Introduction
L-asparaginase (L-asp) is a well-known anticancer
agent used for lymphoid malignancies. Although it is one of the key
drugs in the treatment of acute lymphoblastic leukemia (ALL) in
children, it is also known to induce several acute complications,
including coagulopathy, hypersensitivity, hepatic dysfunction,
hypertriglyceridemia, hyperammonemia and pancreatitis. In patients
with clinical symptoms such as abdominal pain, nausea and emesis,
acute pancreatitis is suspected on the basis of elevated levels of
serum amylase and/or lipase, along with abnormal findings on
imaging studies. Early diagnosis and prompt treatment of acute
pancreatitis is imperative. However, it may not always be possible
using standard diagnostic procedures, such as serum amylase
measurement and abdominal ultrasonography/computed tomography
(US/CT).
This is a report of two pediatric cases of
asparaginase-associated pancreatitis (AAP) diagnosed in its early
stage on the basis of elevated serum elastase-1 levels in the
presence of normal amylase levels.
Case reports
Case 1
A 5-year-old boy with B-precursor ALL had received
multi-agent chemotherapy according to the L-0416 protocol of the
Tokyo Children's Cancer Study Group (TCCSG) and complete remission
was achieved following induction chemotherapy. The patient
underwent subsequent chemotherapies without severe complications.
Nine months after the onset of the disease, he received sequential
chemotherapy comprising dexamethasone (DEX; 6 mg/m2 × 14
days), vincristine (VCR, 1.5 mg/m2 weekly × 4 weeks),
adriamycin (ADR, 25 mg/m2 weekly × 4 weeks) and L-asp
(6,000 U/m2 weekly × 4 weeks). Three days after the
administration of the third dose of L-asp the patient suddenly
developed posterior reversible encephalopathy syndrome and had to
be treated with anticonvulsant, antihypertensive and sedative
agents. During this intensive treatment, pleural effusion and
ascites gradually developed and mechanical ventilation was
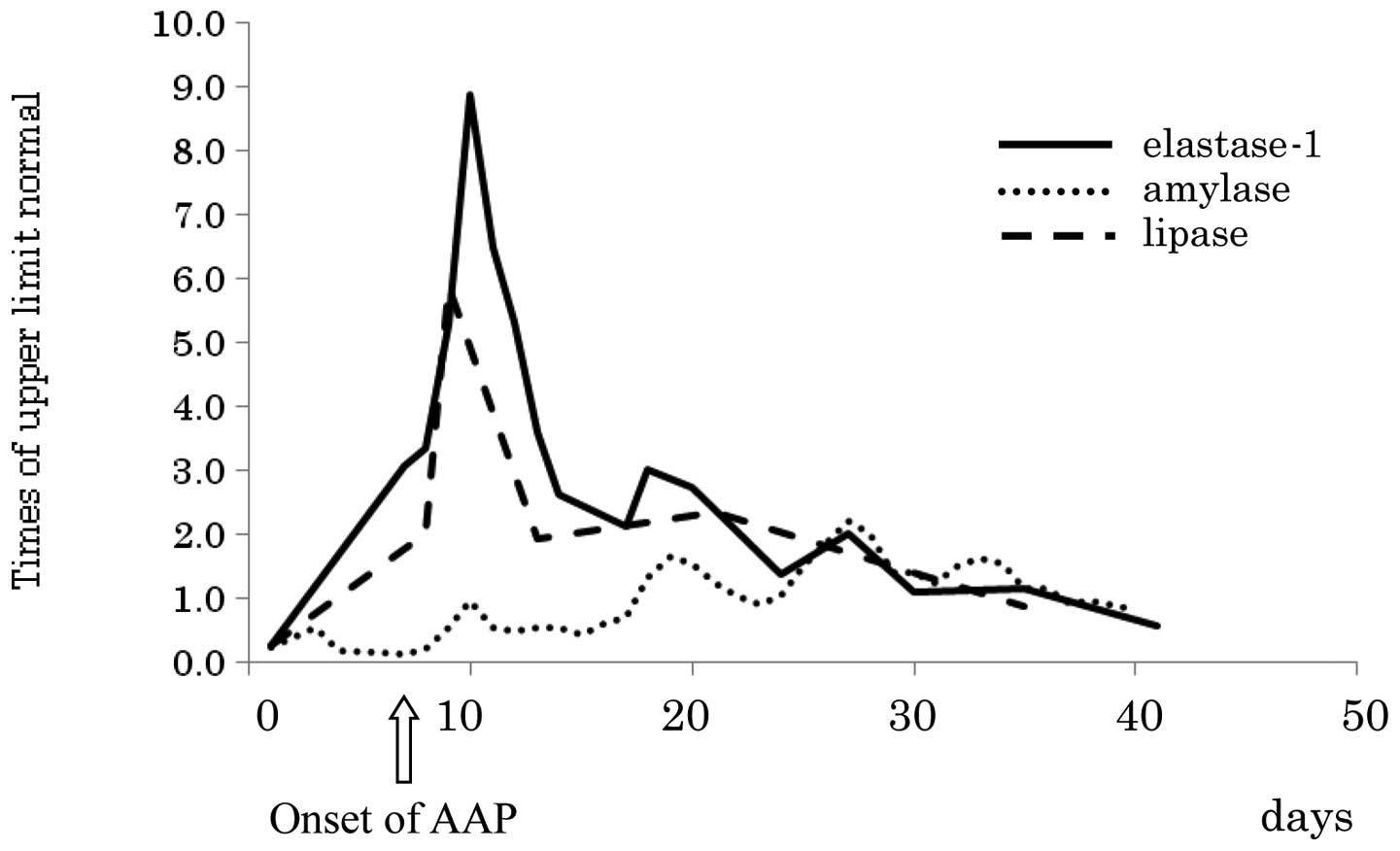
required. The serum amylase levels were normal and CT and US
revealed no abnormality in the pancreas. However, acute
pancreatitis was suspected based on the elevation of serum
elastase-1 levels to 936 ng/dl [upper limit of normal (ULN)] on the
seventh and final day of L-asp administration (Fig. 1), when pleural effusion and ascites
were prominent and presumably associated with acute pancreatitis.
Elevated serum lipase levels were also detected on the following
day. Consequently, treatment for acute pancreatitis was initiated
with octreotide, famotidine and nafamostat. Eleven days after the
detection of elevated serum elastase-1 levels, serum amylase levels
increased to 278 mg/dl (2.2 times the ULN). Thereafter, the
condition of the patient gradually improved without any late
sequelae. The cumulative dose of L-asp administered was 222,000
U/m2.
Case 2
A 10-year-old boy with B-precursor ALL had received
multi-agent chemotherapy according to the L-0416 protocol of TCCSG.
The first remission was achieved without any severe complications.
Six months after the onset of the disease, the patient received
chemotherapy comprising DEX (6 mg/m2 × 14 days), VCR
(1.5 mg/m2 weekly × 4 weeks), ADR (25 mg/m2
weekly × 4 weeks) and L-asp (10,000 U/m2 weekly × 4
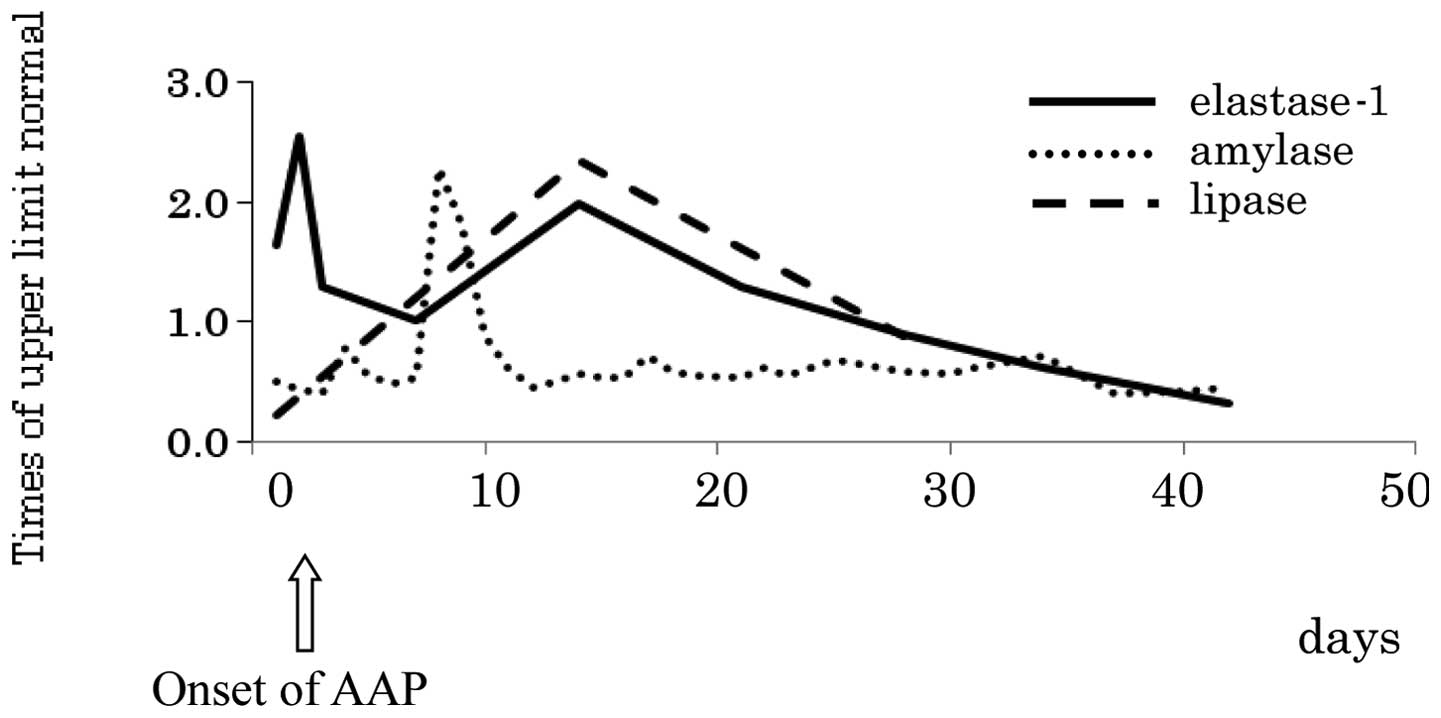
weeks). Two days after the administration of the third L-asp dose,
the patient complained of abdominal pain and emesis. Serum amylase
and lipase levels were normal and imaging studies, namely CT, US
and magnetic resonance imaging, revealed no abnormalities. However,
elevated serum elastase-1 levels to 765 ng/dl were observed
(Fig. 2), which led to the
suspicion of AAP. Consequently, octreotide, famotidine, fentanest
and nafamostat were administered along with parenteral nutrition.
Seven days after the elevation of elastase-1 levels, serum amylase
levels increased to 288 mg/dl (2.3 times the ULN). Therefore, we
were able to diagnose AAP in its early stage. Thereafter, the
condition of the patient improved rapidly without any late
sequelae. The cumulative dose of L-asp administered was 72,000
U/m2.
Discussion
L-asp is a well-known anticancer agent used for the
treatment of lymphoid malignancies. Although it is one of the key
drugs in the treatment of ALL in children (1), it is known to induce several
complications, including coagulopathy, hypersensitivity, hepatic
dysfunction, hypertriglyceridemia, hyperammonemia and pancreatitis.
Of these, AAP has been reported to occur in 3-18% of children with
ALL receiving chemotherapy (2–7). Acute
pancreatitis per se may be a life-threatening disease
(8,9). When a patient develops AAP,
chemotherapy must be interrupted for several months or more and
subsequent administration of L-asp, as recommended in the protocol,
should also be discontinued. Therefore, the overall survival rate
is poorer in patients with compared to those without AAP (10,11).
Serum amylase and lipase levels and findings of
imaging studies are commonly used for the diagnosis of acute
pancreatitis (7,12,13).
Amylase and lipase are the pancreatic enzymes listed in the
metabolites list of Common Terminology Criteria for Adverse Events
as defined by the National Cancer Institute. Elastase-1 is one of
the pancreatic enzymes whose secretion is elevated due to
pancreatic damage (14,15). Whether elastase-1 is a useful marker
in the diagnosis of acute pancreatitis remains to be elucidated
through thorough investigations.
Previous studies reported that elastase-1 is
seemingly less specific and may not be correlated with disease
severity (16,17). By contrast, another study suggested
similar or superior sensitivity of elastase-1 when compared with
that of amylase or lipase in cases of acute pancreatitis (18). A study conducted by Shimizu et
al (19) reported subclinical
pancreatitis accompanied by the elevation of elastase-1 levels in
L-asp-treated ALL patients, who exhibited no symptoms of
pancreatitis and had normal amylase and lipase levels. Although no
patient with definitively diagnosed pancreatitis was included in
that study, the usefulness of elastase-1 levels in the early
diagnosis of AAP was emphasized.
The two cases presented in this study were diagnosed
with definitive pancreatitis by the clinical symptoms and the
subsequent elevation of serum amylase levels. Therefore, elastase-1
may be a beneficial marker for subclinical as well as manifested
pancreatitis in its early stage.
Although early diagnosis and treatment of acute
pancreatitis is imperative, it is occasionally difficult solely by
using standard diagnostic methods. Approximately 1–26% of AAP
patients may suffer from late complications such as pseudo-cyst and
abscess formation (3,8). In our study, the patients recovered
rapidly without any complications, probably due to the mild and
self-limited nature of their AAP. However, early detection and
prompt treatment contributed, to some extent, to the rapid
improvement and lack of late sequelae.
In conclusion, serum elastase-1 appears to be a
useful marker for the early diagnosis of pediatric ALL complicated
by AAP. Therefore, in addition to amylase and lipase levels, the
measurement of elastase-1 levels is recommended when L-asp-treated
patients develop abdominal pain or other symptoms suggestive of the
presence of pancreatitis.
References
|
1.
|
Pui CH and Evans WE: Treatment of acute
lymphoblastic leukemia. N Engl J Med. 354:166–178. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Land VJ, Sutow WW, Fernbach DJ, et al:
Toxicity of L-asparaginase in children with advanced leukemia.
Cancer. 30:339–347. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Sahu S, Saika S, Pai S and Advani SH:
L-asparaginase (Leunase) induced pancreatitis in childhood acute
lymphoblastic leukemia. Pediatr Hematol Oncol. 15:533–538. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Muller HJ and Boos J: Use of
L-asparaginase in childhood ALL. Crit Rev Oncol Hematol. 28:97–113.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Knoderer HM, Robarge J and Flockhart DA:
Predicting asparaginase-associated pancreatitis. Pediatr Blood
Cancer. 49:634–639. 2007. View Article : Google Scholar
|
|
6.
|
Raetz EA and Salzer WL: Tolerability and
efficacy of L-asparaginase therapy in pediatric patients with acute
lymphoblastic leukemia. J Pediatr Hematol Oncol. 32:554–563. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Raja RA, Schmiegelow K and Frandsen TL:
Asparaginase-associated pancreatitis in children. Br J Haematol.
159:18–27. 2012. View Article : Google Scholar
|
|
8.
|
Steinberg W and Tenner S: Acute
pancreatitis. N Engl J Med. 330:1198–1210. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
DeBanto JR, Goday PS, Pedroso MR, et al:
Acute pancreatitis in children. Am J Gastroenterol. 97:1726–1731.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Silverman LB, Gelber RD, Dalton VK, et al:
Improved outcome for children with acute lymphoblastic leukemia:
results of the Dana-Farber Consortium Protocol 91-01. Blood.
97:1211–1218. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Treepongkaruna S, Thongpak N, Pakakasama
S, et al: Acute pancreatitis in children with acute lymphoblastic
leukemia after chemotherapy. J Pediatr Hematol Oncol. 31:812–815.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Yadav D, Agarwal N and Pitchumoni CS: A
critical evaluation of laboratory tests in acute pancreatitis. Am J
Gastroenterol. 97:1309–1318. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Treacy J, Williams A, Bais R, et al:
Evaluation of amylase and lipase in the diagnosis of acute
pancreatitis. ANZ J Surg. 71:577–582. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Satake K, Chung YS and Umeyama K: Serum
elastase 1 levels in pancreatic disease. Am J Surg. 144:239–242.
1982. View Article : Google Scholar
|
|
15.
|
Gullo L, Ventrucci M, Pezzilli R, et al:
Diagnositic value of serum elastase 1 in pancreatic disease. Br J
Surg. 74:44–47. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Büchler M, Malfertheiner P, Uhl W and
Beger HG: Diagnostic and prognostic value of serum elastase 1 in
acute pancreatitis. Klin Wochenschr. 64:1186–1191. 1986.PubMed/NCBI
|
|
17.
|
Millson CE, Charles K, Poon P, et al: A
prospective study of serum pancreatic elastase-1 in the diagnosis
and assessment of acute pancreatitis. Scand J Gastroenterol.
33:664–668. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Flamion B, Delhaye M, Horanyi Z, et al:
Comparison of elastase-1 with amylase, lipase, and trypsin-like
immunoreactivity in the diagnosis of acute pancreatitis. Am J
Gastroenterol. 82:532–535. 1987.PubMed/NCBI
|
|
19.
|
Shimizu T, Yamashiro Y, Igarashi J, et al:
Increased serum trypsin and elastase-1 levels in patients
undergoing L-asparaginase therapy. Eur J Pediatr. 157:561–563.
1998. View Article : Google Scholar : PubMed/NCBI
|