and Clinical Value of CD44
and CD133 in Esophageal Cancer: A Systematic Review and
Meta-analysis. Iran J Allergy Asthma Immunol. 19:105–116.
2020.PubMed/NCBI
|
|
83
|
Miyako S, Koma YI, Nakanishi T, Tsukamoto
S, Yamanaka K, Ishihara N, Azumi Y, Urakami S, Shimizu M, Kodama T,
et al: Periostin in cancer-associated fibroblasts promotes
esophageal squamous cell carcinoma progression by enhancing cancer
and stromal cell migration. Am J Pathol. 194:828–848. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Chen B, Liang S, Guo H, Xu L, Li J and
Peng J: OPN promotes cell proliferation and invasion through NF-κB
in human esophageal squamous cell carcinoma. Genet Res (Camb).
2022:31548272022. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Chiu TJ, Lu HI, Chen CH, Huang WT, Wang
YM, Lin WC and Li SH: Osteopontin expression is associated with the
poor prognosis in patients with locally advanced esophageal
squamous cell carcinoma receiving preoperative chemoradiotherapy.
Biomed Res Int. 2018:90982152018. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Duan Y, Liu G, Sun Y, Wu J, Xiong Z, Jin T
and Chen M: Collagen type VI α5 gene variations may predict the
risk of lung cancer development in Chinese Han population. Sci Rep.
10:50102020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Wang L, Sun Y, Guo Z and Liu H: COL3A1
overexpression associates with poor prognosis and cisplatin
resistance in lung cancer. Balkan Med J. 39:393–400. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Voiles L, Lewis DE, Han L, Lupov IP, Lin
TL, Robertson MJ, Petrache I and Chang HC: Overexpression of type
VI collagen in neoplastic lung tissues. Oncol Rep. 32:1897–1904.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Lee CS, Siprashvili Z, Mah A, Bencomo T,
Elcavage LE, Che Y, Shenoy RM, Aasi SZ and Khavari PA: Mutant
collagen COL11A1 enhances cancerous invasion. Oncogene.
40:6299–6307. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Liu M, Cai R, Wang T, Yang X, Wang M,
Kuang Z, Xie Y, Zhang J and Zheng Y: LAMC2 promotes the
proliferation of cancer cells and induce infiltration of
macrophages in non-small cell lung cancer. Ann Transl Med.
9:13922021. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Akashi T, Ito E, Eishi Y, Koike M,
Nakamura K and Burgeson RE: Reduced Expression of Laminin alpha3
and alpha5 Chains in Non-small Cell Lung Cancers. Jpn J Cancer Res.
92:293–301. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Rousselle P and Scoazec JY: Laminin 332 in
cancer: When the extracellular matrix turns signals from cell
anchorage to cell movement. Semin Cancer Biol. 62:149–165. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Jiang H, Zhao W and Shao W: Prognostic
value of CD44 and CD44v6 expression in patients with non-small cell
lung cancer: meta-analysis. Tumour Biol. 35:7383–7389. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Xu CH, Wang W, Lin Y, Qian LH, Zhang XW,
Wang QB and Yu LK: Diagnostic and prognostic value of serum
periostin in patients with non-small cell lung cancer. Oncotarget.
8:18746–18753. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Wang W, Wang S and Zhang M: Evaluation of
kininogen 1, osteopontin and α-1-antitrypsin in plasma,
bronchoalveolar lavage fluid and urine for lung squamous cell
carcinoma diagnosis. Oncol Lett. 19:2785–2792. 2020.PubMed/NCBI
|
|
96
|
Hou T, Tong C, Kazobinka G, Zhang W, Huang
X, Huang Y and Zhang Y: Expression of COL6A1 predicts prognosis in
cervical cancer patients. Am J Transl Res. 8:2838–2844.
2016.PubMed/NCBI
|
|
97
|
Skyldberg B, Salo S, Eriksson E, Aspenblad
U, Moberger B, Tryggvason K and Auer G: Laminin-5 as a Marker of
Invasiveness in Cervical Lesions. J Natl Cancer Inst. 91:1882–1887.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Noel JC, Fernandez-Aguilar S, Fayt I,
Buxant F, Ansion MH, Simon P and Anaf V: Laminin-5γ2 chain
expression in cervical intraepithelial neoplasia and invasive
cervical carcinoma. Acta Obstet Gynecol Scand. 84:1119–1123. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Kainz C, Kohlberger P, Tempfer C, Sliutz
G, Gitsch G, Reinthaller A and Breitenecker G: Prognostic value of
CD44 splice variants in human stage III cervical cancer. Eur J
Cancer. 31:1706–1709. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Wei WF, Chen XJ, Liang LJ, Yu L, Wu XG,
Zhou CF, Wang ZC, Fan LS, Hu Z, Liang L and Wang W:
Periostin+cancer-associated fibroblasts promote lymph node
metastasis by impairing the lymphatic endothelial barriers in
cervical squamous cell carcinoma. Mol Oncol. 15:210–227. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Gillot L, Lebeau A, Baudin L, Pottier C,
Louis T, Durré T, Longuespée R, Mazzucchelli G, Nizet C, Blacher S,
et al: Periostin in lymph node pre-metastatic niches governs
lymphatic endothelial cell functions and metastatic colonization.
Cell Mol Life Sci. 79:2952022. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Qin S, Yi L, Liang Y, Chen Y, Wang W, Liao
Y, Zhang C, Huang H, Huang J and Yao S: Biological and
Clinicopathological Characteristics of OPN in Cervical Cancers.
Front Genet. 13:8365092022. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Castor MDGFC, Torres LC, Mello RJV, Natal
RA and Vassallo J: Study on collagen parameters in vulvar cancer
and preneoplastic lesions by Second Harmonic Generation microscopy.
Sci Rep. 10:55682020. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Holthoff ER, Byrum SD, Mackintosh SG,
Kelly T, Tackett AJ, Quick CM and Post SR: Vulvar squamous cell
carcinoma aggressiveness is associated with differential expression
of collagen and STAT1. Clin Proteomics. 14:402017. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Wu Z, Shen Y, Gong K, Wu Z, Zhang T, Zhang
X and Li S: Increased osteopontin expression is associated with
progression from vulvar precancerous lesions to vulvar squamous
cell carcinoma. Arch Gynecol Obstet. 289:637–644. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Sgambato A, Tarquini E, Resci F, De Paola
B, Faraglia B, Camerini A, Rettino A, Migaldi M, Cittadini A and
Zannoni GF: Aberrant expression of alpha-dystroglycan in cervical
and vulvar cancer. Gynecol Oncol. 103:397–404. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Brockbank EC, Bridges J, Marshall CJ and
Sahai E: Integrin beta1 is required for the invasive behaviour but
not proliferation of squamous cell carcinoma cells in vivo. Br J
Cancer. 92:102–112. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Hefler LA, Concin N, Mincham D, Thompson
J, Swarte NB, van Eijkeren MA, Sie-Go DM, Hammond I, McCartney AJ,
Tempfer CB and Speiser P: The prognostic value of
immunohistochemically detected CD44v3 and CD44v6 expression in
patients with surgically staged vulvar carcinoma: A multicenter
study. Cancer. 94:125–130. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Johansson N, Vaalamo M, Grénman S,
Hietanen S, Klemi P, Saarialho-Kere U and Kähäri VM: Collagenase-3
(MMP-13) is expressed by tumor cells in invasive vulvar squamous
cell carcinomas. Am J Pathol. 154:469–480. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Bovo AC, da Silva ID, Takita LC, Fochi J,
Stávale JN, Marks G and de Lima GR: A comparative study of MMP-2 in
vulvar neoplasms. Gynecol Oncol. 93:454–457. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Hua H, Li M, Luo T, Yin Y and Jiang Y:
Matrix metalloproteinases in tumorigenesis: An evolving paradigm.
Cell Mol Life Sci. 68:3853–3868. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Kerkelä E, Ala-aho R, Klemi P, Grénman S,
Shapiro SD, Kähäri VM and Saarialho-Kere U: Metalloelastase
(MMP-12) expression by tumour cells in squamous cell carcinoma of
the vulva correlates with invasiveness, while that by macrophages
predicts better outcome. J Pathol. 198:258–269. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Goepel C, Stoerer S and Koelbl H: Tenascin
in preinvasive lesions of the vulva and vulvar cancer. Anticancer
Res. 23:4587–4591. 2003.PubMed/NCBI
|
|
114
|
Surico N, Priori L, Savoia P, Cremona O
and Marchisio PC: Distribution of integrins and extracellular
matrix proteins in vulvar squamous cell carcinomas. Eur J Gynaecol
Oncol. 16:147–154. 1995.PubMed/NCBI
|
|
115
|
Hellman K, Hellström AC, Silfverswärd C,
Salo S, Aspenblad U, Nilsson B, Frankendal B, Tryggvasson K and
Auer G: Cancer of the vagina: Laminin-5gamma2 chain expression and
prognosis. Int J Gynecol Cancer. 10:391–396. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Theocharis AD, Manou D and Karamanos NK:
The extracellular matrix as a multitasking player in disease. FEBS
J. 286:2830–2869. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Diao B and Yang P: Comprehensive analysis
of the expression and prognosis for laminin genes in ovarian
cancer. Pathol Oncol Res. 27:16098552021. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Jing J, Lien CF, Sharma S, Rice J, Brennan
PA and Górecki DC: Aberrant expression, processing and degradation
of dystroglycan in squamous cell carcinomas. Eur J Cancer.
40:2143–2151. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Sgambato A and Brancaccio A: The
dystroglycan complex: From biology to cancer. J Cell Physiol.
205:163–169. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Cabral-Pacheco GA, Garza-Veloz I,
Castruita-De la Rosa C, Ramirez-Acuña JM, Perez-Romero BA,
Guerrero-Rodriguez JF, Martinez-Avila N and Martinez-Fierro ML: the
roles of matrix metalloproteinases and their inhibitors in human
diseases. Int J Mol Sci. 21:97392020. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Lu P, Weaver VM and Werb Z: The
extracellular matrix: A dynamic niche in cancer progression. J Cell
Biol. 196:395–406. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Sahai E, Astsaturov I, Cukierman E,
DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR,
Hunter T, et al: A framework for advancing our understanding of
cancer-associated fibroblasts. Nat Rev Cancer. 20:174–186. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Costea DE, Hills A, Osman AH, Thurlow J,
Kalna G, Huang X, Pena Murillo C, Parajuli H, Suliman S, Kulasekara
KK, et al: Identification of two distinct carcinoma-associated
fibroblast subtypes with differential tumor-promoting abilities in
oral squamous cell carcinoma. Cancer Res. 73:3888–3901. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Obradovic A, Graves D, Korrer M, Wang Y,
Roy S, Naveed A, Xu Y, Luginbuhl A, Curry J, Gibson M, et al:
Immunostimulatory cancer-associated fibroblast subpopulations can
predict immunotherapy response in head and neck cancer. Clin Cancer
Res. 28:2094–2109. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Puram SV, Tirosh I, Parikh AS, Yizhak K,
Gillespie S, Rodman C, Luo CL, Mroz EA, Emerick KS, Deschler DG, et
al: Single-Cell transcriptomic analysis of primary and metastatic
tumor ecosystems in head and neck cancer. Cell. 171:1611–1624.e24.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Hu C, Zhang Y, Wu C and Huang Q:
Heterogeneity of cancer-associated fibroblasts in head and neck
squamous cell carcinoma: Opportunities and challenges. Cell Death
Discov. 9:1242023. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Mirkeshavarz M, Ganjibakhsh M, Aminishakib
P, Farzaneh P, Mahdavi N, Vakhshiteh F, Karimi A, Gohari NS, Kamali
F, Kharazifard MJ, et al: Interleukin-6 secreted by oral
cancer-associated fibroblast accelerated VEGF expression in tumor
and stroma cells. Cell Mol Biol (Noisy-le-grand). 63:131–136. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Bae JY, Kim EK, Yang DH, Zhang X, Park YJ,
Lee DY, Che CM and Kim J: Reciprocal interaction between
carcinoma-associated fibroblasts and squamous carcinoma cells
through interleukin-1α induces cancer progression. Neoplasia.
16:928–938. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Öhlund D, Handly-Santana A, Biffi G,
Elyada E, Almeida AS, Ponz-Sarvise M, Corbo V, Oni TE, Hearn SA,
Lee EJ, et al: Distinct populations of inflammatory fibroblasts and
myofibroblasts in pancreatic cancer. J Exp Med. 214:579–596. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Lavie D, Ben-Shmuel A, Erez N and
Scherz-Shouval R: Cancer-associated fibroblasts in the single-cell
era. Nat Cancer. 3:793–807. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
El Herch I, Tornaas S, Dongre HN and
Costea DE: Heterogeneity of cancer-associated fibroblasts and
tumor-promoting roles in head and neck squamous cell carcinoma.
Front Mol Biosci. 11:13400242024. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Chen J, Zhang L, Zhu Y, Zhao D, Zhang J,
Zhu Y, Pang J, Xiao Y, Wu Q, Wang Y and Zhan Q:
AKT2(S128)/CCTα(S315/319/323)-positive cancer-associated
fibroblasts (CAFs) mediate focal adhesion kinase (FAK) inhibitors
resistance via secreting phosphatidylcholines (PCs). Signal
Transduct Target Ther. 9:212024. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Li W, Xu T, Jin H, Li M and Jia Q:
Emerging role of cancer-associated fibroblasts in esophageal
squamous cell carcinoma. Pathol Res Pract. 253:1550022024.
View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Qin X, Guo H, Wang X, Zhu X, Yan M, Wang
X, Xu Q, Shi J, Lu E, Chen W and Zhang J: Exosomal miR-196a derived
from cancer-associated fibroblasts confers cisplatin resistance in
head and neck cancer through targeting CDKN1B and ING5. Genome
Biol. 20:122019. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Huang W, Zhang L, Yang M, Wu X, Wang X,
Huang W, Yuan L, Pan H, Wang Y, Wang Z, et al: Cancer-associated
fibroblasts promote the survival of irradiated nasopharyngeal
carcinoma cells via the NF-κB pathway. J Exp Clin Cancer Res.
40:872021. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Li X, González-Maroto C and Tavassoli M:
Crosstalk between CAFs and tumour cells in head and neck cancer.
Cell Death Discov. 10:3032024. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Dongre H, Rana N, Fromreide S, Rajthala S,
Bøe Engelsen I, Paradis J, Gutkind JS, Vintermyr OK, Johannessen
AC, Bjørge L and Costea DE: Establishment of a novel cancer cell
line derived from vulvar carcinoma associated with lichen sclerosus
exhibiting a fibroblast-dependent tumorigenic potential. Exp Cell
Res. 386:1116842020. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Milacic M, Beavers D, Conley P, Gong C,
Gillespie M, Griss J, Haw R, Jassal B, Matthews L, May B, et al:
The reactome pathway knowledgebase 2024. Nucleic Acids Res.
52((D1)): D672–D678. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Li T, Fu J, Zeng Z, Cohen D, Li J, Chen Q,
Li B and Liu XS: TIMER2.0 for analysis of tumor-infiltrating immune
cells. Nucleic Acids Res. 48:W509–W514. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Cancer Genome Atlas Network, .
Comprehensive genomic characterization of head and neck squamous
cell carcinomas. Nature. 517:576–582. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Cancer Genome Atlas Research Network and
Albert Einstein College of Medicine; Analytical Biological
Services; Barretos Cancer Hospital; Baylor College of Medicine;
Beckman Research Institute of City of Hope; Buck Institute for
Research on Aging; Canada's Michael Smith Genome Sciences Centre;
Harvard Medical School; Helen F. Graham Cancer Center &Research
Institute at Christiana Care Health Services et al., . Integrated
genomic and molecular characterization of cervical cancer. Nature.
543:378–384. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Cancer Genome Atlas Research Network;
Analysis Working Group; Asan University; BC Cancer Agency; Brigham
and Women's Hospital; Broad Institute; Brown University; Case
Western Reserve University; Dana-Farber Cancer Institute; Duke
University et al., . Integrated genomic characterization of
oesophageal carcinoma. Nature. 541:169–175. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Cancer Genome Atlas Research Network, .
Comprehensive genomic characterization of squamous cell lung
cancers. Nature. 489:519–525. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Bergonzini C, Kroese K, Zweemer AJM and
Danen EHJ: Targeting integrins for cancer therapy-disappointments
and opportunities. Front Cell Dev Biol. 10:8638502022. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Winer A, Adams S and Mignatti P: Matrix
metalloproteinase inhibitors in cancer therapy: Turning past
failures into future successes. Mol Cancer Ther. 17:1147–1155.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Yan Z, Hu X, Tang B and Deng F: Role of
osteopontin in cancer development and treatment. Heliyon.
9:e210552023. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Zagani R, Hamzaoui N, Cacheux W, de
Reyniès A, Terris B, Chaussade S, Romagnolo B, Perret C and
Lamarque D: Cyclooxygenase-2 inhibitors down-regulate osteopontin
and Nr4A2-new therapeutic targets for colorectal cancers.
Gastroenterology. 37:1358–1366.e1-e3. 2009. View Article : Google Scholar
|
|
148
|
Sroka TC, Pennington ME and Cress AE:
Synthetic D-amino acid peptide inhibits tumor cell motility on
laminin-5. Carcinogenesis. 27:1748–1757. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Tran M, Rousselle P, Nokelainen P,
Tallapragada S, Nguyen NT, Fincher EF and Marinkovich MP: Targeting
a tumor-specific laminin domain critical for human carcinogenesis.
Cancer Res. 68:2885–2894. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Heider KH, Sproll M, Susani S, Patzelt E,
Beaumier P, Ostermann E, Ahorn H and Adolf GR: Characterization of
a high-affinity monoclonal antibody specific for CD44v6 as
candidate for immunotherapy of squamous cell carcinomas. Cancer
Immunol Immunother. 43:245–253. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Sandström K, Nestor M, Ekberg T, Engström
M, Anniko M and Lundqvist H: Targeting CD44v6 expressed in head and
neck squamous cell carcinoma: Preclinical characterization of an
111In-labeled monoclonal antibody. Tumour Biol. 29:137–144. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Song K, Yu Z, Zu X, Li G, Hu Z and Xue Y:
Collagen remodeling along cancer progression providing a novel
opportunity for cancer diagnosis and treatment. Int J Mol Sci.
23:105092022. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Singh B, Sims H, Trueheart I, Simpson K,
Wang KC, Patzkowsky K, Wegman T, Soma JM, Dixon R, Jayes F, et al:
A Phase I clinical trial to assess safety and tolerability of
injectable collagenase in women with symptomatic uterine fibroids.
Reprod Sci. 28:2699–2709. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Oo KK, Kamolhan T, Soni A, Thongchot S,
Mitrpant C, O-Charoenrat P, Thuwajit C and Thuwajit P: Development
of an engineered peptide antagonist against periostin to overcome
doxorubicin resistance in breast cancer. BMC Cancer. 21:652021.
View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Nakazawa Y, Taniyama Y, Sanada F,
Morishita R, Nakamori S, Morimoto K, Yeung KT and Yang J: Periostin
blockade overcomes chemoresistance via restricting the expansion of
mesenchymal tumor subpopulations in breast cancer. Sci Rep.
8:40132018. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Zhu M, Saxton RE, Ramos L, Chang DD,
Karlan BY, Gasson JC and Slamon DJ: Neutralizing monoclonal
antibody to periostin inhibits ovarian tumor growth and metastasis.
Mol Cancer Ther. 10:1500–1508. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Lee YJ, Kim IS, Park SA, Kim Y, Lee JE,
Noh DY, Kim KT, Ryu SH and Suh PG: Periostin-binding DNA aptamer
inhibits breast cancer growth and metastasis. Mol Ther.
21:1004–1013. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Liu GX, Xi HQ, Sun XY and Wei B: Role of
periostin and its antagonist PNDA-3 in gastric cancer metastasis.
World J Gastroenterol. 21:2605–2613. 2015. View Article : Google Scholar : PubMed/NCBI
|