Introduction
Ovarian cancer represents the third most prevalent
gynecological malignancy affecting the female population, following
cervical and endometrial cancers (1). GLOBOCAN 2020 reported 313,959 new
cases worldwide, with 207,252 associated deaths. In Vietnam,
ovarian cancer ranks as the 11th most common type of cancer among
females, with ~1,200 cases diagnosed annually (2) and a relatively poor 5-year survival
rate <45% (3). While
established risk factors include BRCA1 and BRCA2 gene mutations
(4), histopathological
characteristics (5) and menopausal
hormone therapy (6), dietary
factors emerge as a modifiable component with a potential
significant influence on mortality rates and survival outcomes
(7,8). The study by Playdon et al
(9) demonstrated that an increased
intake of dietary fiber was associated with an improved survival
rate [hazard ratio (HR), 0.69; 95% confidence interval (CI),
0.53-0.90; P=0.002], while an elevated glycemic index was
associated with poorer outcomes (HR, 1.28; 95% CI, 1.01-1.65;
P=0.03).
The 2020 National Comprehensive Cancer Network
(NCCN) Clinical Practice Guidelines establish surgical tumor
resection combined with adjuvant chemotherapy as the standard
treatment protocol for ovarian cancer (10). Although chemotherapy has proven to
be effective in prolonging survival and enhancing clinical outcomes
(11,12), it can simultaneously damage healthy
cells, leading to adverse effects. These complications typically
manifest as symptom clusters, including fatigue, nausea, vomiting
and the numbness or tingling in the hands and feet, markedly
affecting the quality of life of patients and promoting
chemotherapeutic tolerance (13,14).
Ferreira et al (15)
examined 20 patients with breast cancer undergoing chemotherapy and
reported a mean daily energy intake of 1191.7±458.3 kcal, with an
average protein and lipid consumption of 48.5±21.9 and 38.5±19.1
g/day, respectively. The macronutrient distribution comprised 16.3%
protein, 29.1% lipids and 57.7% carbohydrates, with the majority of
patients exhibiting deficiencies in vitamins A, B1, B3 and B6, as
well as in minerals, including calcium, iron, magnesium and fiber
(15). Similarly, the study by
Matcek (16) on women >70 years
of age with stage III and IV ovarian cancer documented a mean
energy intake of 1189±508 kcal/day, with <50% of patients
meeting recommended intake levels for vitamins C, B1, B9 and B6.
The analysis of five consecutive NHANES surveys (2007-2016) by Zhu
et al (17), revealed that
patients with ovarian cancer averaged 56.7 g/day of protein intake,
with a mean lipid and carbohydrate consumption of 55.7 and 77.2
g/day, respectively.
Current global research has largely focused on food
frequency across different food groups without detailed
quantification of actual consumption patterns, thereby limiting the
accuracy of dietary intake assessments. The 24-h recall method
provides distinct advantages, including the identification of food
combinations affecting micronutrient absorption, insights into food
preparation methods, and the documentation of commonly consumed
processed food brands. However, studies specifically examining
dietary patterns among patients with ovarian cancer remain limited.
Therefore, the present study aimed to evaluate the dietary intake
of patients with ovarian cancer undergoing chemotherapy using a
24-h dietary recall methodology.
Materials and methods
Study design and setting
The present cross-sectional study was conducted
between July, 2023 and February, 2024 at the Departments of
Internal Medicine 5 and 6 of Vietnam National Cancer Hospital
(Hanoi, Vietnam). The present study was approved by the Hanoi
Medical University (Hanoi, Vietnam) under Decision no.
2031/QD-DHYHN dated May 27, 2024, concerning the establishment of
the Bachelor of Nutrition Thesis Evaluation Committee for the
2020-2024 cohort. All participants provided written informed
consent after receiving detailed information about the study's
objectives, procedures and potential implications.
Study population
The present study enrolled 125 patients with ovarian
cancer aged ≥18 years who were undergoing chemotherapy. Eligible
participants included newly admitted patients, interdepartmental
transfers and those returning for scheduled treatment follow-ups.
The exclusion criteria comprised patients unable to provide
information (due to dementia or psychiatric disorders), and those
with edema, physical deformities, spinal curvature, or
pregnancy.
Study procedures
Participants were recruited through convenience
sampling. Following medical record verification and eligibility
confirmation, patients were invited to participate. Data collection
encompassed general information and dietary intake assessment
through 24-h dietary recall interviews. Dietary intake was
estimated using a standardized questionnaire and the National
Institute of Nutrition's photo book (https://drive.google.com/drive/folders/1tKkm4H9O8fLWRrO1rdc0m_Yp2poN_n93?usp=sharing).
To ensure the representation of typical dietary patterns, data
collection was not conducted during special occasions such as
festivals or feasts.
24-h dietary recall protocol
Dietary recall was conducted following a structured
five-step protocol as follows: i) Initial listing of all foods and
beverages consumed within the previous 24 h; ii) systematic probing
for potentially forgotten items; iii) documentation of consumption
time and location for each item; iv) detailed recording of portion
sizes and quantities, including condiments; and v) sfinal
verification of additional food or beverage consumption.
Data collection and assessment
methods
Patient data were collected in-hospital using
standardized questionnaires. Nutritional status assessment
incorporated three validated tools aa follows: i) Patient-generated
subjective global assessment (PG-SGA), categorizing patients as
well-nourished (PG-SGA A), mildly to moderately malnourished
(PG-SGA B), or severely malnourished (PG-SGA C) (18); ii) body mass index (BMI),
classified according to the WHO criteria: Overweight/obese, ≥25;
normal weight, 18.5-24.9; and chronic energy deficiency,
≤18.5(19); iii) mid-upper arm
circumference (MUAC), with malnutrition defined as <23 cm for
adult females as per the National Institute of Nutrition guidelines
(20).
Dietary requirements were established based on the
ESPEN 2021 guidelines for cancer patients, specifying 25-30
kcal/kg/day for energy and 1-1.5 g/kg/day for protein (21). This present study applied standards
of 30 kcal/kg/day for energy and 1.2 g/kg/day for protein, with
animal protein constituting 30-35% of total protein intake
(22). Recommended macronutrient
distribution comprised 20-25% of total energy from lipids (>60%
from plant sources) and 55-65% from carbohydrates (22). Weight calculations were adjusted
according to the nutritional status as follows: i) Patients with a
normal BMI: Current weight used; ii) malnourished patients: Ideal
weight calculated as [ideal BMI (22 kg/m2) x
height2] (23); iii)
overweight/obese patients: Adjusted weight=(current weight-ideal
weight) x0.33 + ideal weight (21).
Statistical analysis
Data processing was performed using EpiData 3.1
software for entry and cleaning. Statistical analyses were
conducted using Jamovi 2.3.18 software. Dietary recall data were
converted to gram equivalents and analyzed using Eiyokun software
for macro- and micronutrient calculations. Data were analyzed using
the Kruskal-Wallis test followed by the
Dwass-Steel-Crichtlow-Fligner test. A P-value <0.05 was
considered to indicate a statistically significant difference.
Results
Of the 125 enrolled patients with ovarian cancer,
56.8% were aged 40-59 years, and 75.2% presented with
advanced-stage disease (stages III and IV). Nutritional risk
assessment using the PG-SGA tool identified malnutrition in 52.0%
of the patients, with 40.0% of the patients were classified as
being mild to moderately malnourished (PG-SGA B) and 12.0% as
severely malnourished (PG-SGA C). BMI classification indicated
malnutrition in 12.0% of the patients and overweight/obesity in
6.4% of the patients. MUAC measurements revealed malnutrition in
20.8% of the study population (Table
I).
 | Table IGeneral characteristics of the study
participants. |
Table I
General characteristics of the study
participants.
| Characteristic | Frequency | Percentage |
|---|
| Age | | |
|
18-39
years | 16 | 12.8 |
|
40-59
years | 71 | 56.8 |
|
≥60
years | 38 | 30.4 |
| Disease stage | | |
|
Stage I | 14 | 11.2 |
|
Stage
II | 17 | 13.6 |
|
Stage
III | 80 | 64.0 |
|
Stage
IV | 14 | 11.2 |
| PG-SGA | | |
|
PG-SGA
A | 60 | 48.0 |
|
PG-SGA
B | 50 | 40.0 |
|
PG-SGA
C | 15 | 12.0 |
| BMI | | |
|
Malnourished
(<18.5) | 15 | 12.0 |
|
Normal
(≥18.5 and ≤24.9) | 102 | 81.6 |
|
Overweight/obese
(≥25) | 8 | 6.4 |
| MUAC | | |
|
Malnourished
(<23 cm) | 26 | 20.8 |
|
Normal | 99 | 79.2 |
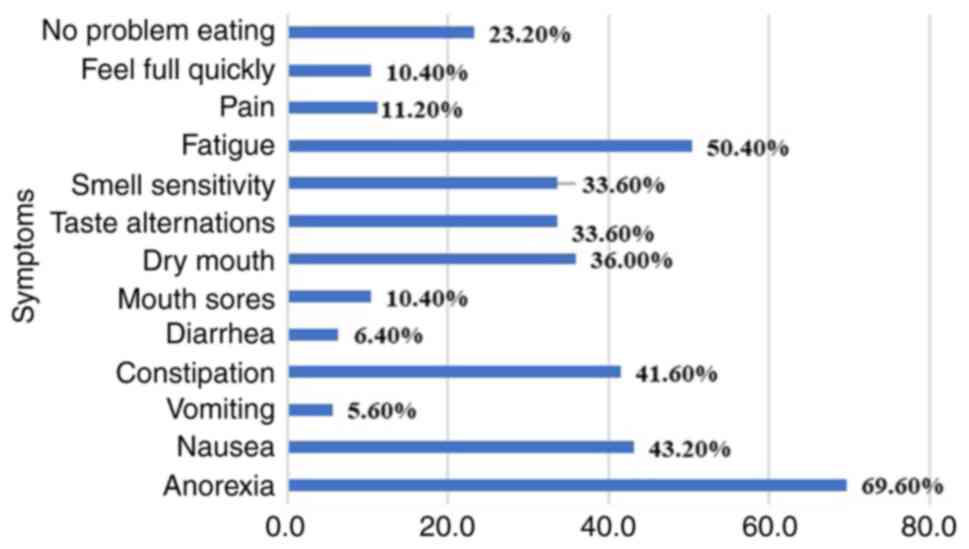
As regards symptoms affecting dietary intake,
appetite loss was predominant (69.6%), followed by fatigue (50.4%),
nausea (43.2%), constipation (41.6%), dry mouth (36.0%), taste
alterations (33.6%) and smell sensitivity (33.6%). Notably, 23.2%
of the participants reported no dietary intake difficulties during
the 2-week observation period (Fig.
1).
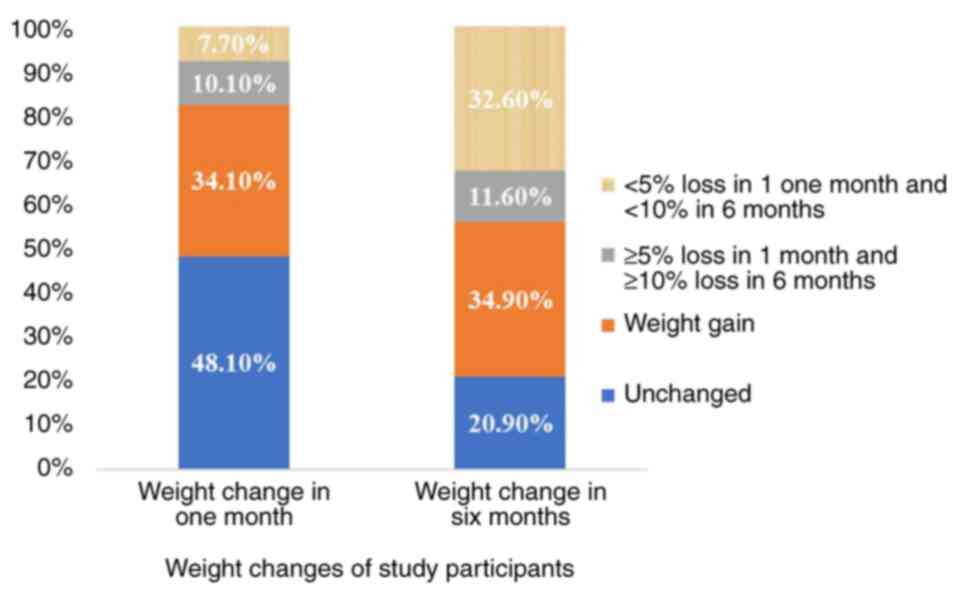
Weight change analysis revealed that 44.2% of the
participants experienced weight loss over a period of 6 months,
with 11.6% losing >10% of their body weight. During the most
recent month, 17.8% reported weight loss (10.1% experiencing >5%
reduction), while 34.1% demonstrated weight gain (Fig. 2).
Dietary assessment revealed a mean daily energy
intake of 1,433.3±488.5 kcal, with only 38.4% of the participants
meeting the recommended requirements. The mean protein consumption
was 65.6±35.0 g/day, with 44.8% achieving recommended levels.
Notably, no participants met the recommended animal-to-total
protein ratio. The mean lipid intake was 37.7±21.5 g/day, with
20.0% meeting recommendations, while only 7.0% achieved the target
plant-to-total liquid ratio. Daily carbohydrate and dietary fiber
intake averaged at 208.5±77.7 g and 9.1±7.8 g, respectively, with a
compliance rate of 28.8 and 8.0%. The macronutrient distribution
exhibited a ratio of 17.9:23.0:59.1 for protein:lipid:carbohydrate
percentages of the total energy intake (Table II).
 | Table IINutritional values from the 24-h
dietary intake of the study participants. |
Table II
Nutritional values from the 24-h
dietary intake of the study participants.
| Nutrient | Mean ± SD | Meets the recommended
intake, n (%) |
|---|
| Energy
(kcal/day) | 1433.3±488.5 | 48 (38.4) |
| Protein | | |
|
Total
protein (g/day) | 65.6±35.0 | 56 (44.8) |
|
Animal-to-total
protein ratio (%) | 58.9±9.8 | 0 (0) |
| Lipids | | |
|
Total lipids
(g/day) | 37.7±21.5 | 25 (20.0) |
|
Plant-to-total
lipid ratio | 42.9±12.9 | 9 (7.0) |
| Carbohydrates
(g/day) | 208.5±77.7 | 36 (28.8) |
| Dietary fiber
(g/day) | 9.1±7.8 | 10 (8.0) |
|
Protein:lipid:carbohydrate (%) | (17.9±5.8:
23.0±8.9: 59.1±12.1) | |
As regards vitamins, the proportion of patients
meeting the recommended intake was lowest for vitamins A and B2, at
29.6 and 28.0%, respectively. Calcium, iron and magnesium had the
lowest rates of meeting the recommended intake (Table III).
 | Table IIIMicronutrient levels in the 24-h
dietary intake of the study participants. |
Table III
Micronutrient levels in the 24-h
dietary intake of the study participants.
| Value | Vitamin A (µg) | Vitamin B1
(mg) | Vitamin B2
(mg) | Vitamin PP
(mg) | Vitamin C (mg) | Iron (mg) | Calcium (mg) | Calcium/ phosphorus
ratio | Magnesium (mg) | Copper (µg) | Zinc (mg) |
|---|
| Mean ± SD | 539.4±662.6 | 2.2±11.3 | 1.8±9.8 | 14.9±12.8 | 166.5±146.1 | 13.9±13.9 | 819.5±992.9 | 0.9±0.8 | 208.4±188.7 | 1,134.2±930.5 | 11.2±38.8 |
| Recommended
intake | 650-700 | 1.1 | 1.2 | 14 | 100 |
17.4-26.1a; 6.7-10b; 6.3-9.4c | 800-1,000 | 0.8-1.5 | 260-300 | 900 | 4.8-16d; 4.2-14e |
| Meeting
recommendations, n (%) | 37 (29.6) | 66 (52.8) | 35 (28.0) | 58 (46.4) | 79 (63.2) | 23 (18.4) | 34 (27.2) | 33 (26.4) | 30 (24.0) | 66 (52.8) | 40 (32.0) |
Age-stratified analysis revealed declining
macronutrient intake with an advancing age. Protein consumption
exhibited the most significant variation, with the youngest age
group (18-39 years) consuming higher amounts (91.6±31.5 g/day)
compared with the middle-aged (64.1±38.7 g/day) and elderly
(59.7±23.6 g/day) participants (P<0.009). While disease
progression demonstrated a trend toward a decreased nutrient intake
across all macronutrients, these differences did not achieve
statistical significance (P>0.05) across disease stages
(Table IV).
 | Table IV24-h dietary values by age group and
disease stage. |
Table IV
24-h dietary values by age group and
disease stage.
| | Nutrient |
|---|
| Age group | Energy | Protein | Lipid | Glucide |
|---|
|
18-39
years | 1740.5±551.4 | 91.6±31.5 | 54.0±26.7 | 222.6±107.1 |
|
40-59
years | 1390.4±493.7 | 64.1±38.7 | 35.4±20.6 | 210.2±77.0 |
|
≥60
years | 1366.5±479.0 | 59.7±23.6 | 36.6±19.3 | 200.4±70.2 |
|
P-valuea | 0.109 | 0.009 | 0.076 | 0.699 |
| Post-hoc
testb | 18-39 group vs. the
40-59 group (P=0.258); 18-39 group vs. ≥60 group (P=0.161); 40-59
group vs. the ≥60 group (P=0.869) | 18-39 group vs. the
40-59 group (P=0.006); 18-39 group vs. ≥60 group
(P=0.006); 40-59 group vs. the ≥60 group (P=0.976) | 18-39 group vs. the
40-59 group (P=0.079); 18-39 group vs. ≥60 group (P=0.097); 40-59
group vs. ≥60 group (P=0.822) | 18-39 group vs. the
40-59 group (P=0.969); 18-39 group vs. ≥60 group (P=0.857); 40-59
group vs. ≥60 group (P=0.848) |
| Disease stage | | | | |
|
Stage I | 1675.1±630.0 | 74.4±38.9 | 48.2±28.0 | 236.6±87.2 |
|
Stage
II | 1420.0±523.7 | 69.3±34.6 | 33.2±19.3 | 212.2±100.3 |
|
Stage
III | 1397.4±461.9 | 64.1±36.5 | 36.1±20.0 | 204.5±72.6 |
|
Stage
IV | 1412.2±416.3 | 60.8±22.8 | 41.9±23.1 | 198.7±17.9 |
|
P-valuea | 0.508 | 0.676 | 0.334 | 0.605 |
| Post-hoc
testb | Stage I vs. stage
II (P=0.633); Stage I vs. stage III (P=0.492); Stage I vs. stage IV
(P=0.769); Stage II vs. stage III: NS; Stage II vs. stage IV
(P=0.999); Stage III vs. stage IV (P=0.965) | Stage I vs. stage
II (P=0.999); Stage I vs. stage III (P=0.803); Stage I vs. stage IV
(P=0.863); Stage II vs. stage III (P=0.927); Stage II vs. stage IV
(P=0.984); Stage III vs. stage IV: NS | Stage I vs. stage
II (P=0.320); Stage I vs. stage III (P=0.499); Stage I vs. stage IV
(P=0.946); Stage II vs. stage III (P=0.865); Stage II vs. stage IV
(P=0.798); Stage III vs. stage IV (P=0.772) | Stage I vs. stage
II (P=0.683); Stage I vs. stage III (P=0.706); Stage I vs. stage IV
(P=0.842); Stage II vs. stage III (P=0.993); Stage II vs. stage IV
(P=0.999); Stage III vs. stage IV (P=0.996) |
Discussion
The present study on 125 patients with ovarian
cancer revealed a 52% malnutrition risk based on PG-SGA assessment,
substantially higher than the 31% reported in the study by Lieu
et al (24) on 100
Vietnamese patients with gynecological cancer undergoing
chemotherapy at the National Hospital of Obstetrics and Gynecology.
The disparity likely reflects the heterogeneous nature of their
study population, which included various gynecological malignancies
rather than focusing specifically on ovarian cancer.
The findings of the present study demonstrate strong
concordance with international data, particularly with those in the
study by Terlikowska et al (25) on 136 patients with ovarian cancer,
which reported a 55.1% malnutrition risk using PG-SGA. This
alignment is further supported by the study by Chantragwe and
Achariyapota (26) on 97 patients
with gynecological cancers in Thailand, documenting a 53.5% overall
malnutrition rate, with patients with ovarian cancer exhibiting a
high vulnerability at 44.2%. The findings of the study by Laky
et al (27) reinforce this
pattern, demonstrating significantly a compromised nutritional
status among patients with ovarian cancer compared with other
gynecological malignancies.
Using BMI as an assessment criterion, the present
study identified malnutrition in 12% of the patients, consistent
with previous studies on Vietnamese patients by Linh et al
(28) (12% in 50 patients) and
Phuong et al (29) (15.5%
in 129 patients). BMI-based assessment revealed lower malnutrition
rates compared to the PG-SGA method, as BMI relies solely on
anthropometric measurements. Moreover, the comprehensive evaluation
of PG-SGA encompasses gastrointestinal symptoms and clinical
parameters, enabling the earlier detection of nutritional risk
before notable weight changes manifest.
Dietary analysis revealed a mean daily energy intake
of 1,433.3 kcal, with only 38.4% of the patients meeting
recommended requirements. This is lower than the 1,536.72 kcal/day
reported in the study by Thuy et al (30) on patients with gynecological
cancers. This difference may be attributed to the superior
nutritional status of their cohort, with 88% classified as PG-SGA
A, suggesting fewer dietary intake barriers. The findings of the
present study also fall below international benchmarks, as
evidenced in the Polish study by Surwillo and Wawrzyniak (31) on patients with various types of
cancers (lung, breast, bone and soft tissue), which reported a mean
intake of 1,608 kcal/day; notably however, only 10% achieved their
recommended energy requirements. These variations likely reflect
differences in recommended energy intake guidelines and baseline
BMI distributions, influencing ideal and adjusted body weight
calculations.
The present study demonstrated a mean daily protein
intake of 65.6 g, closely corresponding with the findings of the
study by Surwillo and Wawrzyniak (31) of 62.7 g per day. Despite a mean
animal protein consumption of 58.9 g/day, none of the participants
achieved the recommended animal-to-total protein ratio. This
deficiency may stem from the misconception of patients that protein
is exclusively derived from animal sources, leading to the
prioritization of animal proteins, while overlooking plant-based
protein sources, such as legumes. Although >50% of the patients
met the overall recommended protein intake, the imbalance between
animal and plant-based proteins could potentially precipitate
digestive complications, particularly constipation due to
inadequate fiber intake, as well as deficiencies in essential
vitamins, minerals, and antioxidants. The prolonged persistence of
this imbalance may elevate the risk of developing metabolic
disorders.
The mean daily lipid intake was 37.7 g, with only
20% of the patients achieving the recommended requirement, the
lowest compliance rate among macronutrients. This observation
aligns with the findings of previous studies on dietary patterns in
patients with cancer, which documented similarly low adherence to
lipid intake recommendations (24,32).
This pattern may reflect traditional Vietnamese dietary
preferences, which emphasize natural flavors rather than the butter
and cheese-rich preparations common in Western cuisine.
Furthermore, the ratio of plant-based to total lipids was
suboptimal, likely influenced by high animal protein consumption,
which naturally affects the proportion of animal-derived lipids in
the diet.
Carbohydrate consumption averaged at 208.5 g daily,
exceeding both the findings reported in the study by Surwillo and
Wawrzyniak (31) pf 203.1 g and
those reported by Byun and Kim (33) of 141.8 g. This elevated intake
reflects characteristic Vietnamese dietary patterns, where
carbohydrate-rich staples, rice, corn and sweet potatoes, serve as
primary energy sources. The observed macronutrient distribution
ratio (protein:lipid:carbohydrate) of 17.9:23.0:59.1 largely aligns
with the National Institute of Nutrition's guidelines for adults
(22), which recommend proportions
of 13-20% protein, 20-25% lipids and 55-65% carbohydrates.
Dietary fiber intake averaged at 9.1 g/day, markedly
below the recommended 20-22 g/day for Vietnamese adults (22). The majority of patients exhibited
deficiencies in certain vitamins, including vitamin C (85%),
vitamin B2 (72%) and vitamin A (70.4%). Mineral deficiencies were
similarly prevalent, with inadequate intake of iron (81.6%),
magnesium (76%) and calcium (72.8%). These nutritional gaps may
stem from disproportionate animal protein consumption, potentially
creating imbalances in essential nutrient intake. Research has
demonstrated that high fiber intake significantly reduces the risk
of developing ovarian cancer compared to a low fiber intake, with
consistent findings across American, European and Asian studies
(34,35). These results emphasize the
importance of dietary guidance focused on enhancing fiber and
micronutrient intake among these patients.
The principal strength of the present study lies in
its detailed assessment of dietary intake among patients with
ovarian cancer undergoing chemotherapy using the 24-h recall
method, contributing valuable data to an understudied field.
However, certain limitations merit attention. The study population
was confined to patients receiving chemotherapy, potentially
limiting generalizability. Additionally, while the 24-h dietary
recall method provides valuable insights, it may not fully capture
long-term dietary patterns, as nutritional status typically
reflects cumulative dietary habits. Future studies would benefit
from implementing 48-to 72-h dietary assessment to provide more
comprehensive evaluations of the nutritional status and eating
behaviors of patients.
In conclusion, the present study reveals that
patients with ovarian cancer undergoing chemotherapy face
substantial malnutrition risks, characterized by inadequate and
imbalanced intake of plant and animal-based foods, vitamins,
minerals and fiber.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
HTL, BVH and TPTD conceptualized and designed the
study. HTL, BVH and TPTD performed the statistical analysis. HTL
and BVH interpreted the data and drafted the original manuscript.
All authors contributed substantially to manuscript revision,
critically reviewed the content, and approved the final version.
HTL and BVH confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved by Hanoi Medical
University (Hanoi, Vietnam) under Decision No. 2031/QD-DHYHN dated
May 27, 2024, concerning the establishment of the Bachelor of
Nutrition Thesis Evaluation Committee for the 2020-2024 cohort. All
participants provided written informed consent after receiving
detailed information about the study's objectives, procedures, and
potential implications.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global Cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics 2012. CA
Cancer J Clin. 65:87–108. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Webb PM and Jordan SJ: Epidemiology of
epithelial ovarian cancer. Best Pract Res Clin Obstet Gynaecol.
41:3–14. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Petrillo M, Marchetti C, De Leo R, Musella
A, Capoluongo E, Paris I, Benedetti Panici P, Scambia G and Fagotti
A: BRCA mutational status, initial disease presentation, and
clinical outcome in high-grade serous advanced ovarian cancer: A
multicenter study. Am J Obstet Gynecol. 217:334.e1–334.e9.
2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gaitskell K, Hermon C, Barnes I, Pirie K,
Floud S, Green J, Beral V and Reeves GK: Million Women Study
Collaborators. Ovarian cancer survival by stage, histotype, and
pre-diagnostic lifestyle factors, in the prospective UK Million
Women Study. Cancer Epidemiol. 76(102074)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lacey JV Jr, Brinton LA, Leitzmann MF,
Mouw T, Hollenbeck A, Schatzkin A and Hartge P: Menopausal hormone
therapy and ovarian cancer risk in the National institutes of
Health-AARP diet and health study cohort. JNCI J Natl Cancer Inst.
98:1397–1405. 2006.PubMed/NCBI View Article : Google Scholar
|
|
7
|
El-Sherif A, El-Sherif S, Taylor AH and
Ayakannu T: Ovarian cancer: Lifestyle, diet and nutrition. Nutr
Cancer. 73:1092–1107. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Thomson CA, Crane TE, Wertheim BC,
Neuhouser ML, Li W, Snetselaar LG, Basen-Engquist KM, Zhou Y and
Irwin ML: Diet quality and survival after ovarian cancer: Results
from the Women's Health initiative. JNCI J Natl Cancer Inst.
106(dju 314)2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Playdon MC, Nagle CM, Ibiebele TI,
Ferrucci LM, Protani MM, Carter J, Hyde SE, Neesham D, Nicklin JL,
Mayne ST and Webb PM: Pre-diagnosis diet and survival after a
diagnosis of ovarian cancer. Br J Cancer. 116:1627–1637.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Armstrong DK, Alvarez RD, Bakkum-Gamez JN,
Barroilhet L, Behbakht K, Berchuck A, Chen LM, Cristea M, DeRosa M,
Eisenhauer EL, et al: Ovarian cancer, version 2.2020, NCCN clinical
practice guidelines in oncology. J Natl Compr Canc Netw.
19:191–226. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ahmed N, Greening D, Samardzija C,
Escalona RM, Chen M, Findlay JK and Kannourakis G: Unique proteome
signature of post-chemotherapy ovarian cancer ascites-derived tumor
cells. Sci Rep. 6(30061)2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Nasioudis D, Mastroyannis SA, Ko EM,
Haggerty AF, Cory L, Giuntoli RL II, Kim SH, Morgan MA and Latif
NA: Delay in adjuvant chemotherapy administration for patients with
FIGO stage I epithelial ovarian carcinoma is associated with worse
survival; an analysis of the National Cancer Database. Gynecol
Oncol. 166:263–268. 2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cancer Council NSW: Side effects of
chemotherapy. Cancer Council NSW, Woolloomooloo NSW. https://www.cancercouncil.com.au/cancer-information/cancer-treatment/chemotherapy/side-effects/.
|
|
14
|
Herzog TJ: Recurrent ovarian cancer: How
important is it to treat to disease progression? Clin Cancer Res.
10:7439–7449. 2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ferreira IB, Marinho E da C, Custódio ID,
Gontijo CA, Paiva CE, Crispim CA and Maia YC: Food intake and the
nutritional status of women undergoing chemotherapy. Ciênc Saúde
Coletiva. 21:2209–2218. 2016.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
16
|
Matcek SE: Assessment of dietary intake in
Newly-diagnosed elderly ovarian cancer patients prior to initiation
of chemotherapy. ProQuest 10838621, 2018. https://www.proquest.com/openview/c231304f7eaa295208ff7f4418b1511c/1?pq-origsite=gscholar&cbl=18750.
|
|
17
|
Zhu G, Li Z, Tang L, Shen M, Zhou Z, Wei
Y, Zhao Y, Bai S and Song L: Associations of dietary intakes with
gynecological cancers: Findings from a cross-sectional study.
Nutrients. 14(5026)2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Bauer J, Capra S and Ferguson M: Use of
the scored Patient-generated subjective global assessment (PG-SGA)
as a nutrition assessment tool in patients with cancer. Eur J Clin
Nutr. 56:779–785. 2002.PubMed/NCBI View Article : Google Scholar
|
|
19
|
World Health Organization (WHO). Body Mass
Index-BMI. WHO, Geneva. https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index.
|
|
20
|
ICMR-National Institute of Nutrition:
Assessment of nutritional status and growth mornitoring. Hyderabad,
India. https://viendinhduong.vn/vi/pho-bien-kien-thuc-chuyen-mon/danh-gia-tinh-trang-dinh-duong-va-theo-doi-tang-truong.html.
|
|
21
|
Muscaritoli M, Arends J, Bachmann P,
Baracos V, Barthelemy N, Bertz H, Bozzetti F, Hütterer E, Isenring
E, Kaasa S, et al: ESPEN practical guideline: Clinical nutrition in
cancer. Clin Nutr. 40:2898–2913. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
National Institute of Nutrition:
Recommended nutritional needs for Vietnamese people, 2016.
|
|
23
|
Ministry of Health Portal: Guidelines for
diagnostic and treatment of obesity. https://thuvienphapluat.vn/van-ban/The-thao-Y-te/Quyet-dinh-2892-QD-BYT-2022-tai-lieu-Huong-dan-chan-doan-va-dieu-tri-benh-beo-phi-533849.aspx.
|
|
24
|
Lieu NTT, Anh NTV, Huong LT and Khanh ĐN:
Nutritional status and actual diet of cancer patients receiving
chemotherapy at the National hospital of obstetrics and gynecology
in 2019-2020. Vietnam J Nutr Food. 16:36–46. 2020.
|
|
25
|
Terlikowska K, Dobrzycka B, Kinalski M and
Terlikowski S: Serum concentrations of carotenoids and Fat-soluble
vitamins in relation to nutritional status of patients with ovarian
cancer. Nutr Cancer. 73:1480–1488. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Chantragawe C and Achariyapota V:
Utilization of a scored patient-generated subjective global
assessment in detecting a malnourished status in gynecologic cancer
patients. Asian Pac J Cancer Prev. 17:4401–4404. 2016.PubMed/NCBI
|
|
27
|
Laky B, Janda M, Bauer J, Vavra C,
Cleghorn G and Obermair A: Malnutrition among gynaecological cancer
patients. Eur J Clin Nutr. 61:642–646. 2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Linh BNT, Dung TTN, Son PTHA, et al: Study
of clinical and paraclinical characteristics of 50 patients with
serous ovarian carcinoma. J Military Med. 352:45–49. 2021.
|
|
29
|
Phuong HT, Hoa NTT, Binh PV, Bach HV and
Huong LT: Nutritional status of ovarian cancer patients at K
hospital in 2018-2019. Vietnam Med J. 526:2023.
|
|
30
|
Thuy HT, Lan NTH and Tam NTT: Nutritional
status of gynecological cancer patients treated at Hanoi Obstetrics
and Gynecology Hospital in 2023. Vietnam J Nutr Food. 20:37–45.
2024.
|
|
31
|
Surwillo A and Wawrzyniak A: Nutritional
assessment of selected patients with cancer. Rocz Panstw Zakl Hig.
64:225–233. 2013.PubMed/NCBI
|
|
32
|
Hanh PTB, Huong LT, Linh NT, Chung VT and
Trang NT: Dietary status of gastrointestinal cancer patients
receiving chemotherapy at Hanoi Medical University Hospital.
Vietnam J Nutrition Food. 13:93–98. 2017.
|
|
33
|
Byun MS and Kim NH: Energy intake and
fatigue in patients receiving chemotherapy. J Korean Biol Nurs Sci.
14:258–267. 2012.
|
|
34
|
Huang X, Wang X, Shang J, Lin Y, Yang Y,
Song Y and Yu S: Association between dietary fiber intake and risk
of ovarian cancer: A meta-analysis of observational studies. J Int
Med Res. 46:3995–4005. 2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Xu H, Ding Y, Xin X, Wang W and Zhang D:
Dietary fiber intake is associated with a reduced risk of ovarian
cancer: A dose-response meta-analysis. Nutr Res. 7:1–11.
2018.PubMed/NCBI View Article : Google Scholar
|