Introduction
Hydatid cyst, also known as cystic echinococcosis,
is a parasitic infection caused by the Echinococcus parasite
(1). It most commonly affects the
lungs and liver, although other organs can also be involved
(2). This disease poses a global
threat as a parasitic infection, mainly affecting regions focused
on farming and domestic animal husbandry. It remains endemic in
several geographical areas, including South Africa, the Middle
East, Australia, the Mediterranean and the Americas (3). There are four species of
Echinococcus: E. vogeli, E. granulosus, E.
multilocularis, and E. oligarthrus that can infect
humans. However, the larval stage of E. granulosus is the
cause of hydatid cysts in 95% of cases (4,5).
Humans are incidental hosts to the parasite, becoming infected
through direct contact with the definitive hosts (canines) or by
ingesting food or water contaminated with the eggs of the parasite
(6,7). Pancreatic hydatid cyst (PHC) is a
rare form of hydatid disease, even in endemic regions where
agriculture and stockbreeding are common occupations (8). The infection is commonly
asymptomatic; however, signs and symptoms of PHC can include
intermittent fever with shivering, loss of appetite, nausea,
vomiting, epigastric pain, obstructive jaundice, weight loss and
recurrent acute pancreatitis (9,10).
The present study reports study the a case of a
67-year-old male patient with primary PHC. The report follows the
SCARE guidelines, and all references have been screened for
reliability (11,12).
Case report
Patient information
A 67-year-old male from a rural area in the
central-eastern part of Iraq visited the Internal Medicine Clinic
at Smart Health Tower (Sulaymaniyah, Iraq) with severe epigastric
pain, fever and vomiting for a period >2 weeks. The patient had
a previous medical history of diabetes mellitus and hypertension.
He had a history of cholecystectomy for gallstones 30 years prior.
During this procedure, a bile duct stone was found, leading to the
decision to perform a Roux-en-Y hepaticojejunostomy, since
endoscopic retrograde cholangiopancreatography (ERCP) was not
accessible in the region at that time. The patient also reported a
history of contact with sheep and goats, as his family owned
livestock. However, the history of ingesting contaminated foods was
unclear.
Clinical findings
A physical examination revealed epigastric fullness
and tenderness without jaundice. Laboratory investigations revealed
a hemoglobin level of 13.1 g/dl (normal range, 13-17 g/dl), a white
blood cell count of 21,600 mm3 (normal range,
4,000-11,000 mm3) and a platelet count of 531,000
mm3 (normal range, 150,000-400,000 mm3).
Other biochemical analyses yielded results which were within the
normal range, including a lipase level of 66.1 IU/l (normal range,
13-85 IU/l), a total serum bilirubin level of 0.462 mg/dl (normal
range, 0.3-1.2 mg/dl), an alkaline phosphatase level of 111 IU/l
(normal range, 40-130 IU/l) and an alanine aminotransferase level
of 6.9 IU/l (normal level, <50 IU/l).
Diagnostic assessment
An endoscopic ultrasound (EUS) revealed a cystic
lesion in the pancreatic head with a solid component. A subsequent
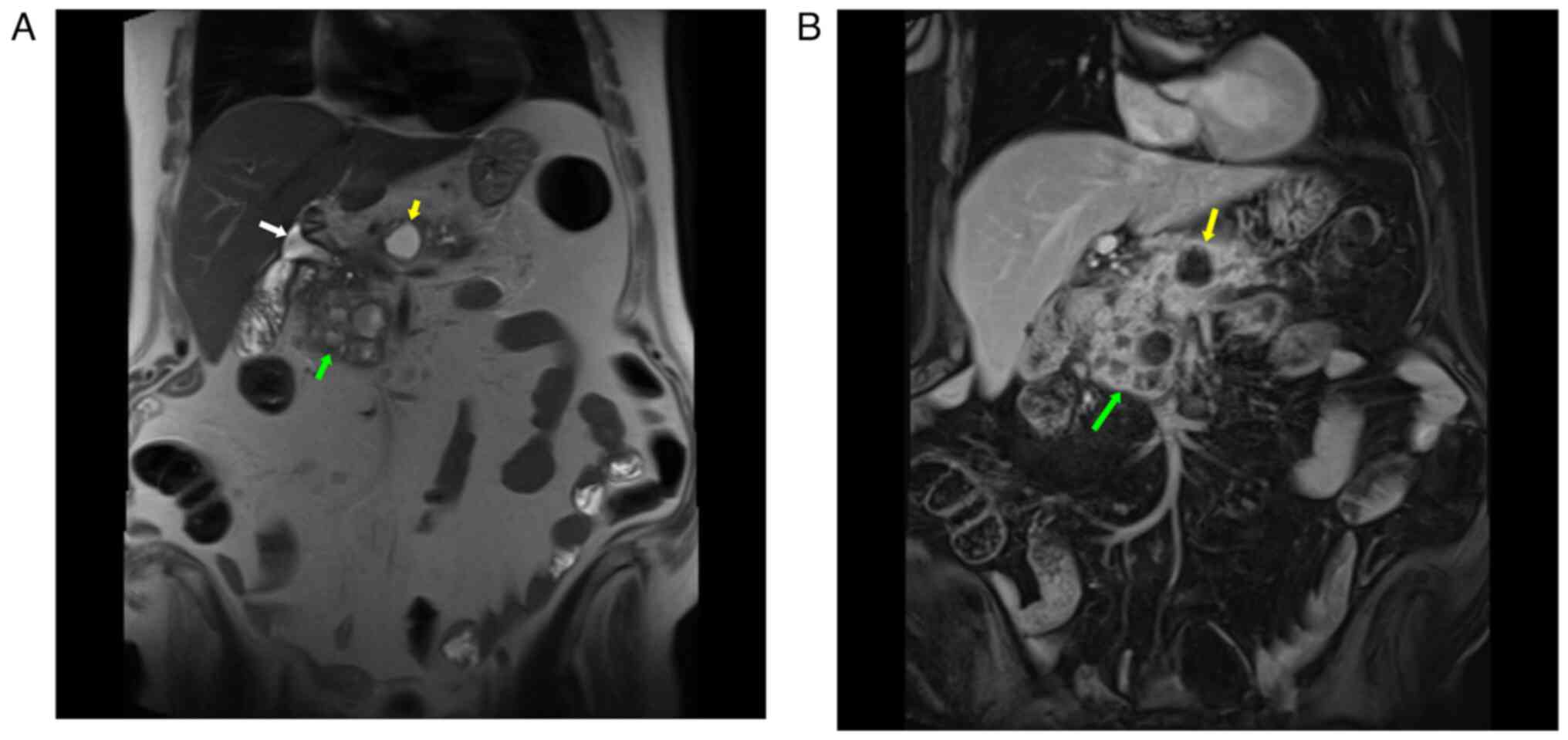
computed tomography (CT) scan confirmed this finding. Magnetic
resonance imaging (MRI) of the abdomen further detailed a
multiloculated cyst situated in the head and uncinate process of
the pancreas, measuring 54x58x51 mm. It had a thick enhancing wall
with multiple thick enhancing septae, diffusion restriction, and no
communication with the pancreatic duct (Fig. 1). At least eight local reactive
lymph nodes were identified (all <7 mm in short-axis diameter).
The lesion adjoined the superior mesenteric vein and portal vein
for a distance of >5 cm; however, there were no signs of
invasion into the gastroduodenal artery, hepatic artery, or
superior mesenteric artery. Another cyst, measuring 20x20 mm, was
observed at the posterior aspect of the pancreatic body, with an
apparent connection to the side branch of the pancreatic duct. The
common bile duct had a diameter of 10 mm, and the main pancreatic
duct was 5 mm, both of which entered the mass region. There were,
additionally, several small pancreatic cysts in the background that
reached out to the spleen. Fine-needle aspiration cytology revealed
a pyogenic inflammatory process with extensive pancreatic fibrosis
and no evidence of malignancy.
Therapeutic intervention
Under general anesthesia and following the
administration of a dose of 1 g Ceftriaxone intravenously supplied
by Acino Swiss, an incision was made in the left subcostal
extension. The intraoperative assessment revealed a large cystic
tumor occupying the head and uncinate process, along with other
cysts distributed over the pancreatic body. Total pancreatectomy
with partial excision of the attached second portion of the
duodenum and splenectomy were performed due to the presence of a
large mass, as indicated by imaging findings. The mass nearly
covered the pancreas and extended toward the spleen. None of the
imaging findings suggested features indicative of a hydatid cyst,
raising concerns among the surgeons and necessitating consideration
of the aforementioned intervention. Hemostasis was achieved, and
two corrugated drains were left in place, followed by thorough
irrigation and layered skin closure. Of note, three biopsy
fragments were sent for a histopathological examination: The
duodenum with the attached head of the pancreas (16.5x8x5.5 cm),
the spleen (11x7.5x3.5 cm) and an irregular gray-brown fragment of
pancreatic tissue (11.5x5.5x2.5 cm). The sections (5-µm-thick) were
paraffin-embedded and fixed with 10% neutral-buffered formalin at
room temperature for 24 h. The sections were then stained with
hematoxylin and eosin (Bio Optica Co.) for 1-2 min at room
temperature and were examined under a light microscope (Leica
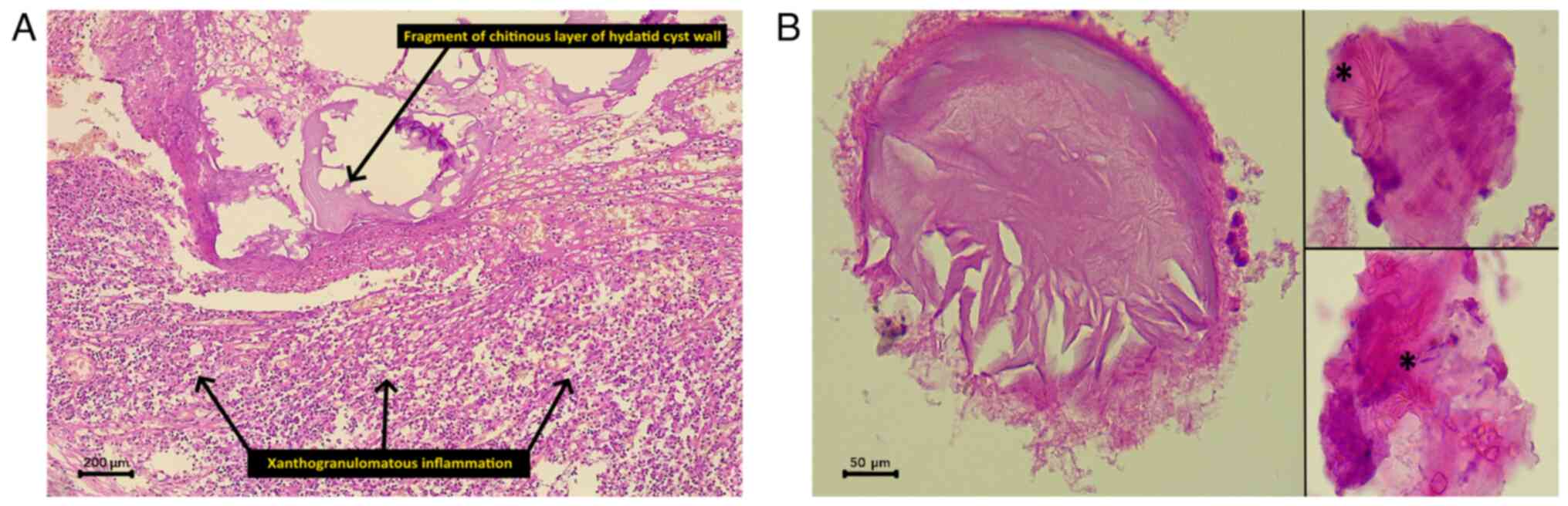
Microsystems GmbH). The pancreatic head and the separate pancreatic
fragment had a firm, dull, gray-cut surface with scattered white
areas. A microscopic examination revealed chronic
xanthogranulomatous pancreatitis, consistent with rare acellular
fragments of the hydatid cyst wall and remnants of hooklets from
the brood capsules (Fig. 2). It
was consistent with a reaction to a hydatid cyst. All the
peripancreatic lymph nodes were benign, and the spleen contained a
benign spindle cell tumor, consistent with an inflammatory
pseudotumor.
Follow-up
Following the surgery, the patient was admitted to
the intensive care unit for 2 days. On the 4th post-operative day,
the patient developed tachypnea and hypoxia. Consequently, a CT
pulmonary angiography was performed, revealing a bilateral
pulmonary artery embolism. He received 6,000 units of heparin
intravenously in two doses, leading to an improved condition. He
was discharged without complications on the 10th post-operative
day. The patient received a 4-week course of albendazole at a
dosage of 800 mg/day (PHARMA développement). The case remained
stable without complications during the 6-month follow-up period,
after which he was lost to follow-up. At 11 months after the
surgery, his family reported his death due to increased insulin
requirements and uncontrollable diabetes.
Discussion
Echinococcosis is a parasitic infection that
originates from the Echinococcus parasite. It can affect
almost every organ and body part (1,3). The
primary hosts for the parasite are dogs, jackals and wolves, and
the intermediate hosts are cattle, sheep, horses and humans
(4). The liver and lungs are the
most commonly affected organs, accounting for 90% of cases. The
involvement of the pancreas is uncommon (1,3,9). The
ingestion of food and water contaminated by the eggs of the
parasite or direct contact with the primary host leads to infection
(13).
Individuals who own livestock have a 3-fold greater
risk of being diagnosed with Echinococcus infection compared
to those who do not own livestock (14). The patient in the present case
report owned livestock and had contact with sheep and goats. PHCs
are uncommon, with a frequency ranging from 0.14 to 2%. PHCs are
commonly unrecognized (90-91%) and distributed unevenly over the
tail (16-19%), body (24-34%) and head (50-58%). In the case
described herein, the PHC affected the head of the pancreas. The
infection may reach the pancreas via the biliary ducts,
retroperitoneal extension, lymphatic spread from the intestinal
mucosa and hematogenous transmission through the pancreatic vessels
(9). The majority of reported
cases fall within 18-38 years of age (9), although the patient in the present
study was 67 years of age. Several similar cases have been reported
in the literature (4,8,9,15-23)
and are summarized in Table I.
 | Table ISummary of some cases of pancreatic
hydatid cyst in the literature. |
Table I
Summary of some cases of pancreatic
hydatid cyst in the literature.
| Authors (year of
publication) | No. of cases | Age (years) | Sex (M/F) | Symptoms | PMH | Cyst location on the
pancreas | Cyst size (cm) | Management | POAR | Complications | Follow-up | (Refs.) |
|---|
| Kothiya et al
(2022) | 1 | 20 | F | Epigastric Pain | None | Pancreatic head | 6.46 | Laparoscopic partial
cystopericystectomy and omentoplasty | Albendazole 15
mg/kg/day, for 8 weeks | None | Uneventful | (15) |
| Cherouaqi et
al (2021) | 1 | 54 | F | Epigastric and left
hypochondriac pain | Hypothyroidism | Pancreatic
isthmus | 5 | Surgical exploration
and resection | Albendazole 800
mg/day, for three months | None | Uneventful | (16) |
| Alsaid et al
(2018) | 1 | 34 | M | Abdominal pain,
dyspnea, fatigue, and weakness | Acute
pancreatitis | The space between the
tail of the pancreas, spleen, left colic angle, left kidney,
stomach, and diaphragm | 21.8 | Surgical exploration
and cyst fenestration | None | Acute edematous
pancreatitis and deep vein thrombosis | Uneventful | (4) |
| Ozsay et al
(2018) | 1 | 23 | F | Epigastric pain | None | Pancreatic tail | 4.47 | Surgical exploration
and enbloc resection of distal pancreas and spleen | Albendazole 800
mg/day, for three months | None | Uneventful | (17) |
| El Bakkaly et
al (2017) | 1 | 5 | F | Epigastric pain,
dietary vomiting, and diarrhea | None | Pancreatic head | N/A | Surgical exploration,
cyst sterilization, and resection | Albendazole for 6
months | None | Uneventful | (18) |
| Ahmed et al
(2016) | 1 | 40 | F | Epigastric pain | None | Pancreatic head and
tail | 5.4 | Surgical exploration,
cyst sterilization, and partial cystectomy | albendazole 10
mg/kg/day, for 8 weeks | None | Uneventful | (8) |
| Makni et al
(2012) | 1 | 38 | M | Abdominal pain,
nausea, and vomiting | None | Pancreatic
corpus | 9.4 | Surgical exploration,
dissection of the pancreatic tail, and distal pancreatectomy with
splenectomy | Albendazole 800
mg/day, for three months | None | Uneventful | (9) |
| Suryawanshi et
al (2011) | 1 | 20 | M | Epigastric pain and
occasional vomiting | None | Pancreatic
head | 8 | Laparoscopic cyst
evacuation and omentoplasty | Albendazole 10
mg/kg/day, for 3 months | None | Uneventful | (19) |
| Derbel et al
(2010) | 7 | 25 | F | Left hypochondriac
pain | N/A (all) | Pancreatic
tail | 6 | Laparotomy and
cystectomy | N/A (all) | None | Uneventful
(all) | (20) |
| | | 19 | F | Right hypochondriac
pain | | Pancreatic
tail | 7 | | | | | |
| | | | | | | Pancreatic body and
tail | | Laparotomy and
cystectomy | | None | | |
| | | | | Epigastric
pain | | | | | | | | |
| | | 32 | F | Left hypochondriac
pain and fever | | N/A | 15 | Laparotomy and
cystectomy | | None | | |
| | | 41 | M | Epigastric pain and
jaundice | | | 15 | | | None | | |
| | | | | Epigastric pain and
jaundice | | Pancreatic
head | | Laparotomy,
cystectomy and splenectomy | | | | |
| | | 38 | M | Left hypochondriac
pain and vomiting | | Pancreatic
head | 5 | Laparotomy,
cystectomy, and cholecystectomy | | Acute
pancreatitis | | |
| | | | | | | Pancreatic body and
tail | | | | | | |
| | | 29 | M | | | | 6 | Laparotomy and
cystectomy | | None | | |
| | | 25 | F | | | | 9 | Laparotomy,
pancreatectomy and splenectomy | | None | | |
| Jai et al
(2007) | 1 | 26 | M | Epigastric pain and
pruritus | None | Pancreatic
head | 3 | Laparotomy and
partial cystectomy | None | None | Uneventful | (21) |
| Wu et al
(2021) | 1 | 28 | F | Abdominal pain and
jaundice | None | Pancreatic
head | 5.64 | Laparotomy and
pancreaticoduodenectomy | albendazole 800
mg/day | None | Uneventful | (22) |
| Soin et al
(2019) | 1 | 34 | F | Epigastric
pain | None | Pancreatic
head | 4 | N/A | N/A | N/A | N/A | (23) |
Pancreatic cysts grow over time (0.3-2 cm per year),
and some patients remain asymptomatic for years before being
diagnosed. In symptomatic PHC cases, the location of the cyst
inside the pancreas determines the clinical findings and
complications. The most commonly reported signs and symptoms are
epigastric pain, fever, nausea, vomiting, weight loss and abdominal
fullness (9). However, obstructive
jaundice can develop if the lesion is situated in the head of the
pancreas (22). The patient
described herein presented with severe epigastric pain, fever and
vomiting. He had no signs of jaundice due to the biliary tree
bypass created by the hepaticojejunostomy performed 30 years prior
due to a bile duct stone. The World Health Organization Informal
Working Group on Echinococcosis (WHO-IGWE) classification
categorizes cysts into active, transitional and inactive, which is
relevant for treatment planning and follow-up. In this
classification, CE1 and CE2 are active cysts; the CE3 group
represents transitional cysts, with CE3b being biologically active;
and the CE4 and CE5 groups are inactive, late-stage cysts (24). In the case in the present study,
imaging did not reveal any characteristics indicative of a hydatid
cyst. Instead, there were signs of pancreatitis and the formation
of an abscess. For that reason, it was inappropriate to apply the
WHO classification to this case.
Direct hemagglutination, immune electrophoresis,
skin tests and enzyme-linked immunoassays can be used to support
the diagnosis; however, the validity of these tests is undermined
by false-positive and false-negative results (17). Various imaging modalities are
useful in the diagnosis of pancreatic cysts, including CT, MRI and
ultrasonography (9). In the case
in the present study, an MRI revealed a multilocular cystic lesion
in the head and the uncinate process of the pancreas with a thick
enhancing wall and multiple thick enhancing septae. EUS and ERCP
can be utilized for aspiration or biopsy of the cyst in the event
of an equivocal diagnosis, enabling biochemical and cytological
examination (13). In the case
described herein, the imaging findings did not suggest a hydatid
cyst, leading to the suspicion and consideration of a cystic
neoplasm in the pancreas. Patients diagnosed with echinococcosis
prior to surgery should receive prophylactic anthelminthic
treatment with albendazole (10 mg/kg/day) for 2 to 4 weeks. This
treatment should be continued for at least 4 weeks post-surgery to
lower the risk of anaphylaxis (23). The patient in the present study did
not receive anthelminthic treatment prior to the surgery as a
diagnosis could not be made before the surgical procedure.
The EUS revealed a large, complex cystic-solid mass
in the pancreatic body. A cytological examination of the fluid
aspirated during the EUS revealed pyogenic inflammation with no
evidence of malignancy. Based on the location of the hydatid cyst,
various surgical techniques have been utilized for treatment,
including pericystectomy, complete excision of the cyst,
cysto-enteric anastomosis, distal pancreatectomy, capitonnage, open
surgery and laparoscopy (7,17,19).
In the present case report, the patient underwent a total
pancreatectomy with partial excision of the attached second portion
of the duodenum, as well as a splenectomy. He was administered a
4-week course of albendazole at a dose of 800 mg/day. During the
surgery, utmost care should be exercised to mitigate the risk of
contamination and subsequent recurrence. This involves minimizing
the spillage of cyst contents through the application of scolicidal
treatments, such as 0.5% cetrimide or 20% hypertonic saline
(8). In the case in the present
study, the entire pancreas was removed, and no chance was left for
the intraoperative spillage of the cyst contents. A
histopathological examination confirmed that the hydatid cyst
caused chronic xanthogranulomatous.
A limitation of the present case report is the
absence of data to definitively confirm that the death of the
patient was due to diabetes complications.
In conclusion, pancreatic hydatid cysts are
exceedingly rare and prone to misdiagnosis. Surgery remains the
cornerstone of treatment, with a definitive diagnosis typically
established through histopathological examinations.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
FHK and OHGH were major contributors to the
conception of the study, as well as to the literature search for
related studies. HAA and REA were involved in the literature
review, study design and writing of the manuscript. HHKA, DAE, DTG,
KFHH, BAA and DHA were involved in the literature review, the
design of the study, the critical revision of the manuscript, and
in the processing of the table. FHK and BAA confirm the
authenticity of all the raw data. RMA was the pathologist who
performed the histopathological diagnosis. SHT was the radiologist
who assessed the case. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hussein DM, Kakamad FH, Amin BJH, Baqi DH,
Tahir SH, Salih AM, Ali RK, Fattah FH, Ahmed GS, Abdalla BA, et al:
Hydatid cyst in the pulmonary artery; a meta-analysis. Barw Med J.
1:22–29. 2023.
|
|
2
|
Thyo EM: Barw Medical Journal, why?! Barw
Med J. 1(1)2023.
|
|
3
|
Abdullah HO, Abdalla BA, Mohammed-Saeed
DH, Tahir SH, Fattah FH, Hassan SJ, Hamasalih HM, Amin BJH, Salih
AM, Noori SS, et al: A comprehensive study of pericardial hydatid
cyst; systematic review and meta-data presentation. Barw Med J.
1:7–18. 2023.
|
|
4
|
Alsaid B, Alhimyar M and Rayya F:
Pancreatic hydatid cyst causing acute pancreatitis: A case report
and literature review. Case Rep Surg. 2018(9821403)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Salamone G, Licari L, Randisi B, Falco N,
Tutino R, Vaglica A, Gullo R, Porello C, Cocorullo G and Gulotta G:
Uncommon localizations of hydatid cyst. Review of the literature. G
Chir. 37:180–185. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Muhedin SS, kakamad FH, Tahir SH, Baba HO,
Salih AM, Qaradakhy AJ, Ali RK and Abdulla BA: Hydatid cyst in the
neck mimicking lymphangioma; a case report with a brief literature
review. Otolaryngol Case Rep. 25(100476)2022.
|
|
7
|
Khalifa R, Nasser F, Elsetouhy A and Farag
I: Hydatid cyst of the neck. A case report and literature review.
Egypt J Ear Nose Throat and Allied Sci. 17:103–105. 2016.
|
|
8
|
Ahmed Z, Chhabra S, Massey A, Vij V, Yadav
R, Bugalia R, Kankaria J and Jenaw RK: Primary hydatid cyst of
pancreas: Case report and review of literature. Int J Surg Case
Rep. 27:74–77. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Makni A, Jouini M, Kacem M and Safta ZB:
Acute pancreatitis due to pancreatic hydatid cyst: A case report
and review of the literature. World J Emerg Surg.
7(7)2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Tatar OC, Şimşek T, Güler SA and Cantürk
NZ: An atypical presentation of hydatid disease, accompanied by a
pancreatic pseudocyst: A case report. Iran J Parasitol. 17:277–281.
2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Agha RA, Franchi T, Sohrab C, Mathew G and
Kirwan A: SCARE Group. The SCARE 2020 guideline: Updating consensus
Surgical Case Report (SCARE) guidelines. Int J Surg. 84:226–230.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Muhialdeen AS, Ahmed JO, Baba HO, Abdullah
IY, Hassan HA, Najar KA, Mikael TM, Mustafa MQ, Mohammed DA, Omer
DA, et al: Kscien's List; A new strategy to discourage predatory
journals and publishers (Second Version). Barw Med J. 1:24–26.
2023.
|
|
13
|
Baba HO, Salih AM, Abdullah HO, Hassan HA,
Ali RK, Kakamad FH, Salih RQ and Hussein H: Primary hydatid cyst of
the posterior neck; a case report with literature review. Int J Sur
Open. 40(100449)2022.
|
|
14
|
Ma T, Wang Q, Hao M, Xue C, Wang X, Han S,
Wang Q, Zhao J, Ma X, Wu X, et al: Epidemiological characteristics
and risk factors for cystic and alveolar echinococcosis in China:
An analysis of a national population-based field survey. Parasit
Vectors. 16(181)2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kothiya PK, Gupta V, Sarawagi R,
Jayashankar E, Sharma J, Wani H, Balaji K and Roshny J: Isolated
primary hydatid cyst of the pancreas: Management challenges of a
cystic masquerade. Ann Hepatobiliary Pancreat Surg. 26:401–406.
2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cherouaqi Y, Nadi A, Idrissi A, El Idrissi
Lamghari A and Rouibaa F: Hydatid cyst of the pancreas: An unusual
cause of abdominal pain. Cureus. 13(e20614)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ozsay O, Gungor F, Karaisli S, Kokulu I
and Dilek ON: Hydatid cyst of the pancreas causing both acute
pancreatitis and splenic vein thrombosis. Ann R Coll Surg Engl.
100:e178–e180. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Bakkaly AE, Merouane N, Dalero O, Oubeja
H, Erraji M, Ettayebi F and Zerhouni H: Primary hydatid cyst of the
pancreas of the child: A case report. Pan Afr Med J.
27(229)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Suryawanshi P, Khan AQ and Jatal S:
Primary hydatid cyst of pancreas with acute pancreatitis. Int J
Surg Case Rep. 2:122–124. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Derbel F, Zidi MK, Mtimet A, Hamida MBH,
Mazhoud J, Youssef S, Jemni H, Ali AB and Hamida RBH: Hydatid cyst
of the pancreas: A report on seven cases. Arab J Gastroenterol.
11:219–222. 2010.
|
|
21
|
Jai SR, El Hattabi K, Bensardi F, Chehab
F, Khaiz D and Bouzidi A: Primary hydatid cyst of the pancreas
causing obstructive jaundice. Saudi J Gastroenterol. 13:191–193.
2007.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wu Y, Gong J, Xiong W, Yu X and Lu X:
Primary pancreatic hydatid cyst: A case report and literature
review. BMC Gastroenterol. 21(164)2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Soin P, Sharma P and Kochar PS: Pancreatic
echinococcosis. Proc (Bayl Univ Med Cent). 32:85–87.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
World Health Organization (WHO): Puncture,
aspiration, injection, re-aspiration: an option for the treatment
of cystic echinococcosis. WHO, Geneva, 2001.
|