Introduction
Stroke is a major global health concern and the
second leading cause of disability and mortality worldwide
(1). In Vietnam, stroke is the
leading cause of mortality and disability (2). Dysphagia is defined as an impairment
in swallowing that results in an abnormal transit of a liquid or
solid bolus from the oral cavity to the stomach. The antero- or
retrograde entry of saliva, food or gastric secretion into the
airway under the level of the vocal folds is defined as aspiration.
This is very common following a stroke, causing aspiration
pneumonia with a prevalence of up to 80% (3). The early detection of problems with
swallowing not only reduces the risk of pneumonia, but also helps
to minimize the risk of malnutrition, dehydration, the length of
hospital stays and mortality, and allows for the spontaneous
recovery of swallowing functions. A number of treatment approaches
for swallowing disorders have been proposed, including compensatory
strategies, rehabilitation techniques, invasive interventions and
surgical management. Swallowing rehabilitation is considered a safe
and highly effective treatment method for patients to help prevent
complications, thereby significantly reducing mortality (4).
The management of swallowing disorders consists of
using thickeners to control and prevent aspiration pneumonia.
During the oral phase of swallowing, the fluid flow is disturbed. A
person can tolerate these factors, and the substances will pass
through the airways into the esophagus. However, individuals with
dysphagia may have trouble controlling this process, and this
affects their ability to protect the airway. One of the solutions
is to alter the consistency of the fluid with a thickener for
improved swallowing coordination. Thickeners are safe and have been
used therapeutically for swallowing disorders for the past 19
years. The European Society for Swallowing Disorders (ESSD)
concluded that increasing the consistency reduces the risk of
aspiration and is a valuable management strategy for dysphagia
(5).
A number of studies have been conducted to examine
the influence of bolus consistency on swallow safety and
effectiveness. Kuhlemeier et al (6) examined 190 patients using
videofluoroscopy (VFS; videofluoroscopic swallowing examination)
with mild to moderate dysphagia due to several causes. The results
of their study revealed that the prevalence of aspiration was
higher when swallowing thin liquids with a cup than when swallowing
ultrathick liquids with a spoon (6). In their study, xanthan gum was used
as a thickener, and the results also revealed a significant
reduction in the aspiration rate from 35.3 to 13.7% with the use of
thin liquids with nectar consistency, and to 9.3% with the use of
spoon-thick liquids (6). Clavé
et al (7) reported that
penetration into the laryngeal vestibule was the most common
indicator of impaired swallow safety and occurred most frequently
with liquid bolus (21.6 mPa.s), less with nectar (295.0 mPa.s), and
least with pudding viscosity (3682.2 mPa.s). Diniz et al
(8) conducted a study on 61
patients following a stroke by increasing the food consistency from
thin to a spoon thick (very thick), and the results revealed a
significant reduction in the aspiration rate. Rofes et al
(9) reported that altering the
bolus consistency from liquid to pudding reduced the prevalence of
aspiration and pneumonia in 98.9% of patients.
According to the study by Jongprasitkul and
Kitisomprayoonkul (10),
conventional swallowing therapy including swallowing exercises and
maneuvers, postural and compensation techniques, food and
environmental modification, and alternative feeding was an
effective treatment for patients with acute stroke with
dysphagia.
In Vietnam, while research on dysphagia following
stroke is mainly focused on methods of screening and diagnosis, to
the best of our knowledge, there are no studies available on the
effectiveness of these interventions. Therefore, the present study
was conducted in an aim to evaluate the effect of food thickeners
combined with swallowing exercises in patients with dysphagia
following cerebral infarction.
Patients and methods
Research design
The present study adopted a quasi-experimental
one-group pre-test/post-test design and a convenience sampling
method. For the experimental intervention, patients who suffered a
stroke and met the study criteria were treated using swallowing
rehabilitation and oral feeding with thickeners. A pre- and
post-test were conducted before and 5, 10, and at 15 days following
treatment.
Participants and study setting
In the present study, 33 patients who suffered a
stroke and were admitted to Hanoi Rehabilitation Hospital (Hanoi,
Vietnam) between July, 2020 and May, 2021 were recruited. The mean
duration of hospitalization was 2.5 months, the minimum was 3
weeks, and the maximum was 4 months.
The inclusion criteria were as follows: i) An age
≥18 years; ii) first-time ischemic stroke; iii) a Montreal
Cognitive Assessment (MoCA) score ≥21 points; iv) a Mann Assessment
of Swallowing Ability (MASA) score ≤177; and v) patients must have
provided written consent to participate in the study.
The exclusion criteria were the following: i)
Patients with cerebral infarction who had respiratory failure and
needed to be intubated, with a loss of consciousness, ii) patients
with other swallowing disorders, or those with brain damage due to
various causes, or those with brain tumors, brain metastases,
traumatic brain injury, nervous system infections, encephalitis, or
meningitis; iii) patients has epilepsy; and iv) patients with
esophageal stenosis and pyloric stenosis.
Intervention and data collection
procedure
Through clinical evaluation, the speech therapist
gathered information about the patient's cognition, motor and
sensory impairments, and appropriateness for oral intake, and then
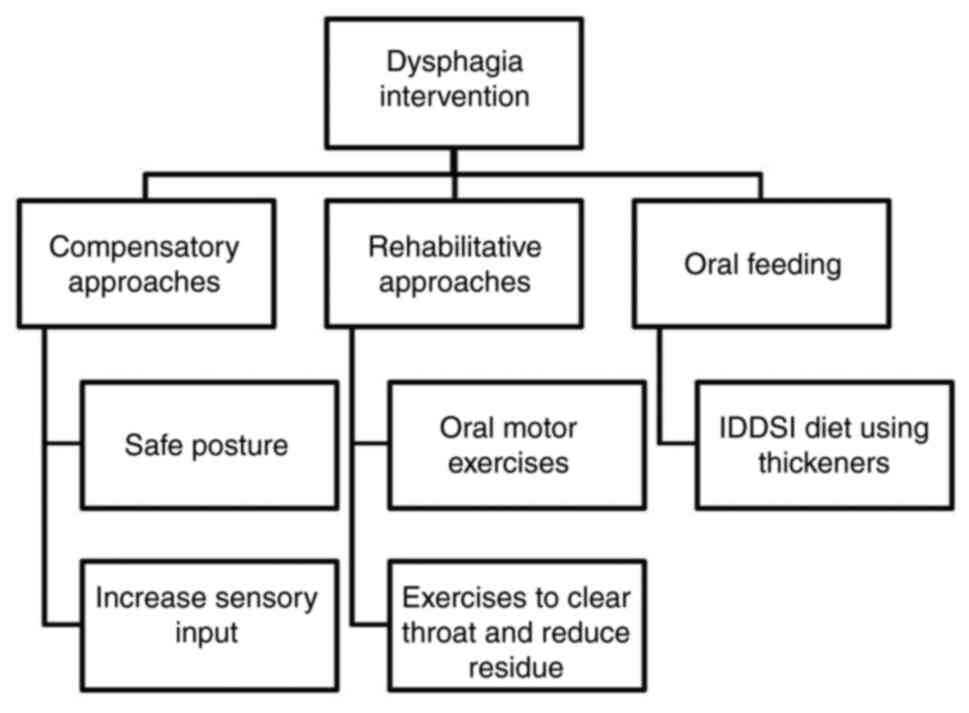
developed an individualized rehabilitation program. Dysphagia
rehabilitation comprises of compensatory and rehabilitative
approaches. Compensatory strategies, including postural adjustments
and increasing sensory input are used to reduce symptoms of
dysphagia without changing the physiology. Rehabilitative
approaches improve swallowing physiology and improve swallow safety
and the tolerance of the least restrictive diet, such as oral motor
exercises, effortful swallow, Mendelsohn maneuver, supraglottic
swallow, Super supraglottic swallow, Masako maneuver and Shaker
exercises. The patients received one 35-min session once a day, 5
days a week for 3 weeks. They were also allowed to eat by mouth
following The International Dysphagia Diet Standardization
Initiative (IDDSI) if considered appropriate. Prerequisites to be
tested with oral feeding included: Consciousness, normal vital
signs, stable respiratory status (SpO2 of 95%,
respiration rates of 12 to 20 breaths per minute,
inhalation/exhalation time=1:2, normal lung sounds), and good
saliva management. Patients who had pneumonia, wet voice, poor
saliva control or no consistencies appeared to be safe for them,
were continued as ‘nil by mouth’. The intervention approaches used
in the present study are illustrated in Fig. 1.
Intervention materials
The present study used Softia, a Japanese
ready-to-use food and beverage thickener supplied by the Asia Food
and Nutrition Corporation. Depending on specific drinks and foods,
the present study used Softia S, Softia U or Softia G. The MASA
data were collected at baseline and at 5, 10, and 15 days following
treatment.
Ethical considerations
The families and patients were provided with a
detailed explanation about the purpose, rights and obligations
while participating in the study. Patients were provided with
information about methods and possible discomforts during the study
period. The study participants could withdraw from the study at any
time.
Instruments
The MASA scale was used to assess the swallowing
function of the patients at baseline and after the intervention. It
was developed by Mann (11) in
2002 as a screening tool for identifying dysphagia in patients who
suffered a stroke.
It is a simple bedside evaluation that carries no
risk of aspiration as no feeds of any quantity are introduced to
the patient. It is inexpensive and does not require specialist
services. Another advantage of this clinical test is that it does
not require any special device or radiation exposure.
The MASA scale consists of 24 items, divided into
four components as follows: General patient examination, oral
preparation phase, oral phase and pharyngeal phase. Each item has a
maximum score of 10, and the total score is 200. The cut-off point
for dysphagia is 177, and that of aspiration is 169; the severity
level of dysphagia and the risk of aspiration was thus determined,
as presented in Table I (12,13).
 | Table ISeverity level and risk of aspiration
in the patients determined using the MASA scale. |
Table I
Severity level and risk of aspiration
in the patients determined using the MASA scale.
| Abnormality | MASA score for
dysphagia | MASA score for the
risk of aspiration |
|---|
| No abnormality | 178-200 | 170-200 |
| Mild | 168-177 | 149-169 |
| Moderate | 139-167 | 148 |
| Severe | <138 | <140 |
Statistical analysis
The data were analyzed using Stata 14.0 software
(StataCorp LLC). Frequencies, percentages and mean/median were
calculated to demonstrate the distribution of demographic
variables, the severity of swallowing disorder, symptoms of
swallowing disorder, the risk of aspiration, the time of
intervention and treatment results. Data were analyzed using the
Chi-squared statistical test (if <20% of cells had an expected
frequency <5) or Fisher's exact test (if >20% of cells had an
expected frequency <5) when testing the difference between the
two groups. A value of P<0.05 was considered to indicate a
statistically significant difference.
Results
Status of dysphagia in the study
participants
The demographic data of patients who suffered a
stroke are presented in Table II.
A total of 33 patients who suffered a stroke were selected for the
study; there were 22 males and 11 females and 81.8% of the
participants were >60 years of age. The majority of the patients
had mild to moderate dysphagia (87.9%), and only 4 patients had
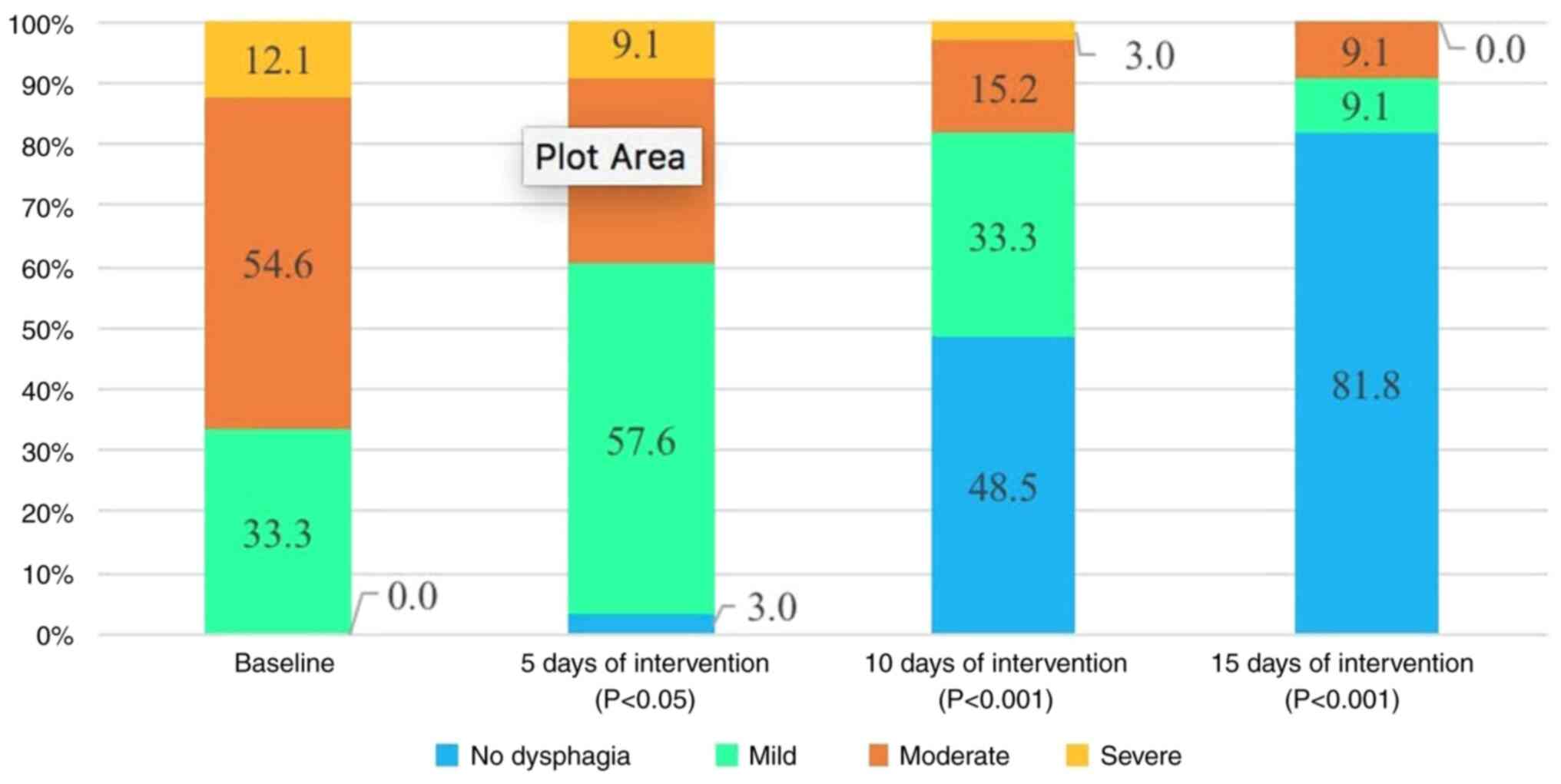
severe dysphagia (12.1%) (Fig. 2).
The most common symptom was cough/choking while swallowing (29
patients, 87.9%). Other symptoms included drooling, food spillage,
residue inside the mouth, the sensation of food stuck in the throat
or the chest, reduced gag reflex, voice change and ineffective
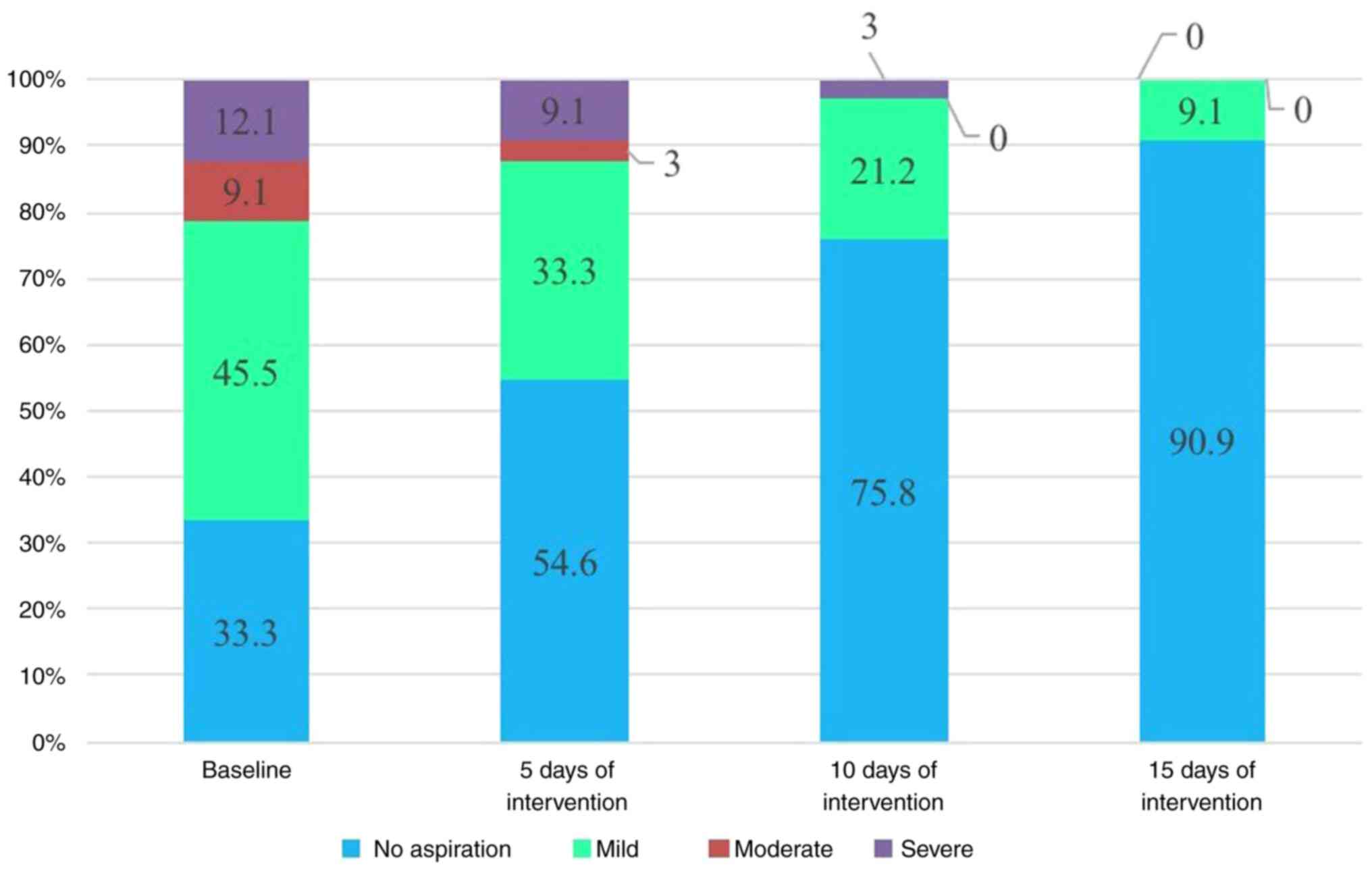
cough. Patients at risk of mild aspiration accounted for a high
percentage of 45.5%. A total of 21.2% of patients had a risk of
severe and moderate aspiration, and 33.3% of patients did not have
a risk of aspiration (Fig. 3).
Intervention was implemented as soon as possible. The majority of
patients received rehabilitation at an early stage, in <1 month
(26 patients,78.8%).
 | Table IIDemographic and clinical
characteristics of the patients. |
Table II
Demographic and clinical
characteristics of the patients.
| Characteristic | No. of patients
(n=33) | Percentage |
|---|
| Age, years | | |
|
20-39 | 1 | 3.0 |
|
40-59 | 5 | 15.2 |
|
60-70 | 16 | 48.5 |
|
>70 | 11 | 33.3 |
| Sex | | |
|
Male | 22 | 66.7 |
|
Female | 11 | 33.3 |
| Stroke lesion
location | | |
|
Right
hemisphere | 15 | 45.5 |
|
Left
hemisphere | 17 | 51.5 |
|
Both | 1 | 3.0 |
| Onset of
intervention | | |
|
<1
week | 3 | 9.1 |
|
1-4
weeks | 23 | 69.7 |
|
1-2
months | 5 | 15.2 |
|
>2
months | 2 | 6.1 |
| Symptoms | | |
|
Residue
inside the mouth | 20 | 60.6 |
|
Drooling | 21 | 63.6 |
|
Cough/choking
while swallowing | 29 | 87.9 |
|
Food
spillage | 22 | 66.7 |
|
Sensation of
food stuck in the throat or chest | 19 | 57.6 |
|
Reduced gag
reflex | 18 | 54.5 |
|
Voice
change | 11 | 33.3 |
|
Ineffective
cough | 5 | 15.2 |
| Time received
rehabilitation | | |
|
<1
month | 26 | 78.8 |
|
≥1
month | 7 | 21.2 |
| Symptoms of
swallowing disoders | | |
|
Choking when
swallowing | 29 | 87.9 |
|
Drooling | 21 | 63.6 |
|
Food
spillage symptoms | 22 | 66.7 |
Before and after intervention
The proportion of patients at risk of developing
severe aspiration pneumonia decreased from 12.1 to 9.1% after 5
days of treatment. After 15 days of treatment, there were no
patients at risk of severe aspiration. The number of patients who
were no longer at risk of developing aspiration pneumonia increased
from 33.3 to 54.6% after 5 days, to 75.8% after 10 days and to
90.9% after 15 days of treatment (Fig.
3).
The proportion of patients who suffered from severe
dysphagia decreased from 12.1 to 9.1% after 5 days, to 3% after 10
days and to 0% after 15 days of treatment. The proportion of
patients without swallowing disorder and mild swallowing disorder
increased from 33.3 to 60.6% after 5 days of treatment, to 81.8%
after 10 days and to 90.9% after 15 days of treatment (P<0.05).
The percentage of patients whose dysphagia resolved after 10 days
was 48.5% and after 15 days this number was 81.8% (Fig. 2).
The rate of swallowing disorders after 15 days of
intervention was 18.2%. In particular, a comparison between groups
regarding the time of intervention revealed that the rate of
swallowing disorders in the early intervention group <1 week
(0%) and 1-4 weeks (0%) was lower than that in the intervention
group at 1-2 months (80%) and >2 months (100%), with the
difference being statistically significant (P<0.001) (Table III).
 | Table IIIAssociation between the onset of
intervention and outcomes in the patients following 15 days of
intervention. |
Table III
Association between the onset of
intervention and outcomes in the patients following 15 days of
intervention.
| | Onset of
intervention | |
|---|
| Outcome | <1 week | 1-4 weeks | 1-2 months | >2 months | Total | P-value |
|---|
| Dysphagia severity,
n (%) | | | | | | |
|
Yes | 0 | 0 | 4(80) | 2(100) | 6 (18.2) |
<0.001a |
|
No | 3(100) | 23(100) | 1(20) | 0 | 27 (81.8) | |
| Total | 3 | 23 | 5 | 2 | 33 | |
Following treatment, all symptoms of dysphagia
improved. The rate of choking when swallowing decreased from 87.9
to 9.1%. Drooling and food spillage symptoms decreased from 63.6
and 66.7 to 12.1%.
Discussion
In 2000, Mann et al (14) conducted a study on 128 patients who
suffered a stroke who were clinically evaluated by the MASA scale
and the results were compared with VFS. Patients were followed-up
for 6 months following the stroke; the MASA scale was proven to be
valuable compared with VFS in diagnosing dysphagia with a
sensitivity of 73% and specificity of 89%; the diagnosis of
aspiration with a specificity of 93% and specificity of 67%
(14).
In the present study, the severity of dysphagia was
evaluated according to the MASA scale. The results revealed that
33.3% of the patients had mild dysphagia, 54.6% had moderate
dysphagia and 12.1% had severe dysphagia. The clinical symptoms of
swallowing disorders included coughing and choking during and after
eating (87.9%), food spillage (66.7%), drooling (63.3%), food
residue inside the mouth (60.6%), the sensation of food being stuck
in the throat or chest (57.6%), decreased gagging reflex (54.6%)
and voice change after swallowing (33.3%). The study by Terré and
Mearin (15) revealed that 47% of
patients with dysphagia coughed while eating, 44% had decreased gag
reflex, and 13% experienced a change in voice.
According to previous research, cough and voice
change after swallowing are key clinical signs of dysphagia
suggesting aspiration. According to the study by Daniels et
al (16), voice change and wet
voice after swallowing had a sensitivity and specificity of 38.1
and 85.3%, and cough after swallowing had a sensitivity of 38.5%
and specificity of 84.8%. When combining these two symptoms,
sensitivity and specificity increased to 92.3 and 66.7%. Although
they are not the gold standard for diagnosing swallowing disorders,
they are easy to use and can help predict the risk of aspiration
pneumonia. If patients are evaluated and treated at an early stage,
the risk of aspiration and other complications from dysphagia will
then be reduced. Some cases of voice change after swallowing are
difficult to recognize and the examiner needs to re-examine several
times (16,17-18).
The results of the present study also demonstrated
that 45.5% of patients had a low risk of aspiration, 12.1% with
high risk and 9.1% with medium risk. According to the study by Mann
et al (14) on 128 patients
who were clinically evaluated within 3 days following a stroke, 51%
of the patients suffered from aspiration. The patients were
assessed by VFS within 10 days after the stroke and the rate of
aspiration was 22% . Another study demonstrated that approximately
one-third of patients who suffered a stroke aspirated on VFS. Among
the patients that aspirated, one-third developed pneumonia and half
of them aspirated silently (19).
Swallowing rehabilitation includes swallowing
exercises and maneuvers, postural and compensation techniques, diet
and environmental modification, and alternative feeding (20). It has been proven to be a simple
and valid approach to reducing the risk of aspiration. Lazarus
et al (21) demonstrated
that supraglottic swallow was effective in closing the vocal cords
to protect the airway during swallowing, especially when combined
with the Mendelsohn maneuver. The study by Bülow et al
(22) demonstrated that effortful
swallow reduced the depth of airway infiltration, and should be
combined with exercises to increase the strength and range of
motion of the tongue. Shaker et al (23) performed a study on 24 patients with
dysphagia and the results revealed that the Shaker exercise
increased the opening of the upper esophageal sphincter and
anterior movement of the larynx, reduced residue in pyriform sinus
and aspiration after swallowing.
Softia is a ready-to-use food and beverage thickener
that was developed in Japan. Softia rapidly increases the viscosity
of the liquid and maintains a stable consistency. The advantage of
Softia is that it dissolves rapidly and is not affected by the
enzyme amylase in saliva. With Softia thickener, the IDDSI diet and
compensatory techniques, such as safe posture, the patient can
actively control the flow of the bolus, thereby improving their
swallowing function.
The present study demonstrated that the proportion
of patients with severe dysphagia decreased to 0% following 15 days
of treatment. The proportion of patients who no longer had
swallowing disorder and mild swallowing disorder increased to 90.9%
after 15 days of treatment.
In the present study, after applying swallowing
rehabilitation exercises in combination with the IDDSI diet using
thickeners, there was an improvement in the risk of aspiration
specifically as follows: The proportion of patients at risk of
severe aspiration decreased after 5 days of treatment from 12.1 to
9.1%. Following 15 days of treatment, there were no patients at
risk of severe aspiration. The number of patients who were no
longer at risk of aspiration increased after 5 days of treatment
from 33.3 to 54.6%, to 75.8% after 10 days and to 90.9% after 15
days of treatment.
According to the study by Clavé et al
(7) penetration into the laryngeal
vestibule occurred most often when swallowing food at liquid
viscosity (21.6 mPa.s); this decreased when the subject was given
nectar (295.0 mPa.s), and further with pudding consistency (3682.2
mPa.s). Rofes et al (9)
also reported a statistically significant result in which
increasing the consistency of food bolus from liquid to pudding
reduced the rate of aspiration and aspiration pneumonia in 98.9% of
patients.
Kuhlemeier et al (6) studied >190 subjects with dysphagia
associated with different causes ranging from mild to moderate by
VFS. The results revealed that the rate of aspiration was higher
when drinking thin liquid from a cup than when having extra-solid
food with a spoon. Similar results proved that swallowing safety
was improved when using xanthan gum as a thickener, as there was a
significant reduction in aspiration from 35.3% with thin liquids to
13.7% with nectar and 9.3% with spoon-thick form). Another study
was conducted on 61 patients post-stroke; when increasing the food
bolus consistency from a thin liquid to spoon-thick form (very
thick), the results revealed a significant reduction in the rate of
aspiration into the larynx, and no patient had any symptoms of
aspiration following intervention (8).
In the present study, following treatment, all
symptoms of dysphagia improved. All the changes in symptoms were
statistically significant (P<0.05). Thus, the combination of
swallowing rehabilitation exercises with the use of thickeners to
adjust the diet for patients with dysphagia contributed to
improving symptoms and helping patients to be more confident. They
no longer felt concerned after choking and coughing several times,
thereby being motivated to practice.
The results of the present study demonstrated that
the number of patients whose dysphagia resolved after 10 days was
48.5% and after 15 days this number was 81.8%. The approach of
swallowing intervention by combining swallowing exercises with
adjusting the food consistency with thickeners proved to be very
effective. According to the study by Kwakkel et al (24), patients would recover the most
during the first 6 months after a stroke). Therefore, the sooner
the intervention, the better the prognosis of patients recovering
from dysphagia. Thus, the onset of intervention is one of the
prognostic factors for patients. Patients who suffer a stroke need
to be screened for swallowing disorders and received treatment as
soon as they are in the intensive care unit.
The present study had certain limitations which
should be mentioned. Firstly, the use of a single-group design, and
lack of a control group suggest that the results should be
generalized with caution. Secondly, the present study only used the
MASA scale, a clinical evaluation to assess dysphagia. Another
limitation of the present study was the small sample size. The
present study was conducted with a limited number of participants,
which may affect the generalizability and reliability of the
findings. According to the results of the present study, the
authors propose the following recommendations: i) Future studies
are required to employ randomized controlled trials to enhance the
validity of the conclusion; and ii) further studies are require to
enhance the validity of the study results, and future studies may
use medical devices to objectively measure the results of the
intervention, such as VFS.
In conclusion, as demonstrated in the present study,
the majority of the patients who suffered a stroke had mild and
moderate dysphagia. A combination of swallowing rehabilitation
exercises and using thickeners to adjust the diet for patients with
dysphagia helped reduce the severity of swallowing dysfunction, and
the rate of aspiration and improved all symptoms, particularly
choking. Patients who received early intervention had a better
prognosis and recovery from dysphagia.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
VMP, TVN and THL were involved in the conception and
design of the study, were performed the statistical analysis of the
data. VMP, TVN and TTHN were involved in the investigative aspects
of the study. VMP, TVN and THL were involved in the interpretation
of the data. VMP, TVN, TTHN and THL were involved in the writing of
the origional draft of the manuscript, and in the writing,
reviewing and editting of the manuscript. All authors read and
agreed to the published version of the manuscript. VMP and THL
confirm the the authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved by the Hanoi Medical
University Institutional Ethical Review Board under Decision No.
268/GCN-HDDDNCYSH-DHYHN, dated June 8, 2020. All patients were
provided a written consent to participate in this study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Krishnamurthi RV, Ikeda T and Feigin VL:
Global, regional and country-specific burden of ischaemic stroke,
intracerebral haemorrhage and subarachnoid haemorrhage: A
systematic analysis of the global burden of disease study 2017.
Neuroepidemiology. 54:171–179. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Carr C, Kahn L, Mathkour M, Biro E, Bui CJ
and Dumont AS: The shifting burden of neurosurgical disease:
Vietnam and the middle-income nations. Neurosurg Focus.
45(E12)2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Takizawa C, Gemmell E, Kenworthy J and
Speyer R: A systematic review of the prevalence of oropharyngeal
dysphagia in stroke, Parkinson's disease, Alzheimer's disease, head
injury, and pneumonia. Dysphagia. 31:434–441. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Vesey S: Dysphagia and quality of life. Br
J Community Nurs. 18:S14–19. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Newman R, Vilardell N, Clavé P and Speyer
R: Effect of bolus viscosity on the safety and efficacy of
swallowing and the kinematics of the swallow response in patients
with oropharyngeal dysphagia: White paper by the European society
for swallowing disorders (ESSD). Dysphagia. 31:232–249.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kuhlemeier KV, Palmer JB and Rosenberg D:
Effect of liquid bolus consistency and delivery method on
aspiration and pharyngeal retention in dysphagia patients.
Dysphagia. 16:119–122. 2001.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Clavé P, Arreola V, Romea M, Medina L,
Palomera E and Serra-Prat M: Accuracy of the volume-viscosity
swallow test for clinical screening of oropharyngeal dysphagia and
aspiration. Clin Nutr. 27:806–815. 2008.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Diniz PB, Vanin G, Xavier R and Parente
MA: Reduced incidence of aspiration with spoon-thick consistency in
stroke patients. Nutr Clin Pract. 24:414–418. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Rofes L, Arreola V and Clavé P: The
volume-viscosity swallow test for clinical screening of dysphagia
and aspiration. Nestle Nutr Inst Workshop Ser. 72:33–42.
2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jongprasitkul H and Kitisomprayoonkul W:
Effectiveness of conventional swallowing therapy in acute stroke
patients with Dysphagia. Rehabil Res Pract.
2020(2907293)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mann G: MASA, the mann assessment of
swallowing ability. Vol. 1 New York, NY: Cengage Learning;
(2002).
|
|
12
|
Antonios N, Carnaby-Mann G, Crary M,
Miller L, Hubbard H, Hood K, Sambandam R, Xavier A and Silliman S:
Analysis of a physician tool for evaluating dysphagia on an
inpatient stroke unit: The modified mann assessment of swallowing
ability. J Stroke Cerebrovasc Dis. 19:49–57. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kwon S, Sim J, Park J, Jung Y, Cho KH, Min
K, Kim MY, Kim KM and Im SH: Assessment of aspiration risk using
the mann assessment of swallowing ability in brain-injured patients
with cognitive impairment. Front Neurol. 10(1264)2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mann G, Hankey GJ and Cameron D:
Swallowing disorders following acute stroke: Prevalence and
diagnostic accuracy. Cerebrovasc Dis. 10:380–386. 2000.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Terré R and Mearin F: Oropharyngeal
dysphagia after the acute phase of stroke: Predictors of
aspiration. Neurogastroenterol Motil. 18:200–205. 2006.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Daniels SK, Brailey K, Priestly DH,
Herrington LR, Weisberg LA and Foundas AL: Aspiration in patients
with acute stroke. Arch Phys Med Rehabil. 79:14–19. 1998.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Warms T and Richards J: ‘Wet Voice’ as a
predictor of penetration and aspiration in oropharyngeal dysphagia.
Dysphagia. 15:84–88. 2000.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Murray J, Langmore SE, Ginsberg S and
Dostie A: The significance of accumulated oropharyngeal secretions
and swallowing frequency in predicting aspiration. Dysphagia.
11:99–103. 1996.PubMed/NCBI View Article : Google Scholar
|
|
19
|
McCullough GH, Rosenbek JC, Wertz RT,
McCoy S, Mann G and McCullough K: Utility of clinical swallowing
examination measures for detecting aspiration post-stroke. J Speech
Lang Hear Res. 48:1280–1293. 2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Palmer JB, Pelletier CA and Matsuo K:
Rehabilitation of patients with swallowing disorders. In: Braddom
R. L., Chan L., Harrast M. A. et al., Editors. Physical
Medicine and Rehabilitation. 4th. Philadelphia: Elsevier Saunders,
2011.
|
|
21
|
Lazarus CL, Logemann JA, Rademaker AW,
Kahrilas PJ, Pajak T, Lazar R and Halper A: Effects of bolus
volume, viscosity, and repeated swallows in nonstroke subjects and
stroke patients. Arch Phys Med Rehabil. 74:1066–1070.
1993.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bülow M, Olsson R and Ekberg O:
Videomanometric analysis of supraglottic swallow, effortful
swallow, and chin tuck in patients with pharyngeal dysfunction.
Dysphagia. 16:190–195. 2001.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Shaker R, Easterling C, Kern M, Nitschke
T, Massey B, Daniels S, Grande B, Kazandjian M and Dikeman K:
Rehabilitation of swallowing by exercise in tube-fed patients with
pharyngeal dysphagia secondary to abnormal UES opening.
Gastroenterology. 122:1314–1321. 2002.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kwakkel G, Kollen B and Lindeman E:
Understanding the pattern of functional recovery after stroke:
Facts and theories. Restor Neurol Neurosci. 22:281–299.
2004.PubMed/NCBI
|