Introduction
The COVID-19 epidemic began in China at the end of
2019, and became a pandemic by 2020(1). The first case of infection in Japan
was reported on January 14, 2020(2). As the number of infected individuals
increased rapidly, the government and municipalities called for
voluntary restraints on events that could increase the risk of
infection, such as cross-prefecture travel and dining, affecting
numerous areas, including public administration, medical facilities
and educational institutions. Medical facilities took measures such
as postponing routine medical examinations and non-urgent
surgeries. To reduce the risk of infection, patients began to avoid
visits to doctors, particularly for pediatrics and otolaryngology
in Japan (3). In emergency
transport, an increase in the number of difficult cases and a
longer time spent at the scene were noted (4). Similarly, Taiwan and Germany
experienced a decline in the number of emergency transport requests
(5,6), making it challenging to find suitable
facilities for certain cases (7).
The present study examined the impact of COVID-19
infection on the emergency transfers of patients with obstetric and
gynecological diseases in Kochi Prefecture, Japan. Kochi Prefecture
has a population of ~680,000. In 2021, the percentage of older
adults aged ≥65 years was 35.2%, markedly higher than the national
average of 28.4% (8). Surrounded
by the Pacific Ocean and the Shikoku Mountains, Kochi Prefecture is
situated in a difficult location for receiving medical care beyond
the prefectural border, apart from some areas, and the provision of
medical care must be completed within the prefecture. The numbers
of physicians and hospital beds per 100,000 individuals have
exhibited a steady decline in Kochi Prefecture. However, it is
still higher than the national average, partly owing to the decline
in the population in Kochi. As of 2022, there were 313.9 physicians
(national average, 253.6) and 1,105.2 general hospital beds
(national average, ~701.4) per 100,000 individuals (9). According to the Fire and Disaster
Management Agency of the Ministry of Internal Affairs and
Communications, there were about 40,000 emergency medical calls per
year, with 581.5 calls per 10,000 individuals in 2021. In the same
year, the national figure was 491.2 dispatches per 10,000, and
Kochi Prefecture had a higher number of dispatches per population
than the national average (10).
As of 2021, seven general hospitals, six clinics and
one midwifery center were handling childbirth deliveries in Kochi
Prefecture. Of note, ~30% of deliveries in Kochi are performed at
clinics. Owing to the aging of obstetricians and gynecologists,
more temporary facilities have suspended deliveries in recent
years. Thus, obstetric and gynecological care, particularly
perinatal care, is not robust. Although the number of deliveries is
decreasing with the declining birthrate, the number of high-risk
pregnancies is increasing owing to the higher age of pregnant
women, patients with complex social backgrounds and pregnancies
complicated by psychiatric disorders. Moreover, the number of cases
that require individualized care is increasing.
Notably, access to and the quality of medical care
in Japan is high by global standards, and the disparity between
regions in the country is the lowest worldwide (11). However, the regional cities in
Japan are experiencing a declining population and an uneven
distribution of medical facilities and physicians. The challenges
in rural areas, where medical resources and medical institutions
are limited, could differ from those in urban areas, where there
are many medical institutions or major medical departments, such as
internal medicine.
When a situation such as the recent pandemic occurs
and causes a prolonged disruption to the medical field, making the
most of limited medical resources is an important issue. The
present study first examined the extent to which the pandemic
caused confusion in the medical field, focusing on the field of
obstetrics and gynecology, which is not directly related to the
practice of COVID-19 medical care. As regards making the most of
limited medical resources, by focusing on departments with limited
resources, the present study provides insight that may be useful
during emergencies. The changes in emergency transfers for
obstetric and gynecological cases in Kochi Prefecture in the pre-
and post-pandemic period were compared in an aim to discover clues
with which to solve the issue of facilitating emergency medical
care in an emergency situation.
Subjects and methods
Study design and setting
This cross-sectional study was conducted by
extracting data on emergency transport of obstetric and
gynecological diseases in Kochi Prefecture from January, 209 to
December, 2021 from the database ‘Kochi-Iryo-Net’ (https://www.kochi-iryo-net/).
Japan has a nationwide fire/ambulance service that
can be availed by dialing the emergency number 119. This
taxpayer-funded service is available to anyone, anytime and
anywhere at no charge. When an individual calls 119 during an
emergency, the nearest fire station dispatches an ambulance to the
patient, locates a receiving hospital based on the chief complaint
and condition of the patient, and subsequently transfers the
patient to medical personnel. Fire stations are operated and
managed by municipal governments, and each station is equipped with
fire engines and ambulances according to the size of the local
population. As of 2021, there were 41 fire stations in Kochi
Prefecture.
The Kochi-Iryo-Net is a database established in 2015
as part of the medical and disaster information system of Kochi
Prefecture. The database contains information about fire and
ambulance dispatches and crew details, dates and times of calls,
destination medical institutions and distance between patients from
the fire department. Upon arrival at the destination (medical
institution), an attending doctor recorded pertinent information
regarding institution names, locations where patients were
collected, types and degrees of conditions or urgency in the
institutional medical record database. The Kochi Prefectural
Government then integrated this information into the Kochi-Iryo-Net
database. The data that support the findings of the present study
are available from the Kochi Prefecture database. However, these
data are not publicly available as they report the surveillance
conducted by Kochi Prefecture Healthcare Policy Division Department
for monitoring emergency medical care.
Study participants
From the Kochi-Iryo-Net, data were extracted on
transports made between January, 2019 and December, 2021 that
indicated obstetrics and gynecology as the disease classification.
Since the disease name was written in a free description format by
the receiving physician, it was additionally converted to the
ICD-10 code for the corresponding disease name.
The period from January to December, 2019 was
defined as the pre-expansion period of COVID-19 infection
(pre-pandemic), and that from January, 2020 to December, 2021 was
considered as the expansion period of COVID-19 infection (during
the post-pandemic period).
In order to protect patient privacy, all data were
anonymized by the Kochi Prefecture Medical Policy Division. The
data obtained were already in an anonymized state. The study
protocol was approved by the Ethics Committee of Kochi University
School of Medicine (approval no. 2021-142). The present study was
conducted in accordance with the Ethical Guidelines for Medical and
Biological Research Involving Human Subjects by the Ministry of
Education, Culture, Sports, Science and Technology; the Ministry of
Health, Labour and Welfare; and the Ministry of Economy, Trade and
Industry and the Declaration of Helsinki (2013 amendment).
Variables
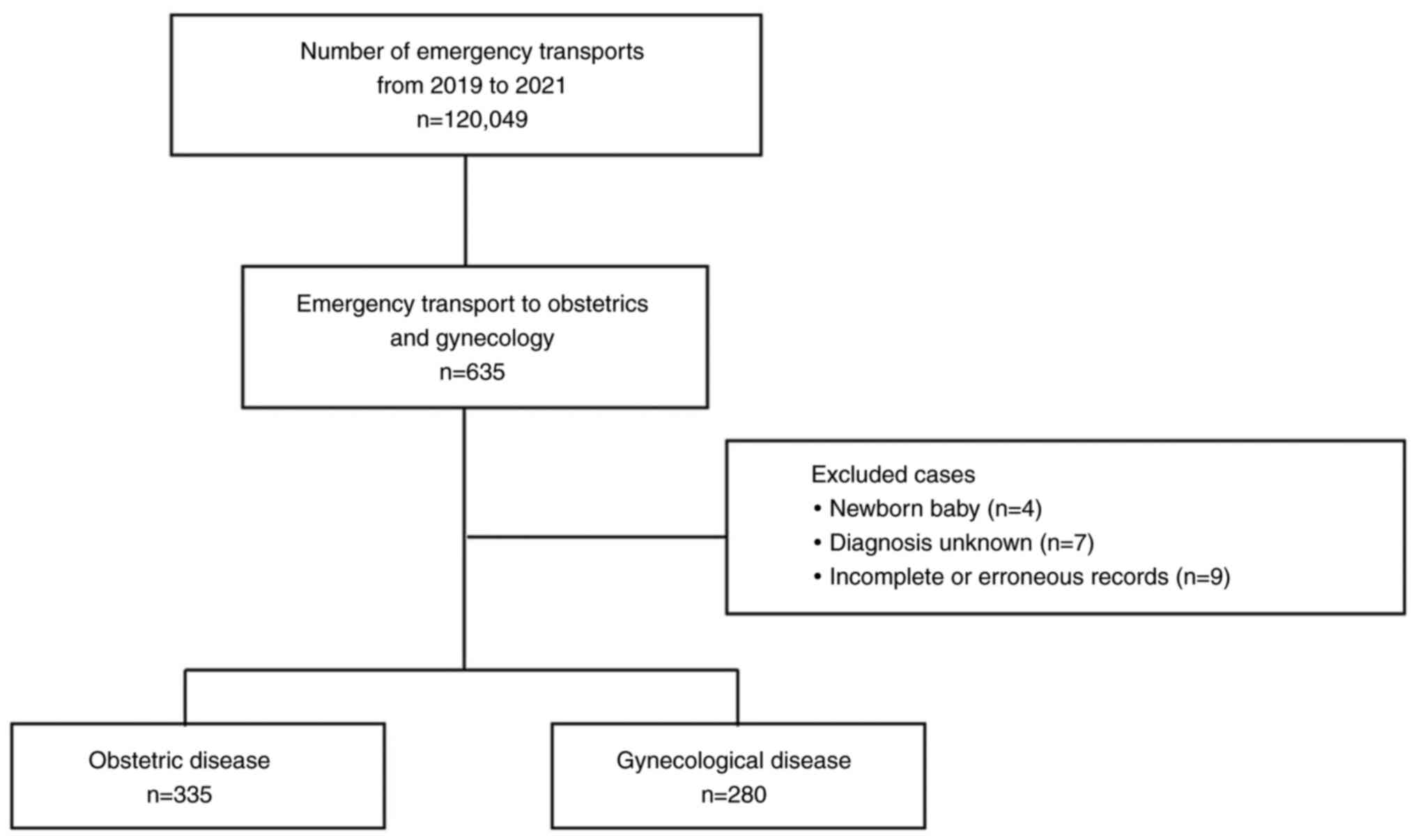
Only the cases classified as obstetrics and
gynecology diseases were included in the present study. Cases
classified as ‘O: Pregnancy, delivery, and postpartum’ by the
ICD-10 code were classified as obstetric cases, and those with
other codes were classified as gynecological cases. Newborns who
were transported together with their mothers for out-of-hospital
deliveries (n=4), cases with unknown diseases (n=7), and those with
incorrectly entered or incompletely recorded transport dates and
times (n=9) were excluded from the study (Fig. 1).
The type of transport was examined separately for
transfers and non-transfers. The time required for transport was
examined in terms of the time required to arrive at the scene, time
spent at the scene, and time from the emergency call to the
transfer to the physician at the receiving facility.
Statistical analysis
All analyses were performed using Stata/MP 16.0
software (StataCorp LLC). Chi-squared tests were performed to
evaluate the number of transports, severity and type of transport,
and the P-values obtained were corrected using the Bonferroni
method. A Kruskal-Wallis test was performed to examine age and
transport time. A two-sided P-value <0.05 was considered to
indicate a statistically significant difference.
Results
Between January, 2019 and December, 2021, a total of
120,049 emergency cases were transported in Kochi Prefecture, of
which 635 were sent to obstetrics and gynecology departments
(Fig. 1).
The number of transports, post-transportation
outcomes and type of transport for obstetric diseases are presented
in Table I. However, there was no
significant difference in the number of transports before and after
COVID-19. There were 88 transfers between hospitals (75.2%) before
the spread of COVID-19 infection; however, the number decreased to
77 (72.6%) in 2020 and 68 (60.7%) in 2021. As regards
post-transportation outcomes, 2.6% of cases were managed as
outpatients before the spread of COVID-19 infection; however, after
the spread of COVID-19 infection, the number of cases increased to
6 (5.7%) and 21 (18.8%) in 2020 and 2021, respectively. The number
of cases admitted to the hospital after transport was 114 (97.4%)
in 2019, 100 (94.3%) in 2020 and 91 (81.2%) in 2021, exhibiting a
decreasing trend. During this period, no cases were deceased at the
time of transport.
 | Table IEmergency transport of patients with
obstetric diseases. |
Table I
Emergency transport of patients with
obstetric diseases.
| | Pre-pandemic | Post-pandemic | |
|---|
| Parameter | All | 2019 | 2020 | 2021 | P-value |
|---|
| Number of
transports | | | | | 0.98 |
|
All | 120,049 | 41,740 | 38,585 | 39,724 | |
|
Obstetric
disease | 335 | 117 | 106 | 112 | |
| Outcome, n (%) | | | | | <0.01 |
|
Outpatient | 30 | 3 (2.6) | 6 (5.7) | 21 (18.8) | |
|
Hospitalization | 305 | 114 (97.4) | 100 (94.3) | 91 (81.2) | |
| Type of transport, n
(%) | | | | | 0.04 |
|
Transfer | 233 | 88 (75.2) | 77 (72.6) | 68 (60.7) | |
|
No
transfer | 102 | 29 (24.8) | 29 (27.4) | 44 (39.3) | |
The numbers of childbirth deliveries and childbirth
delivery facilities in Kochi Prefecture over the 3-year period are
presented in Table II. The number
of emergency transports for obstetric diseases as a percentage of
the number of childbirth deliveries remained at a similar rate of
2.5-2.7% per year. The outcome, age of the patients, and time
required for transport for the cases excluding transfers are
presented in Table III.
Significantly fewer cases were admitted to the hospital after
transport, and more patients were managed as outpatients. The age
of tge patients transported did not differ significantly. The time
required to arrive at the scene was 7-8 min, the time spent at the
scene was 9-12 min, and the time elapsed from the emergency call to
the physician at the receiving facility was 35-40 min; however,
there was no significant difference in time to transport before and
after the spread of COVID-19 infection.
 | Table IINumber of deliveries, delivery
facilities and transports in Kochi Prefecture. |
Table II
Number of deliveries, delivery
facilities and transports in Kochi Prefecture.
| Parameter | 2019 | 2020 | 2021 |
|---|
| No. of childbirth
deliveries in the prefecture | 4,731 | 4,303 | 4,090 |
| Facilities advocating
obstetrics and gynecology | 13 | 14 | 14 |
| Childbirth delivery
facility | | | |
|
General
hospital | 7 | 7 | 7 |
|
Clinic | 7 | 6 | 6 |
|
Maternity
hospital | 1 | 1 | 1 |
| Transport | 117 | 106 | 112 |
|
(per
childbirth delivery) | 2.5 | 2.5 | 2.7 |
| Transfer | 88 | 77 | 68 |
|
(per
childbirth delivery) | 1.86 | 1.79 | 1.66 |
| No transfer | 29 | 29 | 44 |
|
(per
childbirth delivery) | 0.6 | 0.7 | 1.1 |
 | Table IIIEmergency transport patients other
than those transferred owing to obstetric diseases. |
Table III
Emergency transport patients other
than those transferred owing to obstetric diseases.
| | Pre-pandemic | Post-pandemic | |
|---|
| Parameter | 2019 | 2020 | 2021 | P-value |
|---|
| No. of
transports | 29 | 29 | 44 | |
| Outcome, n (%) | | | | 0.03 |
|
Outpatient | 3 (10.3) | 6 (20.7) | 19 (43.2) | |
|
Hospitalization | 26 (89.7) | 23 (79.3) | 25 (56.8) | |
| Age, years; median
(quartile range) | 30 (25-30) | 30 (25-35) | 30 (25-35) | 0.07 |
| Time of transport,
min; median (quartile range) | | | | |
|
Time
required to arrive on-site | 7 (6-9) | 8 (7-10) | 8 (6-10) | 0.34 |
|
On-site
time | 9 (6-13) | 10 (7-13) | 12 (7.5-16) | 0.13 |
|
Time
required for hospitalization | 34 (27-44) | 42 (28-49) | 37 (31.5-45) | 0.41 |
The number of transports, post-transportation
outcomes and type of transport for gynecological diseases are
presented in Table IV. The
outcome, age of the patient and time required for transport for the
cases excluding transfers are presented in Table V. No significant differences were
observed in outcomes, type of transport, the age of the patients
and time required for transport.
 | Table IVEmergency transport of patients with
gynecological diseases. |
Table IV
Emergency transport of patients with
gynecological diseases.
| | Pre-pandemic | Post-pandemic | |
|---|
| Parameter | All | 2019 | 2020 | 2021 | P-value |
|---|
| Number of
transports | | | | | 0.35 |
|
All | 120,049 | 41,740 | 38,585 | 39,724 | |
|
Gynecological
disease | 280 | 108 | 81 | 91 | |
| Outcome, n (%) | | | | | 0.18 |
|
Outpatient | 144 | 58 (53.7) | 42 (51.9) | 44 (48.4) | |
|
Hospitalization | 136 | 50 (46.3) | 39 (48.1) | 47 (51.6) | |
| Type of transport,
n (%) | | | | | 0.97 |
|
Transfer | 56 | 21 (19.4) | 16 (19.8) | 19 (20.9) | |
|
No
transfer | 224 | 87 (80.6) | 65 (80.3) | 72 (79.1) | |
 | Table VPatients transported to emergency
departments other than transfers owing to gynecological
diseases. |
Table V
Patients transported to emergency
departments other than transfers owing to gynecological
diseases.
| | Pre-pandemic | Post-pandemic | |
|---|
| Parameter | 2019 | 2020 | 2021 | P-value |
|---|
| No. of
transports | 87 | 65 | 72 | |
| Outcome, n (%) | | | | 0.71 |
|
Outpatient | 54 (62.1) | 42 (64.6) | 43 (59.7) | |
|
Hospitalization | 33 (37.9) | 23 (35.4) | 29 (40.3) | |
| Age, years; median
(quartile range) | 35 (20-50) | 35 (25-50) | 37.5 (25-62.5) | 0.40 |
| Time of transport,
min; median (quartile range) | | | | |
|
Time
required to arrive on site | 8 (7-10) | 8 (6-10) | 8 (6-9.5) | 0.51 |
|
On-site
time | 13 (9-18) | 14 (10-18) | 14 (9-18) | 0.95 |
|
Time
required for hospitalization | 36 (30-42) | 36 (30-42) | 39 (30.5-49.5) | 0.54 |
Discussion
Using data on emergency transports in Kochi
Prefecture, the present study examined the impact of COVID-19
infection on emergency obstetric and gynecological care. No marked
changes were observed in the number of emergency transports, or the
time required for transport, suggesting that the measures taken to
prevent infection had minimal impact on emergency care.
To date, at least to the best of our knowledge, no
study has examined emergency transport for obstetrics and
gynecology cases on a regional basis. In Osaka, one of the largest
cities in Japan, the number of cases of difficulty in transporting
pregnant women was lower than that of other cases and remained the
same even under pandemic conditions (12).
The present study covered the period from 2019 to
2021; 2019 was considered pre-pandemic, and 2020 and 2021 were
during the post-pandemic period. Even during the COVID-19 pandemic,
in 2020, unknown infectious diseases spread globally, infection
control measures were in a state of flux, and medical practices
underwent a period of great uncertainty (13). In addition, numerous infected
individuals were older adults with a high risk of serious illness
if they became infected (13). By
2021, infection control measures had been established to a certain
extent. The number of infected individuals was increasing, although
the main source of infection was young individuals, and the number
of severe cases decreased. During this period, the number of
pregnant women infected with COVID-19 also increased, and infected
pregnant women were at a high risk of developing severe illness
(14). Thus, the situations of
infected patients varied slightly during the pandemic.
As regards the impact of COVID-19 on obstetrics and
gynecology during this period, in April 2020, the Japanese Society
of Reproductive Medicine issued a statement on the postponement of
fertility treatment (15), and the
Japanese Society of Surgery proposed the postponement of
non-emergency surgery (16). In
fact, according to a survey by the Japan Society of Obstetrics and
Gynecology, the number of surgeries (for both benign and malignant
diseases) and the number of patients seeking fertility treatment
decreased (17). As regards
prenatal check-ups, some facilities reported that they made efforts
to provide remote medical care as an infection control measure
(18,19); however, they were not requested to
take measures such as reducing the number of patient visits.
However, there were calls for individuals to refrain
from moving to other prefectures as a countermeasure against
infection. As a result, some facilities refused to transfer
patients from other prefectures for delivery, or requested that
individuals stay at home for 2 weeks after moving.
In the present study, emergency transport in the
field of obstetrics and gynecology was examined separately for
obstetric and gynecological diseases during the period when the
above measures were taken in daily medical care. For gynecological
diseases, the number of transports and the time required for
transport did not change over the 3-year study period, and it is
considered that the same operations carried out in peacetime were
continued even in the pandemic situation.
By contrast, in Kochi Prefecture, there were two
changes in obstetric conditions: A decrease in the proportion of
transfers and a decrease in the number of patients admitted to
hospital after emergency transport (Table I). Transfer to another hospital for
obstetric disorders refers to the transfer of a pregnant woman who
had been managed in a primary or secondary facility to a
higher-level facility with a neonatal intensive care unit or
maternal fetal intensive care unit owing to a sudden change in her
condition. The decline in hospital transfers may be due to changes
in the management of pregnant women, such as the early referral of
patients who are at a high risk for preterm birth, etc., to
higher-level facilities. In cases in which shortening of the
cervical length or uterine contractions were observed during the
preterm period at the primary facility, hospitalization management
was previously administered at the primary facility and pregnant
women were transported when the disease worsened. During this
period, however, there was an increase in referrals to higher-level
facilities at an early stage, rather than hospitalization
management at primary facilities. This may have been due in part to
a decrease in the number of primary facilities where
hospitalization management could be provided. To avoid bringing
infections into the hospital, patient hospitalizations other than
those for delivery may have been avoided as much as possible.
Subsequently, the decrease in the number of cases
requiring hospitalization after transportation was considered.
Usually, pregnant women have a family doctor and receive regular
check-ups. If there is a change in their condition, they first
consult with their family doctor and ask whether they should
schedule an appointment. The fact that pregnant women request an
ambulance means that their condition has suddenly changed and they
are not in a situation in which they can consult by phone. However,
there was an increase in the number of cases not requiring
hospitalization as they were judged to have been mild. This finding
may be due to an increase in the number of cases that were
undecided between hospitalization and careful outpatient management
at the time of transport, and outpatient management was opted over
hospitalization. This situation may have occurred as numerous
facilities imposed visiting restrictions due to COVID-19, and
patients preferred outpatient management, or as medical
institutions avoided hospitalization due to a hospital bed shortage
or to reduce the chance of bringing COVID-19 into the hospital.
However, it cannot be ruled out that there was an increase in the
number of cases in which emergency calls were made even though the
symptoms were mild. This could be due to the social unrest caused
by COVID-19 or also since more facilities blocked deliveries and
emergency calls made on holidays and during the night as the family
doctor could not be reached. This point requires further
investigation as countermeasures vary depending on the cause. In
the former case, it is necessary to raise awareness about the
proper use of ambulances. In the latter case, it is necessary to
review the medical system. In addition, the indications and timing
of therapeutic interventions, such as inpatient treatment, may
differ depending on whether the patient is being treated at a
primary or higher-level facility. Moreover, during this period, the
pandemic may have affected the implementation of these
interventions. Using a more objective measure of severity to
confirm what changed (e.g., scoring urgency based on patient
background, symptoms, laboratory findings) was also considered
crucial. In addition, accumulating more detailed information on
symptoms and findings may facilitate the future development of
tools to assist diagnosis using artificial intelligence and other
methods (20,21).
The present study used a database covering emergency
transports within Kochi Prefecture. The number of individuals
infected with COVID-19 is reported by prefecture (those diagnosed
with COVID-19 are tabulated by prefecture and published on
prefectural websites, etc.), which makes it easier to identify
trends based on infection status than reports from a single center,
which we believe is a strength of this study.
Despite its strengths, the present study has the
following limitations: The names of diseases in the database were
freely described, and for some cases, it was difficult to grasp the
number of weeks of pregnancy and accurate diagnoses. There were
also cases in which the outcome was unknown. In the field of
obstetrics, maternal deaths, stillbirths, premature births and
other complications have increased since the pandemic occurred
(22,23). Conversely, there have been reports
of an increase in maternal transport, although the rate of
premature births remained the same as before the pandemic (24). Details such as changes in diseases
could not be evaluated in the present study. In addition, the
present study evaluated the cases of difficult transportation only
based on the time required for transportation. Difficult
transportation is generally evaluated by the number of facilities
that were requested to accept transportation and the extension of
on-site stay time. However, owing to the unique circumstances of
Kochi, these indicators may not be able to determine difficult
transportation. First, the number of facilities contacted was not
listed in the data used herein. In Kochi, the number of hospitals
is limited, and the number of facilities that can accept
transportation is limited. Therefore, the number of times
transportation was requested was not an indicator of cases of
difficult transportation even if it was listed. Second, on-site
stay time was associated with the time it takes to determine the
patient's destination, which is usually performed after the patient
has been placed in an ambulance. However, Kochi Prefecture is
geographically wide from east to west, and medical institutions are
concentrated in the center of the prefecture. Therefore, in some
areas, the time on site may not be an indicator of difficulty of
transport, as patients often leave the site and head to the central
part of the prefecture before a decision is made on where to
transport them. The fact that hospitals could maintain normal
medical functions to a certain extent in the department of
obstetrics and gynecology, which was not directly affected by
COVID-19 infection, was a factor that prevented major disruptions
in emergency transport. With fewer facilities handling deliveries
owing to a shrinking population, it is unclear whether facilities
can maintain their medical functions when a new pandemic or other
socially disruptive event occurs in the future. Furthermore, it has
been predicted that Kochi Prefecture will be hit by a huge Nankai
Trough earthquake in the near future, at which time medical
treatment functions will be temporarily paralyzed, and will likely
take some time to recover (25).
In considering emergency obstetrics and gynecology care in rural
areas, one future challenge is establishing a medical care system
that does not disadvantage patients, such as by decreasing the
number of delivery facilities, in an environment that changes year
by year. To this end, strengthening cooperation between hospitals
and clinics, applying artificial intelligence technology to support
diagnoses, using information and communication technology, and
broadening the area of medical cooperation are some of the measures
that can be implemented.
Acknowledgements
The authors would like to thank Dr Ryuhei Nagai,
Associate Professor of the Department of Obstetrics and Gynecology,
Kochi Medical School, Kochi University, Dr Nagamasa Maeda,
Professor of the Department of Obstetrics and Gynecology, Kochi
Medical School, Kochi University, Dr Kingo Nishiyama, Professor of
the Department of Disaster and Emergency Medicine, Kochi Medical
School, Kochi University, and Dr Narifumi Suganuma, Professor of
the Department of Environmental Medicine, Kochi Medical School,
Kochi University, for their advice and guidance in the preparation
of this study. The authors are also grateful to Ms. Marina Minami,
Department of Environmental Medicine, Integrated Center for
Advanced Medical Technologies (ICAM-Tech), Kochi Medical School,
Kochi University, for her great support and specific advice on
statistical analysis and for proofreading the entire manuscript.
The authors also received suggestions from Ms. Hina Miyata, Medical
Course, Kochi Medical School, Kochi University, who is conducting
similar research. Above all, the authors would like to thank the
staff of the Kochi Prefecture Medical Policy Division for providing
data for this study, as well as the members of the emergency
medical team and other medical professionals who cooperated with
Kochi-Iryo-Net daily to collect information.
Funding
Funding: No funding was received.
Availability of data and materials
The data supporting the present findings are under
license from Kochi Prefecture and are not publicly available. The
dataset is surveillance conducted by the Kochi Prefecture
Healthcare Policy Division Department, for monitoring emergency
medical care and is not publicly available, although its use may be
permitted following ethical review.
Authors' contributions
TT was involved in the conceptualization and
methodology of the study, and in the writing the original draft of
the manuscript. MM and HM were involved in the study methodology.
RN and KN were involved in the study methodology, and supervised
the study. TT and MM confirm the authenticity of all the raw data.
All authors (TT, MM, HM, RN, KN, NS, and NM) were involved in the
interpretation of and in reporting the findings of the study. All
authors were involved in the conceptualization of the study,
contributed to, and have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
An opt-out recruitment was adopted to obtain consent
in the present study on the Kochi-Iryo-Net website. There was no
objection from participants to use their information. The present
study was approved by the Ethical Review Committee of Kochi
University School of Medicine in 2021 (no. 2021-142). The present
study was approved by and complied with the Ethical Guidelines for
Medical and Biological Research Involving Human Subjects of the
Ministry of Education, Culture, Sports, Science and Technology; the
Ministry of Health, Labour and Welfare; and the Ministry of
Economy, Trade and Industry and the Declaration of Helsinki (2013
amendment).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chams N, Chams S, Badran R, Shams A, Araji
A, Raad M, Mukhopadhyay S, Stroberg E, Duval EJ, Barton LM and
Hussein IJ: COVID-19: A multidisciplinary review. Front Public
Health. 8(383)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Imai N, Gaythorpe KAM, Bhatia S, Mangal
TD, Cuomo-Dannenburg G, Unwin HJT, Jauneikaite E and Ferguson NM:
COVID-19 in Japan, January-March 2020: Insights from the first
three months of the epidemic. BMC Infect Dis.
22(493)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yumiko M: Impact of new coronavirus
infections on clinic management. Japan Medical Association Research
Institute, 2021 (In Japanese). https://www.jmari.med.or.jp/wp-content/uploads/2021/10/RE106.pdf.
Accessed April 30, 2024.
|
|
4
|
Igarashi Y, Yabuki M, Norii T, Yokobori S
and Yokota H: Quantitative analysis of the impact of COVID-19 on
the emergency medical services system in Tokyo. Acute Med Surg.
8(e709)2021.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Tai HCH, Kao YH, Lai YW, Chen JH, Chen WL
and Chung JY: Impact of the COVID-19 pandemic on medical-seeking
behavior in older adults by comparing the presenting complaints of
the emergency department visits. BMC Emerg Med.
23(63)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hegenberg K, Althammer A, Gehring C,
Prueckner S and Trentzsch H: Pre-hospital emergency medical
services utilization amid COVID-19 in 2020: Descriptive study based
on routinely collected dispatch data in Bavaria, Germany.
Healthcare (Basel). 11(1983)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ryu MY, Park HA, Han S, Park HJ and Lee
CA: Emergency transport refusal during the early stages of the
COVID-19 pandemic in Gyeonggi Province, South Korea. Int J Environ
Res Public Health. 19(8444)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kochi Prefecture: Chapter 2: Current
Situation and Future Projections for the Elderly, etc. (In
Japanese). https://www.pref.kochi.lg.jp/doc/2018022700035/file_contents/file_20212184113656_1.pdf.
Accessed April 30, 2024.
|
|
9
|
Japan Medical Association: Japan medical
analysis platform. Regional Statistics: Kochi (In Japanese).
https://jmap.jp/cities/detail/pref/39. Accessed April
30, 2024.
|
|
10
|
Ministry of Internal Affairs and
Communications Fire and Disaster Management Agency: The State of
Emergency and Rescue Services, 2022 edition (In Japanese).
https://www.fdma.go.jp/publication/rescue/post-4.html.
Accessed April 30, 2024.
|
|
11
|
Fullman N, Yearwood J, Abay SM, Abbafati
C, Abd-Allah F, Abdela J, Abdelalim A, Abebe Z, Abebo TA, Aboyans
V, et al: Measuring performance on the healthcare access and
quality index for 195 countries and territories and selected
subnational locations: A systematic analysis from the global burden
of disease study 2016. Lancet. 391:2236–2271. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ota K, Nishioka D, Katayama Y, Kitamura T,
Masui J, Ota K, Nitta M, Matsuoka T and Takasu A: Influence of the
COVID-19 outbreak on transportation of pregnant women in an
emergency medical service system: Population-based, ORION registry.
Int J Gynaecol Obstet. 157:366–374. 2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
El-Shabasy RM, Nayel MA, Taher MM,
Abdelmonem R, Shoueir KR and Kenawy ER: Three waves changes, new
variant strains, and vaccination effect against COVID-19 pandemic.
Int J Biol Macromol. 204:161–168. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kumar R, Yeni CM, Utami NA, Masand R,
Asrani RK, Patel SK, Kumar A, Yatoo MI, Tiwari R, Natesan S, et al:
SARS-CoV-2 infection during pregnancy and pregnancy-related
conditions: Concerns, challenges, management and mitigation
strategies-a narrative review. J Infect Public Health. 14:863–875.
2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Japanese Society for Reproductive
Medicine: Statement from the Japanese Society for Reproductive
Medicine on new coronavirus infection (COVID-19), 2020 (In
Japanese). http://www.jsrm.or.jp/announce/187.pdf. Accessed April
30, 2024.
|
|
16
|
Japan Surgical Society: Recommendations
for surgical procedures for patients with positive or suspected new
coronavirus, 2020 (In Japanese). https://jp.jssoc.or.jp/modules/aboutus/index.php?content_id=53.
Accessed April 30, 2024.
|
|
17
|
Komatsu H, Banno K, Yanaihara N and Kimura
T: Board Members of Japan Society of Obstetrics and Gynecology.
Prevention and practice during the COVID-19 emergency declaration
period in Japanese obstetrical/gynecological facilities. J Obstet
Gynaecol Res. 46:2237–2241. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nakagawa K, Umazume T, Mayama M, Chiba K,
Saito Y, Kawaguchi S, Morikawa M, Yoshino M and Watari H:
Feasibility and safety of urgently initiated maternal telemedicine
in response to the spread of COVID-19: A 1-month report. J Obstet
Gynaecol Res. 46:1967–1971. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mallampati DP, Talati AN, Fitzhugh C,
Enayet N, Vladutiu CJ and Menard MK: Statewide assessment of
telehealth use for obstetrical care during the COVID-19 pandemic.
Am J Obstet Gynecol MFM. 5(100941)2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Li W, Dong Y, Liu W, Tang Z, Sun C, Lowe
S, Chen S, Bentley R, Zhou Q, Xu C, et al: A deep belief
network-based clinical decision system for patients with
osteosarcoma. Front Immunol. 13(1003347)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Li W, Zhou Q, Liu W, Xu C, Tang ZR, Dong
S, Wang H, Li W, Zhang K, Li R, et al: A machine learning-based
predictive model for predicting lymph node metastasis in patients
with Ewing's Sarcoma. Front Med (Lausanne).
9(832108)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Chmielewska B, Barratt I, Townsend R,
Kalafat E, van der Meulen J, Gurol-Urganci I, O'Brien P, Morris E,
Draycott T, Thangaratinam S, et al: Effects of the COVID-19
pandemic on maternal and perinatal outcomes: A systematic review
and meta-analysis. Lancet Glob Health. 9:e759–e772. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Molina RL, Tsai TC, Dai D, Soto M,
Rosenthal N, Orav EJ and Figueroa JF: Comparison of pregnancy and
birth outcomes before vs during the COVID-19 pandemic. JAMA Netw
Open. 5(e2226531)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Homma C, Hasegawa J, Nishimura Y, Furuya
N, Nakamura M and Suzuki N: Declaration of emergency state due to
COVID-19 spread in Japan reduced maternal transports without
reduction in preterm delivery. Int J Gynaecol Obstet. 161:854–860.
2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Watanabe T, Katata C, Matsushima S, Sagara
Y and Maeda N: Perinatal care preparedness in Kochi prefecture for
when a Nankai Trough earthquake occurs: Action plans and disaster
liaisons for pediatrics and perinatal medicine. Tohoku J Exp Med.
257:77–84. 2022.PubMed/NCBI View Article : Google Scholar
|