Introduction
Glycated hemoglobin A1c (HbA1c) is a form of
hemoglobin that is measured in order to identify the average
concentration of plasma glucose over the relatively long-term
period of two to three months prior to the date of measurement.
Since HbA1c testing can be performed at any time of the day and
without any special patient preparation (for example, fasting is
not required) and provides more accurate information about the
disease and the patient, it offers improved convenience for
patients and health care providers compared to the oral glucose
tolerance test or taking fasting plasma glucose measurements
(1,2). On
this basis, it has been suggested that HbA1c may serve as a better
indicator for glucose control in diabetic patients than fasting
blood sugar levels (3,4). Furthermore, HbA1c levels have been
proposed as a diagnostic tool for identifying patients with
undiagnosed diabetes or that have an elevated risk of developing
diabetes (5). In 2011, the World
Health Organization and the American Diabetic Association accepted
HbA1c levels ≥6.5% as a diagnostic criterion for diabetes mellitus
(6,7).
However, it is important to take age, race/ethnicity,
anemia/hemoglobinopathies (and other diseases for which HbA1c may
be an unsatisfactory criterion for the diagnosis of type 2
diabetes) into consideration when using the HbA1c levels to
diagnose diabetes (8–15). Further studies are thus required to
promote a more appropriate standard for HbA1c in the diagnosis of
type 2 diabetes. Furthermore, while HbA1c values have been
previously reported to increase with age in Japanese patients
(11), there are no reports about the
association between HbA1c and gender and age in Chinese adults. In
view of whether HbA1c levels may vary with the race or ethnicity of
patients (16,17), the present study aims to evaluate the
association between gender, age and HbA1c levels in Chinese adults
that have not been diagnosed with diabetes mellitus.
Materials and methods
Study subjects
The present retrospective study comprised of 18,265
Chinese adults (aged 18–99 years, average age 51.312±15.252 years;
11,770 males, average age 52.892±15.445 years; 6,495 females,
average age 48.449±14.466 years) who were not known to be suffering
with diabetes and who underwent a comprehensive health examination
between June 2014 and May 2015 at the Shenzhen Third People's
Hospital (Shenzhen, China). The inclusion criteria for the study
was as follows: i) Han ethnicity; ii) age ≥18 years; iii) resident
of mainland China for >1 year; and iv) no previous diagnosis of
diabetes. Exclusion criteria was as follows: Previously known
diabetes, pregnancy, heart/liver/kidney dysfunction, long-term oral
administration of drugs affecting blood glucose, long-term history
of smoking, anemia/hemoglobinopathies, and surgery within the past
month (13,18). The age range of the participants was
divided into seven groups: 18–29, 30–39, 40–49, 50–59, 60–69, 70–79
and ≥80 years. The study protocol was approved by the Ethics
Committee of Shenzhen Third People's Hospital. All the participants
included in the present study provided written informed
consent.
Sample collection and measurement
A 2 ml venous blood sample was collected in the
morning following 8–12 h of overnight fasting. Blood sample HbA1c
levels were measured within 2 h using a high-performance liquid
chromatography VARIANT™ II hemoglobin testing system (Bio-Rad
Laboratories, Inc., Hercules, CA, USA). Detection was performed
strictly in accordance with the manufacturer's instructions using
the original kit, calibration, and quality control. The intra- and
inter-assay coefficients of variation for HbA1c were both <0.8%.
All procedures were carried out by trained doctors at Shenzhen
Third People's Hospital.
Statistical analysis
All data are presented as the mean ± standard
deviation (SD) for variables with normal distribution, the median
(interquartile range) for variables with a non-normal distribution,
or as the number of participants. One variable comparison between
two groups was analysed using an independent sample t-test.
Analysis of one-way ANOVA was first used in multiple groups
comparison, and pairwise comparison in multiple groups was
conducted using the LSD-T method. Correlation analysis among
different variables was performed with Pearson correlation analysis
and linear regression. A value of P<0.05 was considered to
indicate a statistically significant difference. All statistical
analysis was performed using the SPSS software, version 21.0 (IBM
SPSS, Armonk, NY, USA).
Results
Comparison of HbA1c levels in males
and females
As shown in Table I,
there were significant differences (P<0.0001) in HbA1c levels
between the male and female groups in the total study population
(referred to all personnel) and the HbA1c <6.5% (referred to
HbA1c <6.5% personnel). It specifically demonstrated that the
overall levels of HbA1c were higher in male than that in female
(Table I).
 | Table I.Comparison of HbA1c levels of
different gender subjects. |
Table I.
Comparison of HbA1c levels of
different gender subjects.
|
| All personnel | HbA1c <6.5%
personnel | HbA1c ≥6.5%
personnel |
|---|
|
|
|
|
|
|---|
| Groups | No. | HbA1c (%) | No. | HbA1c (%) | No. | HbA1c (%) |
|---|
| Male | 11,770 | 5.619±0.894 | 10,542 | 5.385±0.446 | 1,228 | 7.621±1.212 |
| Female | 6,495 | 5.454±0.706 | 6,192 | 5.347±0.427 | 303 | 7.635±1.400 |
| t-value | 13.730 |
| 5.547 |
| −0.178 |
|
| P-value | <0.0001 |
| <0.0001 |
| 0.859 |
|
Comparison of HbA1c levels across
different age groups
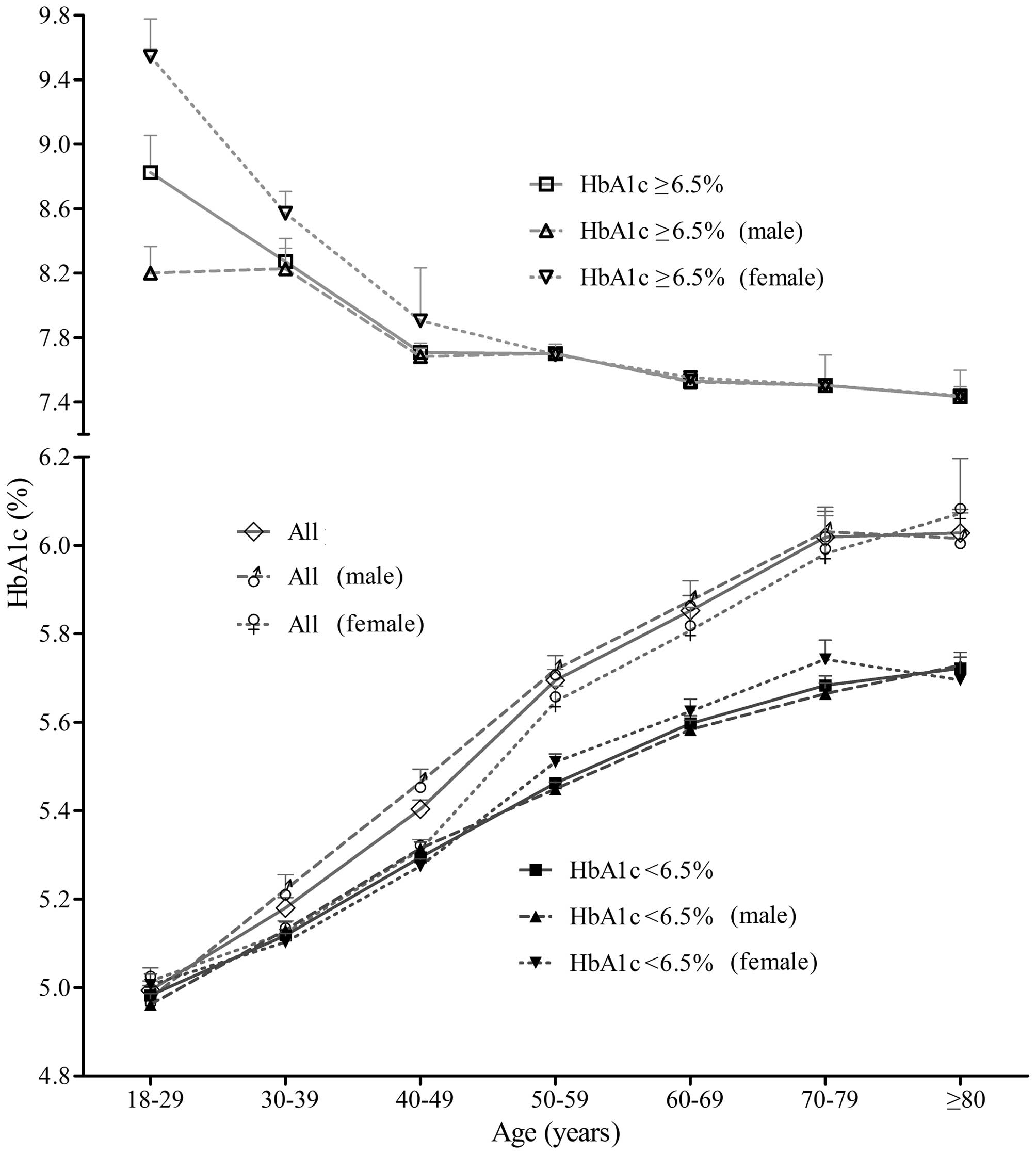
HbA1c test results for all age groups are shown in
Table II and Fig. 1. The data suggested two interesting
results: i) HbA1c values of all personnel and HbA1c <6.5%
personnel, in both males and females, gradually increased with age
until 79 years, and then plateaued (Fig.
1); ii) HbA1c levels of HbA1c ≥6.5% patients of either gender
gradually decreased with age (Fig. 1).
An independent sample t-test was performed on HbA1c levels for
males and females of the same age group. The results showed that
the difference of HbA1c values in different gender of 30–59 years
old subjects was statistically significant (P<0.05), and male
HbA1c levels were higher than those of females (Table II). The difference in HbA1c levels in
different gender of the other four age-groups was not significant
(P>0.05) (Table II).
 | Table II.Comparison of HbA1c levels of
different age groups. |
Table II.
Comparison of HbA1c levels of
different age groups.
|
| All personnel | Male | Female |
|
|
|---|
|
|
|
|
|
|
|
|---|
| Age groups,
years | No. | HbA1c (%) | No. | HbA1c (%) | No. | HbA1c (%) | t-value | P-value |
|---|
| 18–29 | 1,380 | 4.994±0.399 | 727 | 4.975±0.405 | 653 | 5.014±0.392 | −1.829 |
0.068 |
| 30–39 | 2,697 | 5.180±0.605 | 1,566 | 5.221±0.681 | 1,131 | 5.123±0.473 |
4.392 | <0.001 |
| 40–49 | 4,449 | 5.404±0.700 | 2,698 | 5.464±0.790 | 1,751 | 5.310±0.519 |
7.847 | <0.001 |
| 50–59 | 4,905 | 5.695±0.881 | 3,308 | 5.718±0.949 | 1,597 | 5.646±0.718 |
2.954 |
0.003 |
| 60–69 | 2,329 | 5.852±0.853 | 1,548 | 5.875±0.897 | 781 | 5.807±0.759 |
1.914 |
0.056 |
| 70–79 | 1,499 | 6.019±0.950 | 1,144 | 6.031±0.958 | 355 | 5.981±0.924 |
0.885 |
0.377 |
| ≥80 | 1,006 | 6.028±0.858 | 779 | 6.015±0.826 | 227 | 6.072±0.959 | −0.872 |
0.383 |
Correlation between HbA1c levels and
age
Linear regression analysis showed that HbA1c levels
were positively correlated with age in all personnel (increase of
0.020% per decade) and HbA1c <6.5% personnel (increase of 0.014%
per decade), the linear regression equations were HbA1c (%) = 0.020
× age (years) + 4.523 (r=0.369; P<0.0001) and HbA1c (%) = 0.014
× age (years) + 4.659 (r=0.485; P<0.0001), respectively. By
contrast, HbA1c levels were negatively correlated with age in HbA1c
≥6.5% personnel (decreased 0.012% per decade), the linear
regression equation was HbA1c (%) = −0.012 × age (years) + 8.345
(r=0.124; P<0.0001).
Discussion
The results of the current study suggest that
greater attention should be given to patient gender and age when
selecting HbA1c as the criterion in diabetes screening, as has been
reported in previous studies (8,11,13,19–21). HbA1c levels, which were significantly
higher in male than that in female and increased steadily as age
rose, differ significantly by gender and age.
The HbA1c levels of male individuals were
significantly higher than those of females in the 30–59 years
age-groups (P<0.05). It is most likely due to factors such as
blood pressure and blood lipids of males in this age-group have
worse control conditions, and women may be easily affected by
physiological cycle. As in previous reports (19,22–24), gender differences were noted in the
relationship between HbA1c and age. It is possible that this finding
is related to lower hemoglobin levels in menstruating women with
more rapid erythrocyte turnover, as suggested previously (19). Women in peri- and post-menopausal
age-groups had a steeper slope than men.
With increased age, many changes occur in humans,
such as: i) The function of pancreatic islets gradually declines;
ii) tissue sensitivity to insulin and insulin receptor activity
slowly decrease; and iii) muscle tissue gradually reduces and the
consumption of glucose generally decreases. Under the combined
effect of these factors, blood glucose increases with age
incrementally, so that the HbA1c levels are also elevated,
especially with advancing age. Moreover, linear regression analysis
showed that HbA1c levels rose by 0.014% per decade in HbA1c
<6.5% individuals, confirming three previous reports (21,25,26) that indicate age is a significant
independent impact factor of HbA1c.
The strengths of our study are the large sample
size, the strict but random selection of the population and the
wide range of the age distribution. Although our study has an
obvious limitation, that of greatly different numbers of men and
women participants, we feel that our results are compelling and
indicative of the need for further research.
In conclusion, the present study clearly illustrates
the effect of gender and age on HbA1c values in Chinese
populations, which illustrates the diagnostic titer of HbA1c for
diabetes varies in different age/gender groups. Therefore, we
suggest that age and gender should be considered in the application
of HbA1c for the diagnosis of diabetes.
Acknowledgements
The present study was supported by grants from the
Shenzhen Science and Technology Innovation Committee (grant nos.
JCYJ20130401164749996, JCYJ20140411113637598 and
JCYJ20140411111718161).
References
|
1
|
Rohlfing CL, Little RR, Wiedmeyer HM,
England JD, Madsen R, Harris MI, Flegal KM, Eberhardt MS and
Goldstein DE: Use of GHb (HbA1c) in screening for undiagnosed
diabetes in the U.S. population. Diabetes Care. 23:187–191. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kumpatla S, Aravindalochanan V, Rajan R,
Viswanathan V and Kapur A: Evaluation of performance of A1c and FPG
tests for screening newly diagnosed diabetes defined by an OGTT
among tuberculosis patients-a study from India. Diabetes Res Clin
Pract. 102:60–64. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lippi G, Mattiuzzi C and Targher G:
Glycated hemoglobin, diabetes, and cardiovascular risk in
nondiabetic adults. N Engl J Med. 362:2030–2031; author reply 2031.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bicescu G: Glycated hemoglobin, diabetes,
and cardiovascular risk in nondiabetic adults. Maedica (Buchar).
5:80–81. 2010.PubMed/NCBI
|
|
5
|
International Expert Committee:
International Expert Committee report on the role of the A1C assay
in the diagnosis of diabetes. Diabetes Care. 32:1327–1334. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Metzger BE, Buchanan TA, Coustan DR, de
Leiva A, Dunger DB, Hadden DR, Hod M, Kitzmiller JL, Kjos SL, Oats
JN, et al: Summary and recommendations of the Fifth International
Workshop-Conference on Gestational Diabetes Mellitus. Diabetes
Care. 30(Suppl 2): S251–S260. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Colagiuri S: Glycated haemoglobin (HbA1c)
for the diagnosis of diabetes mellitus - practical implications.
Diabetes Res Clin Pract. 93:312–313. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Davidson MB and Schriger DL: Effect of age
and race/ethnicity on HbA1c levels in people without known diabetes
mellitus: Implications for the diagnosis of diabetes. Diabetes Res
Clin Pract. 87:415–421. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Selvin E, Francis LM, Ballantyne CM,
Hoogeveen RC, Coresh J, Brancati FL and Steffes MW: Nontraditional
markers of glycemia: Associations with microvascular conditions.
Diabetes Care. 34:960–967. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cohen RM, Franco RS, Khera PK, Smith EP,
Lindsell CJ, Ciraolo PJ, Palascak MB and Joiner CH: Red cell life
span heterogeneity in hematologically normal people is sufficient
to alter HbA1c. Blood. 112:4284–4291. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Inoue M, Inoue K and Akimoto K: Effects of
age and sex in the diagnosis of type 2 diabetes using glycated
haemoglobin in Japan: The Yuport Medical Checkup Centre study. PLoS
One. 7:e403752012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kramer CK, Araneta MR and Barrett-Connor
E: A1C and diabetes diagnosis: The Rancho Bernardo Study. Diabetes
Care. 33:101–103. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang L, Shen X, Yan S, Xu F and Wu P: The
effectiveness of age on HbA1c as a criterion for the diagnosis of
diabetes in Chinese different age subjects. Clin Endocrinol (Oxf).
82:205–212. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao X, Chang Mei H, Chen L, Jiang L, He
M, Chen J, Hu Z, Ye H, Hu H, Zhou L, et al: An increased level of
haemoglobin A1C predicts a poorer clinical outcome in patients with
acute pancreatitis. Clin Endocrinol (Oxf). 77:241–245. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang L, Shen X, Yan S, Yuan X, Lu J and
Wei W: HbA1c in the diagnosis of diabetes and abnormal glucose
tolerance in patients with Graves' hyperthyroidism. Diabetes Res
Clin Pract. 101:28–34. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ziemer DC, Kolm P, Weintraub WS, Vaccarino
V, Rhee MK, Twombly JG, Narayan KM, Koch DD and Phillips LS:
Glucose-independent, black-white differences in hemoglobin A1c
levels: A cross-sectional analysis of 2 studies. Ann Intern Med.
152:770–777. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kumar PR, Bhansali A, Ravikiran M,
Bhansali S, Dutta P, Thakur JS, Sachdeva N, Bhadada SK and Walia R:
Utility of glycated hemoglobin in diagnosing type 2 diabetes
mellitus: A community-based study. J Clin Endocrinol Metab.
95:2832–2835. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Koda M, Kitamura I, Okura T, Otsuka R,
Ando F and Shimokata H: The associations between smoking habits and
serum triglyceride or hemoglobin A1c levels differ according to
visceral fat accumulation. J Epidemiol. 2015.PubMed/NCBI
|
|
19
|
Yang YC, Lu FH, Wu JS and Chang CJ: Age
and sex effects on HbA1c. A study in a healthy Chinese population.
Diabetes Care. 20:988–991. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yates AP and Laing I: Age-related increase
in haemoglobin A1c and fasting plasma glucose is accompanied by a
decrease in beta cell function without change in insulin
sensitivity: Evidence from a cross-sectional study of hospital
personnel. Diabet Med. 19:254–258. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pani LN, Korenda L, Meigs JB, Driver C,
Chamany S, Fox CS, Sullivan L, D'Agostino RB and Nathan DM: Effect
of aging on A1C levels in individuals without diabetes: Evidence
from the Framingham Offspring Study and the National Health and
Nutrition Examination Survey 2001–2004. Diabetes Care.
31:1991–1996. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Karar T, Alhammad RI, Fattah MA, Alanazi A
and Qureshi S: Relation between glycosylated hemoglobin and lipid
and thyroid hormone among patients with type 2 diabetes mellitus at
King Abdulaziz Medical City, Riyadh. J Nat Sci Biol Med. 6(Suppl
1): S75–S79. 2015.PubMed/NCBI
|
|
23
|
Takao T, Matsuyama Y, Suka M, Yanagisawa H
and Iwamoto Y: The combined effect of visit-to-visit variability in
HbA1c and systolic blood pressure on the incidence of
cardiovascular events in patients with type 2 diabetes. BMJ Open
Diabetes Res Care. 3:e0001292015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wu CH, Yao WJ, Lu FH, Wu JS and Chang CJ:
Relationship between glycosylated hemoglobin, blood pressure, serum
lipid profiles and body fat distribution in healthy Chinese.
Atherosclerosis. 137:157–165. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sacks DB, Arnold M, Bakris GL, Bruns DE,
Horvath AR, Kirkman MS, Lernmark A, Metzger BE and Nathan DM:
Guidelines and recommendations for laboratory analysis in the
diagnosis and management of diabetes mellitus. Clin Chem.
57:e1–e47. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sacks DB, Arnold M, Bakris GL, Bruns DE,
Horvath AR, Kirkman MS, Lernmark A, Metzger BE and Nathan DM:
National Academy of Clinical Biochemistry; Evidence-Based
Laboratory Medicine Committee of the American Association for
Clinical Chemistry: Guidelines and recommendations for laboratory
analysis in the diagnosis and management of diabetes mellitus.
Diabetes Care. 34:e61–e99. 2011. View Article : Google Scholar : PubMed/NCBI
|