Introduction
Hepatocellular carcinoma (HCC) is a highly prevalent
cancer worldwide, and is frequently caused by infection with
hepatitis B or C. Early-stage HCC can be cured by surgery or local
ablation, and inhibition of recurrence has been achieved using
antiviral agents. However, prevention of HCC recurrence after
radical treatment remains insufficient. Many HCC cases are in an
advanced stage or unresectable at the time of diagnosis. Moreover,
although unresectable advanced HCC can be treated with hepatic
arterial infusion chemotherapy (HAIC) and systemic chemotherapy,
the therapeutic effects are limited (1–3) and
the prognosis of advanced cases of HCC is poor.
Large-scale randomized placebo-controlled trials
have shown that sorafenib, a multi-kinase inhibitor, prolongs
overall and disease progression-free survival in patients with HCC
(4,5). Based on these findings, sorafenib is
recommended for treatment of advanced stage HCC (Child-Pugh A-B,
grade 1–2 performance status cases with portal tumor thrombus,
lymph node metastasis or distant metastasis) in the Barcelona
Clinic Liver Cancer (BCLC) staging system-based therapeutic
strategy for HCC (6). In Japan,
the use of sorafenib for unresectable hepatocellular carcinoma was
approved in May 2009, and the indication for sorafenib may be
expanded in the future. However, to date, the effect of sorafenib
has only been compared with untreated groups, and further evidence
is required to position sorafenib in the treatment algorithm for
HCC, for which various treatment methods are available (7,8).
The response rate of advanced HCC to HAIC is
approximately 30–40% (9–16), and HAIC (as well as sorafenib) is
recommended for treatment of advanced HCC, particularly in Japan
(17,18). However, comparison of the effects
of sorafenib with other treatment methods for HCC has not been
carried out. Therefore, in the present study, we retrospectively
compared the efficacy of sorafenib for unresectable advanced HCC
with that of HAIC.
Patients and methods
Patients
A total of 107 Child-Pugh class A patients with
advanced HCC were treated at Kagoshima Kouseiren Hospital between
July 1, 2004 and May 31, 2010; 72 patients were treated with HAIC
and 35 with sorafenib. Diagnosis of HCC was established based on
typical radiographic evidence and tumor markers such as
α-fetoprotein (AFP) and des-γ-carboxy prothrombin [DCP, also known
as protein induced by vitamin K absence or antagonist
(PIVKA-II)].
Of the 107 patients, 65 were selected for further
analysis based on the criteria below. These patients included 45
treated with HAIC and 20 treated with sorafenib. All 65 patients
had advanced HCC unsuitable for surgical resection, liver
transplantation, or nonsurgical interventions [such as
radiofrequency ablation or transcatheter arterial chemoembolization
(TACE)] because of multiple tumors involving both lobes of the
liver or portal invasion in the first or main portal branch
(19). Other eligibility criteria
included Eastern Cooperative Oncology Group (ECOG) performance
status 0 or 1 for sorafenib or 0 to 2 for HAIC, no other serious
medical condition, no history of systematic chemotherapy with
sorafenib, no concurrent malignancy of another type, and previously
described laboratory findings for sorafenib (20). In addition, we excluded patients
who had more than two distant metastases or a distant metastasis of
size >1 cm.
The average total and daily alcohol consumption was
calculated assuming that 633 ml of beer or 120 ml of shochu (a
traditional Japanese distilled spirit) contains 25 g of ethanol,
which is the typical ethanol content of Japanese beer and shochu.
Excess alcohol intake was defined as >75 g of ethanol per day,
using data obtained by questionnaire. Body mass index (BMI) was
calculated by dividing body weight (kg) by the square of the height
(m2). Informed consent was obtained from all patients
before treatment. This study was performed retrospectively and was
approved by the Ethics Committee of the Kagoshima Prefectural
Federation of Agricultural Cooperatives for Health and Welfare.
Treatment and dose modification
Sorafenib for unresectable HCC was approved in Japan
in May 2009. Before this date, all patients underwent HAIC, while
after May 2009 patients were treated with sorafenib or HAIC. HAIC
was administered in three regimens. Regimen A consisted of daily
cisplatin (5 mg/m2) followed by 5-fluorouracil (5-FU,
250 mg/body) on days 1–5, 8–12 and 15–19, with days 6, 7, 13, 14,
20 and 21 as rest days. Cisplatin and 5-FU were administered by a
mechanical infusion pump through implanted reservoir over 1 and 23
h, respectively (21). Regimen B
consisted of cisplatin (50 mg/body), mitomycin C (MMC, 10 mg/body)
and epirubicin (EPI, 30 mg/body) as a bolus injection on day 1, and
daily cisplatin (5 mg/m2) followed by 5-FU (250 mg/body)
on days 8–12 and 15–19. Cisplatin and 5-FU after day 8 were
administered by a mechanical infusion pump through implanted
reservoir over 1 and 23 h, respectively. Regimen C consisted of
cisplatin (50 mg/body), MMC (10 mg/body) and EPI (30 mg/body) as a
bolus injection through a catheter on day 1. All anticancer agents
were administered through the common or proper hepatic artery.
Regimens A, B and C were administered to 25, 12 and 8 patients,
respectively, and the cycles were repeated when possible. Sorafenib
was administered orally at 400 mg twice a day. Selection of the
treatment was made by each physician, patient or family members
after informed consent was obtained.
Evaluation
The therapeutic effect was assessed using the
Response Evaluation Criteria in Solid Tumors (RECIST) (22). HAIC was evaluated for every course
(every 4 or 6 weeks), and sorafenib treatment was evaluated every
month using computed tomography (CT) and tumor markers such as AFP
and DCP. Side effects were evaluated following the Common
Terminology Criteria for Adverse Events (CTCAE) v3.0 (JCOG/JSCO
edition) (23). The
discontinuation criteria were as follows: difficulty with
continuation of treatment due to disease progression or an adverse
effect of grade 3 or higher, a Child-Pugh score ≥10 points or
uncontrollable hepatic encephalopathy, intractable ascites, total
bilirubin ≥4.0 mg/dl, or a performance status of grade 3 or 4 or
worsening of the grade by ≥2 categories. Additional therapies were
administered on the basis of performance status, hepatic reserve
capacity, tumor responses to HAIC or sorafenib, and
complications.
The primary endpoint was overall survival (OS), and
the secondary efficacy endpoints were overall response rate [ORR =
complete response (CR) + partial response (PR)] and disease control
rate [DCR = CR + PR + stable disease (SD)]. OS was calculated from
the time of the first treatment with HAIC or sorafenib until death
or the last follow-up visit.
Statistical analysis
For comparison between two independent groups, the
Mann-Whitney U test and Fisher’s exact test were used as
appropriate. For the cumulative survival and discontinuation rates,
a log-rank test was performed using the Kaplan-Meier method. For
multivariate analysis, logistic regression analysis and a Cox
proportional hazards model were used. Cluster analysis was used to
divide the sorafenib group into a limited number of maximally
differing clusters based on the duration of sorafenib
administration. This analysis was performed using the hierarchical
agglomerative clustering method (24). A P-value <0.05 was considered to
indicate a significant difference. The analyses were performed
using XLSTAT version 2009 (Addinsoft Corp., new York, NY).
Results
Comparison of background factors, tumor
factors and survival rate between the HAIC and sorafenib
groups
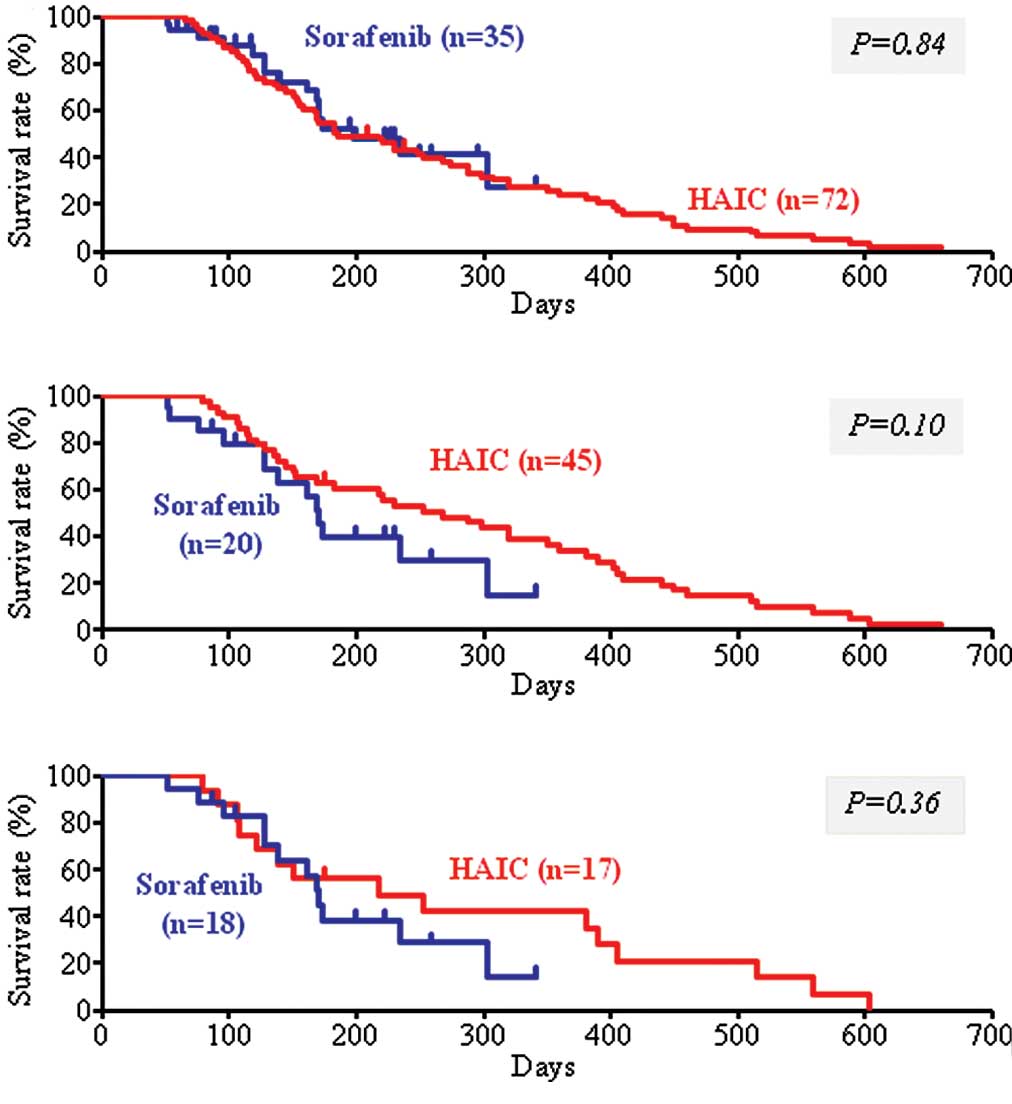
Of the 107 patients with advanced HCC treated at our
hospital between July 1, 2004 and May 31, 2010, the survival rate
did not differ between the 72 patients treated with HAIC and the 35
patients treated with sorafenib (Fig.
1A). Among these patients, 45 in the HAIC group and 20 in the
sorafenib group were included in further analysis. A comparison of
patient background factors between the HAIC and sorafenib groups
showed significant differences in prothrombin time (PT) and
pre-treatment, but not in age, gender, history of excess alcohol
intake, serum albumin, tumor markers, size of the main tumor, and
presence or absence of portal vein tumor thrombosis in the first
branch or trunk (Vp3 or Vp4, respectively) (Table I). The mean follow-up period was
317 days (55–1438 days) in the HAIC group and 166 days (51–341
days) in the sorafenib group. There was no significant difference
in survival rate between the two groups (Fig. 1B), or between subgroups of patients
who received pre-treatment in the HAIC and sorafenib groups
(Fig. 1C).
 | Table I.Clinical characteristics and
tumor-related background factors of the advanced hepatocellular
carcinoma patients treated with HAIC and sorafeniba. |
Table I.
Clinical characteristics and
tumor-related background factors of the advanced hepatocellular
carcinoma patients treated with HAIC and sorafeniba.
| Factor | HAIC (n=45) | Sorafenib (n=20) | P-valueb |
|---|
| Age (range), in
years | 69.6 (47–84) | 69.6 (44–83) | 0.88 |
| Gender
(male/female) | 0.71/0.29 | 0.85/0.15 | 0.35 |
| Virus marker
(HBV/HCV/NBNC) | 0.24/0.40/0.36 | 0.25/0.50/0.25 | 0.74 |
| Excess alcohol
intakec (+/−) | 0.31/0.69 | 0.35/0.65 | 0.77 |
| Diabetes mellitus
(+/−) | 0.27/0.73 | 0.30/0.70 | 0.77 |
| Body weight (kg) | 54.6 (37.8–72.5) | 55.9
(38.4–68.9) | 0.87 |
| Body mass index
(kg/m2) | 20.6
(15.8–27.1) | 21.9
(16.0–28.4) | 0.69 |
| Total bilirubin
(mg/dl) | 1.2 (0.3–2.7) | 1.1 (0.5–1.9) | 0.80 |
| AST (IU/l) | 74.7 (22–206) | 80.6 (25–201) | 0.39 |
| ALT (IU/l) | 53.2 (13–198) | 53.1 (17–178) | 0.74 |
| Serum albumin
(g/dl) | 3.6 (2.4–4.5) | 3.6 (2.8–4.4) | 0.73 |
| White blood cell
(×103/μl) | 3.8 (2.1–5.7) | 4.2 (2.5–6.8) | 0.88 |
| Neutrophils
(×103/μl) | 2.3 (1.1–4.1) | 2.6 (1.3–5.0) | 0.82 |
| Platelet count
(×104/μl) | 16.3
(5.3–47.7) | 14.0
(6.1–26.2) | 0.48 |
| Prothrombin time
(%) | 81.1 (56–100) | 87.4 (58–115) | <0.05 |
| α-fetoprotein
(×103 ng/ml) | 8.8 (0–55.9) | 7.3 (0–97.3) | 0.16 |
| DCP
(×103 mAU/ml) | 11.5 (0–176.0) | 11.4 (0–86.8) | 0.92 |
| Tumor diameter (≥50
mm/<50 mm) | 0.49/0.51 | 0.40/0.60 | 0.60 |
| Tumor thrombus (Vp3
or 4; +/−) | 0.64/0.36 | 0.50/0.50 | 0.29 |
| Distant metastasis
(+/−) | 0.13/0.87 | 0.25/0.75 | 0.29 |
| Previous treatment
(+/−) | 0.38/0.62 | 0.90/0.10 | <0.001 |
| Locoregional
therapyd | 0.9 (0–2) | 1.8 (0–6) | 0.23 |
| TACEe | 2.0 (0–4) | 4.3 (0–8) | <0.001 |
Comparison of the therapeutic effects and
treatment discontinuation between the HAIC and sorafenib
groups
Assessment of the therapeutic effect using RECIST
criteria (22) indicated that CR,
PR and SD were achieved in 2 (4.4%), 8 (17.8%) and 21 (46.7%)
cases, respectively, in the HAIC group, and in 0 (0%), 0 (0%) and
13 (65.0%) cases, respectively, in the sorafenib group (Table II). Thus, the overall response rate
(ORR) in the sorafenib group was significantly lower than that in
the HAIC group (0 vs. 22.2%, P=0.03). However, there was no
significant difference in the DCR between the 2 groups (65.0 vs.
68.8%, P=0.78).
 | Table II.Comparison of the therapeutic effects
and discontinuation of treatment between the HAIC- and
sorafenib-treated groupsa. |
Table II.
Comparison of the therapeutic effects
and discontinuation of treatment between the HAIC- and
sorafenib-treated groupsa.
| Decision case
(%) | HAIC (n=45) | Sorafenib
(n=20) | P-valueb |
|---|
| Effect: overall
response | | | |
| Complete response
(CR) | 2 (4.4) | 0 (0.0) | 0.150 |
| Partial response
(PR) | 8 (17.8) | 0 (0.0) | |
| Stable disease
(SD) | 21 (46.7) | 13 (65.0) | |
| Progressive
disease (PD) | 14 (31.1) | 7 (35.0) | |
| ORR (CR+PR) | 10 (22.2) | 0 (0.0) | 0.030 |
| DCR
(CR+PR+SD) | 31 (68.8) | 13 (65.0) | 0.780 |
|
Discontinuation/continuation | 41 (91.1)/4
(8.9) | 19 (95.0)/1
(5.0) | 1.000 |
| Reason of
discontinuation | | | |
| Disease
progression | 41 (91.1) | 7 (35.0) | <0.001 |
| Side effects | 0 (0.0) | 12 (60.0) | |
| Liver
dysfunction | 0 | 3 | |
| Skin
disorder | 0 | 4 | |
| Diarrhea | 0 | 4 | |
| Hepatic
encephalopathy | 0 | 1 | |
The treatment course, including the discontinuation
rate and reasons for discontinuation, were compared between the
HAIC and sorafenib groups (Table
II). Treatment was discontinued in 41 (91.1%) cases in the HAIC
group and in 19 (95%) cases in the sorafenib group, with no
significant difference between the groups. However, the reason for
discontinuation was disease progression including depressed hepatic
reserve function due to HCC progression in all cases in the HAIC
group, while the reason for discontinuation was adverse effects of
grade 3 or higher in 12 (60.0%) cases in the sorafenib group,
showing a significantly higher occurrence of adverse effects in the
sorafenib group (P<0.001).
Comparison of sorafenib administration
for less than and greater than 60 days
Since administration was discontinued due to side
effects in more than half of the patients in the sorafenib group,
the cumulative discontinuation rate and duration of administration
were investigated using the Kaplan-Meier method. Treatment was
discontinued in the early phase (within 60 days) in 11/20 (55%) of
the patients. In addition, hierarchical agglomerative clustering
identified two sorafenib subgroups, and on this basis the patients
(n=20) were divided into those for whom administration was
discontinued within a period of <60 days (n=11, sorafenib-I
subgroup) and those who received sorafenib for ≥60 days (n=9,
sorafenib-II subgroup; administration was discontinued after >60
days or continued). The mean durations (range) of sorafenib
administration and follow-up were 31 (14–45) and 123 (51–259) days,
respectively, in the sorafenib-I subgroup, and 106 (67–161) and 218
(104–341) days, respectively, in the sorafenib-II subgroup. There
were no significant differences in background and tumor factors
between the two subgroups (Table
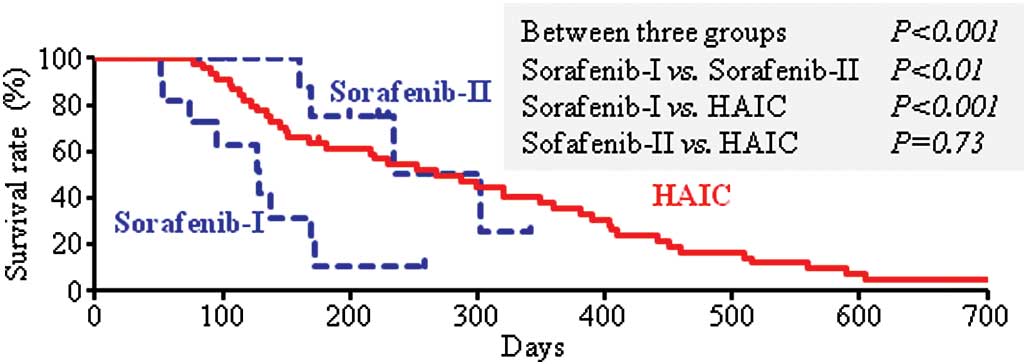
III). However, the survival rate differed significantly among
the two sorafenib subgroups and the HAIC group (multi-group
log-rank test, P<0.001) (Fig.
2). A between-group comparison showed that survival was
significantly shorter in the sorafenib-I subgroup compared to the
sorafenib-II subgroup and the HAIC group. There was no significant
difference in survival time between the sorafenib-II subgroup and
the HAIC group.
 | Table III.Clinical characteristics of the
advanced hepatocellular carcinoma patients treated with
sorafeniba:
Comparative evaluation of the sorafenib-I (administration <60
days) and sorafenib-II (administration ≥60 days) groups. |
Table III.
Clinical characteristics of the
advanced hepatocellular carcinoma patients treated with
sorafeniba:
Comparative evaluation of the sorafenib-I (administration <60
days) and sorafenib-II (administration ≥60 days) groups.
| Factor | Sorafenib-I
(n=11) | Sorafenib-II
(n=9) | P-valueb |
|---|
| Age (range), in
years | 69.9 (44–83) | 69.2 (58–78) | 0.57 |
| Gender
(male/female) | 0.82/0.18 | 0.89/0.11 | 1.00 |
| Virus marker
(HBV/HCV/NBNC) | 0.37/0.45/0.18 | 0.11/0.56/0.33 | 0.60 |
| Excess alcohol
intakec (+/−) | 0.27/0.73 | 0.44/0.56 | 0.64 |
| Diabetes mellitus
(+/−) | 0.18/0.82 | 0.44/0.56 | 0.34 |
| Body weight
(kg) | 53.6
(38.4–68.4) | 58.9
(48.0–68.9) | 0.25 |
| Body mass index
(kg/m2) | 21.6
(16.0–28.4) | 22.2
(18.4–24.8) | 0.82 |
| Initial dose of
sorafenib (mg/kg/day) | 15.5
(6.9–17.4) | 13.6
(5.8–15.4) | 0.24 |
| Total bilirubin
(mg/dl) | 1.2 (0.5–1.8) | 1.0 (0.6–1.9) | 0.21 |
| AST (IU/l) | 93.5 (25–201) | 64.9 (27–116) | 0.32 |
| ALT (IU/l) | 56.4 (17–178) | 51.2 (26–73) | 0.47 |
| Serum albumin
(g/dl) | 3.5 (2.8–4.4) | 3.7 (3.0–4.2) | 0.12 |
| White blood cell
(×103/μl) | 4.2 (2.5–6.8) | 4.2 (2.6–6.2) | 0.88 |
| Neutrophils
(×103/μl) | 2.6 (1.4–5.0) | 2.5 (1.3–4.6) | 0.88 |
| Platelet count
(×104/μl) | 15.4
(7.0–26.2) | 12.4
(6.1–19.1) | 0.15 |
| Prothrombin time
(%) | 85.1 (72–98) | 90.2 (58–115) | 0.29 |
| α-fetoprotein
(×103 ng/ml) | 0.9 (0–5.2) | 12.4 (0–97.3) | 0.62 |
| DCP
(×103 mAU/ml) | 17.8 (0–86.8) | 4.2 (0–27.9) | 0.40 |
| Tumor diameter (≥50
mm/<50 mm) | 0.36/0.64 | 0.44/0.56 | 1.00 |
| Tumor thrombus (Vp3
or 4; +/−) | 0.64/0.36 | 0.33/0.67 | 0.37 |
| Distant metastasis
(+/−) | 0.27/0.73 | 0.22/0.78 | 1.00 |
| Previous treatment
(+/−) | 0.91/0.09 | 0.89/0.11 | 1.00 |
| Locoregional
therapyd | 1.9 (0–6) | 1.6 (0–4) | 0.72 |
| TACEe | 3.9 (0–7) | 4.6 (0–8) | 0.40 |
The treatment discontinuation rate was 100% (11
cases) in the sorafenib-I subgroup and 89% (8 cases) in the
sorafenib-II subgroup, with no significant difference between the
subgroups. The reason for discontinuation was disease progression
in 4 cases and side effects in 7 in the sorafenib-I subgroup, and
disease progression in 3 cases and side effects in 5 in the
sorafenib-II subgroup, with no significant difference between the
subgroups (Table IV). However, the
reasons for discontinuation of sorafenib differed from those for
discontinuation of HAIC (Table
II). After discontinuation of sorafenib, HAIC was performed in
2 (18.2%) cases in the sorafenib-I subgroup, and in 6 (66.7%) cases
in the sorafenib-II subgroup (P=0.02). Of the 12 cases in which
sorafenib was discontinued due to side effects, additional HAIC was
performed in 1 of 7 cases in the sorafenib-I subgroup, but in all 5
cases in the sorafenib-II subgroup (14.3 vs. 100%, P=0.02).
 | Table IV.Comparison of treatment
discontinuation and post-treatment in the sorafenib-I and
sorafenib-II groups. |
Table IV.
Comparison of treatment
discontinuation and post-treatment in the sorafenib-I and
sorafenib-II groups.
| Decision case | Sorafenib-I
(n=11) | Sorafenib-II
(n=9) | P-valuea |
|---|
|
Discontinuation/continuation | 11/0 | 8/1 | 0.45 |
| Reason of
discontinuation | | | |
| Disease
progression | 4 | 3 | 1.00 |
| Side effects | 7 | 5 | |
| Liver
dysfunction | 2 | 1 | |
| Skin
disorder | 2 | 2 | |
| Diarrhea | 2 | 2 | |
| Hepatic
encephalopathy | 1 | 0 | |
| Post-treatment with
HAIC | | | |
| Yes | 2 (1)b | 6 (5)b | 0.02 |
| No | 9 (6)b | 2 (0)b | (0.02)b |
Of the factors shown in Table III, body weight, dose of
sorafenib/body weight, total bilirubin, serum albumin, platelet
counts and prothrombin time (%) differed between the sorafenib-I
and -II subgroups at a level of P<0.3. These factors were
subjected to multivariate logistic regression analysis, but none
was found to be an independent predictor of classification into
either of the two subgroups.
Prognostic factors in advanced
hepatocellular carcinoma
Prognostic factors were investigated in the 65
patients with advanced HCC. Univariate analysis (log-rank test) of
the 18 factors shown in Table V
revealed that the survival rate differed significantly between the
different treatment methods and between high and low DCP levels.
Multivariate analysis using a Cox proportional hazards model was
performed using 7 factors with P<0.3 in the univariate analysis
[age, gender, alanine aminotransferase (ALT), DCP, tumor thrombus,
tumor size, and treatment method]. From this analysis, a DCP level
≥1000 and discontinuation of sorafenib within 60 days (sorafenib-I
subgroup) were independent risk factors contributing to a poor
prognosis, and the hazard ratio in the sorafenib-I subgroup was
3.34 compared to HAIC (Table V).
To eliminate the possible bias of the 4 cases in which treatment
was discontinued due to marked disease progression in the
sorafenib-I subgroup, survival rate and prognostic factors were
analyzed for the 7 cases in which treatment was discontinued due to
side effects and in which the disease condition was not markedly
changed. These 7 patients were compared with the sorafenib-II
subgroup and the HAIC group. In this analysis, administration of
sorafenib for <60 days remained a poor prognostic factor by
log-rank test (P=0.01 vs. sorafenib-II; P<0.01 vs. HAIC).
 | Table V.Evaluation of the prognostic factors
in the advanced hepatocellular carcinoma cases. |
Table V.
Evaluation of the prognostic factors
in the advanced hepatocellular carcinoma cases.
| Factor
(categories) | Univariatea
|
Multivariateb
|
|---|
| n=65 | P-value | HR | (95% CI) | P-value |
|---|
| Age (≥70/<70),
in years | 35/30 | 0.07 | 0.65 | (0.35–1.19) | 0.16 |
| Gender
(male/female) | 49/16 | 0.10 | 1.37 | (0.65–2.87) | 0.41 |
| Virus marker (HBV
or HCV/NBNC) | 44/21 | 0.77 | | | |
| Excess alcohol
intakec (+/−) | 21/44 | 0.36 | | | |
| Diabetes mellitus
(+/−) | 18/47 | 0.43 | | | |
| TB (mg/dl)
(≥1.2/<1.2) | 31/34 | 0.35 | | | |
| AST (IU/l)
(≥50/<50) | 41/24 | 0.56 | | | |
| ALT (IU/l)
(≥40/<40) | 37/28 | 0.23 | 1.03 | (0.57–1.87) | 0.92 |
| ALB (g/dl)
(≥3.5/<3.5) | 43/22 | 0.99 | | | |
| PLT
(×104 μl) (≥15/<15) | 31/34 | 0.70 | | | |
| PT (%)
(≥80/<80) | 43/22 | 0.79 | | | |
| AFP (ng/ml)
(≥1000/<1000) | 32/33 | 0.98 | | | |
| DCP (mAU/ml)
(≥1000/<1000) | 36/29 | 0.02 | 1.87 | (1.03–3.38) | 0.04 |
| Tumor thrombus (Vp3
or 4) (+/−) | 39/26 | 0.19 | 1.25 | (0.67–2.31) | 0.48 |
| Tumor diameter (mm)
(≥50/<50) | 29/36 | 0.10 | 1.37 | (0.74–2.51) | 0.31 |
| Distant metastasis
(+/−) | 11/54 | 0.36 | | | |
| Previous treatment
(+/−) | 36/29 | 0.37 | | | |
| Treatment | | | | | |
| HAIC | 45 | <0.001 | 1 | | |
|
Sorafenib-Id | 11 | | 3.34 | (1.45–7.66) | <0.01 |
|
Sorafenib-IId | 9 | | 0.79 | (0.27–2.34) | 0.67 |
Discussion
Prolongation of survival by sorafenib compared to a
placebo and the efficacy of HAIC for advanced HCC have been
reported (1,2,4,5,10–12).
However, comparison of the efficacy between sorafenib and HAIC has
not been investigated. In this retrospective study, we demonstrated
that the disease control rate (DCR=CR+PR+SD) and OS rate in
patients with advanced unresectable HCC did not differ
significantly between sorafenib treatment and HAIC, although the
overall response rate (ORR=CR+PR) with sorafenib treatment was
lower than that for HAIC.
The prognosis was also found to be very poor when
sorafenib treatment was discontinued within 60 days due to serious
side effects. Although it is possible that the Kaplan-Meier curves
for subgroups established based on events during the follow-up
period (i.e., treatment cessation) included serious bias, side
effects led to the discontinuation of treatment in more than half
of the the cases in the sorafenib group, and many of these cases
received additional treatment that may have prolonged survival.
Thus, the present study suggests that early discontinuation of
sorafenib was the most important factor influencing survival of
patients with advanced HCC of Child-Pugh A, even if the reason for
discontinuation was not disease progression.
A prospective cohort study on the combination
therapy of HAIC and sorafenib for advanced HCC is currently
underway (25), but the
therapeutic effects of regimens including combination therapy and
monotherapy of HAIC or sorafenib remain unclear. In the present
study, the survival rate was comparable between HAIC and sorafenib
(Fig. 1), and there was no
significant difference in the DCRs (Table II). However, the overall response
rate for sorafenib was 0%, which was significantly lower than that
for HAIC. In the SHARP study (4),
the response rate of sorafenib was 2% and the DCR was 43%,
suggesting that the therapeutic effect depended on control of
disease progression, but not on tumor size reduction. Similar
findings were observed in a phase II study of sorafenib conducted
in the US and Europe (26), and in
a phase I study conducted in Japan (20). Our study suggests that a similar
survival rate may be achieved by different treatment methods
independently of the response rate when the DCR is similar.
Therefore, it is important to consider not only the response rate
but also the DCR, including SD cases, in the treatment of advanced
HCC.
Discontinuation of HAIC occurred in 41 cases and was
due to disease progression in all cases, whereas discontinuation of
sorafenib occurred due to side effects in 12 cases (60.0% of the
patients treated with sorafenib) (Table II). Typical side effects of
sorafenib include skin disorder (including hand-foot skin
reactions), hypertension, liver dysfunction, hepatic
encephalopathy, diarrhea, interstitial lung disease and hemorrhage;
and the incidence of hand-foot skin reactions and diarrhea are high
(25,27). In our study, discontinuation of
treatment was sometimes avoided by prevention and countermeasures,
but discontinuation due to liver dysfunction, diarrhea and erythema
multiforme was required in many cases. The incidence of adverse
events of grade 3 or higher caused by sorafenib was 13% in the
SHARP study and 9% in the Asia-Pacific study (4,5), and
tolerability was favorable in these studies. However, complications
of liver failure and hepatic encephalopathy have been reported, and
a causal relationship with development of liver failure within 3
weeks of sorafenib administration and death has been suggested.
In our study, improvement of symptoms after
discontinuation was slow in patients who developed severe side
effects in the early phase (administration <60 days), and
malaise, anorexia and fever developed. Many patients died without
switching to other treatments due to concomitant malnutrition and
disease progression. In contrast, patients who developed no or mild
side effects in the early phase were able to tolerate long-term
administration (≥60 days); even in cases in which drug
administration was finally discontinued due to side effects,
patients recovered from the side effects and a switch to another
therapy was possible. These clinical differences may have
influenced the differences in survival. Using the Kaplan-Meier
method, the survival time was significantly shorter in the
sorafenib-I subgroup compared to that in the sorafenib-II subgroup
and the HAIC group (Fig. 2). In
addition, short-term sorafenib administration (<60 days) was an
independent factor predicting a poor prognosis in multivariate
analysis using a Cox proportional hazards model (Table V). The DCP level has been reported
to be a factor contributing to the prognosis of HCC (28). Since the condition of the patients
in the sorafenib-I subgroup influenced the prognosis, in addition
to DCP, it is likely that severe early side effects of sorafenib
and the associated discontinuation of treatment markedly influence
the survival of patients with advanced HCC.
Only a few treatment methods are available for
advanced HCC accompanied by portal invasion in the first portal
branch or main portal branch (29,30).
In the treatment algorithm for HCC in Japan, sorafenib and HAIC are
recommended for such cases of advanced HCC, but the first choice
has not been specified. Based on our results, the survival rate did
not differ significantly between sorafenib treatment and HAIC
(Fig. 1), but the survival rate of
patients was lower in patients who discontinued sorafenib treatment
in the early phase of therapy compared to the survival rate of
patients who tolerated long-term sorafenib treatment (sorafenib-II)
and those treated with HAIC (Fig.
2). In addition, HAIC was applicable after side
effect-associated discontinuation in some cases in patients treated
with long-term sorafenib, whereas sorafenib was not administered to
any patients in the HAIC group because the discontinuation of HAIC
was due to disease progression in all cases. Sorafenib in
combination with other treatments, including HAIC, is likely to
markedly prolong the overall survival of HCC patients, including
those in an advanced stage (31).
However, Abou-Alfa et al concluded that the combination of
sorafenib and intravenous doxorubicin is not yet indicated for
routine clinical use, based on the results of a double-blind phase
II multinational study (32).
Based on these findings, we speculate that patients with advanced
HCC accompanied by portal invasion in the first portal branch or
main portal branch should first be treated with sorafenib if they
are likely to tolerate sorafenib for more than 60 days. HAIC should
then be considered as an additional treatment for cases in which
sorafenib cannot be continued.
The effect of sorafenib has been suggested to depend
on the treatment period, which is influenced by the development of
serious side effects. Vincenzi et al reported that the tumor
control rate was higher in patients with skin toxicity of grade 1
or higher than in those without this toxicity (48.3 vs. 19.4%)
(33). After dose reduction for
skin toxicity, it has been suggested that the dose can be increased
again in some cases after amelioration of the adverse effect
(34). Thus, if long-term
sorafenib administration can be achieved by controlling skin
toxicity, the therapeutic effect may be further increased. Several
background factors such as single nucleotide polymorphisms (SNPs)
that contribute to the therapeutic effect of interferon on chronic
hepatitis C have been reported (35,36).
This suggests that tolerability of long-term sorafenib
administration may also be predictable before treatment, which may
allow the selection of patients for whom sorafenib is appropriate.
In this study, we were unable to identify any factors that
significantly discriminated between patients with and without
tolerability of long-term sorafenib. Thus, further analysis,
including examination of SNPs, is required for safe and effective
sorafenib treatment for HCC in an increased number of cases
(37).
There were several limitations to this study. First,
this was a retrospective study, and the number of cases was small;
therefore, a bias due to the unbalanced number of cases cannot be
ruled out. However, no previous study has compared the effect of
sorafenib on advanced HCC with those of other treatments, and makes
the findings valuable in the absence of other information. Second,
HAIC was performed after discontinuation of sorafenib treatment due
to side effects in 8 cases; therefore, the effect of sorafenib
alone could not be assessed in these cases. However, less than one
cycle of HAIC was performed after discontinuation of sorafenib,
suggesting that the additional effect of HAIC may have been
limited.
In conclusion, treatment of advanced HCC with
sorafenib may achieve a survival rate equivalent to that achieved
by HAIC, through control of disease progression independent of
tumor size reduction. However, early discontinuation of sorafenib
due to adverse effects may be associated with a poor prognosis, and
further investigation of the eligibility criteria for sorafenib
administration is required.
References
|
1.
|
Cabibbo G, Latteri F, Antonucci M and
Craxì A: Multimodal approaches to the treatment of hepatocellular
carcinoma. Nat Clin Pract Gastroenterol Hepatol. 6:159–169. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Kim BK, Park JY, Choi HJ, Kim DY, Ahn SH,
Kim JK, Lee DY, Lee KH and Han KH: Long-term clinical outcomes of
hepatic arterial infusion chemotherapy with cisplatin with or
without 5-fluorouracil in locally advanced hepatocellular
carcinoma. J Cancer Res Clin Oncol. June 16–2010.(Epub ahead of
print).
|
|
3.
|
Ikeda M, Maeda S, Ashihara H, Nagahama H,
Tanaka M and Sasaki Y: Transcatheter arterial infusion chemotherapy
with cisplatin-lipiodol suspension in patients with hepatocellular
carcinoma. J Gastroenterol. 45:60–67. 2010. View Article : Google Scholar
|
|
4.
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR,
Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici
M, Voliotis D and Bruix J: SHARP investigators study group:
sorafenib in advanced hepatocellular carcinoma. N Engl J Med.
359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J,
Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D and Guan Z:
Efficacy and safety of sorafenib in patients in Asia-Pacific region
with advanced hepatocellular carcinoma: a phase III randomized,
double-blind, placebo-controlled trial. Lancet Oncol. 10:25–34.
2009. View Article : Google Scholar
|
|
6.
|
Llovet JM, Di Bisceglie AM, Bruix J,
Kramer BS, Lencioni R, Zhu AX, Sherman M, Schwartz M, Lotze M,
Talwalkar J and Gores GJ: Panel of experts in HCC-design clinical
trials: design and endpoints of clinical trials in hepatocellular
carcinoma. J Natl Cancer Inst. 100:698–711. 2008. View Article : Google Scholar
|
|
7.
|
Kudo M: The 2008 Okuda lecture: management
of hepatocellular carcinoma: from surveillance to
molecular-targeted therapy. J Gastroenterol Hepatol. 25:439–452.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Cabrera R and Nelson DR: The management of
hepatocellular carcinoma. Aliment Pharmacol Ther. 31:461–476. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Urabe T, Kaneko S, Matsushita E, Unoura M
and Kobayashi K: Clinical pilot study of intrahepatic arterial
chemotherapy with methotrexate, 5-fluorouracil, cisplatin and
subcutaneous interferon-alpha-2b for patients with locally advanced
hepatocellular carcinoma. Oncology. 55:39–47. 1998. View Article : Google Scholar
|
|
10.
|
Kuroda M, Kobayashi Y, Urawa N, Yamamoto
M, Mifuji R, Araki J, Tanaka H, Horiike S, Itani T, Furjita N,
Konishi M, Iwasa M, Kaito M and Adachi Y: Hepatic arterial infusion
of 5-fluorouracil in combination with subcutaneous interferon-alpha
for advanced hepatocellular carcinoma. Hepatogastroenterology.
54:518–521. 2007.
|
|
11.
|
Uka K, Aikata H, Takaki S, Miki D, Kawaoka
T, Jeong SC, Takahashi S, Toyota N, Ito K and Chayama K:
Pretreatment predictor of response, time to progression, and
survival to intraarterial 5-fluorouracil/interferon combination
therapy in patients with advanced hepatocellular carcinoma. J
Gastroenterol. 42:845–853. 2007. View Article : Google Scholar
|
|
12.
|
Ando E, Tanaka M, Yamashita F, Kuromatsu
R, Yutani S, Fukumori K, Sumie S, Yano Y, Okuda K and Sata M:
Hepatic arterial infusion chemotherapy for advanced hepatocellular
carcinoma with portal vein tumor thrombosis: analysis of 48 cases.
Cancer. 95:588–595. 2002. View Article : Google Scholar
|
|
13.
|
Tanioka H, Tsuji A, Morita S, Horimi T,
Takamatsu M, Shirasaka T, Mizushima T, Ochi K, Kiura K and Tanimoto
M: Combination chemotherapy with continuous 5-fluorouracil and
low-dose cisplatin infusion for advanced hepatocellular carcinoma.
Anticancer Res. 23:1891–1897. 2003.PubMed/NCBI
|
|
14.
|
Yoshikawa M, Ono N, Yodono H, Ichida T and
Nakamura H: Phase II study of hepatic arterial infusion of a
fine-powder formulation of cisplatin for advanced hepatocellular
carcinoma. Hepatol Res. 38:474–483. 2008. View Article : Google Scholar
|
|
15.
|
Kondo M, Nagano H, Sakon M, Yamamoto H,
Morimoto O, Arai I, Miyamoto A, Eguchi H, Dono K, Nakamori S,
Umeshita K, Wakasa K, Ohmoto Y and Monden M: Expression of
interferon alpha/beta receptor in human hepatocellular carcinoma.
Int J Oncol. 17:83–88. 2000.PubMed/NCBI
|
|
16.
|
Ota H, Nagano H, Sakon M, Eguchi H, Kondo
M, Yamamoto T, Nakamura M, Damdinsuren B, Wada H, Marubashi S,
Miyamoto A, Dono K, Umeshita K, Nakamori S, Wakasa K and Monden M:
Treatment of hepatocellular carcinoma with major portal vein
thrombosis by combined therapy with subcutaneous interferon-alpha
and intra-arterial 5-fluorouracil; role of type 1 interferon
receptor expression. Br J Cancer. 93:557–564. 2005. View Article : Google Scholar
|
|
17.
|
Kudo M: Current status of molecularly
targeted therapy for hepatocellular carcinoma: clinical practice.
Int J Clin Oncol. 15:242–255. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Shen YC, Hsu C and Cheng AL: Molecular
targeted therapy for advanced hepatocellular carcinoma: current
status and future perspectives. J Gastroenterol. 45:794–807. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Park JY, Ahn SH, Yoon YJ, Kim JK, Lee HW,
Lee do Y, Chon CY, Moon YM and Han KH: Repetitive short-course
hepatic arterial infusion chemotherapy with high-dose
5-fluorouracil and cisplatin in patients with advanced
hepatocellular carcinoma. Cancer. 110:129–137. 2007. View Article : Google Scholar
|
|
20.
|
Furuse J, Ishii H, Nakachi K, Suzuki E,
Shimizu S and Nakajima K: Phase I study of sorafenib in Japanese
patients with hepatocellular carcinoma. Cancer Sci. 99:159–165.
2008.PubMed/NCBI
|
|
21.
|
Ando E, Yamashita F, Tanaka M and Tanikawa
K: A novel chemotherapy for advanced hepatocellular carcinoma with
tumor thrombosis of the main trunk of the portal vein. Cancer.
79:1890–1896. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Therasse P, Arbuck SG, Eisenhauer EA,
Wanders J, Kaplan RS, Rubinstein L, Verweij J, van Glabbeke M, van
Oosterom AT, Christian MC and Gwyther SG: New guidelines to
evaluate the response to treatment in solid tumors. European
Organization for Research and Rreatment of Cancer, national Cancer
Institute of the United States, national Cancer Institute of
Canada. J Natl Cancer Inst. 92:205–216. 2000. View Article : Google Scholar
|
|
23.
|
Japanese translation of common terminology
criteria for adverse events (CTCAE), and instructions and
guidelines. Int J Clin Oncol. 9(Suppl. 3): S1–S82. 2004.(In
Japanese).
|
|
24.
|
Rouillier P, Senesse P, Cottet V, Valléau
A, Faivre J and Boutron-Ruault MC: Dietary patterns and the
adenomacarcinoma sequence of colorectal cancer. Eur J Nutr.
44:311–318. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Furuse J: Sorafenib for the treatment of
unresectable hepatocellular-carcinoma. Biologics. 2:779–788.
2008.PubMed/NCBI
|
|
26.
|
Abou-Alfa GK, Schwartz L, Ricci S, Amadori
D, Santoro A, Figer A, de Greve J, Douillard JY, Lathia C, Schwartz
B, Taylor I, Moscovici M and Saltz LB: Phase II study of sorafenib
in patients with advanced hepatocellular carcinoma. J Clin Oncol.
24:4293–4300. 2006. View Article : Google Scholar
|
|
27.
|
Yang CH, Lin WC, Chuang CK, Chang YC, Pang
ST, Lin YC, Kuo TT, Hsieh JJ and Chang JW: Hand-foot skin reaction
in patients treated with sorafenib: a clinicopathological study of
cutaneous manifestations due to multitargeted kinase inhibitor
therapy. Br J Dermatol. 158:592–596. 2008. View Article : Google Scholar
|
|
28.
|
Hakamada K, Kimura N, Miura T, Morohashi
H, Ishido K, Nara M, Toyoki Y, Narumi S and Sasaki M:
Des-gamma-carboxy prothrombin as an important prognostic indicator
in patients with small hepatocellular carcinoma. World J
Gastroenterol. 14:1370–1377. 2008. View Article : Google Scholar
|
|
29.
|
Bruix J and Llovet JM: Prognostic
prediction and treatment strategy in hepatocellular carcinoma.
Hepatology. 35:519–524. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Woo HY, Bae SH, Park JY, Han KH, Chun HJ,
Choi BG, Im HU, Choi JY, Yoon SK, Cheong JY, Cho SW, Jang BK, Hwang
JS, Kim SG, Kim YS, Seo YS, Yim HJ and Um SH: A randomized
comparative study of high-dose and low-dose hepatic arterial
infusion chemotherapy for intractable, advanced hepatocellular
carcinoma. Cancer Chemother Pharmacol. 65:373–382. 2010. View Article : Google Scholar
|
|
31.
|
Kudo M and Ueshima K: Positioning of a
molecular-targeted agent, sorafenib, in the treatment algorithm for
hepatocellular carcinoma and implication of many complete remission
cases in Japan. Oncology. 78(Suppl. 1): S154–S166. 2010. View Article : Google Scholar
|
|
32.
|
Abou-Alfa GK, Johnson P, Knox JJ, Capanu
M, Davidenko I, Lacava J, Leung T, Gansukh B and Saltz LB:
Doxorubicin plus sorafenib vs. doxorubicin alone in patients with
advanced hepatocellular carcinoma: a randomized trial. JAMA.
304:2154–2160. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Vincenzi B, Santini D, Russo A, Addeo R,
Giuliani F, Montella L, Rizzo S, Venditti O, Frezza AM, Caraglia M,
Colucci G, del Prete S and Tonini G: Early skin toxicity as a
predictive factor for tumor control in hepatocellular carcinoma
patients treated with sorafenib. Oncologis. 15:85–92. 2010.
View Article : Google Scholar
|
|
34.
|
La Vine DB, Coleman TA, Davis CH,
Carbonell CE and Davis WB: Frequent dose interruptions are required
for patients receiving oral kinase inhibitor therapy for advanced
renal cell carcinoma. Am J Clin Oncol. 33:217–220. 2010.PubMed/NCBI
|
|
35.
|
Tanaka Y, Nishida N, Sugiyama M, Tokunaga
K and Mizokami M: Lambda-interferons and the single nucleotide
polymorphisms: a milestone to tailor-made therapy for chronic
hepatitis C. Hepatol Res. 40:449–460. 2010. View Article : Google Scholar
|
|
36.
|
Okanoue T, Itoh Y, Hashimoto H, Yasui K,
Minami M, Takehara T, Tanaka E, Onji M, Toyota J, Chayama K,
Yoshioka K, Izumi N, Akuta N and Kumada H: Predictive values of
amino acid sequences of the core and nS5A regions in antiviral
therapy for hepatitis C: a Japanese multi-center study. J
Gastroenterol. 44:952–963. 2009. View Article : Google Scholar
|
|
37.
|
Villanueva A, Minguez B, Forner A, Reig M
and Llovet JM: Hepatocellular carcinoma: novel molecular approaches
for diagnosis, prognosis, and therapy. Annu Rev Med. 61:317–328.
2010. View Article : Google Scholar : PubMed/NCBI
|