1. Introduction
Children commonly present with acute pain that is
either localized or generalized in the body. The pain may
occasionally be underrated and thus inadequately treated with the
possible consequence of significant issues for the health of the
affected child. The revised International Association for the Study
of Pain defines pain as an unpleasant sensory and emotional
experience associated with or resembling that associated with
actual or potential tissue damage (1). The clinical assessment of pain in
pediatric patients must include several aspects, such as the
psychological history of the child and their family, a thorough
physical examination, and when necessary, laboratory analyses and
radiological findings. Clinical indications should be drawn from
the quality, location, duration, frequency and intensity of the
pain. Pain is regarded as a symptom of an underlying condition, and
perceptions of pain may be felt in accordance with different
factors, such as the age, cognition, sex, previous pain
experiences, temperament and psychological attitude of each patient
(1). Pain has been temporally
distinguished as acute and chronic and arbitrarily defined as acute
when it lasts for 3 months and chronic when the duration is 6
months (2,3). Acute pain may also be referred to as
a painful episode that is transitory and only lasts until the
noxious stimulus ends or the underlying damage or pathological
event(s) have been removed. Acute pain may further be a temporal
manifestation of a chronic disorder.
Pain is a subjective experience (4). Despite the development and greater
awareness of instruments, guidelines, and educational and training
strategies, recent studies have shown that clinicians still do not
pay sufficient attention to pain management, particularly in
children. Inadequate clinical evaluations, inappropriate scale
measurements and the treatment of acute pain in various situations
have been clearly identified as contributing to this issue
(5). In children who are <2
years of age, the situation is more pronounced, as the pain, even
if treated, is sometimes managed with incorrect or inadequate
dosages (5). Acute pediatric pain
evaluations must include the pain quality, characteristics,
location, onset, duration, aggravating and alleviating factors, and
the impact on function (6-9).
In children and adolescents, the intensity and quality of pain may
be assessed using self-report measures, such as drawings, images of
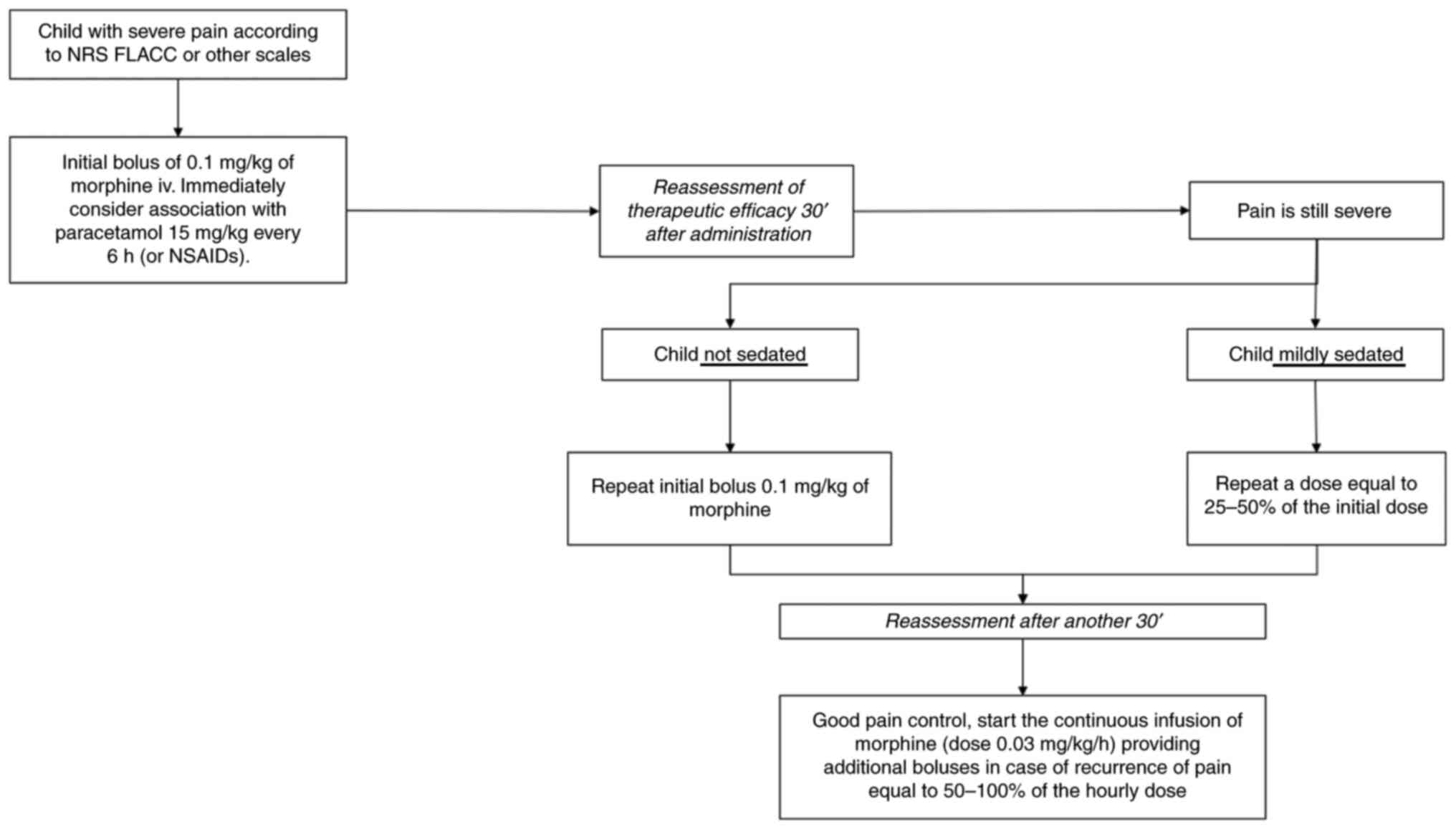
faces, graded color intensities and other systems (8). The aim of the present review was
therefore to report the modalities used to measure the presence and
grades of acute pain in children, and the different strategies to
approach and treat such pain in different clinical situations. A
flowchart for the management of children with severe pain is
presented in Fig. 1.
2. Literature search methods
A literature review was conducted by collecting
articles, including clinical trials, primary research articles and
reviews from online bibliographic databases (i.e., MEDLINE, Embase,
PubMed, Cochrane Central and Scopus) covering the period from
January, 2000 to December, 2022. The key words used for the search
were derived from medical subject heading terms, namely ‘pain and
children (pediatric)’, ‘pediatric’, ‘child’, ‘infant’, ‘toddler’ OR
pain therapeutic strategies (‘analgesic’ or ‘analgesia’) OR pain
pharmacological treatments OR opioid medications OR pain and
nonpharmacological therapies. Relevant studies were examined
manually and are included in the present reference list. As the
subject of the present study was notably wide, the literature data
that were included were those that were, in the authors' opinion,
more representative.
Once the initial results had been collected, two
reviewers analyzed the titles and abstracts and screened them for
the inclusion criteria, which were studies with any level of
evidence that reported clinical results published over the past 22
years (2000-2022). Comparative, cross-sectional, retrospective,
prospective and survey studies, case series, and case reports on
the pediatric population were included. All the articles written in
languages other than English were excluded. Articles that dealt
with different topics, had poor scientific methodologies, or were
without an accessible abstract were also excluded. In addition,
articles that did not match the inclusion criteria were ruled out.
After removing the duplicate records, the main search articles that
related to the study were included.
3. Acute pain in children
Diverse events cause acute pain in children, which
affects various body organs and requires treatment by different
types of specialists. Numerous clinical studies have addressed
scale measurements of pain and clinical trials for pain treatment.
However, to the best of our knowledge, no common agreement has been
reached on the methods to use to measure pain in children or
treatment strategies, although several options have been proposed
for each topic. The present literature review indicates that a wide
range of scales are used to measure acute pediatric pain, with
different options employed for pharmacological and
non-pharmacological treatment strategies.
The causes and treatment of acute pain are
significant challenges, particularly among children and
adolescents. Current guidelines recommend assessing and relieving
(1,3,8) pain
in all children in all instances; yet in clinical practice,
particularly in the pediatric population, management is suboptimal
and not completed (5). In a survey
of acute pain management in children that involved 929 Italian
pediatricians, Marseglia et al (10) reported the results obtained for
6,335 patients with a uniform distribution of different types of
acute pain. Pain was more frequently found to be of moderate
intensity (42.2%, P<0.001) and a short duration (within a few
days: 98.4%, P<0.001). Only 50.1% of the respondents used an
algometric scale to measure pain, and 60.5% always prescribed a
treatment. In the group of children with mild to moderate pain
(n=4,438), the most commonly used first-line nonopioid treatments
were ibuprofen (53.3%) and acetaminophen (44.4%) (10). In the authors' experience,
analgesics can be used without causing complications; however, the
side-effects of these analgesics should be taken into
consideration, as these can aggravate issues that already present
in patients with comorbidities. For example, non-steroidal
anti-inflammatory drugs (NSAIDs), cause gastric toxicity, which
adds to basic reflux, and a reduction in renal flow, which adds to
the poor intake of water. The hepatotoxic effect of paracetamol can
contribute to malnutrition and the effects of cytochrome inhibitor
drugs. Opioids can worsen constipation, nausea and dystonia and can
cause itching, which the child will not be able to scratch, as well
as urinary retention (globus vesicalis), particularly if the child
is receiving glycopyrrolate therapy.
The World Health Organization (WHO) recommends a
step approach, with pain divided into mild, moderate and severe
(11). In the case of mild pain,
the suggested treatment is non-opioid medications. For moderate
pain, weak opioids should be used, with strong opioids used for
severe pain. The most difficult task in the evaluation is the
individuation of the pain condition and the application of the
appropriate therapy.
In the assessment of acute pain in children, among
the other key factors, are the evaluation of the grade of the pain
and the correct treatment required for its attenuation or
cessation.
4. Scales for pain grade measurement in
pediatric patients
Various tools are available to measure the grades of
acute pain in children. A list of scales to measure the properties
of self-reported pain intensity is presented in Table I. No single scale is advocated as
optimal for use with all types of pain or across the developmental
age span. Scales must be applied with due consideration of several
factors, including the age of the child, the clinical localization
and severity of the pain, and the cognitive and psychological
structure of the child (9,12-14).
In children with neurocognitive disabilities and in the context of
emergency rooms/urgent situations, the measurement of the severity
of pain becomes more complex and difficult. The
inability/difficulty of children to communicate verbally or
non-verbally, the presence of stereotyped or involuntary movements,
altered facial and body expressiveness, and sensory disabilities
may limit the validity of pain measurement.
 | Table IAcute pain scales. |
Table I
Acute pain scales.
| Scale name | Type of scale | Age | Scoring system | Scale | Indications |
|---|
| Faces Pain Rating
Scale |
Self-evaluation | 4-8 years | Picture-based scale
where child select 1 of 6 faces to represent their pain
experience | 0-10 (0-3 mild, 4-6
moderate, 7-10 severe) | Cognitively
adequate child with motor impairment |
| Numerical Rating
Scale (NRS) | | >8 years | Ask the patient to
assign a number to their pain (0 no pain, 10 worst pain ever) | 0-10 (0-3 mild, 4-6
moderate, 7-10 severe) | Cognitively
adequate child without motor impairment |
| FLACC (Face Legs
Activity Cry Consolability) |
Hetero-valuation | 0-3 years | 5 Behaviour items
each scored from 0 to 2 to a total of 10 points | 0-10 (0-3 mild, 4-6
moderate, 7-10 severe) | |
| FLACC-R
(Revised) | | 2 months-7 years or
any age nonverbal or with intellectual impairment | Compared to ‘FLACC’
includes additional pain behaviours often found in children who are
non-verbal or with cognitive impairment | 0-10 (0-3 mild, 4-6
moderate, ≥7 severe) | |
| NCCPC-R
(Non-Communicating Children's Pain Checklist-Revised) | | 3-18 years | Scale with 30 total
items with 7 subscales (vocal, social, facial, activity, body and
limbs, physiological, and eating/sleeping) each item scored from 0
to 3 according to the frequency of its occurrence. | Total score of ≥7
indicates pain. | Children with
cognitive impairment, non-verbal or unable by age to provide pain
self-assessment |
| PPP (Pediatric Pain
Profile) | | 1-18 years | Two-part
individualized measure allowing caregivers to describe their
child's pain behaviours on good days and bad days and complete a
20-item measure scored on a 0-3 scale | Total score of ≥14
indicates clinically significant pain, 10-19 is mild, 20-29 is
moderate, 30-39 is severe, and >40 is very severe pain. | |
| EVENDOL (EValuation
ENfant DOuLeur) | | 0-7 years | Five items (vocal
or verbal expression, Facial expression, movements, postures,
interaction with the environment) evaluated at rest and at
mobilization, | Total score ranges
from 0 to 15. Treatment threshold ≥4 | |
| Color Analogue
Scale (CAS) | | 4-10 years | Gradations in
colour, area and length so as to easily associate scale positions
with diffused levels of pain intensity | The back of the
tool has a numerical rating scale providing means to assign a
numerical pain score between 1 and 10 cm in 0,25 cm increment | |
5. Therapeutic strategies
Various types of acute pediatric treatments are
available depending on the age of the patient, the intensity of the
pain, and the characteristics and types of organs affected. As the
topic is extremely wide, the present review summarizes the
treatment strategies more frequently used. The therapeutic
strategies can be divided into non-pharmacological techniques and
pharmacological drugs. The use of several other analgesics is not
considered (e.g., nitrous oxide, methoxyflurane, ketamine,
diamorphine) as this was beyond the scope of the present
review.
Non-pharmacological techniques
Research has shown that non-pharmacological options,
including physical and psychological strategies, may be helpful in
treating pain. Children may benefit from cognitive behavioral
strategies, such as the use of imagery or relaxation. The
application of non-pharmacological techniques has been employed to
control pain, stress, and anxiety in children and their parents
(9). The present review provides a
summary of some of the suggested non-pharmacological strategies
aimed at the attenuation or cessation of acute pain in children. In
their review of 39 trials with 3,394 participants, Uman et
al (15) examined the effects
of psychological interventions on needle-related procedural pain
and distress in children and adolescents aged 2-19 years. They
found strong evidence in support of distraction and hypnosis for
needle-related pain and distress in this population (15). Similarly, Accardi and Milling
(16) reported the effectiveness
of hypnosis in reducing procedure-related pain in children. A
systematic literature search on non-pharmacological interventions
used for pain management in children in emergency departments was
conducted by Wente (9). Among the
14 articles examined, distraction was used in 10 studies, sucrose
in two studies, cold application in one study, and parental holding
and positioning in one study. Furthermore, decreased pain, distress
and anxiety in the parent, child, and/or observer were noted when
these procedures were used (9).
Cognitive-behavioral strategies should be related to the age and
degree of cognitive development of the patient: The oral
administration of sucrose and glucose, kangaroo care, tactile
stimulation, rocking, singing and soft music, and an environment
with soft, fused lights can be effective for infants. For children
of school age, the application of cold spray, ice, hot moist packs,
massaging and pressure can be useful and satisfying. Furthermore,
the use of bandages, dressings and splints are other simple systems
that can be used to reduce pain symptoms and anxiety, as these
cover the view of the ‘wound’ that is causing psychophysical
distress in the child (2). A study
involving 98 children and 97 control children/parents examined the
beliefs of parents about pain and the efficacy of a parental
educational intervention on pain intensity in children and the
experience of pain-related unpleasantness at 24 h post-discharge
from the emergency department (17). According to the researchers, the
active participation of parents in their child's pain management
may be more effective than a passive educational intervention
(17). Music therapy has also been
shown to be a form of distraction that alleviates some types of
pain and distress experienced by children undergoing medical
procedures in a pediatric emergency department (18). In a previous comprehensive review
that included 13 studies and involved 778 patients, the effects of
music therapy and opioid treatment on pain anxiety among patients
who underwent orthopedic surgery were evaluated. Significant
differences were found between the two groups regarding the use of
music therapy to reduce pain; however, no statistically significant
differences were found in the use of opioids and physiological
variables between the two groups. The authors maintained that the
timing, duration, and type of music intervention can be modified in
relation to specific clinical settings and medical teams (19). A summary of the non-pharmacological
techniques used for pain management in children is presented in
Table II.
 | Table IINon-pharmacological therapy. |
Table II
Non-pharmacological therapy.
| Type of method | Age |
|---|
| Physical
methods | |
|
Comforting
touch (cuddles, stroking, holding) | All ages |
|
Comfort
positioning | All ages |
|
Cutaneous
stimulation | >1 months |
|
Pressure/massage | All ages |
|
Hot/cold
treatments | All ages |
|
Pacifier and
sucrose solution | <1 years |
|
Cognitive-comportamental methods | |
|
Information/communication | >6 years |
|
Psychological
preparations | >6 years |
|
Direct
involvement in pain management/assessment | >6 years |
|
Distraction
tools (music, videos, apps, toys with light/sounds) | All ages |
|
Desensitization | >2 years |
|
View/imagery
(story-telling, guided imagery, favor activity) | >6 years |
|
Relaxation
(deep breathing, music, muscles relaxing) | All ages |
|
Breathing
out/controlled breathing | Teenagers |
Criticism has been expressed as regards the use of
non-pharmacological treatments in the context of acute pediatric
pain where pharmacological, physical (splint, ice) and
psychological (distraction, breathing) treatments may be more
effective. In addition, the literature provides evidence of the
difficulties faced by nurses in applying non-pharmacological
treatments due to inadequate cooperation from physicians, the heavy
workloads of nurses and multiple responsibilities, the low ratio of
nurses per patient, and the unfavorable attitudes of nurses to
non-pharmacological pain management (20).
Pharmacological strategies
Pharmacological therapies are the most commonly used
types of treatments for any type of pain. The drugs commonly
utilized, as well as the routes of administration, doses and
indications on their use are summarized in Table III.
 | Table IIIPharmacological therapies for acute
pain. |
Table III
Pharmacological therapies for acute
pain.
| Drug | Route of
administration | Single dose | Maximum dose | Indications |
|---|
| Non-opioids | | | | |
|
Paracetamol | Per os | 10-15 mg/kg, every
4-6 h | 60-75 mg/kg/die (4
g/die) | From birth |
| | Rectal | 15-20 mg/kg, every
4-6 h | 60-90
mg/kg/die | |
| | i.v. | Per os | 90
g/kg/die | |
|
NSAIDs | | | | |
|
Ibuprofen | Per os | 5-10 mg/kg, every
6-8 h | 20-30
mg/kg/die | >3 months |
|
Ketoprofen | Per os | 1-3 mg/kg, every
8-12 h | 4-9 mg/kg/die | >6 years |
|
Ketorolac | Per os | 0.5 mg/kg, every
6-8 h | 3 g/kg/die | >16 years |
|
Naproxen
sodium | Per os | 1 mg/kg, every 8
h | 3 g/kg/die | >14 years |
|
Acetylsalicylic
acid | i.v. | 5-10 mg/kg, every
8-12 h | 20 g/kg/die | Not indicated in
pediatric age. If necessary >2 years |
| Opioids | Per os
(i.v.) | 10 mg/kg, every 6-8
h | 80 g/kg/die | >16 years |
|
Weak | | | | |
|
Codeine | Per os or
rectal | 0.5-1 mg/kg, every
6-8 h | 240 mg/die | >12 years |
|
Tramadol
hydrochloride | Per os | 1-2 mg/kg, every
6-8 h | 400 mg/die | >1 year |
|
Strong | | | | |
|
Fast-release
morphine sulfate | i.v. | 0.15-0.3 mg/kg,
every 4 h | | >1 year |
|
Morphine
hydrochloride | i.v. | Bolus 0.05-0.1
mg/kg, every 2-4 h | 5 mg/dose | From birth |
| | | CI 0.02-0.03
mg/kg/h | | |
|
Fentanyl | Intra nasal
injections | 1-2 µg/kg/dose
(repeatable after 30-60 min) | 100 µg | |
| | i.v. | Bolus 0.001-0.002
mg/kg; CI 0.001 mg/kg/h | | >2 years |
Non-opioid medications. The non-opioid pain
medications most commonly used are NSAIDs, which act via their
inhibitory actions on cyclooxygenase (COX)-2 enzymes. COX-2 enzymes
facilitate the production of pro-inflammatory prostaglandins; thus,
prostaglandin production is inhibited to obtain an analgesic
effect. Among the most commonly used NSAIDs is ibuprofen. Other
COX-2 inhibitors, such as indomethacin, meloxicam and Celebrex, are
more frequently used to treat inflammatory and rheumatological
disorders than acute pain (20,21A previous randomized controlled
trial of acetaminophen, ibuprofen and codeine treatment for acute
pain in children with musculoskeletal trauma conducted by Clark
et al (21) involved 336
pediatric patients with 100 children in each treatment group.
According to the authors of that study, ibuprofen provided the
optimal analgesic effect of the three medications studied. In
another study, a group of children presenting with uncomplicated
extremity fractures was treated in a randomized trial with the oral
administration of either morphine or ibuprofen (22). In that trial, 66 children were in
the morphine group and 68 in the ibuprofen group. No significant
differences in analgesic efficacy were reported between the groups,
although morphine was associated with a significantly greater
number of adverse effects. The authors of that study maintained
that ibuprofen remains safe and effective for outpatient pain
management in children with uncomplicated fractures (22). In another randomized clinical trial
performed by Chang et al (23), of 411 patients with acute extremity
pain (mean score, 8.7 on an 11-point numerical rating scale) in an
emergency department, no significant differences in pain reduction
at 2 h were found. The main pain scores decreased by 4.3 with
ibuprofen and acetaminophen, 4.4 with oxycodone and acetaminophen,
3.5 with hydrocodone and acetaminophen, and 3.9 with codeine and
acetaminophen. According to the authors of that study, the
analgesic effects of NSAIDs were equally efficacious as opioids
when treating musculoskeletal pain in adult patients (23).
As is well known, the use of ibuprofen is not
recommended for patients with hemorrhagic pathologies, significant
dehydration, gastrointestinal disorders and impaired renal
function. Jelinek (24)
demonstrated that the intravenous administration of ketorolac
exhibited an equivalent efficacy in reducing moderate to severe
pain as intravenous morphine, although with fewer side-effects.
Marzuillo et al (25)
reviewed the pharmacokinetics of ketorolac and confirmed its
efficacy without severe side-effects, if used for a short period of
time. Recently, a pilot single central randomized controlled trial
demonstrated that ketorolac had comparable results to morphine when
used in children aged 6-17 years with suspected appendicitis
(26). The use of ketorolac
sublingually as a valid alternative in the absence of intravenous
access was also suggested (26).
Neri et al (27)
demonstrated that sublingual ketorolac and tramadol were equally
effective. In cases of suspected bone fractures, studies have shown
that sublingual ketorolac and tramadol are effective analgesics for
pain management in children aged 4-17 years (25,26).
Paracetamol has been cited in numerous studies as
the first-line analgesic agent in emergency departments. Its
efficacy is valuable at the correct dose (15 mg/kg) in the
treatment of mild to moderate pain. It is characterized by its
rapid action and the possibility of different routes of
administration (28). A previous
meta-analysis revealed that the safety and tolerability profiles of
paracetamol and ibuprofen were similar in terms of their efficacy
for both pain and fever, and they were rarely associated with
severe side-effects (28). In
instances of mild or moderate pain, it is preferable to administer
paracetamol per os to achieve fairly rapid action and
excellent tolerance in the majority of children. By contrast, the
rectal route is burdened by slow absorption and unpredictable
efficacy both with respect to action time and analgesic capacity
(29). In a multicenter emergency
department study in 2018, Benini et al (7) found that both paracetamol and
ibuprofen were inappropriately used in 83 and 63% of pediatric
cases, respectively.
Ketamine, a drug that blocks the effects of
glutamate, has been shown to be an effective analgesic in children
when administered at sub-dissociative doses (30). Back pain, headache, extremity or
musculoskeletal pain, acute abdominal pain and renal colic are
controlled by the intravenous administration of ketamine when used
appropriately (31,32). In recent years, two systematic
reviews and meta-analyses demonstrated that ketamine was
non-inferior to opioid medications for acute pain management, as it
had a similar analgesic effect and safety profile (33,34).
Opioid medications. Opioid infusion is
usually indicated for patients with chronic pain. OF note, a bolus
of an intravenous opioid is advised for patients with sudden-onset
severe pain or reserved for breakthrough pain for patients who are
already receiving opioid infusions. Researchers have recommended
that the starting opioid in opioid-naïve patients should be
morphine or hydromorphone (30).
Typically, immediate-release oral opioids are ordered for pain at
intervals of 3-4 h to minimize breakthrough pain and opioid
side-effects (30). Additional
smaller doses can be administered every 2 h for breakthrough doses.
In general, oral use is preferred over intravenous administration,
except in cases of poor absorption or an inability to administer
drugs enterally (i.e., colitis, mucositis, vomiting). The
sublingual route of administration is safe and efficacious both for
ketorolac and opioids (34,35).
In the trauma setting, intranasal sufentanil or diamorphine
administration have both been reported as highly efficacious in the
treatment of severe pain (36,37).
6. Conclusion
The role of the pediatricians in the treatment of
acute pain is extremely complex due to the poor collaboration of
and difficulties encountered by the children and their parents to
correctly indicate the duration, intensity and localization of the
pain. The task of pediatricians consists of carefully evaluating
the underlying cause for acute pain in children to consequently
administer appropriate treatment. The list of methodologies used to
reveal the scales of acute pain and the type of treatment to be
used for specific causes of acute pain is wide. Thus, treatment
needs to be carried out according to the duration, localization and
severity of the pain, reflecting the experience of the single
pediatric specialist.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
PP, RF, LM, MCF and ADN conceived and designed the
study. GT and ADS performed the literature search. CM, LS and MCF
analyzed the data obtained from the literature. PP, AP and RF wrote
the manuscript. All authors (ADN, LS, MCF, GT, CM, ADS, SS, AP, MC,
RF, LM and PP) were involved in the preparation of the final draft
and in the revision of the manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Raja SN, Carr DB, Cohen M, Finnerup NB,
Flor H, Gibson S, Keefe FJ, Mogil JS, Ringkamp M, Sluka KA, et al:
The revised international association for the study of pain
definition of pain: Concepts, challenges, and compromises. Pain.
161:1976–1982. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Coda BA and Bonica JJ: General
considerations of acute pain. In: Loeser JD, Butler SH, Chapman CR
and Turk DC (eds) Bonica's management of pain, 3rd edition.
Philadelphia: Lippincott Williams & Wilkins, pp222-240,
2001.
|
|
3
|
Olson KA: Pain in children. Children can
experience a wide variety of painful conditions-from migraine
headaches to growing pains. Pract Pain Manag. 15:1–18. 2015.
|
|
4
|
American Academy of Pediatrics. Committee
on Psychosocial Aspects of Child and Family Health; Task Force on
Pain in Infants, Children, and Adolescents. The assessment and
management of acute pain in infants, children, and adolescents.
Pediatrics. 108:793–497. 2001.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mathews L: Pain in children: Neglected,
unaddressed and mismanaged. Indian J Palliat Care. 17
(Suppl):S70–S73. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ferrante P, Cuttini M, Zangardi T,
Tomasello C, Messi G, Pirozzi N, Losacco V, Piga S and Benini F:
PIPER Study Group. Pain management policies and practices in
pediatric emergency care: A nationwide survey of Italian hospitals.
BMC Pediatr. 13(139)2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Benini F, Castagno E, Barbi E, Congedi S,
Urbino A, Biban P, Calistri L and Mancusi RL: Multicentre emergency
department study found that paracetamol and ibuprofen were
inappropriately used in 83 and 63% of paediatric cases. Acta
Paediatr. 107:1766–1774. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gai N, Naser B, Hanley J, Peliowski A,
Hayes J and Aoyama K: A practical guide to acute pain management in
children. J Anesth. 34:421–433. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wente SJK: Nonpharmacologic pediatric pain
management in emergency departments: A systematic review of the
literature. J Emerg Nurs. 39:140–150. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Marseglia GL, Alessio M, Da Dalt L,
Giuliano M, Ravelli A and Marchisio P: Acute pain management in
children: A survey of Italian pediatricians. Ital J Pediatr.
45(156)2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ventafridda V, Saita L, Ripamonti C and De
Conno F: WHO guidelines for the use of analgesics in cancer pain.
Int J Tissue React. 7:93–96. 1985.PubMed/NCBI
|
|
12
|
Birnie KA, Hundert AS, Lalloo C, Nguyen C
and Stinson JN: Recommendations for selection of self-report pain
intensity measures in children and adolescents: A systematic review
and quality assessment of measurement properties. Pain. 160:5–18.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Stinson JN, Kavanagh T, Yamada J, Gill N
and Stevens B: Systematic review of the psychometric properties,
interpretability and feasibility of self-report pain intensity
measures for use in clinical trials in children and adolescents.
Pain. 125:143–157. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bulloch B, Garcia-Filion P, Notricia D,
Bryson M and McConahay T: Reliability of the color analog scale:
Repeatability of scores in traumatic and nontraumatic injuries.
Acad Emerg Med. 16:465–469. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Uman LS, Chambers CT, McGrath PJ and
Kisely SR: Psychological interventions for needle-related
procedural pain and distress in children and adolescents. Cochrane
Database Syst Rev: CD005179, 2006.
|
|
16
|
Accardi MC and Milling LS: The
effectiveness of hypnosis for reducing procedure-related pain in
children and adolescents: A comprehensive methodological review. J
Behav Med. 32:328–339. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
LeMay S, Johnston C, Choinière M, Fortin
C, Hubert I, Fréchette G, Kudirka D and Murray L: Pain management
interventions with parents in the emergency department: A
randomized trial. J Adv Nurs. 66:2442–2449. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hartling L, Newton AS, Liang Y, Jou H,
Hewson K, Klassen TP and Curtis S: Music to reduce pain and
distress in the pediatric emergency department: A randomized
clinical trial. JAMA Pediatr. 167:826–835. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Patiyal N, Kalyani V, Mishra R, Kataria N,
Sharma S, Parashar A and Kumari P: Effect of music therapy on pain,
anxiety, and use of opioids among patients underwent orthopedic
surgery: A systematic review and meta-analysis. Cureus.
13(e18377)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zeleke S, Kassaw A and Eshetie Y:
Non-pharmacological pain management practice and barriers among
nurses working in debre tabor comprehensive specialized hospital,
ethiopia. PLoS One. 16(e0253086)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Clark E, Plint AC, Correll R, Gaboury I
and Passi B: A randomized, controlled trial of acetaminophen,
ibuprofen, and codeine for acute pain relief in children with
musculoskeletal trauma. Pediatrics. 119:460–467. 2007.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Poonai N, Bhullar G, Lin K, Papini A,
Mainprize D, Howard J, Teefy J, Bale M, Langford C, Lim R, et al:
Oral administration of morphine versus ibuprofen to manage
postfracture pain in children: A randomized trial. CMAJ.
186:1358–1363. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chang AK, Bijur PE, Esses D, Barnaby DP
and Baer J: Effect of a single dose of oral opioid and nonopioid
analgesics on acute extremity pain in the emergency department: A
randomized clinical trial. JAMA. 318:1661–1667. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Jelinek GA: Ketorolac versus morphine for
severe pain. Ketorolac is more effective, cheaper, and has fewer
side effects. BMJ. 321:1236–1237. 2000.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Marzuillo P, Calligaris L, Amoroso S and
Barbi E: Narrative review shows that the short-term use of
ketorolac is safe and effective in the management of
moderate-to-severe pain in children. Acta Paediatr. 107:560–567.
2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Eltorki M, Busse JW, Freedman SB, Thompson
G, Beattie K, Serbanescu C, Carciumaru R, Thabane L and Ali S:
Intravenous ketorolac versus morphine in children presenting with
suspected appendicitis: A pilot single-centre non-inferiority
randomised controlled trial. BMJ Open. 12(e056499)2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Neri E, Maestro A, Minen F, Montico M,
Ronfani L, Zanon D, Favret A, Messi G and Barbi E: Sublingual
ketorolac versus sublingual tramadol for moderate to severe
post-traumatic bone pain in children: A double-blind, randomised,
controlled trial. Arch Dis Child. 98:721–724. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kanabar DJ: A clinical and safety review
of paracetamol and ibuprofen in children. Inflammopharmacology.
25:1–9. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Mak WY, Yuen V, Irwin M and Hui T:
Pharmacotherapy for acute pain in children: Current practice and
recent advances. Expert Opin Pharmacother. 12:865–881.
2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chumpitazi CE, Chang C, Atanelov Z,
Dietrich AM, Lam SHF, Rose E, Ruttan T, Shahid S, Stoner MJ, Sulton
C, et al: Managing acute pain in children presenting to the
emergency department without opioids. J Am Coll Emerg Physicians
Open. 3(e12664)2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Schwenk ES, Viscusi ER, Buvanendran A,
Hurley RW, Wasan AD, Narouze S, Bhatia A, Davis FN, Hooten WM and
Cohen SP: Consensus guidelines on the use of intravenous ketamine
infusions for acute pain management from the American society of
regional anesthesia and pain medicine, the American academy of pain
medicine, and the American society of anesthesiologists. Reg Anesth
Pain Med. 43:456–466. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Majidinejad S, Esmailian M and Emadi M:
Comparison of intravenous ketamine with morphine in pain relief of
long bones fractures: A double blind randomized clinical trial.
Emerg (Tehran). 2:77–80. 2014.PubMed/NCBI
|
|
33
|
Karlow N, Schlaepfer CH, Stoll CRT,
Doering M, Carpenter CR, Colditz GA, Motov S, Miller J and Schwarz
ES: A systematic review and meta-analysis of ketamine as an
alternative to opioids for acute pain in the emergency department.
Acad Emerg Med. 25:1086–1097. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Balzer N, McLeod SL, Walsh C and Grewal K:
Low-dose ketamine for acute pain control in the emergency
department: A systematic review and meta-analysis. Acad Emerg Med.
28:444–454. 2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Díaz-Chávez EP, Medina-Chávez JL,
Avalos-González J, Hernández-Moreno JJ, Cabrera-Mendoza AU and
Trujillo-Hernández B: Comparison of sublingual ketorolac vs IV
metamizole in the management of pain after same-day surgery. Cir
Cir. 77:45–49. 2009.PubMed/NCBI(In Spanish).
|
|
36
|
Minkowitz HS, Singla NK, Evashenk MA,
Hwang SS, Chiang YK, Hamel LG and Palmer PP: Pharmacokinetics of
sublingual sufentanil tablets and efficacy and safety in the
management of postoperative pain. Reg Anesth Pain Med. 38:131–139.
2013.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Borland M, Jacobs I, King B and O'Brien D:
A randomized controlled trial comparing intranasal fentanyl to
intravenous morphine for managing acute pain in children in the
emergency department. Ann Emerg Med. 49:335–340. 2007.PubMed/NCBI View Article : Google Scholar
|