Introduction
According to clinical data, malnutrition is observed
in 50-80% of patients with gastrointestinal cancer, and it is
associated with poor clinical outcomes and longer periods of
hospitalization (1,2). In particular, patients with
pancreatic or gastric cancer have been shown to have the highest
frequency of weight loss (3).
However, the clinical manifestations of malnutrition, particularly
micronutrient deficiency, which is not apparent immediately, can
exist for a long period of time before the clinical signs of severe
malnutrition and its complications appear (4,5).
The present study describes the case of a female
patient who had previously undergone a gastrectomy, as well as a
subsequent pancreaticoduodenectomy with cholecystectomy,
bile-jejunostomy, pancreatojejunostomy and gastrojejunostomy. For
this reason, the distal gastric resection, duodenum and partial
pancreatic resection, gallbladder resection and intestinal
anastomoses in the post-operative reconstruction of the digestive
tract, caused poor digestive function, ultimately resulting in
malnutrition and micronutrient deficiencies. The aim of the present
case report was to share the clinical experience of the authors
with the clinical manifestations of malnutrition and micronutrient
deficiency following gastrointestinal surgery.
Case report
A 70-year-old female patient presented in the
outpatient cancer clinic for a follow-up appointment and was
admitted to Viet Duc University Hospital (Hanoi, Vietnam) for
treatment in the Oncology Department on February 1, 2023.
According to her medical history, the patient had
undergone a partial gastrectomy with gastroduodenostomy (Billroth
I) in January, 2009 for stomach cancer and pancreaticoduodenectomy
due to tumor recurrence with lymph node metastases of the head of
the pancreatic region in March, 2020. She had undergone seven
cycles of adjuvant chemotherapy and this was then discontinued due
to significant toxicities and intolerance.
Upon a physical examination at the time of
admission, the patient was alert, fatigued and hemodynamically
stable. She had mildly pale skin and mucous membranes. The
peripheral lymph nodes were not palpable. The abdomen was soft,
non-tender, with deep palpation, and no masses were present.
The notable physical findings in the patient were
generalized edema with mild facial edema, moderate bilateral
pitting edema of the lower extremities and no ascites. Accompanied
by dry cutaneous lesions, red stretch marks were observed on her
extremities; these were more evident in the lower limbs. Her legs
were red and swollen, with small ulcers, and the patient had
refused to walk for 2 days due to pain (Fig. 1). There were no oral mucosal
lesions. There were no other notable findings from the physical
examination.
The patient had a nutrition consultation on February
2, 2023. The assessment of her nutritional status was PG-SGA C, her
height was 160 cm, her current weight was 42 kg and her body mass
index was 16.4 kg/m2 (with edema). She had lost weight
unintentionally; her normal healthy weight had been 53 kg and she
had reached 38 kg 1 month prior. The nutrition-focused physical
examination revealed moderate to severe loss of muscle and
subcutaneous fat. There were signs of micronutrient deficiency,
such as the partial loss of lingual papillae on the surface of the
tongue edges, dry and pale skin combined with ulcers, and
perifollicular petechiae hemorrhage on her anterior shins
bilaterally.
The patient stated that she had not been eating well
due to anorexia, and had a poor appetite from the second surgery in
2020. The 24-h food recall revealed that her meals consisted of
rice, porridge and milk with 5-6 meals/day, with a total energy
count of 900-1,000 kcal/day, a protein intake of 35-40 g/day, and a
poor vegetable and fruit intake. Her daily intake was noted to
average 50-60% of the nutritional demand. She had normal bowel
movements once per day. Currently, she was being treated with
Creon® at 25.000 UI orally, three times daily. She did
not receive any vitamins or mineral supplementation.
Laboratory tests revealed hypoproteinemia with an
albumin level of 24.1 g/l, prealbumin level of 3.6 mg/dl and lack
of a certain micronutrients, indicated as follows: Zinc, 6.5
µmol/l; iron, 7.8 µmol/l; ferritin, 18.5 µg/l; corrected calcium,
2.1 mmol/l; and 25-OHD, 10.8 ng/ml. A complete blood count revealed
megaloblastic anemia, with a red blood cell count of 2.85 T/l, a
hemoglobin count of 93 g/l and a hematocrit of 0.29%. Her mean
corpuscular volume/mean corpuscular hemoglobin/mean corpuscular
hemoglobin concentration ratio was 102.6/32.8/320.
Other biochemical indicators of glucose (3.64
mmol/l), electrolytes (sodium, 140.5 mmol/l; potassium, 3.6 mmol/l;
chloride, 107.5 mmol/l), magnesium (0.85 mmol/l), phosphorus (1.15
mmol/l), urea (7.54 mmol/l) and creatinine (54.23 µmol/l) were
within the normal range, and the levels of liver enzymes and
bilirubin were slightly elevated as follows: aspartate
aminotransferase, 67.7 U/l; alanine aminotransferase, 61.98 U/l;
total bilirubin, 31.4 µmol/l; direct bilirubin, 13.4 µmol/l.
The patient's serum levels of carcinoembryonic
antigen (10.94 ng/ml) and cancer antigen 19-9 (87.69 U/ml) were
slightly elevated. A contrast-enhanced computed tomography was
performed and this ruled out recurrent cancer. No thrombus in the
veins and arteries was observed on the Doppler ultrasound of the
lower extremities on both sides. A clinical immunology-allergy
specialist consultation was requested and immunology testing was
performed to rule out vasculitis. Accordingly, the patient was
diagnosed with macrocytic anemia, micronutrient deficiency and
severe malnutrition.
The patient had a risk of refeeding syndrome;
however, her phosphorus (1.15 mmol/l), potassium (3.6 mmol/l) and
magnesium (0.85 mmol/l) levels were normal; thus, it was decided to
provide intensive nutrition from oral feeding combined with
supplemental parenteral nutrition. The patient received dietary
advice and was encouraged to take the medical formula
(Peptamen®) as an oral nutritional supplement with short
peptide enteral nutrition preparationsto potentially improve
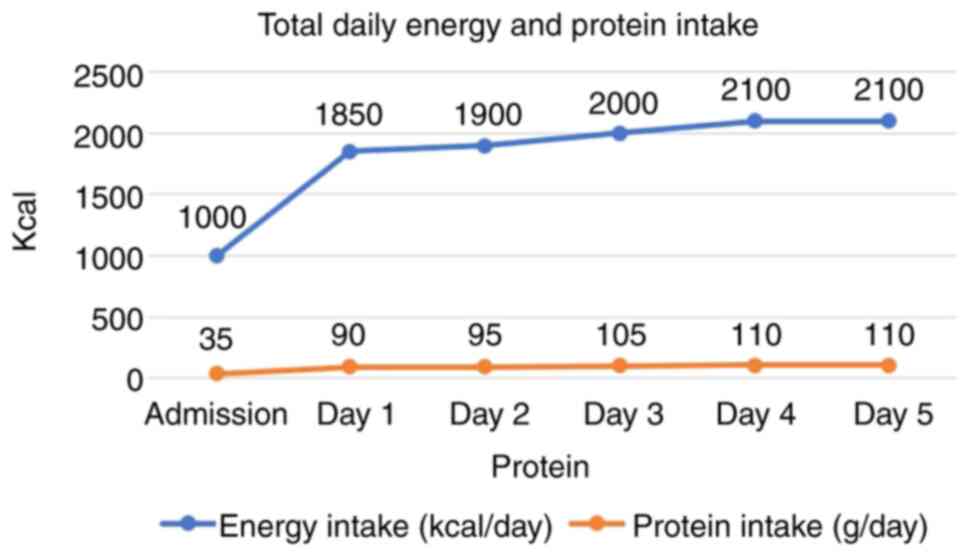
absorption and optimal micronutrient intake. The total daily energy
and protein intake of the patient is presented in Fig. 2.
As partial parenteral nutrition, the patient
received 500 ml of 10% Aminoplasmal (acid amin)® and 250
ml of 20% SMOFlipid®(Lipid). She was also administered
daily infusions of 20% human albumin solution. Parenteral
micronutrients, including multivitamins, trace elements and
electrolytes, were provided daily. She also received daily an
intramuscular injection of vitamin B12 (1,000 mcg), as well as via
oral route daily, 20 mg zinc, 3,000 UI vitamin D3 and B complex
C® (vitamin B1 15 mg, vitamin B2 10 mg, vitamin B6 5 mg,
Vitamin PP 50 mg and vitamin C 100 mg) twice a day, Energy
Pharmaton® (multivitamins) once a day, Tardyferon
B9® (50 mg of elemental iron as ferrous sulfate with
0.35 mg folic acid) twice a day and 500 mg of calcium as calcium
citrate twice a day. Creon® was also administered to the
patient for use at home to better correct pancreatic exocrine
insufficiency (PEI) with doses of 50,000 units of lipase with meals
and 25,000 units with each snack, with a total of nine capsules of
Creon® at 25.000 UI per day.
The symptoms of the patient markedly improved
following 5 days of treatment with rapid cutaneous improvement, and
the resolution of her edema. Her weight increased from 38 to 42 kg.
Her lower legs on both sides were no longer red and swollen, the
small ulcers were dry, and healing and red stretch marks gradually
developed scabs (Fig. 3). The
appetite of the patient had increased, with an improvement in the
quality of her dietary intake. She was able to mobilize both lower
extremities without pain and was discharged in a good clinical
condition from the hospital on the 6th day of admission. Nutrition
counseling was provided to the caregiver prior to discharge.
Discussion
Following gastrointestinal surgeries, the rapid and
uncontrolled passage of food into the intestine leads to a
decreased digestibility and absorption of macronutrients and
micronutrients due to the absence of the jejunum and duodenum, and
the damage to the extrinsic parasympathetic innervation, combined
with a lack of coordination of the gallbladder bile and pancreatic
secretion into the duodenum. Malabsorption may result from the
incomplete digestion of proteins and lipids due to the absence of
pepsin and hydrochloric acid, combined with late contact of the
ingested food with the pancreatic juice. In addition, the more
important cause, malabsorption, is a consequence of exocrine
pancreatic insufficiency following pancreaticoduodenectomy
(6). The obvious symptoms that can
be seen are the progressive worsening of malnutrition with weight
loss, and a decrease in the muscle mass fat mass of the patient.
This is also accompanied by anemia, edema and malnourishment due to
malnutrition and micronutrient deficiencies. In such cases, the
amount of malabsorption leads to clinical malnutrition that
necessitates nutritional support, including parenteral
nutrition.
PEI is defined as a deficiency of exocrine
pancreatic enzymes resulting in an inability to maintain normal
digestion (7). The factors that
contribute to PEI following pancreatic surgery are the loss of
pancreatic tissue volume, extensive denervation following lymph
node dissection, the asynchronous mixing of pancreatic-biliary
secretions with the meal, and a surgically altered anatomy
(6,8). In addition, an increased incidence of
pancreatic insufficiency following upper gastrointestinal surgery
has also been observed, where extra-pancreatic factors impair the
final activity of pancreatic enzymes (9). These consequences lead to the reduced
absorption of protein, fat and fat-soluble vitamins, leading to
weight loss and malnutrition. Fat malabsorption is the predominant
cause of the symptoms of pancreatic steatorrhea, resulting in
weight loss, as well as deficiencies in the fat-soluble vitamins A,
D, E and K (10). In addition, fat
absorption may decrease following partial or total gastrectomy, due
to the lack or decrease in the levels of digestive enzymes and less
contact between ingested food, digestive enzymes and biliary salts
(6).
Pancreatic enzyme replacement therapy is indicated
for the conditions described above presenting with clinically clear
steatorrhea, weight loss, or symptoms related to maldigestion and
malabsorption. For adults, therapy should commence with doses of
50,000 units of lipase with main meals, and half the dose to be
taken with a snack (6,7,11).
In the patient in the present study, manifestations of pancreatic
insufficiency were not apparent, possibly as the patient had
previously been supplemented with pancreatic enzymes, but still had
symptoms of anorexia, bloating and progressive weight loss without
steatorrhea. There was no accurate test available to diagnose this,
such as the measurement of fecal elastase-1 or 3-day fecal fat
quantification. Thus, based on clinical experience, the dose of
pancreatic enzymes was increased to optimize treatment after
determining the method of drug administration and the patient's
compliance and need to monitor her response.
Dermatitis resembling flaky paint-hyperpigmented
areas on arms, thighs and calves, is possibly due to deficiencies
in protein. In addition, there can also be skin damage due to a
lack of essential fatty acids and/or a combination of multiple
micronutrient deficiencies such as zinc, vitamin C, niacin and
riboflavin (12).
A closer look at vitamins, as well as trace
elements, should be considered to assess for a decreased intake of
foods and post-operative malabsorption and the need for
supplementation. Over time, virtually all gastric surgical
procedures potentially lead to micronutrient deficiencies due to
the resection or exclusion of functionally active gastric mucosa
necessary for gastric acid and intrinsic factor secretion, which in
turn, is essential for correct micronutrient absorption. The acid
environment of the stomach facilitates protein degradation,
allowing for the release and dissolution of calcium, magnesium,
iron and other trace elements for eventual absorption, and is also
essential for the absorption, secretion and activation of ascorbic
acid (13). Additionally, the
resection of the duodenum during the pancreaticoduodenectomy may
place patients at risk of developing iron and mineral deficiencies.
Zinc deficiency has been reported in up to 68% of patients
undergoing pancreas resection, predominately following
pancreaticoduodenectomy, and is associated with PEI (14).
The majority of water-soluble vitamins are easily
absorbed from the proximal gastrointestinal tract. The rapid
transit of food through the intestine allows for the decreased time
absorption for these vitamins. Fat-soluble vitamins and essential
fatty acids are considered to be absorbed in the mid- and distal
ileum, due to the necessity of bile acid and pancreatic lipase to
facilitate absorption; therefore, these are affected by conditions
with fat malabsorption, as in the case of the patient described
herein. Calcium absorption begins due to the intragastric acid pH
favoring the dissolution of calcium salts to form soluble calcium
chloride, a step facilitating the proper absorption of this ion
through vitamin D-dependent transcellular transport in the duodenum
and proximal jejunum (13).
Following the removal of the duodenum during a
pancreaticoduodenectomy, patients exhibit markedly diminished
calcium absorption.
Another notable finding in this patient is
megaloblastic anemia, which may be due to vitamin B12, and/or folic
acid (vitamin B9) deficiencies. In addition, anemia is caused by a
combination of iron deficiency.
Nutritional anemias resulting from a vitamin B12,
folate, or iron deficiency are common in individuals who have had a
gastrectomy, both total or subtotal gastrectomy. A previous
retrospective cohort study on long-term gastric cancer survivors
without recurrence or metastasis following gastrectomy revealed
that the cumulative incidence rate of anemia following surgery
exhibited a linear increase, presenting as in 18.7% in the 1st
year, and increasing to 39.5% in the 5th year (15). Iron deficiency anemia is found in
~30% of patients who have undergone a gastrectomy, due to a reduced
iron intake and defects in iron absorption in the bypass of the
duodenum and upper jejunum, or chronic bleeding in the gastric
mucosa. The prevalence of vitamin B12 deficiency anemia is ~50% in
gastrectomy cases caused by a lack of intrinsic factor secretion
following surgery (15). A key
role is played by the corpus oxyntic mucosa composed of parietal
cell mass depletion, whose main function is gastric acid secretion
and intrinsic factor production, mostly located in the body, and to
a lesser extent in the antrum and fundus (13).
Vitamin deficiencies are typically subclinical and
require testing for diagnosis. However, due to the lack of these
laboratory tests at the Viet Duc University Hospital, the authors
were only able to perform a few micronutrient tests and mainly
administer empiric treatment in the case that symptoms of
deficiency were suspected. Note that ferrous iron is the preferred
form due to its high bioavailability. Vitamin C has been shown to
enhance iron absorption and increase the proliferation of dermal
fibroblasts, a function critical for wound healing (16).
In conclusion, by describing the present clinical
case, the present study hopes to highlight the impacts of nutrition
on the clinical outcomes of patients following gastrointestinal
cancer surgery. Post-discharge individualized dietary counseling
and regular nutrition assessment are effective interventions to
reduce post-operative weight loss and malnutrition. Deficiencies in
several micronutrients, such as iron, vitamin B12, calcium and
ascorbic acid may lead to potentially severe consequences when not
promptly diagnosed and treated. Thus, it is critical to routinely
monitor patients who have undergone any previous gastric surgery
for micronutrient deficiency. Therefore, the success of surgery not
only helps the patient to remove cancerous tumors, but also helps
the body to recover and function following surgery, the pivotal
role of nutritional interventions.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors (TTD, PLTP, PTN, AGP and HNV)
contributed to the conception and design of the study. Material
preparation was performed by TTD and HNV. Data collection and
analysis were performed by PLTP, PTN and AGP. Analysis was
performed by PTN and AGP. The first draft of the manuscript was
written by TTD, PTN and HNV, and all authors commented on previous
versions of the manuscript. TTD and PTN confirm the authenticity of
all the raw data. All authors have read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for her participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Barker LA, Gout BS and Crowe TC: Hospital
malnutrition: Prevalence, identification and impact on patients and
the healthcare system. Int J Environ Res Public Health. 8:514–527.
2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Corish CA and Kennedy NP: Protein-energy
undernutrition in hospital in-patients. Br J Nutr. 83:575–591.
2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tisdale MJ: Cachexia in cancer patients.
Nat Rev Cancer. 2:862–871. 2002.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Saunders J and Smith T: Malnutrition:
Causes and consequences. Clin Med (Lond). 10:624–627.
2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Norman K, Haß U and Pirlich M:
Malnutrition in older adults-recent advances and remaining
challenges. Nutrients. 13(2764)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Altomare DF and Rotelli MT (eds):
Nutritional support after gastrointestinal surgery. Cham: Springer
International Publishing, 2019.
|
|
7
|
Struyvenberg MR, Martin CR and Freedman
SD: Practical guide to exocrine pancreatic insufficiency-breaking
the myths. BMC Med. 15(29)2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ghaneh P and Neoptolemos JP: Exocrine
pancreatic function following pancreatectomy. Ann N Y Acad Sci.
880:308–318. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lee AHH and Ward SM: Pancreatic exocrine
insufficiency after total gastrectomy-a systematic review. J
Pancreas. 20:130–137. 2019.
|
|
10
|
Gilliland TM, Villafane-Ferriol N, Shah
KP, Shah RM, Tran Cao HS, Massarweh NN, Silberfein EJ, Choi EA, Hsu
C, McElhany AL, et al: Nutritional and metabolic derangements in
pancreatic cancer and pancreatic resection. Nutrientsc.
9(243)2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Capurso G, Traini M, Piciucchi M,
Signoretti M and Arcidiacono PG: Exocrine pancreatic insufficiency:
Prevalence, diagnosis, and management. Clin Exp Gastroenterol.
12:129–139. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hoffman M, Micheletti RG and Shields BE:
Nutritional dermatoses in the hospitalized patient. Cutis 105: 296,
302-308.E1-E5, 2020.
|
|
13
|
Carabotti M, Annibale B and Lahner E:
Common pitfalls in the management of patients with micronutrient
deficiency: Keep in mind the stomach. Nutrients.
13(208)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yu HH, Yang TM, Shan YS and Lin PW: Zinc
deficiency in patients undergoing pancreatoduodenectomy for
periampullary tumors is associated with pancreatic exocrine
insufficiency. World J Surg. 35:2110–2117. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jun JH, Yoo JE, Lee JA, Kim YS, Sunwoo S,
Kim BS and Yook JH: Anemia after gastrectomy in long-term survivors
of gastric cancer: A retrospective cohort study. Int J Surg.
28:162–168. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Bechara N, Flood VM and Gunton JE: A
systematic review on the role of vitamin C in tissue healing.
Antioxidants (Basel). 11(1605)2022.PubMed/NCBI View Article : Google Scholar
|