Introduction
With the aging of the population and increase in
desk jobs, cervical disc degenerative diseases have become
increasingly common and affect the patients' quality of life
(1). These diseases occur as a
result of the degeneration of the cervical discs. When degenerative
changes occur, the moisture content of the cervical disc nucleus
markedly decreases, which results in the loss of viscosity and
flexibility (1). These alterations
then result in decreased clearance between the cervical vertebrae,
small joint disorder, cervical instability, cervical biomechanical
disturbance and abnormality of the cervical structure, all of which
can cause clinical symptoms and physical signs, including neck and
shoulder pain and arms paralysis (2).
Currently, the two most common methods of treating
cervical disc degenerative diseases caused by the pathology
described earlier include removal of the lesion and intervertebral
bone-graft fusion with internal fixation (3). The curative effects of these techniques
have been demonstrated; however, each technique presents certain
disadvantages (4). More
specifically, removal of the lesion results in decreased clearance
between cervical vertebrae and cervical instability. In addition,
spinal fusion with rigid devices, including steel plates, bolts and
fusion cages, accelerates the degeneration of adjacent cervical
vertebrae and facet joints (3,4). This
accelerated degeneration is a result of alterations in the normal
physiological shape and biomechanical structure of the cervical
spine (4).
Accordingly, the structure and biomechanics of
cervical discs and the disc nucleus have been extensively
investigated. Prosthetic disc nuclei and artificial cervical discs
have been developed in order to treat cervical diseases in recent
years (5). In 1966, Fernström
(6) described the implantation of a
stainless steel ball as a treatment for cervical disease. However,
this technique had certain disadvantages, such as the loss of
height between the discs when the implanted ball sank into the disc
over time. In the past 40 years, researchers have made rapid
progress in the fields of material science and biomechanics.
Artificial disc replacement and prosthetic disc nucleus replacement
are now effective procedures to treat cervical disc degenerative
diseases (7,8). These techniques can maintain the normal
physiologic function, preserve the height and increase the total
volume between the cervical discs, support compressive forces and
relieve the symptoms of spinal disease (9,10). The
numerous advantages of prosthetic disc nucleus replacement include
a minimally invasive surgery, low associated costs and safe
procedure (10).
There are two types of internal fixation, flexible
and rigid (11). Rigid fixation
solves the problem of spinal instability; however, it is associated
with problems such as osteoporosis of the adjacent vertebrae,
spinal canal stenosis, facet joint disorders and adjacent segment
degeneration (11). Biomechanical
analysis has demonstrated that these symptoms are caused by
excessive rigidity of the internal fixation (12). Thus, degradable internal fixation
systems have also been developed. However, these materials have
several issues, including the short duration of support, production
of fragments and lack of mechanical strength (12). Recently, flexible stabilization
devices have been designed by Strauss et al (11) and Leahy et al (12). Flexible stabilization devices
consisting of woven fabrics of elastic polyester have been used to
stabilize the zygapophysial joints via a pedicle screw-lamina hook
system. Consequently, a flexible stabilization device is preferable
to a rigid device since it provides improved mobility and quality
of life following surgery. However, flexible stabilization devices
require a two-step process, involving an initial implantation of
the prosthesis and subsequently placement of the stabilization
system. This two-step process increases the difficulty of the
procedure and lengthens the surgery duration (11,12).
Based on the aforementioned developments, an
anterior spinal instrumentation system combining a prosthetic disc
nucleus with a flexible stabilization device (ASI combining PDN/FD)
was developed in the present study and examined by in vivo
experiments. The main advantages of PDN/FD include the following
three features: i) The prosthetic disc nucleus has good
biomechanical properties and can replicate the physiological
function of the disc nucleus; ii) the wing-like weave functions as
an artificial ligament, which increases the stability of the
adjacent vertebrae; and iii) the wing-like weave helps maintain the
location of the prosthetic disc nucleus, preventing the nucleus
from breaking off to the spinal canal and aiding early
mobilization. There is currently no measurable standard to analyze
the results of PDN/FD surgery. Therefore, a novel evaluation method
was established in the current study, involving pressure
measurement combined with imaging analysis and histology. A
comparison of the adjacent intervertebral disc degeneration in dogs
treated with PDN/FD compared with those treated with a plate
fixation system demonstrated reduced degeneration in the PDN/FD
group. Thus, this is a promising technique for the treatment and
repair of degenerating cervical discs.
Materials and methods
Materials
Polyvinyl alcohol (PVA) type 1799, with a molecular
weight of 74,800–79,200 and an alcoholysis degree of 99.9%, was
purchased from Beijing Huaer Co., Ltd. (Beijing, China). Ketamine
and penicillin were obtained from the 309th Hospital of PLA
(Beijing, China). The experiments of the present study were
approved by the Ethics Committee of the 309th Hospital of PLA.
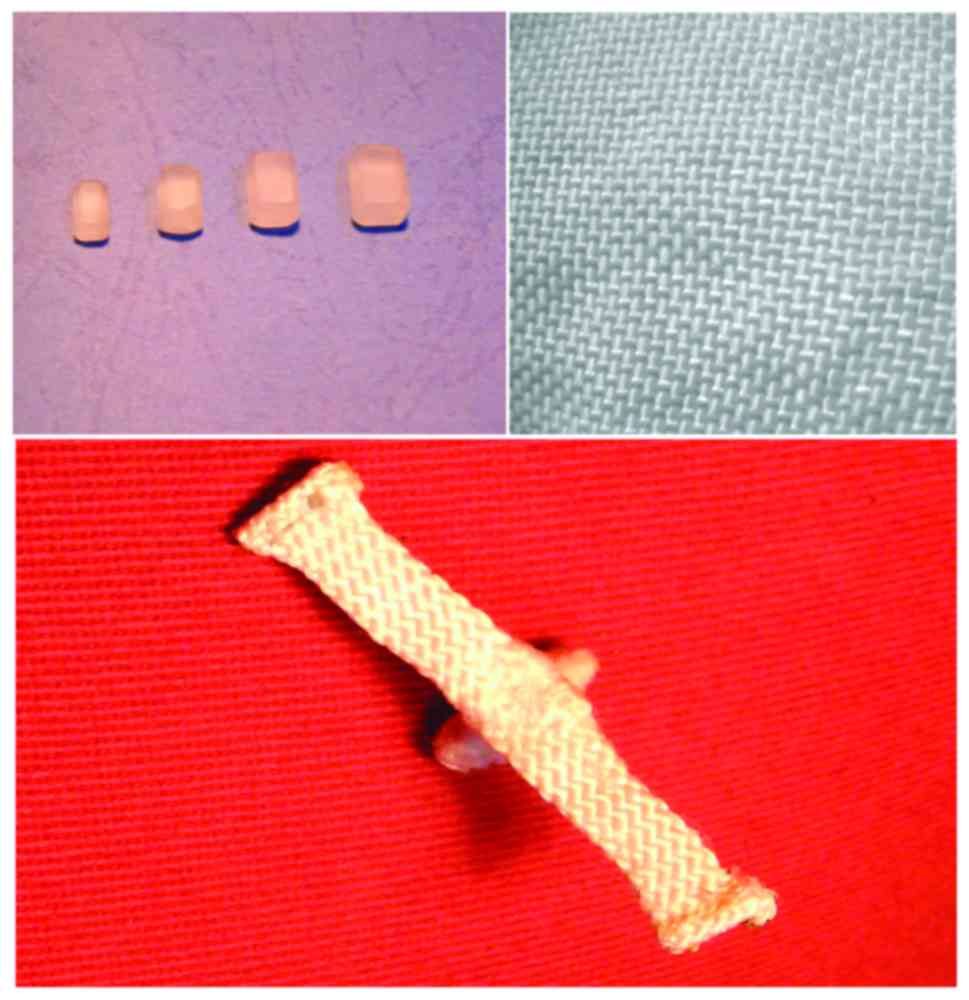
Implanted materials
The PDN/FD consisted of an artificial alar ligament,
a 2.5-mm connecting ligament and a prosthetic disc nucleus composed
of a core and surrounding material (Fig.
1). The alar ligament, connecting ligament and core-surrounding
material were composed of polyethylene with an ultra-high molecular
weight supplied by the College of Textiles, Tianjin Polytechnic
University (Tianjin, China), while the core was composed of PVA
hydrogel. In order to allow normal physiological activities, a 2-mm
extension was made for the alar ligament. The prosthetic disc
nucleus was surrounded with a radiopaque thread supplied by the
College of Textiles, Tianjin Polytechnic University (Tianjin,
China). Furthermore, a plate fixation system was used in the
control group, which consisted of a titanium plate with 2–4 holes
and 5–10 titanium alloy screws, and was supplied by Beijing
Sinotech Medical Supplies Co., Ltd. (Beijing, China).
Manufacture of PVA hydrogel
PVA was dissolved in water in a high-pressure
container at a temperature of 90°C for 6 h. The solution was then
cast into a mold and frozen at −20°C for 6–12 h. Next, the frozen
PVA hydrogel was melted by keeping it at room temperature for 1–2
h. This freeze-melt process was repeated three times, and the
frozen solution was subsequently vacuum dehydrated for 8 h.
Finally, the sample was placed in sterile water at 37°C for 2 days
to achieve saturation and to form a hydrogel.
Measurement of dehydration and
swelling of PVA hydrogel
The prepared PVA hydrogel was accurately weighed and
denoted by W0, while its volume was measured and denoted
by V0. Next, the PVA hydrogel was placed into an
electro-thermostat device at a temperature of 25°C, and its weight
(Wt) and volume (Vt) were measured at
different time points (denoted by t) until they were stable. The
dehydration ratio (Wr) and volume shrinkage percentage
(Q) of the PVA hydrogel were calculated according to equations 1
and 2, respectively.
Wr=WtW0x100%
Q=VtV0x100%
When a constant weight was achieved, the dehydrated
PVA hydrogel was weighed (Wd) and then placed in
deionized water. The swelling ratio (Swt) was calculated
according to equation 3.
Swt=Wt–WdWdx100%
Animal grouping
The healthy dogs were selected as the animal model
in the present study. In total, 18 healthy mixed-breed dogs (age,
1.5–2.5 years; 9 males and 9 females; body weight, 20.0–30.0 kg)
were maintained in a temperature controlled room (temperature,
20°C; humidity, 45%) with a 12-h light/dark cycle and free access
to water and food) at the Animal Experiment Center at the 309th
Hospital of PLA. The dogs were divided into two groups (n=9 in each
group), with dogs in Group A receiving PDN/FD and dogs in Group B
receiving a plate fixation system.
Surgical method
Dogs were anesthetized with an intravenous injection
of ketamine (10 mg/kg), and placed in a supine position. An 1-cm
incision was made on the left side of midline, and soft tissues
were cleared from the anterior aspect of the vertebral body. The
exposed centrum and annulus fibrosus were bluntly dissected
following sharp dissection of the prevertebral fascia. The pressure
transducer was not connected to the spinal needle until the centrum
was confirmed with X-rays obtained with a C-arm device. Next, a
multifunctional patient monitor (Dash 4000; GE Healthcare, Little
Chalfont, UK) was connected for invasive manometry measurement. The
system was filled with lactated Ringer's solution (College of
Textiles, Tianjin Polytechnic University). A lumbar spinal needle
was inserted vertically at C4/5 to record the pressure, with a
horizontal pressure setting of zero. Discectomy of C3/4 was
performed subsequent to cutting the annulus fibrosus. In Group A,
the PDN/FD was placed with a titanium screw fixing each end of the
alar ligament to the centrum, whereas a plate fixation system was
placed in Group B. Following the implant placement, the pressure at
C4/5 was recorded again with the method described earlier. The
difference between the preoperative and postoperative pressures was
calculated as the brace pressure. To study without the
interferences of brace intensity, the pressure in the dog's
intervertebral disc adjacent to operative segments was monitored
and the two groups were maintained to the same brace pressure at 2
mmHg. Subsequently, the incision was securely sutured after
flushing with streptomycin, and the dogs received 1.6 million units
of penicillin intramuscularly prior to waking from anesthesia and
once daily for the following 3 days. Wound healing, ambulatory
state, diet and complications were monitored.
Imaging
Lateral anteroposterior and flexion-extension
radiographs were obtained prior to surgery, in order to rule out
the possibility of preexisting degenerative disease, and at 6
months after surgery. Radiographs were analyzed to determine any
alterations in the intervertebral height, cervical physiological
curve and vertebral position. At the same time, magnetic resonance
imaging (MRI) was performed to evaluate the degenerative changes at
C2/3 because C2/3 was adjacent to C3/4 (operated segment) and C4/5
disc was only measured in the operation. This was performed
according to the Pearce standard (13).
Histopathology
Animals were euthanized and the disc at C2/3 was
collected 6 months after surgery. Disc specimens were observed
grossly for evidence of inflammation and degeneration of the
annulus fibrosus and end plate. Briefly, the C2/3 sample was
decalcified in 10% nitric acid and embedded in paraffin wax
following fixation in formaldehyde (20°C) solution for 72 h. Next,
4-mm sections were prepared and stained with hematoxylin and eosin.
The degeneration level of C2/3 was classified according to the
scale described by Lou et al (14), as follows: Level 1, numerous matrix
components, with thin and ordered collagenous fibers; level 2, few
matrix components, with thick and disordered collagenous fibers;
level 3, twisted, thick and disordered tufted collagenous fibers;
and level 4, collagenous fibers more disordered and gathered into a
mass as indicated in a previous study by Lou et al (14).
Statistical analysis
Data were analyzed using statistic software of SPSS
22.0 (IBM Corp., Armonk, NY, USA). The degree of degeneration of
the intervertebral disc adjacent to the operative segment (C2/3)
was evaluated according to the Pearce standard. Histological
differences were evaluated according to degeneration level. Pearce
levels and degeneration levels in group A and B were evaluated with
a Student's t-test.
Results
Dehydration and swelling properties of
the PVA hydrogel
Dehydration of the PVA hydrogel occurred mainly in
the initial 12 h, with the mass and volume decreasing by 33.7 and
50.7%, respectively. The final dehydration ratio was 28.8%, while
the volume shrinkage percentage was 26.3%. Furthermore, PVA
hydrogel swelling was mainly observed in the initial 24 h, with the
swelling ratio increasing by a maximum of 84.7%, and subsequently
trending toward stability. At 72 h, the hydrogel was completely
swollen, with the mass increasing to 112.7% of the PVA hydrogel
mass prior to dehydration.
Imaging and histopathology
results
Instability was defined as a difference in
angulation of >20° between the flexion and extension radiographs
at the intervertebral disc space. According to this definition,
there were four cases of C2/3 instability in Group B (44.4%), while
no cases of instability were observed in Group A, as demonstrated
in radiograph and MRI scan results (Figs. 2 and 3). At 6 months after surgery, the mean
Pearce level of C2/3 in Group A was 1.89, which was markedly higher
compared with the Pearce level of 3.22 in Group B (P<0.05).
Similarly, the degeneration degree of C2/3 in Group A was 1.67,
which as significantly lower compared with the level of 2.78 in
Group B (P<0.05; Tables I and
II).
 | Table I.C2/3 disc degeneration demonstrated
according to the Pearce level of the dogs. |
Table I.
C2/3 disc degeneration demonstrated
according to the Pearce level of the dogs.
| Pearce level | Group A, n | Group B, n | Subtotal, n |
|---|
| 1 | 3 | 0 | 3 |
| 2 | 4 | 1 | 5 |
| 3 | 2 | 5 | 7 |
| 4 | 0 | 3 | 3 |
| 5 | 0 | 0 | 0 |
| Mean | 1.89 | 3.22 | 2.56 |
| Total | 9 | 9 | 18 |
 | Table II.Histological differences were
evaluated according to the level of C2/3 disc degeneration in dogs
from the two groups. |
Table II.
Histological differences were
evaluated according to the level of C2/3 disc degeneration in dogs
from the two groups.
| Degeneration
level | Group A, n | Group B, n | Subtotal, n |
|---|
| 1 | 4 | 0 | 4 |
| 2 | 4 | 3 | 7 |
| 3 | 1 | 5 | 6 |
| 4 | 0 | 1 | 1 |
| Mean | 1.67 | 2.78 | 2.22 |
| Total | 9 | 9 | 18 |
Discussion
In the present study, the core of the prosthetic
disc nucleus was composed of PVA hydrogel, which possessed good
water absorbency, with a water content of 70–80% in the hydrated
state, close to the normal human physiological conditions. Swelling
PVA hydrogel was selected as the core of the prosthetic disc
nucleus in order to reduce trauma and risk. A previous study
(15) have indicated that prosthetic
disc nuclei should not exhibit excessive creep deformation and
should recover their height well once external forces are
withdrawn, within the range of human intervertebral disc
biomechanics. Furthermore, 10-million-cycle fatigue testing of PVA
hydrogel at 4 Hz frequency demonstrated that the height and elastic
modulus were not altered significantly (15).
The degeneration of adjacent intervertebral disc is
affected by various factors, including the brace pressure. In the
present study, the difference between preoperative and
postoperative pressures was calculated as the brace pressure.
Significant positive correlations were detected between the Pearce
level, degeneration level and brace pressure in each group.
Accordingly, it is suggested that pressure alterations affecting
the degeneration of adjacent cervical discs must not be ignored.
Excessively increased pressure in the disc adjacent to the operated
segment may result in the degeneration of that segment. Therefore,
attention should be paid not only to the reconstruction of cervical
lordosis and stability, but also to the accurate distraction forces
during surgery. Pressure monitoring of the adjacent disc during
surgery reduces the risk of future degeneration. In the current
study, there was no significant differences in the brace pressure
between Groups A and B. As a consequence, the effect of implanted
materials was evaluated directly without the confounding factor of
distraction force.
Anterior bone-graft fusion and internal fixation
have commonly been used to restore the disc height, lessen the
cervical facet joint loading and stabilize the fusion segments
(15). However, bone-graft fusion
disturbs the normal mechanical transmission of the cervical
vertebrae and increases the load on adjacent segments, resulting in
stress concentration and potentially accelerating the degeneration
of adjacent segments (16).
Treatment for joint disease has altered from fusion to artificial
joint replacement, with artificial disc replacement (including
whole disc replacement and prosthetic disc nucleus replacement)
being performed in place of spinal fusion (17). Prosthetic disc nucleus replacement
has certain advantages over the traditional procedure, including
reconstruction of the physiological function units, decrease of the
load on adjacent segments and reduction of the likelihood of
degeneration. The present study confirmed that the Pearce levels
and degeneration levels in Group A that was treated with PDN/FD
were significantly lower in comparison with those of Group B, in
which a plate fixation system was used. Evidently, PDN/FD prevented
the degeneration of adjacent segments more effectively as compared
with the plate fixation system. In addition, PDN/FD restored the
normal intervertebral height and the physiological annulus
fibrosus. At the same time, the synthetic alar ligament
strengthened the anterior longitudinal ligament, which reinforced
the endogenous factors promoting cervical stability, avoided stress
concentration in the bilateral facet joints and contributed to the
recovery of the physiological curvature.
As previously reported (18), lumbar intervertebral discs are in a
hydrostatic state due to their diffluent matrix composed of
proteoglycan protein and water. As a result, the internal pressure
of lumbar intervertebral discs can be measured. Furthermore, there
are no significant pressure differences among different lumbar
intervertebral discs (18). Due to
the hydrostatic property of cervical intervertebral discs,
intervertebral disc manometry was used in the present study to
quantify brace pressure to compare the impact of different brace
pressure on adjacent segments. However, small absolute values and
inconsistencies between intraoperative and postoperative
positioning led to measurement errors. Therefore, in the current
study, the pressure differences were measured to avoid systematic
errors and to minimize measurement errors in the absolute values.
However, this manometry technique can injure the normal cervical
intervertebral disc and accelerate its degeneration. To address
this problem, the adjacent segment below the operative segment,
which is relatively resistant to deterioration, was used in
measurements in the present study, while the easily deteriorated
segment above the operated segment was selected for observation.
Furthermore, one-step surgery was performed in order to reduce
duplication surgery, avoiding further injury. Nevertheless,
intervertebral disc manometry is in its initial stages of study.
Various issues remain to be clarified, including the influence of
pressure changes on the degeneration in adjacent segments.
In conclusion, the present study demonstrated that
disc degeneration may be decreased by using ASI combining PDN/FD
compared with plate systems. PDN/FD may offer a promising method
for the treatment of cervical disc degenerative diseases.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Axelsson P and Karlsson BS: Intervertebral
mobility in the progressive degenerative process: A
radiostereometric analysis. Eur Spine J. 13:567–572. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sohn HM, You JW and Lee JY: The
relationship between disc degeneration and morphologic changes in
the intervertebral foramen of the cervical spine: A cadaveric MRI
and CT study. J Korean Med Sci. 19:101–106. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Goffin J, Van Loon J, Van Calenbergh F and
Plets C: Long-term results after anterior cervical fusion and
osteosynthetic stabilization for fractures and/or dislocations of
the cervical spinal. J Spinal Disord. 8:500–508. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Katsuura A, Hukuda S, Saruhashi Y and Mori
K: Kyphotic malalignment after anterior cervical fusion is one of
the factors promoting the degenerative process in adjacent
interventebral levels. Eur Spine J. 10:320–324. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nandyala SV, Marquez-Lara A, Fineberg SJ
and Singh K: Comparison between cervical total disc replacement and
anterior cervical discectomy and fusion of 1 to 2 levels from 2002
to 2009. Spine (Phila Pa 1976). 39:53–57. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fernström U: Arthroplasty with
intercorporal endoprothesis in herniated disc and in painful disc.
Acta Chir Scand Suppl. 357:154–159. 1966.PubMed/NCBI
|
|
7
|
Coffin J, Van Calenbergh F, Van Loon J,
Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Sgrambiglia R and
Pointillart V: Intermedediate follow-up after treatment of
degenerative disc disease with the Bryan cervical prosthesis:
Single-level and bi-level. Spine (Phila Pa 1976). 28:2673–2678.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Goffin J, van Loon J, Van Calenbergh F and
Lipscomb B: A clinical analysis of 4- and 6-year follow-up results
after cervical disc replacement surgery using the bryan cervical
disc prosthesis. J Neurosurg Spine. 12:261–269. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kim SW, Limson MA, Kim SB, Arbatin JJ,
Chang KY, Park MS, Shin JH and Ju YS: Comparison of radiographic
changes after ACDF versus Bryan disc arthroplasty in single and
bi-level cases. Eur Spine J. 18:218–231. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Laxer EB, Darden BV, Murrey DB, Milam RA,
Rhyne AL, Claytor B, Nussman DS, Powers TW, Davies MA, Bryant SC,
et al: Ajacent segment disc pressure following two-level cervical
disc replacement versus simulated anterior cervical fusion. Stud
Health Technol Inform. 123:488–492. 2006.PubMed/NCBI
|
|
11
|
Strauss PJ, Novotny JE, Wilder DG, Grobler
LJ and Pope MH: Multidirectional stability of the Graf system.
Spine (Phila Pa 1976). 19:965–972. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Leahy JC, Mathias KJ, Heaton A, Shepherd
DE, Hukins DW, Deans WF, Brian MW and Wardlaw D: Design of spinous
process hooks for flexible fixation of the lumbar spine. Proc Inst
Mech Eng H. 214:pp. 479–487. 2000; View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pfirrmann CW, Metzdorf A, Zanetti M,
Hodler J and Boos N: Magnetic resonance classification of lumbar
intervertebral disc degeneration. Spine (Phila Pa 1976).
26:1873–1878. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lou C, Chen Q and Li F: Correlation
between MR imaging and pathological features of mucleus pulposus
degeneration in the lumbar disc. Chin J Orthop. 23:531–535.
2003.
|
|
15
|
Ji B, Gao J, Ma Y, et al: Manufacture of
prosthetic nucleus and analysis of stress-relaxation properties. J
Univ Sci Tech Beijing. 27:589–592. 2005.(In Chinese).
|
|
16
|
Hilibrand AS, Carlson GD, Palumbo MA,
Jones PK and Bohlman HH: Radiculopathy and myelopathy at segments
adjacent to the site of a previous anterior cervical arthrodesis. J
Bone Joint Surg Am. 81:519–528. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park DK, Lin EL and Phillips FM: Index and
adjacent level kinematics after cervical disc replacement and
anterior fusion: In vivo quantitative radiographic analysis. Spine
(Phila Pa 1976). 36:721–730. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang P, Dong Q and Xue Y: Pressure
measurement and pathological study of the lumbar disc herniation.
Chin J Orthop. 22:129–133. 2002.
|