Introduction
Purple urine bag syndrome (PUBS) is an uncommon
condition that occurs in urinary catheterized patients with urinary
tract infection (UTI). It was first described in 1978, though a
possible mechanism was not established until 1988 (1,2). With
regard to the mechanism, tryptophan is metabolized by intestinal
bacteria, after which the by-product indoxyl sulfate is expelled
into the urine and digested into indoxyl by sulfatases/phosphatases
produced by certain bacteria including Escherichia coli (E.
coli), Proteus mirabilis, Morganella morganii (M. morganii),
Klebsiella pneumoniae, Providencia stuartii, Providencia
rettgeri and Pseudomonas aeruginosa (2,3). This
indoxyl may convert into indigo and indirubin in the urine drainage
bag and create purple discoloration (2).
A higher prevalence of PUBS has been reported in
females and in patients with alkaline urine, an indwelling urinary
catheter and constipation (3). The
majority of patients with PUBS are catheterized due to significant
disability, typically being chair-bound or bed-bound elderly
patients (3). In previous years, PUBS
has been considered to be a benign syndrome rather than a disease
with lethal potential, and appropriate empirical oral antibiotics
including ciprofloxacin remain to be suggested for its treatment
(3). To the best of our knowledge,
there have been no previous studies on the clinicopathological or
epidemiological trends of PUBS; therefore, the current study
retrospectively reviewed PUBS cases for characteristic analysis. A
systematic review of PUBS cases reported between October 1980 and
August 2016 was conducted, in which data regarding patient age and
gender, comorbidities (diabetes mellitus, uremia, constipation and
residence in long-term care facility), vital signs (presence or
absence of fever), laboratory tests results [seral white blood cell
(WBC) count, urine pH value] and mortality were evaluated. This
aimed to identify trends in the epidemiology of PUBS. Through the
systematic approach, the different clinicopathological aspects and
general trends of PUBS were determined.
Materials and methods
Search strategy and article
selection
A systematic review was designed to investigate
clinicopathological characteristics in PUBS, including patient age
and gender, urine pH value, presence of fever, shock (defined by
hypotension), WBC count, constipation and comorbidities (diabetes
mellitus, uremia), urine culture bacteriology, rates of patients in
long-term care units and mortality. To determine the trends in the
epidemiology of PUBS, the differences in these characteristics over
three decades were also analyzed. A search was performed for
articles in the PubMed database (https://www.ncbi.nlm.nih.gov/pubmed/) including the
word ‘purple urine bag syndrome’ in the title, published in the
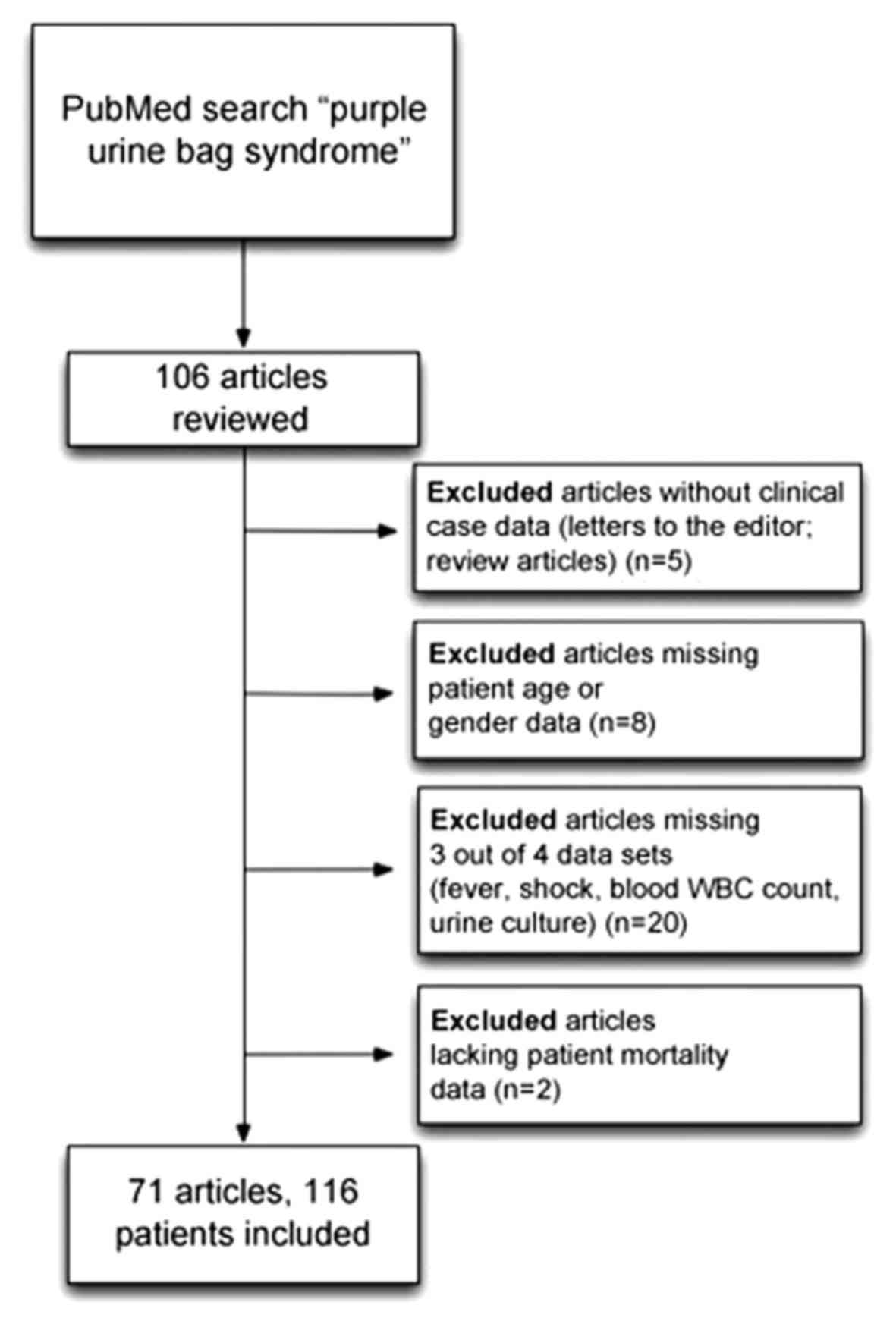
period from January 1, 1980 to September 1, 2016. A total 106
relevant articles were identified. Of these, 33 articles were
excluded owing to ineligibility or lack of essential information.
The full exclusion criteria are depicted in (Fig. 1). Therefore, 71 articles with patient
data on 116 cases (4–74) were collected for review (Table I). The articles were divided into
three groups by publication year: 1991 to 2000, 2001 to 2010 and
2011 to 2016. The following clinical features were defined as: i)
Elderly patients: age ≥65 years old; ii) fever: body temperature
≥38°C; iii) hypotension: systolic blood pressure <90 mmHg or
diastolic blood pressure <60 mmHg.
 | Table I.Case demongraphics of the 71 articles
included in the present study. |
Table I.
Case demongraphics of the 71 articles
included in the present study.
| Author | Year | Language | Country | Cases | Mean age ± SD
(years old) | Refs. |
|---|
| Umeki | 1993 | Japanese | Japan | 4 | 80±1.41 | (4) |
| Nobukuni et
al | 1995 | Japanese | Japan | 5 | 60.4±10.61 | (5) |
| Al-Jubouri and
Vardhan | 2001 | English | UK | 1 | 85 | (6) |
| Ihama and
Hokama | 2002 | English | Japan | 1 | 93 | (7) |
| Vallejo-Manzur
et al | 2005 | English | USA | 1 | 72 | (9) |
| Wang et
al | 2005 | English | Taiwan | 2a | 61 | (10) |
| Rohaut et
al | 2005 | French | France | 1 | 81 | (8) |
| Achtergael et
al | 2006 | English | Belgium | 1 | 77 | (11) |
| Beunk et
al | 2006 | English | UK | 1 | 84 | (12) |
| Tang | 2006 | English | Hong Kong | 2 | 76±8.49 | (13) |
| Su et
al | 2007 | English | Taiwan | 1 | 61 | (20) |
| Nair et
al | 2007 | English | UK | 1 | 83 | (18) |
| Bar-Or et
al | 2007 | English | USA | 1 | 68 | (14) |
| Gautam et
al | 2007 | English | India | 1 | 70 | (15) |
| Ting et
al | 2007 | English | Taiwan | 1 | 72 | (21) |
| Lazimy et
al | 2007 | French | France | 1 | 74 | (17) |
| Harun et
al | 2007 | English | Brunei | 2 | 60±21.21 | (16) |
| Pillai et
al | 2007 | English | UK | 1 | 76 | (19) |
| Lin et
al | 2008 | English | Taiwan | 10 | 75.3±2.12 | (24) |
| Chiang et
al | 2008 | Chinese | Taiwan | 1 | 73 | (22) |
| Chung et
al | 2008 | English | Taiwan | 1 | 85 | (23) |
| Vidarsdottir et
al | 2008 | Icelandic | Iceland | 1 | 72 | (27) |
| Shiao et
al | 2008 | English | Taiwan | 14 | 80.9±11.5 | (26) |
| Muneoka et
al | 2008 | Japanese | Japan | 6 | 87.7±16.26 | (25) |
| Tasi et
al | 2009 | English | Taiwan | 2 | 64±19.8 | (30) |
| Al-Sardar and
Haroon | 2009 | English | UK | 1 | 82 | (28) |
| Wu et
al | 2009 | English | Taiwan | 1 | 95 | (32) |
| van Iersel and
Mattijssen | 2009 | English | Netherlands | 1 | 72 | (31) |
| Pillai et
al | 2009 | English | Singapore | 1 | 69 | (29) |
| Ferrara et
al | 2010 | English | Italy | 1 | 81 | (33) |
| Hirzallah and
D'Souza | 2010 | English | Jordan | 1 | 78 | (34) |
| Siu and
Watanabe | 2010 | English | USA | 1 | 48 | (35) |
| Su et
al | 2010 | English | Taiwan | 1 | 81 | (36) |
| Kang et
al | 2011 | English | Korea | 3 | 74.7±0 | (37) |
| Keenan and
Thompson | 2011 | English | USA | 1 | 97 | (38) |
| Khan et
al | 2011 | English | USA | 1 | 39 | (39) |
| Peters et
al | 2011 | English | Australia | 1 | 82 | (40) |
| Zeier et
al | 2011 | English | Singapore | 1 | 75 | (41) |
| Bocrie et
al | 2012 | English | France | 1 | 87 | (42) |
| Cantaloube et
al | 2012 | French | France | 2 | 81.5±0.71 | (43) |
| Dominguez Alegria
et al | 2012 | Spanish | Spain | 1 | 78 | (44) |
| Meekins et
al | 2012 | English | USA | 1 | 67 | (45) |
| Montasir and
Mustaque | 2013 | English | Bangladesh | 1 | 86 | (46) |
| Bhattarai et
al | 2013 | English | USA | 1 | 87 | (47) |
| Canavese et
al | 2013 | English | Italy | 3 | 79±19.52 | (48) |
| Duff | 2013 | English | USA | 1 | 57 | (49) |
| Iglesias Barreira
et al | 2013 | Spanish | Spain | 2 | 93.5±2.12 | (50) |
| Mohamad and
Chong | 2013 | English | Brunei | 1 | 78 | (51) |
| Ungprasert et
al | 2013 | English | USA | 1 | 44 | (52) |
| Wolff et
al | 2013 | French | France | 1 | 90 | (53) |
| Yaqub et
al | 2013 | English | Pakistan | 1 | 83 | (54) |
| Agapakis et
al | 2014 | English | Greece | 1 | 82 | (55) |
| Chassin-Trubert
et al | 2014 | Spanish | Chile | 1 | 72 | (56) |
| Delgado et
al | 2014 | English | Mexico | 1 | 60 | (57) |
| Hloch et
al | 2014 | Czech | Czech Republic | 1 | 73 | (58) |
| Restuccia and
Blasi | 2014 | English | Italy | 1 | 81 | (59) |
| Sheehan | 2014 | English | USA | 1 | 80 | (60) |
| Abubacker et
al | 2015 | English | India | 1 | 36 | (61) |
| Alex et
al | 2015 | English | India | 1 | 83 | (62) |
| Karim et
al | 2015 | English | USA | 1 | 83 | (63) |
| Kenzaka | 2015 | English | Japan | 1 | 72 | (64) |
| Mohamed Faisal
et al | 2015 | English | Malaysia | 1 | 68 | (65) |
| Mondragon-Cardona
et al | 2015 | English | Colombia | 1 | 71 | (66) |
| Neweling and
Janssens | 2015 | German | Germany | 1 | 78 | (67) |
| Redwood et
al | 2015 | English | USA | 1 | 90 | (68) |
| Van Keer et
al | 2015 | English | Belgium | 2 | 80.5±0.71 | (69) |
| Demelo-Rodriguez
et al | 2016 | English | Spain | 1 | 83 | (70) |
| Faridi et
al | 2016 | English | India | 1 | 76 | (71) |
| Richardson-May | 2016 | English | UK | 1 | 94 | (72) |
| Sriramnaveen et
al | 2016 | English | India | 1 | 85 | (73) |
| Tul Llah et
al | 2016 | English | USA | 1 | 52 | (74) |
Statistical analysis
The data was analyzed with SPSS statistical software
for Windows, version 11.5 (SPSS Inc., Chicago, IL, USA). Values are
presented as the mean ± standard deviation. Statistical
χ2 tests were performed and the threshold for
significance was set at P<0.05 (two-tailed).
Results
Description of the selected
articles
In the present study, 106 relevant articles were
retrieved. Following application of the inclusion and exclusion
criteria, 71 eligible articles (4–74) were
selected (57 in English, 4 in French, 3 in Spanish, 3 in Japanese,
1 in Chinese, 1 in German, 1 in Icelandic and 1 in Czech; Fig. 1 and Table
I). All the selected articles were images in clinical medicine,
individual case reports or serial case reports. The 71 articles
included a total of 116 PUBS cases aged from 36 to 100 years old
with a mean age ± standard deviation of 75.6±12.8 years. Of these,
47 cases were male (40.5%) and 69 were female (59.5%). Of these, 98
cases (84.5%) were elderly (≥65 years old).
Clinical characteristics in PUBS
The mean age of the patients was 75.6 years old, and
PUBS was more commonly observed in females than in males (1.5:1
ratio). As PUBS is associated with infectious pathology, mean WBC
was determined for the cases, which was elevated to 12,242
cells/µl. Only 11.8% of cases presented with fever, and 8.6% of
cases with shock. There were 6.9% of cases with acidic urine
(pH<7), while the remaining cases (93.1%) had urine pH>7. The
majority of cases (69.8%) had constipation, and 58.3% lived in
long-term care units. Regarding chronic co-morbidity, 19.2% of
cases had diabetes mellitus and 18.8% were uremic patients. Overall
mortality rate was 6.8%, thus indicating that PUBS may be
associated with patients' mortality and not always a benign
process.
Clinical characteristics in trend per
decade of PUBS cases
Regarding patient age, urine pH value, the presence
of fever, shock or uremia, a history of diabetes, and residence in
a long-term care unit, there were no significant changes over
subsequent decades among the PUBS cases (Table II). However, an increase in WBC count
from 2001–2010 to 2011–2016 (P=0.002; Table II), and in the male: female ratio
with each decade (P=0.018; Table I
and Fig. 2) were identified. Notably,
WBC count reached 17,060±14,480 cells/µl in the most recent five
years. Conversely, decreases in constipation rates (P=0.011;
Table II) and mortality rates
(P=0.001; Table II and Fig. 3) were also identified over the
subsequent decades. These decreasing rates may be attributed to
advancements in antibiotic treatment and the application of early
goal-directed-therapy (EGDT).
 | Table II.Comparisons of purple urine bag
syndrome cases (n=116) over the last three decades. |
Table II.
Comparisons of purple urine bag
syndrome cases (n=116) over the last three decades.
|
|
| Decade, mean±SD or
% (total cases, n) |
|
|---|
|
|
|
|
|
|---|
|
Characteristics | Total period, mean
± SD or % (total cases, n) | 1991–2000 | 2001–2010 | 2011–2016 | P-value
(two-tailed) |
|---|
| Age | 75.6±12.8
(116) | 69.1±13.1 (9) | 75.9±11.3 (59) | 75.8±16.8 (48) | 0.857 |
| Mean WBC count,
cells/µl | 12,242.7±10,661.5
(27) | NA | 9,203.3±3,736.7
(15) | 17,060.0±14,480.4
(12) | 0.002 |
| Urine pH value | 8.0±0.9 (72) | 8.1±0.7 (6) | 8.0±0.9 (36) | 8.0±1.1 (30) | 0.368 |
| Male: female | 47:69 (116) | 2:7 (9) | 22:39 (61) | 23:23 (46) | 0.018 |
| Fever | 12.1 (14/116) | 22.2 (2/9) | 9.8 (6/61) | 13.0 (6/46) | 0.360 |
| Shock | 8.6 (10/116) | 0.0 (0/9) | 9.8 (6/61) | 8.7 (4/46) | 0.418 |
| Constipation | 69.8 (44/63) | 100.0 (4/4) | 68.4 (26/38) | 66.7 (14/21) | 0.011 |
| Diabetes
mellitus | 19.2 (19/99) | 11.1 (1/9) | 25.6 (11/43) | 14.9 (7/47) | 0.266 |
| Uremia | 18.8 (21/112) | 11.1 (1/9) | 20.0 (12/60) | 18.6 (8/43) | 0.267 |
| Long-term care
unit | 58.3 (35/60) | NA | 60.0 (27/45) | 53.3 (8/15) | 0.057 |
| Mortality | 6.8 (8/116) | 11.1 (1/9) | 8.2 (5/61) | 4.3 (2/46) | 0.001 |
Bacteriology statistics
Bacterial species identified in urine cultures of
the PUBS patients are listed in Table
II. Culture results were not available for 9 cases, and there
was no bacteria growth for 2 cases. Among the 105 patients with
positive results, 3 patients yielded unidentified mixed organisms.
The top five most common bacterial species identified were E.
coli., Enterococcus spp., Proteus spp., M. morganii and
Klebsiella spp.
Discussion
It is well established that urinary tract infection
(UTI) may occur at variable ages, while PUBS is commonly observed
in elderly compared with non-elderly patients (3), as in the present report (84.5 vs.
15.5%). As we know, PUBS can be observed in sepsis of asymptomatic
bacteriuria (ABU) or CA-UTI.
The mechanism of PUBS originates from the dietary
digestion and absorption of tryptophan in the bowel. Bacteria in
the intestine metabolize the tryptophan to indole, and further
hepatic enzymes form the conjugate indoxyl sulfate for secretion
into urine by the kidneys. In the urinary tract, gram-negative
bacteria phosphatases and sulfatases metabolize the indoxyl sulfate
to indoxyl, and through oxidation, this may convert to indigo and
indirubin (2). For patients with
indwelling catheters, blue indigo deposited on the urine drainage
bag surface and red indirubin dissolved in the urine mixes into a
purple discoloration (2). A previous
study demonstrated that not all bacterial organisms of the same
species produce the phosphatase and sulfatase enzymes (2). Based on the above mechanism, bacteriuria
should be present in all patients with PUBS, which should be
diagnosed as ABU for those without clinical symptoms or signs
including fever or shock. A case control study reported that
bacterial counts in urine were significantly higher (by 1 to 2
logs) in patients with PUBS compared with those without the
syndrome, thus suggesting that a higher bacterial load in the urine
is an important factor leading to PUBS (75).
Regarding gender, females are generally more
vulnerable to UTI and PUBS, and female gender has been previously
considered a risk factor of catheter-associated (CA)-UTI among
urinary catheterized patients (76,77). In
the present study, the number of PUBS cases became equal between
the genders within the most recent 5 years. A similar finding was
observed in a recent prospective observational study performed
between November 2011 and October 2013 (78). This study analyzed the incidence of
healthcare-associated urinary tract infections in patients admitted
to the urology ward of University Hospital 12 de Octubre in Spain
with an indwelling urinary catheter. The incidence of CA-UTI in
males vs. females was 8.22 vs. 8.46% without significant difference
(78). The study also analyzed the
four most frequently cultured bacteria species in CA-UTI (E.
coli, Enterococcus, Klebsiella, Pseudomonas) and identified no
significant difference between genders. The diversities in the
results of these studies results may be affected by other
unidentified factors, including urinary catheter management or
personal hygiene influence.
In accordance with PUBS being associated with
infectious pathology of the urinary tract, the mean WBC count of
all reviewed cases was elevated to 12,242/µl. Furthermore, WBC
count significantly increased with time between 2001–2010 and
2011–2016.
There were 11.8% of PUBS cases presenting with fever
and 8.6% of cases presenting with hypotension without significant
difference between the decades. A total of 58.3% of subjects lived
in long-term care units, and 19.2% had a history of diabetes. Urine
pH value was the most stationary variable in each decade, varying
between 8.0 and 8.1, which is compatible with the recognized
conclusion from studies on PUBS: That PUBS more readily occurs in
alkaline over acidic urine (2–4).
A small cohort study of Taiwanese patients
demonstrated chronic kidney disease (CKD) to be a risk factor for
PUBS (79). The serum and urine
levels of indoxyl sulfate are increased markedly in patients with
chronic kidney disease or in those undergoing dialysis due to
impaired renal clearance (80). In
the present study, 18.8% of PUBS cases had a history of uremia.
Previous studies have also indicated comorbid conditions including
diabetes mellitus, dementia and iron deficiency anemia are
independent risk factors for ABU and UTI (80,81).
It has previously been concluded there is an
association of CA-UTI with increased mortality rate and prolonged
length of stay in acute care facilities (82). Furthermore, for PUBS involving
Fournier's gangrene in immunosuppressed patients, the morbidity and
mortality rates were increased (30).
Nevertheless, in uremic patients with PUBS, the elimination of
indoxyl sulfate during dialysis is limited as it is bound to
albumin, leading to exponential increase in serum indoxyl sulfate
concentration. When treating patients with CKD and PUBS, clinicians
should consider the elevated serum and urinary concentration of
indoxyl sulfate due to its potential role in the progression of
CKD, as well as its contribution to cardiovascular events (57).
Constipation is considered to be a predisposing
factor in PUBS due to the increased time it elicits for bacterial
deamination. In the present study, constipation rate significantly
decreased after 2001, though this may have been an artifact based
on the relatively small number of cases reported in the decade of
1991–2000.
Overall mortality rate was 6.8%, thus indicating
that PUBS is not always a benign process. However, mortality rate
declined with time over the three decades, concordant with the
introduction of EGDT for severe sepsis in 2001 (83). Therefore, this progress may be
attributed to the new recommendation of EGDT, which may achieve
aggressive correction of septic shock when combined with early
appropriate antibiotic administration. Nonetheless, the mortality
rate of patients with severe sepsis declined following the
implementation of EGDT (84–87). A recent meta-analysis study also
concluded that important factors contributing to improved outcome
are time-to-first antibiotic administration and appropriate
antibiotic use (88).
In conclusion, the ratio of males: females with PUBS
increased over recent decades. Therefore, the urine color in
catheterized patients should be monitored not only in female but
also male patients. PUBS may not always be a benign process, and
emphasis is required on early examination and aggressive antibiotic
administration. Although WBC count was elevated over the recent
decades, the morality rate was lowest in the most recent five years
and decreased by decade; the overall mortality rate was 6.8%, and
lowered to 4.3% in the last five years.
This was a case-controlled study that searched
relevant articles in the PubMed database. A limitation of this may
have been the exclusion of cases based on inadequate information,
leading to bias and introducing confounding factors. Furthermore,
the relatively small number of PUBS studies in each decade may have
limited the accuracy of statistical analyses. There may also be
cases of PUBS unreported in the PubMed database which were
unaccounted for.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the authors on reasonable request.
Authors' contributions
The final version of the manuscript has been read
and approved by all authors. YHW collected the data and wrote the
draft. SYJ planned and revised the study and is the primary
correspondent.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Barlow GB and Dickson JAS: PURPLE URINE
BAGS. Lancet. 311:220–221. 1978. View Article : Google Scholar
|
|
2
|
Dealler SF, Hawkey PM and Millar MR:
Enzymatic degradation of urinary indoxyl sulfate by Providencia
stuartii and Klebsiella pneumoniae causes the purple urine bag
syndrome. J Clin Microbiol. 26:2152–2156. 1988.PubMed/NCBI
|
|
3
|
Su FH, Chung SY, Chen MH, Sheng ML, Chen
CH, Chen YJ, Chang WC, Wang LY and Sung KY: Case analysis of purple
urine-bag syndrome at a long-term care service in a community
hospital. Chang Gung Med J. 28:636–642. 2005.PubMed/NCBI
|
|
4
|
Umeki S: Purple urine bag syndrome (PUBS)
associated with strong alkaline urine. Kansenshogaku Zasshi.
67:1172–1177. 1993.(In Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nobukuni K, Kawahara S, Nagare H and
Fujita Y: Study on purple pigmentation in five cases with purple
urine bag syndrome. Kansenshogaku Zasshi. 69:1269–1271. 1995.(In
Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Al-Jubouri MA and Vardhan MS: A case of
purple urine bag syndrome associated with Providencia rettgeri. J
Clin Pathol. 54:4122001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ihama Y and Hokama A: Purple urine bag
syndrome. Urology. 60:9102002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rohaut B, Bachmeyer C, Lecomte I, Ravet N
and Grateau G: A urine bag turns purple. Rev Med Interne.
26:666–667. 2005.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vallejo-Manzur F, Mireles-Cabodevila E and
Varon J: Purple urine bag syndrome. Am J Emerg Med. 23:521–524.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang IK, Ho DR, Chang HY, Lin CL and
Chuang FR: Purple urine bag syndrome in a hemodialysis patient.
Intern Med. 44:859–861. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Achtergael W, Michielsen D, Gorus FK and
Gerlo E: Indoxyl sulphate and the purple urine bag syndrome: A case
report. Acta Clin Belg. 61:38–41. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Beunk J, Lambert M and Mets T: The purple
urine bag syndrome. Age Ageing. 35:5422006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tang MW: Purple urine bag syndrome in
geriatric patients. J Am Geriatr Soc. 54:560–561. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bar-Or D, Rael LT, Bar-Or R, Craun ML,
Statz J and Garrett RE: Mass spectrometry analysis of urine and
catheter of a patient with purple urinary bag syndrome. Clin Chim
Acta. 378:216–218. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gautam G, Kothari A, Kumar R and Dogra PN:
Purple urine bag syndrome: A rare clinical entity in patients with
long term indwelling catheters. Int Urol Nephrol. 39:155–156. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Harun NS, Nainar SK and Chong VH: Purple
urine bag syndrome: A rare and interesting phenomenon. South Med J.
100:1048–1050. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lazimy Y, Delotte J, Machiavello JC,
Lallement M, Imbenotte M and Bongain A: Purple urine bag syndrome:
A case report. Prog Urol. 17:864–865. 2007.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nair UV, Chattopadhyay I, Giles M, Curtis
G and Mannion PT: Purple urine bag syndrome in an octogenarian
male. Br J Hosp Med (Lond). 68:1052007.PubMed/NCBI
|
|
19
|
Pillai RN, Clavijo J, Narayanan M, et al:
An association of purple urine bag syndrome with intussusception.
Urology. 70:812 e1–2. 2007. View Article : Google Scholar
|
|
20
|
Su YJ, Lai YC and Chang WH: Purple urine
bag syndrome in a dead-on-arrival patient: case report and articles
reviews. Am J Emerg Med. 25:861 e5–6. 2007. View Article : Google Scholar
|
|
21
|
Ting IW, Wang R, Wu VC, Hsueh PR and Hung
KY: Purple urine bag syndrome in a hemodialysis patient. Kidney
Int. 71:9562007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chiang HC, Huang MS and Cheng CC: An
experience providing home care to a victim of cerebral vascular
accident and purple urine bag syndrome. Hu Li Za Zhi. 55:98–104.
2008.(In Chinese). PubMed/NCBI
|
|
23
|
Chung SD, Liao CH and Sun HD: Purple urine
bag syndrome with acidic urine. Int J Infect Dis. 12:526–527. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lin CH, Huang HT, Chien CC, Tzeng DS and
Lung FW: Purple urine bag syndrome in nursing homes: Ten elderly
case reports and a literature review. Clin Interv Aging. 3:729–734.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Muneoka K, Igawa M, Kurihara N, Kida J,
Mikami T, Ishihara I, Uchida J, Shioya K, Uchida S and Hirasawa H:
Biochemical and bacteriological investigation of six cases of
purple urine bag syndrome (PUBS) in a geriatric ward for dementia.
Nippon Ronen Igakkai Zasshi. 45:511–519. 2008.(In Japanese).
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shiao CC, Weng CY, Chuang JC, Huang MS and
Chen ZY: Purple urine bag syndrome: A community-based study and
literature review. Nephrology (Carlton). 13:554–559. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vidarsdottir H, Palsson R and Gudbjartsson
T: Case of the month; purple urine bag syndrome (PUBS).
Laeknabladid. 94:383–385. 2008.(In Icelandic). PubMed/NCBI
|
|
28
|
Al-Sardar H and Haroon D: Purple urinary
bag syndrome. Am J Med. 122:e1–e2. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Pillai BP, Chong VH and Yong AM: Purple
urine bag syndrome. Singapore Med J. 50:e193–e194. 2009.PubMed/NCBI
|
|
30
|
Tasi YM, Huang MS, Yang CJ, Yeh SM and Liu
CC: Purple urine bag syndrome, not always a benign process. Am J
Emerg Med. 27:895–897. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
van Iersel M and Mattijssen V: Purple
urine bag syndrome. Neth J Med. 67:340–341. 2009.PubMed/NCBI
|
|
32
|
Wu HH, Yang WC and Lin CC: Purple urine
bag syndrome. Am J Med Sci. 337:3682009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ferrara F, D'Angelo G and Costantino G:
Monolateral purple urine bag syndrome in bilateral nephrostomy.
Postgrad Med J. 86:6272010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hirzallah MI and D'Souza DL: Purple urine
bag syndrome in a patient with a nephrostomy tube. N Z Med J.
123:68–70. 2010.PubMed/NCBI
|
|
35
|
Siu G and Watanabe T: Purple urine bag
syndrome in rehabilitation. PM R. 2:303–306. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Su HK, Lee FN, Chen BA and Chen CC: Purple
urine bag syndrome. Emerg Med J. 27:7142010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kang KH, Jeong KH, Baik SK, Huh WY, Lee
TW, Ihm CG, Lee SH and Moon JY: Purple urine bag syndrome: Case
report and literature review. Clin Nephrol. 75:557–559. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Keenan CR and Thompson GR III: Purple
urine bag syndrome. J Gen Intern Med. 26:15062011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Khan F, Chaudhry MA, Qureshi N and Cowley
B: Purple urine bag syndrome: An alarming hue? A brief review of
the literature. Int J Nephrol. 2011:4192132011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Peters P, Merlo J, Beech N, Giles C, Boon
B, Parker B, Dancer C, Munckhof W and Teng HS: The purple urine bag
syndrome: A visually striking side effect of a highly alkaline
urinary tract infection. Can Urol Assoc J. 5:233–234. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zeier MG, Lee KG and Tan CS: An elderly
nursing home resident with unusual urine bag discoloration. NDT
Plus. 4:445–446. 2011.PubMed/NCBI
|
|
42
|
Bocrie OJ, Bouchoir E, Camus A, Popitean L
and Manckoundia P: Purple urine bag syndrome in an elderly subject.
Braz J Infect Dis. 16:597–598. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Cantaloube L, Lebaudy C, Hermabessière S
and Rolland Y: Pastel in the urine bag. Geriatr Psychol
Neuropsychiatr Vieil. 10:5–8. 2012.(In French). PubMed/NCBI
|
|
44
|
Domínguez Alegría AR, Vélez Díaz-Pallares
M, Moreno Cobo MA, Arrieta Blanco F and Bermejo Vicedo T: Purple
urine bag syndrome in elderly woman with nutritional supplements.
Nutr Hosp. 27:2130–2132. 2012.(In French). PubMed/NCBI
|
|
45
|
Meekins PE, Ramsay AC and Ramsay MP:
Purple urine bag syndrome. West J Emerg Med. 13:499–500. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Al Montasir A and Al Mustaque A: Purple
urine bag syndrome. J Family Med Prim Care. 2:104–105. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bhattarai M, Bin Mukhtar H, Davis TW,
Silodia A and Nepal H: Purple urine bag syndrome may not be benign:
A case report and brief review of the literature. Case Rep Infect
Dis. 2013:8638532013.PubMed/NCBI
|
|
48
|
Canavese C, Airoldi A, Quaglia M, Barbè
MC, Brustia M, Vidali M, Bagnati M, Andreone S, Corrà T, Sciarrabba
C, et al: Recognizing purple bag syndrome at first look. J Nephrol.
26:465–469. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Duff ML: Case report: Purple urine bag
syndrome. J Emerg Med. 44:e335–e336. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Iglesias Barreira R, Albiñana Pérez MS,
Rodríguez Penín I and Bilbao Salcedo J: Purple urine bag syndrome
in two institutionalised patients. Rev Esp Geriatr Gerontol.
48:45–47. 2013.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Mohamad Z and Chong VH: Purple urine bag:
Think of urinary tract infection. Am J Emerg Med. 31:265 e5–6.
2013. View Article : Google Scholar
|
|
52
|
Ungprasert P, Ratanapo S, Cheungpasitporn
W, Kue-A-Pai P and Bischof EF Jr: Purple urine bag syndrome. Clin
Kidney J. 6:3442013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Wolff N, Indaburu I, Muller F and Mariescu
Depaire N: Purple urine bag syndrom. Prog Urol. 23:538–539.
2013.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Yaqub S, Mohkum S and Mukhtar KN: Purple
urine bag syndrome: A case report and review of literature. Indian
J Nephrol. 23:140–142. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Agapakis D, Massa E, Hantzis I, Paschoni E
and Satsoglou E: Purple Urine Bag Syndrome: A case report of an
alarming phenomenon. Hippokratia. 18:92–94. 2014.PubMed/NCBI
|
|
56
|
Chassin-Trubert CAM: Purple urine bag
syndrome: Report of one case. Rev Med Chil. 142:1482–1484. 2014.(In
Spanish). PubMed/NCBI
|
|
57
|
Delgado G, Martínez-Reséndez M and
Camacho-Ortiz A: Purple urine bag syndrome in end-stage chronic
kidney disease. J Bras Nefrol. 36:542–544. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Hloch O, Gladišová D and Horáčková M:
Purple urine bag syndrome - rare but substantial symptom of urinary
infection. Vnitr Lek. 60:512–513. 2014.(In Czech). PubMed/NCBI
|
|
59
|
Restuccia MR and Blasi M: A PUBS Case in a
Palliative Care Unit Experience. Case Rep Oncol Med.
2014:1697822014.PubMed/NCBI
|
|
60
|
Sheehan M: Monolateral purple urine bag
syndrome in a patient with bilateral nephrostomy tubes. Urol Nurs.
34:135–138. 2014.PubMed/NCBI
|
|
61
|
Abubacker NR, Jayaraman SMRK, Sivanesan MK
and Mathew R: Purple Urine Bag Syndrome. J Clin Diagn Res.
9:OD01–OD02. 2015.PubMed/NCBI
|
|
62
|
Alex R, Manjunath K, Srinivasan R and Basu
G: Purple urine bag syndrome: Time for awareness. J Family Med Prim
Care. 4:130–131. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Karim A, Abed F and Bachuwa G: A
unilateral purple urine bag syndrome in a patient with bilateral
nephrostomy tubes. BMJ Case Rep. 2015.https://doi.org/10.1136/bcr-2015-212913
View Article : Google Scholar
|
|
64
|
Kenzaka T: Purple urine bag syndrome in a
patient with a urethral balloon catheter and a history of ileal
conduit urinary diversion. Korean J Intern Med. 30:4202015.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Mohamed Faisal AH, Shathiskumar G and
Nurul Izah A: Purple urine bag syndrome: Case report from a nursing
home resident with a false alarm of urosepsis. Med J Malaysia.
70:265–266. 2015.PubMed/NCBI
|
|
66
|
Mondragón-Cardona A, Jiménez-Canizales CE,
Alzate-Carvajal V, Bastidas-Rivera F and Sepúlveda-Arias JC: Purple
urine bag syndrome in an elderly patient from Colombia. J Infect
Dev Ctries. 9:792–795. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Neweling F and Janssens U: Lila Urin bei
einem Patienten mit beidseitiger Nephrostomie. Med Klin Intensivmed
Notf Med. 111:731–733. 2016.(In German). View Article : Google Scholar
|
|
68
|
Redwood R, Medlin J and Pulia M: Elderly
Man With Dark Urine. Purple urine bag syndrome. Ann Emerg Med.
66:436, 4402015. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Van Keer J, Detroyer D and Bammens B:
Purple Urine Bag Syndrome in Two Elderly Men with Urinary Tract
Infection. Case Rep Nephrol. 2015:7469812015.PubMed/NCBI
|
|
70
|
Demelo-Rodríguez P, Galán-Carrillo I and
Del Toro-Cervera J: Purple urine bag syndrome. Eur J Intern Med.
35:e3–e4. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Faridi MS, Rahman MJ, Mibang N, Shantajit
N and Somarendra K: Purple Urine Bag Syndrome- An Alarming
Situation. J Clin Diagn Res. 10:PD05–PD06. 2016.PubMed/NCBI
|
|
72
|
Richardson-May J: Single case of purple
urine bag syndrome in an elderly woman with stroke. BMJ Case Rep.
Aug 3–2016.https://doi.org/10.1136/bcr-2016-215465
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Sriramnaveen P, Reddy YS, Sridhar A,
Kishore CK, Manjusha Y and Sivakumar V: Purple urine bag syndrome
in chronic kidney disease. Indian J Nephrol. 26:67–68. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Tul Llah S, Khan S, Dave A, Morrison AJ,
Jain S and Hermanns D: A Case of Purple Urine Bag Syndrome in a
Spastic Partial Quadriplegic Male. Cureus. 8:e5522016.PubMed/NCBI
|
|
75
|
Mantani N, Ochiai H, Imanishi N, Kogure T,
Terasawa K and Tamura J: A case-control study of purple urine bag
syndrome in geriatric wards. J Infect Chemother. 9:53–57. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Vincitorio D, Barbadoro P, Pennacchietti
L, Pellegrini I, David S, Ponzio E and Prospero E: Risk factors for
catheter-associated urinary tract infection in Italian elderly. Am
J Infect Control. 42:898–901. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Eckenrode S, Bakullari A, Metersky ML,
Wang Y, Pandolfi MM, Galusha D, Jaser L and Eldridge N: The
association between age, sex, and hospital-acquired infection
rates: Results from the 2009–2011 National Medicare Patient Safety
Monitoring System. Infect Control Hosp Epidemiol. 35 Suppl 3:S3–S9.
2014. View
Article : Google Scholar : PubMed/NCBI
|
|
78
|
Jiménez-Alcaide E, Medina-Polo J,
García-González L, Arrébola-Pajares A, Guerrero-Ramos F,
Pérez-Cadavid S, Sopeña-Sutil R, Benítez-Sala R, Alonso-Isa M,
Lara-Isla A, et al: Healthcare-associated urinary tract infections
in patients with a urinary catheter: Risk factors, microbiological
characteristics and patterns of antibiotic resistance. Arch Esp
Urol. 68:541–550. 2015.(In Spanish). PubMed/NCBI
|
|
79
|
Yang CJ, Lu PL, Chen TC, Tasi YM, Lien CT,
Chong IW and Huang MS: Chronic kidney disease is a potential risk
factor for the development of purple urine bag syndrome. J Am
Geriatr Soc. 57:1937–1938. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Jackson SL, Boyko EJ, Scholes D, Abraham
L, Gupta K and Fihn SD: Predictors of urinary tract infection after
menopause: A prospective study. Am J Med. 117:903–911. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Nicolle LE: Urinary tract infections in
the elderly. Clin Geriatr Med. 25:423–436. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Chant C, Smith OM, Marshall JC and
Friedrich JO: Relationship of catheter-associated urinary tract
infection to mortality and length of stay in critically ill
patients: A systematic review and meta-analysis of observational
studies. Crit Care Med. 39:1167–1173. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Rivers E, Nguyen B, Havstad S, Ressler J,
Muzzin A, Knoblich B, Peterson E and Tomlanovich M; Early
Goal-Directed Therapy Collaborative Group, : Early goal-directed
therapy in the treatment of severe sepsis and septic shock. N Engl
J Med. 345:1368–1377. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Liu B, Ding X and Yang J: Effect of early
goal directed therapy in the treatment of severe sepsis and/or
septic shock. Curr Med Res Opin. 32:1773–1782. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Xing L, Tong L, Jun L, Xinjing G and Lei
X: Effect of early goal-directed therapy on mortality in patients
with severe sepsis or septic shock: A Meta analysis. Zhonghua Wei
Zhong Bing Ji Jiu Yi Xue. 27:735–738. 2015.(In Chinese). PubMed/NCBI
|
|
86
|
Cai G, Tong H, Hao X, Hu C, Yan M, Chen J
and Yan J: The effects of early goal-directed therapy on mortality
rate in patients with severe sepsis and septic shock: A systematic
literature review and Meta-analysis. Zhonghua Wei Zhong Bing Ji Jiu
Yi Xue. 27:439–442. 2015.(In Chinese). PubMed/NCBI
|
|
87
|
Puskarich MA, Marchick MR, Kline JA,
Steuerwald MT and Jones AE: One year mortality of patients treated
with an emergency department based early goal directed therapy
protocol for severe sepsis and septic shock: A before and after
study. Crit Care. 13:R1672009. View
Article : Google Scholar : PubMed/NCBI
|
|
88
|
Kalil AC and Kellum JA: Is Early
Goal-Directed Therapy Harmful to Patients With Sepsis and High
Disease Severity? Crit Care Med. 45:1265–1267. 2017. View Article : Google Scholar : PubMed/NCBI
|